Abstract
Background
The combination of gemcitabine and docetaxel (GT) has been demonstrated to be effective against various types of solid tumors, including sarcoma. However, the regimen has not been confirmed in large, well-designed clinical trials in refractory metastatic osteosarcoma.
Methods
We retrospectively reviewed the records of patients with refractory metastatic osteosarcoma at Peking University People’s Hospital who were treated with gemcitabine (1000 mg/m2) intravenously (IV) on Day 1 and Day 8, and docetaxel (75 mg/m2) IV on Day 8, repeated every 21 days.
Results
A total of 52 patients with a median age of 18.4 years were treated with GT at the Peking University People’s Hospital from August 2012 to August 2017. A total of 174 courses were administered. Only five patients with pulmonary metastasis achieved a best response of stable disease (SD), while all other patients had progressive disease. The result was disappointing with an ORR of 0%, a DCR of 9.6%, and a median DOR of 3.5 months. Grade 3 or 4 toxicities were observed in 69 (39.7%) courses and in 28 (53.8%) patients, most of which were myelosuppression, especially thrombocytopenia. No fatal adverse effect (AE) was found.
Conclusion
The combination of gemcitabine and docetaxel (GT) as a salvage regimen is well-tolerated but not as effective as expected in refractory metastatic osteosarcoma. This report highlights the need for the development of new approaches with higher activity in these patients.
Similar content being viewed by others
Background
Following the implementation of chemotherapy in the 1970s, the treatment of osteosarcoma (OS) has made important progress. However, survival rates continue to be unsatisfactory in the refractory metastatic setting [1].Treatment of these patients is usually difficult and disappointing [2,3,4,5].
The first line chemotherapy regimens for patients with OS are designed typically based on four drugs, namely high-dose methotrexate (HDMTX), doxorubicin, cisplatin and ifosfamide [6]. These agents have been incorporated into various chemotherapy protocols. However, OS can develop resistance to conventional agents, resulting in tumor progression or relapse. Local treatment methods such as surgical resection and sometimes radiotherapy are useful in these patients, but unfortunately not able to stop widespread metastases [2]. Once metastasis has occurred and patients have shown refractory to conventional agents, none of current salvage treatments has provided satisfactory results to significantly prolong overall survival [1, 3, 6, 7].
Gemcitabine hydrochloride is a pyrimidine nucleoside analog. Gemcitabine is able to inhibit DNA replication through two different mechanisms: inhibiting DNA synthesis and obstructing repair mechanisms [8]. Docetaxel is a semisynthetic analog of paclitaxel. Docetaxel causes cell cycle arrest and induces apoptosis by promoting microtubule assembly and inhibiting their disassembly. The combination of gemcitabine and docetaxel were initially studied due to their different mechanisms of action and their partially non-overlapping toxicity. Synergistic antitumor activity of the combination of gemcitabine and docetaxel (GT) has been demonstrated in several in vitro studies, including OS [9].
The GT regimen has been used as salvage therapy in several soft tissue sarcoma (STS). An initial clinical study evaluating the efficacy of GT demonstrated a response rate of 53% in 34 adult patients with leiomyosarcoma [10]. A subsequent retrospective study of 35 patients with bone sarcoma and STS treated with GT had an objective response rate (ORR) of 43%, but they had several different tumor types [9]. Only a few studies have reported efficacy and toxicity in OS, including several retrospective [11,12,13,14,15,16,17] and one prospective [18] clinical trials. Unfortunately, the results of these studies were controversial and the number of patients was relatively small, ranging from 4 to 35.
Based on the encouraging results in sarcoma, and due to a lack of effective salvage regimens for OS, we have applied GT to patients with refractory metastatic OS at Peking University People’s Hospital from the year of 2012. In this study, we retrospectively reviewed the records of patients treated with GT, with the following purposes: (1) To establish whether the GT regimen is effective in refractory metastatic OS, including ORR, DCR and DOR. (2) To examine the tolerability of GT regimen in heavily treated patients with refractory metastatic OS.
Methods
Eligibility
We retrospectively reviewed the patients treated with GT at Peking University People’s Hospital from August 2010 to August 2017. Information about their treatment courses were obtained from the pharmacy medical records in the hospital. Patients were selected according to the following criteria: (1) high-grade OS confirmed histologically; (2) Disease progression was confirmed during the first line treatment with 4-drug protocols consisting of doxorubicin, cisplatin, high-dose methotrexate and ifosfamide (more than 3 months from the initiation of the first line chemotherapy); (3) primary or secondary metastatic disease; (4) received more than 2 courses of the GT regimen; (5) no concurrent treatment was given while on the GT regimen; (6) follow-up information and evaluation after chemotherapy were available.
Regimen
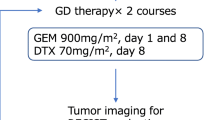
Gemcitabine (1000 mg/m2) was given intravenously (IV) over 90 min on day 1 and 8. Ondansetron (16 mg) was administered prior to initiation of chemotherapy on day 1 and 8. Docetaxel (75 mg/m2) was given IV on day 8 over 60 min after gemcitabine. To minimize the severity and incidence of hypersensitivity and the fluid retention associated with docetaxel, dexamethasone treatment was given daily from day 7 to day 9. Each cycle was 21 days. Cycles of chemotherapy were administered until off study criteria were met. Myeloid growth factor support between cycles was given when hematologic toxicity was observed.
Assessment of toxicity
The toxicity associated with chemotherapy was documented for each cycle according to the National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE version 4.0) [19]. For the patients with unacceptable toxicity, treatment was postponed for up to 42 days, initiated at day 1 of any cycle to allow recovery from toxicity until grade 3/4 symptoms had been resolved. Subsequently, the dosage of GT was resumed at 75% of the previous one. Any patient requiring > 42 days recovery time or > 2 reductions due to toxicity was to be withdrawn from the study.
Assessment of efficacy
According to the regular protocol for patients with refractory sarcoma in our hospital, the baseline assessment included chest computed tomography (CT, with each layer ≤5 mm) and bone scan or [18F]2-fluoro-2-deoxy-D-glucose-positron emission tomography (FDG-PET). If the patients had lesions other than lung metastasis, CT and/or magnetic resonance imaging (MRI) of those lesions was required. Patient follow-up included a chest CT, a CT scan and/or MRI of the baseline lesion every 2 months, and radionuclide bone scans or PET/CT every 6 months. Response to GT therapy was assessed by the RECIST 1.1 criteria [20]. A patient with the outcome of partial response (PR), complete response (CR) or progressive disease (PD) at any stage was scored as having that overall outcome, a patient with the outcome of stable disease (SD) was re-evaluated after two subsequent cycles of therapy. The ORR was defined as the percentage of patients experiencing a CR or PR. The DCR was defined as the percentage of CR, PR or SD. The DOR was defined as the time interval from the initial of treatment to the point of PD in patients who were previously scored as CR, PR or SD. Treatment with GT was to be stopped in case of life-threatening toxicity or progression of the disease. In such cases, patients were encouraged to take part in other clinical trials with targeted therapy, surgery or definitive radiotherapy if possible. Progression-free survival was analyzed using the Kaplan-Meier Method.
Results
Patients characteristics
A total of 52 patients and 174 treatment courses were identified. The characteristics of the patients included in this study are summarized in Table 1. The median age of the patients was 18.4 years (range 8–47 years). Among the patients, 47 (90.4%) had a primary lesion in the extremities, while only five patients had primary lesions in the axial skeleton, with two in the sacrum, one in the lumbar region and the other two in the pelvic region. The Eastern Cooperative Oncology Group (ECOG) score in these patients was relatively high, with only 35 (67.3%) of them having a score of less than 2. At the time of the initial diagnosis, 36 (69.2%) patients had localized disease. Before the GT treatment, 40 (77.0%) patients had metastatic lesions in lung, 4 (7.7%) in bone, and 8 (15.4%) in multiple organs. All patients had previously received chemotherapy of 4-drug protocol, and most of them (44/52, 84.6%) were heavy-treated, with a chemotherapy period of more than 6 months, while eight patients had received prior radiation therapy and 48 had undergone previous surgery. All these patients were classified as conventional OS.
Response and survival
Unfortunately, no PR or CR was confirmed in this study. The ORR for the confirmed responses according to RECIST1.1 guidelines was 0%. Only five patients with pulmonary metastasis were confirmed as SD. No PR or CR was observed in patients with extrapulmonary lesions, including recurrent lesions and extrapulmonary metastatic lesions. The disease control rate (DCR) was 9.6% (Table 2). Three of the patients had received four courses of GT before PD was observed. Two patients had received six courses of GT in 5.1 months. The median duration of response (DOR) was 3.5 (range 2.0–5.7) months. All the other 47 patients had shown an outcome of PD, in which one patient with prior pulmonary metastasis died due to the rupture of a new onset intracranial lesion after the first course of GT. For patients who experienced PD at first or in the subsequent evaluations, enlargement of the primary lesions was the most common reason (48.1%). Additionally, 23.1% patients showed new lesions while baseline lesions remained stable. Also, 28.8% patients experienced both new lesions and enlargement of baseline lesions. The progression-free survival curve is shown in Fig. 1.
Toxicity
Grade 3 or 4 toxicities were observed in 39.7% courses and in 53.8% of the patients. Myelosuppression, especially thrombocytopenia, was the most common toxicity observed. No fatal adverse effect (AE) occurred. The Grade 3 and 4 toxicities observed in the 174 courses of the GT regimen and 52 patients are summarized in Table 3. Neutropenia was found in 55 (31.6%) courses and in 22 (42.3%) patients. Thrombocytopenia was found in 66 (37.9%) courses and in 28 (53.8%) patients. Anemia was found in 52 (29.9%) courses and in 16 (30.8%) patients. Other Grade 3 or 4 toxicities were found in the following aspects: (1) gastrointestinal disorders, including nausea, vomiting, diarrhea and oral mucositis; (2) hepatic disorder, characterized by a transient elevation of alanine transaminase (ALT) or aspartate transaminase (AST); (3) metabolism and nutrition disorders, including hypokalemia, hypocalcemia and hyperglycemia in one patient with prior diabetes. All incidences of Grade 3 or 4 toxicities were less than 5% excluding blood and lymphatic system disorder.
Discussion
The GT has a broad spectrum of clinical activity in patients with carcinoma and sarcoma. Research on leiomyosarcoma encouraged the use of GT in sarcoma. In 2002 Hensley reported a retrospective study of 34 leiomyosarcoma with an ORR of 53% [10]. The French Sarcoma Group reported in 2006 an ORR of 24% in 133 STS including leiomyosarcoma [21]. Gemcitabine as a single drug treatment was reported as an effective agent in angiosarcoma by the Italian Rare Cancer Network, with an ORR of 68% [22]. Previous studies have demonstrated that the regimen is well tolerated. However, the prognosis of refractory metastatic OS was disappointing. Doctors have tried to apply the same regimen in this set of patients. Unfortunately, the results of the studies using the same dosage and schedule in OS as that in STS were controversial and the number of patients was relatively small, ranging from 4 to 35 [11,12,13,14,15,16,17,18, 27, 28]. We used the GT in refractory metastatic OS from 2012 to 2017 and used the collected data to investigate the value of GT as salvage therapy. However, in this retrospective study, we did not find evidence to demonstrate that it as an active regimen in OS, with a ORR of 0%, especially in patients with extrapulmonary lesions, since they all experienced disease progression during the GT treatment. In addition, in our study, most patients (48.1%) were evaluated as PD due to the enlargement of baseline lesions. In seven patients with oligometastases who were recorded as PD after GT treatment, their local treatment, such as surgical resection or definitive radiotherapy, was administered based on a multidisciplinary discussion. Four of them had developed secondary metastasis during follow-up (mean 6.4 months, range 3.2–14.5 months), while the other three patients remained disease-free at the latest follow-up. This reminds us that local treatment remains essential for patients with resectable lesions.
This study has several limitations. First, as in most of other reports, our study was retrospective, and most of the patients were heavily treated with various modalities including surgery, radiation, and biological agents, making the interpretation of our data difficult. To guarantee the uniformity of the data, the inclusion criteria were designed and rigidly implemented. The pharmacy medical records of these 52 patients were separately reviewed by two different doctors. Second, overall survival was not investigated in our study. Most of the 52 patients showed PD after the GT regimen, and various salvage therapies were given afterwards, including targeted therapy, radiotherapy, palliative surgery and symptomatic and supportive treatment. The following treatments were considered to have an impact on the overall survival of each patient. In this study, however, we just focused on the GT regimen and overall survival was not adequate to address the activity of a certain regimen.
In previous studies, GT was used as a second-line chemotherapy and response data was reported in ten of them [11,12,13,14,15,16,17,18, 23, 24, 27, 28]. These studies are reviewed in Table 4. The reported ORRs ranged from 0 to 30%, while the DCR ranged from 22.3 to 75%. All of these studies were retrospective, except for a prospective study conducted by Fox E. et al. that was suspended due to poor activity, in which no CR and only one PR was met in fourteen patients [18]. The tumor response rate observed in our study, which was similar to that of Fox et al. [18]. was not as promising as others. The following reasons should be considered to explain the poor outcome. First, in previous studies GT was often used as adjuvant therapy concurrently with or prior to local treatment, which was likely to overestimate the activity of chemotherapy itself. In 2006, Lee J.A. et al. reported a retrospective study including 53 patients with OS using the GT regimen as adjuvant (n = 25) or palliative chemotherapy (n = 28). In this study all patients who showed a response, both PR or complete metabolic response (CMR), according to PET/CT, had concurrently received local treatment, such as radiotherapy or surgical resection of metastatic lesions. For patients that received GT as palliative treatment alone, only one patient was evaluated as SD, while the other fourteen patients were evaluated as PD. In our study, patients were treated with GT as a single treatment without any concurrent therapy. This should be considered when drawing conclusions. Second, 3/10 [12, 13, 17], 2/10 [15, 24] and [27, 28] of the previous studies reviewed in Table 4 were reported from the same hospital or group at the same time. Thus, the duplication of data should be considered in the analysis. Finally, when comparing with other studies in which both relapsed and refractory patients were included (Table 4), only refractory cases were included in our study. As shown in previous studies, late relapse favorably impacts outcome after relapse [7, 29]. We assumed that the more progressive character in this set of patients who were resistant to first-line chemotherapy was another important reason for the poor response rate. Also, any generalization outside the specific subset of patients studied should be carefully omitted.
The toxicity of the GT regimen was acceptable in the current study. Similar to previous reports in OS, Ewing sarcoma and STS [10, 21, 26], the most common grade 3/4 AE related to the GT therapy in our study was blood and lymphatic system disorders, especially neutropenia and thrombocytopenia. Grades 3 and 4 electrolyte abnormalities and transient elevations in ALT/AST were also observed, but less commonly (< 5%). Other common AEs related to gemcitabine and docetaxel, such as rushes, fluid retention and weight gain were not observed in this study. Also, no hypersensitive reaction was found. As patients in our study were already heavily-treated before GT administration, one third of whom had a ECOG performance score of more than 2, the toxicity of this regimen was relatively mild compared with other second-line regimen in OS, such as IE, CE and CT [25].
Recently, small molecule anti-angiogenesis tyrosine kinase inhibitors (TKIs), such as sorafenib, have exhibited more promising potential compared to other target therapies in OS patients [30, 31]. which, in a sense, have become a breakthrough second-line therapy for OS. We have also changed our strategy in these rapidly exacerbating patients and conducted a clinical trial to determine the efficacy of apatinib, an inhibitor for VEGFR-2, in OS. Based on this result, the GT should only be recommended as salvage therapy in frail patients nowadays.
Conclusions
The GT is recommended in several guidelines as a second-line therapy in OS. However, our study has demonstrated the low tumor response rate in this palliative set of patients. Although this regimen is well tolerated, the disappointing activity prevents us from using it as the salvage therapy in the future. We wonder whether the effectiveness of this regimen is overestimated in the treatment of refractory OS. More effective regimen should be considered and future research should be directed toward more promising agents. Based on the current results of clinical trials in OS, anti-angiogenesis therapy could be a better choice for refractory patients.
Abbreviations
- AE:
-
Adverse effect
- CE:
-
Cyclophosphamide-Etoposide
- CR:
-
Complete response
- CT:
-
Computed Tomography
- CTCAE:
-
National Cancer Institute Common Terminology Criteria for Adverse Events
- DCR:
-
Disease control rate
- DOR:
-
Duration of response
- FDG-PET:
-
[18F]2-fluoro-2-deoxy-D-glucose-positron emission tomography
- GT:
-
Gemcitabine and Docetaxel
- HDMTX:
-
High-dose methotrexate
- IE:
-
Ifosfamide-Etoposide
- IV:
-
Intravenous
- MRI:
-
Magnetic Resonance Imaging
- NCI:
-
National Cancer Institute
- ORR:
-
Objective response rate
- OS:
-
Osteosarcoma
- PD:
-
Progressive disease
- PR:
-
Partial response
References
Kempf-Bielack B, et al. Osteosarcoma relapse after combined modality therapy: an analysis of unselected patients in the cooperative osteosarcoma study group (COSS). J Clin Oncol. 2005;23(3):559–68.
Bielack SS, et al. Prognostic factors in high-grade osteosarcoma of the extremities or trunk: an analysis of 1,702 patients treated on neoadjuvant cooperative osteosarcoma study group protocols. J Clin Oncol. 2002;20(3):776–90.
Chou AJ, Geller DS, Gorlick R. Therapy for osteosarcoma: where do we go from here? Paediatr Drugs. 2008;10(5):315–27.
Bacci G, et al. Bone metastases in osteosarcoma patients treated with neoadjuvant or adjuvant chemotherapy: the Rizzoli experience in 52 patients. Acta Orthop. 2006;77(6):938–43.
Kager L, et al. Primary metastatic osteosarcoma: presentation and outcome of patients treated on neoadjuvant cooperative osteosarcoma study group protocols. J Clin Oncol. 2003;21(10):2011–8.
Luetke A, et al. Osteosarcoma treatment - where do we stand? A state of the art review. Cancer Treat Rev. 2014;40(4):523–32.
Bacci G, et al. Treatment and outcome of recurrent osteosarcoma: experience at Rizzoli in 235 patients initially treated with neoadjuvant chemotherapy. Acta Oncol. 2005;44(7):748–55.
Gandhi V, et al. Excision of 2′,2′-difluorodeoxycytidine (gemcitabine) monophosphate residues from DNA. Cancer Res. 1996;56(19):4453–9.
Leu KM, et al. Laboratory and clinical evidence of synergistic cytotoxicity of sequential treatment with gemcitabine followed by docetaxel in the treatment of sarcoma. J Clin Oncol. 2004;22(9):1706–12.
Hensley ML, et al. Gemcitabine and docetaxel in patients with unresectable leiomyosarcoma: results of a phase II trial. J Clin Oncol. 2002;20(12):2824–31.
Navid F, et al. Combination of gemcitabine and docetaxel in the treatment of children and young adults with refractory bone sarcoma. Cancer. 2008;113(2):419–25.
Yu WX, et al. Comparison of pemetrexed plus cisplatin with gemcitabine plus docetaxel in refractory/metastatic osteosarcoma: clinical outcomes from a retrospective database monitored in a single institute. Oncol Lett. 2014;8(5):2243–8.
He A, et al. Comparison of pirarubicin-based versus gemcitabine-docetaxel chemotherapy for relapsed and refractory osteosarcoma: a single institution experience. Int J Clin Oncol. 2013;18(3):498–505.
Rapkin L, et al. Gemcitabine and docetaxel (GEMDOX) for the treatment of relapsed and refractory pediatric sarcomas. Pediatr Blood Cancer. 2012;59(5):854–8.
Song BS, et al. Gemcitabine and docetaxel for the treatment of children and adolescents with recurrent or refractory osteosarcoma: Korea Cancer center hospital experience. Pediatr Blood Cancer. 2014;61(8):1376–81.
Palmerini E, et al. Gemcitabine and docetaxel in relapsed and unresectable high-grade osteosarcoma and spindle cell sarcoma of bone. BMC Cancer. 2016;16:280.
Qi WX, et al. Efficacy and safety of gemcitabine-docetaxel combination therapy for recurrent or refractory high-grade osteosarcoma in China: a retrospective study of 18 patients. Jpn J Clin Oncol. 2012;42(5):427–31.
Fox E, et al. Phase II study of sequential gemcitabine followed by docetaxel for recurrent Ewing sarcoma, osteosarcoma, or unresectable or locally recurrent chondrosarcoma: results of sarcoma Alliance for research through collaboration study 003. Oncologist. 2012;17(3):321.
Chen AP, et al. Grading dermatologic adverse events of cancer treatments: the common terminology criteria for adverse events version 4.0. J Am Acad Dermatol. 2012;67(5):1025–39.
Wahl RL, et al. From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med. 2009;50(Suppl 1):122S–50S.
Bay JO, et al. Docetaxel and gemcitabine combination in 133 advanced soft-tissue sarcomas: a retrospective analysis. Int J Cancer. 2006;119(3):706–11.
Stacchiotti S, et al. Gemcitabine in advanced angiosarcoma: a retrospective case series analysis from the Italian rare Cancer network. Ann Oncol. 2012;23(2):501–8.
Gosiengfiao Y, et al. Gemcitabine with or without docetaxel and resection for recurrent osteosarcoma: the experience at Children's Memorial Hospital. J Pediatr Hematol Oncol. 2012;34(2):e63–5.
Lee JA, et al. Higher gemcitabine dose was associated with better outcome of osteosarcoma patients receiving gemcitabine-docetaxel chemotherapy. Pediatr Blood Cancer. 2016;63(9):1552–6.
Xiao X, Wang W, Wang Z. The role of chemotherapy for metastatic, relapsed and refractory osteosarcoma. Paediatr Drugs. 2014;16(6):503–12.
Dileo P, et al. Gemcitabine and vinorelbine combination chemotherapy for patients with advanced soft tissue sarcomas: results of a phase II trial. Cancer. 2007;109(9):1863–9.
Tanaka K, et al. Feasibility and efficacy of gemcitabine and docetaxel combination chemotherapy for bone and soft tissue sarcomas: multi-institutional retrospective analysis of 134 patients. World J Surg Oncol. 2016;14(1):306.
Takahashi M, et al. Efficacy and safety of gemcitabine plus docetaxel in Japanese patients with unresectable or recurrent bone and soft tissue sarcoma: results from a single-institutional analysis. PLoS One. 2017;12(5):e0176972.
Leary SE, et al. Survival of pediatric patients after relapsed osteosarcoma: the St. Jude Children's Research Hospital experience. Cancer. 2013;119(14):2645–53.
Grignani G, et al. A phase II trial of sorafenib in relapsed and unresectable high-grade osteosarcoma after failure of standard multimodal therapy: an Italian sarcoma group study. Ann Oncol. 2012;23(2):508–16.
Grignani G, et al. Sorafenib and everolimus for patients with unresectable high-grade osteosarcoma progressing after standard treatment: a non-randomised phase 2 clinical trial. Lancet Oncol. 2015;16(1):98–107.
Acknowledgements
We are thankful to our colleagues in the Pathology Department of Peking University People’s Hospital who provided expertise that greatly assisted the study.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Contributions
WG devised the project, the main conceptual ideas and proof outline. JX worked out almost all of the technical details, and performed the statistical analysis. LX verified the analytical methods. All authors discussed the results and contributed to the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for the study was obtained from the ethics committee of Peking University People’s Hospital (Beijing, China). No consent forms were needed because this was a retrospective study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Xu, J., Guo, W. & Xie, L. Combination of gemcitabine and docetaxel: a regimen overestimated in refractory metastatic osteosarcoma?. BMC Cancer 18, 987 (2018). https://doi.org/10.1186/s12885-018-4872-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-018-4872-x