Abstract
Background
Patients suffering from squamous cell carcinoma of the larynx (LSCC) with lymphatic metastasis have a relatively poor prognosis and often require radical therapeutic management. The mechanisms which drive metastasis to the lymph nodes are largely unknown but may be promoted by a pro-angiogenic tumor microenvironment. In this study, we examined whether the number of microvessels and the expression level of vascular endothelial growth factor (VEGF) in the primary tumor are correlated with the degree of lymph node metastasis (N-stage), tumor staging (T) and survival time in LSCC patients.
Methods
Tissue-Microarrays of 97 LSCC patients were analyzed using immunohistochemistry. The expression of VEGF was scored as intensity of staining (low vs high) and the number of CD31-positive vessels (median </≥7 vessels per visual field) was counted manually. Scores were correlated with N-stage, T-stage and 5-year overall survival rate.
Results
A high expression of angiogenic biomarkers was not associated with poor overall survival in the overall cohort of patients. Instead high CD31 count was associated with early stage cancer (p = 0.004) and in this subgroup high VEGF expression correlated with poor survival (p = 0.032). Additionally, in early stage cancer a high vessel count was associated with an increased recurrence rate (p = 0.004).
Conclusion
Only in the early stage subgroup a high expression of angiogenic biomarkers was associated with reduced survival and an increased rate of recurrence. Thus, biomarkers of angiogenesis may be useful to identify high risk patients specifically in early stage LSCC.
Similar content being viewed by others
Background
Head and neck carcinomas with lymphatic metastasis usually require radical therapeutic management and are associated with poor prognosis. This is particularly true for squamous cell carcinoma of the larynx (LSCC). In addition, patients with lymph node (LN) involvement have a worse prognosis compared to patients without LN metastasis [1]. The identification of early stage LSCC patients at high risk therefore could help improving prognosis and treatment selection and preventing recurrence [2, 3]. Although clinically of high importance, the mechanisms which drive metastasis to the lymph nodes in LSCC are still largely unknown. It has been suggested that a pro-angiogenic tumor microenvironment may promote lymphatic metastasis [4,5,6]. The presence of neovascularization around neoplastic tissue is a typical finding in many solid tumors. Angiogenesis seems to be an important biological parameter implicated in tumor growth, metastasis and progression [4, 5]. However, in LSCC controversial data with respect to the impact of angiogenesis on metastasis have been reported. Some studies suggested angiogenesis as a precursor for regional lymph node metastasis [6] and implicated microvessel density in local tumor progression [7]. In contrast, other studies did not show any prognostic relation between angiogenesis and prognosis, especially in patients with LSCC [8,9,10,11].
Well defined markers of angiogenesis are CD31 and vascular endothelial growth factor (VEGF). CD31 is highly expressed on the surface of endothelial cells and well established for the monitoring of vessel density in malignant tissue. It is a member of the Immunoglobulin-superfamily PECAM-1 [12] and it was reported that CD31 is involved in angiogenesis for example in early breast cancer [13]. CD31 was even used as a prognostic marker for nasopharyngeal cancer [14]. Sion-Vaardy et al. found a significantly increased number of vessels in head and neck tumors with deeper invasion [15]. Kyzas et al., however, have questioned the role of CD31 for the prognosis of LSCC in their study on 69 patients with LSCC and oral cancer. They rather suggested that the expression of VEGF might have prognostic significance in these patients [16].
VEGF is an important growth factor and signaling molecule involved in vasculogenesis and angiogenesis [17]. VEGF was reported to influence the pathogenesis of LSCC as a parameter of angiogenesis [16, 18,19,20,21]. In addition, a gene polymorphism of VEGF was suspected to be a risk factor for LSCC [22]. Chen et al. found as well that VEGF influenced the pathogenesis of head and neck cancer and supposed an important role of VEGF as a serological biomarker [23]. In contrast, Burian et al. were not able to demonstrate a relevant impact of elevated VEGF in the prognostic relevance of LSCC [8].
The controversial results regarding the role of these angiogenic factors may be due to the heterogeneity of the patient cohorts with regard to early or late stage disease. The aim of this study therefore was to investigate a possible relation between markers of angiogenesis, N-stage, T-stage, overall survival and recurrence rates in a cohort of 97 patients with LSCC with a special emphasis on tumor stage.
Methods
Study population and ethics approval
Patients with LSCC treated in the Department of Otorhinolaryngology, Head and Neck Surgery at the University Hospital Essen between 1995 and 2004 were included in this study. Samples of tumor tissue were collected during diagnostic biopsies or tumor resection and were stored for later analysis. Preparation of tissue and immunohistochemistry were performed between March 2014 and December 2014. Patient characteristics and data on survival were retrospectively assessed by extracting the corresponding data from the patient medical charts. Analysis of experimental data was performed in a completely anonymous fashion. The study was approved by the local ethics committee of the Medical Faculty of the University Duisburg-Essen (12–5192-BO) and was performed according to Declaration of Helsinki. Based on the retrospective and anonymous character of the study the approval contained a waiver for written informed consent. Tumor staging was performed according to the criteria of the Tumor-Node-Metastasis staging system, first reported by Pierre Denoix in the 1940’s and adapted and compiled by the International Union against Cancer (UICC) [24]. Treatment regimens were planned according to tumor stage, surgical possibilities and patients´ decision. Patients with low T stage (T1 and T2) underwent mostly surgical therapy (70%). For patients with high T-stage (T3 + T4) surgery followed by RTX was chosen in the majority of cases (66%); more details on the treatment regimens are listed in Table 1.
Recurrence was defined as local relapse or cervical lymph node metastasis within 5 years after diagnosis. Overall recurrence rate was 27% (16 out of 59 patients from whom recurrence data were available, Table 1).
Preparation of tissue microarrays and immunohistochemistry
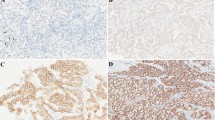
For preparation of tissue microarrays whole slides were inspected by a trained pathologist and regions of interest containing malignant tissue areas were marked. The tissue cores of 3 mm thickness were extracted from formalin-fixed/paraffin-embedded tumor tissue blocks using a skin biopsy punch (PFM, Cologne, Germany) and cut into 5 μm sections. Subsequently, the cores were de-parafinised and the antigens were retrieved by HIAR (heat-induced antigen retrieval) in citrate buffer pH 6.0 (Sigma–Aldrich, Taufkirchen, Germany). Samples were incubated with the primary antibodies (monoclonal mouse anti-human CD31, eBioscience, San Diego, USA and polyclonal rabbit anti-human VEGF, Millipore, Schwalbach, Germany) at 4 °C overnight. Then samples were incubated with peroxidase-coupled secondary antibodies for 30 min at room temperature and developed with AEC solution (Invitrogen, Karlsruhe, Germany) for 10 min. Nuclei were stained with haematoxylin (Carl Roth, Karlsruhe, Germany) for 1 min. Samples were covered with Kaisers glycerin gelatin (Merck, Darmstadt, Germany) and analyzed with a Zeiss Axioscope 2 microscope (Zeiss, Jena, Germany) at 200-fold magnification. Three trained scientists independently performed blinded scoring. VEGF expression was scored as intensity of the staining reaction in the samples and the immune reactive score (IRS) was calculated as mean IRS score of the three independent observers. VEGF was scored as negative, weak, medium and strong and subsequently categorized into low and high expression grade (Fig. 1a). Absolute numbers of CD31-positive vessels were quantified in four visual microscopic fields per sample and were expressed as mean per sample (Fig. 1b and c). Scores were correlated with N-stage, T-stage, recurrence and 5-year overall survival rate.
Immunohistochemical staining and analysis. Immunohistochemical staining of VEGF (a) and CD31 (b) was evaluated. The immune reactive score (IRS) of VEGF was calculated as intensity of the staining reaction, evaluated by three independent observers. VEGF was scored as absent (−), weak (+), medium (++), and strong (+++) (Magnification = 200×) and categorized in low and high. Low includes −/+ and high includes ++/+++. CD31 was scored by absolute vessel counting per visual field (b). The median of the counted CD31-positive vessels was 7.3 per visual field (c) and was used as a cut-off to categorize patients into low (< 7) vs high (≥7)
Statistical analysis
Statistical analyses were performed using SPSS© (Statistical Package for the Social Sciences, IBM©) statistical software version 20.0. The level of significance was set to p < 0.05. All P-values were based on two sided tests. The 5-years-survival curves were plotted according to the Kaplan–Meier method. Significance was tested using the log-rank test. Kruskal-Wallis-test and Mann-Whitney-U test were used to correlate clinical-pathological parameters such as T- and N-stage, respectively, with the number of CD31-positive vessels and VEGF expression. Chi square test was performed to analyze recurrence rates and CD31/VEGF expression in patients with early stage LSCC.
Results
Patient cohort
Ninety-seven patients were included in the study and for all patients complete clinical and immunohistochemical data was available. Patients were predominantly male (89%) and tumor stage equally distributed from T1 to T4. VEGF staining was evaluable in 87/97 patients and CD31 data in 89/97 patients. Follow up data were available for 59 (out of 97 patients) in the overall cohort, 34 (out of 50) patients with low T-stage and 44 (out of 67) patients with negative N-stage. Patient demographics are described in Table 1.
Immunohistochemical scores for VEGF and CD31
VEGF was scored as described above and the number of CD31 positive intratumoral vessels per visual field was quantified and ranged between 0 and 30 (example shown in Fig. 1a+b). Patients were divided into two groups according to the median of CD31-positive vessels, which was calculated as 7.3 (fig. 1c). In subsequent analyses patients with low (< 7) vs high (≥7) vessel count were compared.
A high number of CD31-positive vessels correlates with low T-stage and negative N-stage
As expected, a positive N-stage significantly correlated with high T-stage in our cohort (p = 0.001; Fig. 2a). Interestingly, a high number of CD31-positive vessels was significantly associated with lower T-stage (T1 + T2) (p = 0.004; Fig. 2b). In addition, the number of CD31-positive vessels also correlated with N-stage. Interestingly, a high vessel count was rather associated with the absence of lymph node metastasis (N0 status) and not with N+ status (Fig. 2c, p = 0.028). These data show that low stage LSCC is characterized by high vessel density. VEGF staining intensity was not significantly associated with T- or N-stage (data not shown).
Vessel density is increased in early stage LSCC. T-stage was determined in LSCC patients (n = 97). The number of patients without (N0) or with lymph node metastasis (N+) was determined for each T-stage. High T-stage correlated with positive node status (Kruskal-Wallis test; p = 0.001) (a). The absolute number of vessels per microscopic visual field was determined by immunohistochemistry and correlated with tumor T-stage (b) and N-stage (c). A high vessel count correlated with low T-stage (Kruskal-Wallis test; p = 0.004) and the absence of lymph node metastasis (Mann-Whitney-U test; p = 0.028). Data are depicted as box-plots indicating mean and absolute numbers of CD31 positive vessels and error bars
Prognostic relevance of angiogenic biomarkers
The potential prognostic value of the two biomarkers in the total cohort of LSCC patients was tested. However, neither vessel density nor VEGF expression were associated with overall survival in the total cohort (data not shown). Based on these results a potential correlation of VEGF and CD31 with overall survival was assessed separately in patients with early (T1 and T2, N0) and late (T3 and T4, N+) stage LSCC using Kaplan-Meier analysis. Strong VEGF expression was associated with poor survival in N0 patients, although not reaching statistical significance (p = 0.116; Fig. 3a). No association was found in patients with positive N-stage (p = 0.927, not shown). Strong VEGF expression also correlated with poor survival in patients with low T-stage (T1 and T2; p = 0.032; Fig. 3a). Again no correlation was found in patients with high T-stage (T3 and T4; p = 0.846; not shown). Thus, strong VEGF expression was associated with poor survival in early stage but not in late stage LSCC. In contrast, CD31 vessel count was not associated with overall survival in this LSCC cohort, neither in patients with early nor late stage disease (data not shown). Finally, we analyzed a potential link between CD31/VEGF and recurrence-free survival. No correlation was found between the VEGF score and the number of recurrences in early stage LSCC within the 5-year follow-up period. In contrast, our analyses revealed a potential link between vessel count and recurrence rate. As shown in fig. 4a patients with low T-stage and a low number of CD31-positive vessels had a tendency for better recurrence free survival compared to patients with low T-stage and high CD31-positive vessel number, although not reaching statistical significance (Fig. 4a, p= 0.098). Low CD31 vessel count significantly correlated with reduced recurrence rate in patients with negative N-stage (p = 0.004) (Fig. 4b).
Reduced expression of VEGF correlates with improved survival in early stage LSCC. Patients with negative N-stage (n = 67) (a) and low T-stage (T1 + T2, n = 50) (b) were grouped into either VEGF high or VEGF low and further examined in terms of their survival. Kaplan Meier analysis of survival and log rank test were performed
High vessel count is associated with an increased recurrence rate in early stage LSCC. Chi-square-Test was applied to comparerelapse rates and vessel count in patients with (a) low T-stage or (b) negative N-stage. Patients with a high number of CD31-positive vessels early stage LSCC had a significantly higher relapse rate compared to patients with early LSCC and low number of CD 31-positive vessels. a Patients were grouped according to T-stage and vessel count. Number of patients with relapse within 5 years is indicated. Chi-square test; p = 0.098. b Patients were grouped according to N-stage and vessel count. Number of patients with relapse within 5 years is indicated. Chi-square test; p = 0.004
Collectively, these data show that low expression of angiogenic biomarkers seems to be associated with improved clinical outcome in early stage, but not in advanced LSCC.
Discussion
A potential role for angiogenesis in the prognosis of cancer has been demonstrated in previous studies for different cancer types [5, 25,26,27,28,29,30,31,32]. It was the aim of this study to provide new information about the relation between angiogenesis, tumor stage and prognosis of LSCC.
Angiogenic biomarkers are particularly associated with early tumor stages
In non-laryngeal HNSCC, studies by Gleich et al. reported an association of angiogenesis with increasing T and N stage in oropharyngeal cancer (OPC) (higher T-stages here defined as T2-T4) [30], but there was no statistical correlation between tumor aggressiveness and tumor angiogenesis in low T stages (here defined as T1) [33]. For LSCC, the literature provides controversial information whether angiogenesis is an early event in LSCC development or whether it is associated with increased tumor stages [24, 29, 34]. Some studies did not show any relation between angiogenesis and prognosis, especially in patients with LSCC [8,9,10,11]. In our study we demonstrated a significant correlation of CD31-positive vessels with early T-stages and the absence of LN metastasis (N0 status). There is a controversy in the literature regarding a direct relation between tumor stage and VEGF, another potential marker of angiogenesis. Some studies did not show any association [35] while others revealed significant correlations especially between N-stage and VEGF [27, 36,37,38]. Interestingly, Wang et al. even reported a strong association of VEGF expression with lymph node metastasis in primary laryngeal carcinomas [27]. In contrast, other studies did not reveal any association of angiogenesis with the presence of LN metastasis [25, 28]. In our analysis there was no direct correlation between T- or N-stage and VEGF.
Angiogenic biomarkers and their influence on prognosis
As mentioned above the VEGF expression of patients with LSCC is not directly related to T- or N-stage when analyzing the entire cohort. We noted, however, that patients with initial negative N-stage and low T-stage who have a strong VEGF expression showed reduced overall survival. This is in line with findings by Krecicki et al. who reported that a pro-angiogenic tumor microenvironment may promote lymphatic metastasis [6] and consecutively shorter survival. They identified vessel endothelial cells with antibodies against factor VIII and analyzed the vessel density (VD) per image in 55 patients with laryngeal cancer. In their study VD correlated with the existence of nodal metastases (P = 0.02) in contrast to histological grading of the tumor or the T-stage. The authors hypothesized that angiogenesis in laryngeal cancer may be of some value in predicting N-stage. In another study, Kupisz et al. found a direct correlation between increased tumor angiogenesis and increased T-stage, histologic grade and a shorter survival rate [25]. Teknos et al. reported that highly-vascularized tumors were associated with worse survival [26]. Williams et al. detected a higher regional recurrence rate in tumors with high angiogenesis and used it as an independent prognostic indicator [39]. Pignataro et al. as well showed that patients with poorly vascularized tumors had a tendency for better prognosis. Similar to our study, no relation between microvessel density and clinical pathological features or prognosis in the later tumor stages was found. The authors suggested that angiogenesis might be an early event in laryngeal tumorigenesis [29]. In our study positive N-stage was not associated with high expression of angiogenic biomarkers in the primary tumor lesion suggesting that that these events are not directly spatiotemporally linked. Instead we found a potential link between angiogenesis and shorter survival exclusively in patients with early stage LSCC. A possible explanation for our findings would be that early stage tumors, which are highly angiogenic prepare the tumor for metastasis. However, these metastasis become clinically detectable at far later time points, when the microenvironment of the primary tumor is no longer characterized by highly expressed angiogenic biomarkers.
In patients with early tumor stage, we also investigated the recurrence rate and found that early recurrence was associated with a higher number of CD31-positive vessels, indicative of a pro-angiogenic microenvironment. Similarly, Bolzoni Villaret et al. analyzed angiogenesis and lymphangiogenesis using immunohistochemistry with antibodies against CD31 and podoplanin. Twenty seven patients with poor outcome were identified and compared with a selected sample of 28 patients. Based on analysis of these groups they concluded that patients with early T-stages of laryngeal cancer showing a pro-angiogenic microenvironment had a significantly higher rate of relapse [2]. Using semiquantitative scoring analysis Murray et al. [40] reported that angiogenesis (CD31 IHC) might be a significant predictor for relapse in patients with negative N-stage. In our study we can substantiate these findings using a large cohort of LSSC patients and exact absolute counting of vessels.
Relevance of presence of angiogenic biomarkers in early tumor stages in prognosis
In summary in this study we identified VEGF and CD31 as prognostic factors for the clinical outcome of patients with early stage laryngeal cancer. In particular, we demonstrated a significant correlation of CD31-positive vessels with early T-stages and the absence of LN metastasis (N0 status), respectively, but higher relapse rate and we identified strong VEGF expression as a marker of poor survival in patients with a low T-stage and a negative N-stage. Based on these data one could hypothesize that angiogenesis is of special clinical relevance at non-metastatic early tumor stages and determines later tumor progression already at this stage. Based on the data presented in this study we postulate that the quantification of high VEGF and CD31 in early tumor stages could be a useful tool to identify patients with poor prognosis at early tumor and lymph node stages. This could help to improve the clinical management of these patients. As several anti-angiogenic drugs have been developed in the past years [41] these drugs can be considered as additional therapeutic options in high risk LSCC patients with highly angiogenic cancers. Along this line, Beatrice et al. suggested to perform a special anti-angiogenic RCTX in patients with high capillary count even in case of surgical R0 resection. Our results further underscore the hypothesis that a pro-angiogenic microenvironment in early, non-metastatic stages might prepare the tumor for recurrence. Furthermore it indicates that high vessel densities, as well as strong VEGF expression, are characteristic for smaller tumors and might precede the development of metastasis at later stages. These findings would argue in favor of a more radical treatment of a small subgroup of patients with a highly angiogenic tumor microenvironment. However, further studies, ideally in a prospective design, should be performed to substantiate these findings.
Conclusion
Patients with low T-stage and negative N-stage are generally known to have a good five-year survival rate. However, our study identified a subgroup of patients with strong VEGF expression and high CD31-positive vessel number, which was linked to poor prognosis and increased risk for relapse. Thus, our study provides further evidence that quantification of angiogenesis in a subgroup of patients with laryngeal cancer could help to predict patient outcome and to better guide therapeutic decisions in this cancer entity.
Abbreviations
- IRS:
-
Immune Reactive Score
- LN:
-
Lymph Node
- LSCC:
-
laryngeal squamous cell carcinoma
- VEGF:
-
vascular endothelial growth factor
References
Boffeta P, Merletti F, Faggiano F, Migliaretti G, Ferro G, Zanetti R, Terracini B. Prognostic factors and survival of laryngeal cancer patients from Turin, Italy. A population-based study. Am J Epidemiol. 1997;145:1100–5.
Bolzoni Villaret A, Barbieri D, Peretti G, et al. Angiogenesis and lymphangiogenesis in early-stage laryngeal carcinoma: prognostic implications. Head Neck. 2013;35:1132–7.
Lionello M, Staffieri A, Marioni G. Potential prognostic and therapeutic role for angiogenesis markers in laryngeal carcinoma. Acta Otolaryngol. 2012;132:574–82.
Beatrice F, Cammarota R, Giordano C, et al. Angiogenesis: prognostic significance in laryngeal cancer. Anticancer Res. 1998;18:4737–40.
Liotta LA, Steeg PS, Stetler-Stevenson WG. Cancer metastasis and angiogenesis: an imbalance of positive and negative regulation. Cell. 1991;64:327–36.
Krecicki T, Dus D, Kozlak J, et al. Quantitative evaluation of angiogenesis in laryngeal cancer by digital image measurement of the vessel density. Auris Nasus Larynx. 2002;29:271–6.
Lentsch EJ, Goudy S, Sosnowski J, Major S, Bumpous JM. Microvessel density in head and neck squamous cell carcinoma primary tumors and its correlation with clinical staging parameters. Laryngoscope. 2006;116:397–400.
Burian M, Quint C, Neuchrist C. Angiogenic factors in laryngeal carcinomas: do they have prognostic relevance? Acta Otolaryngol. 1999;119:289–92.
Teppo H, Soini Y, Melkko J, Koivunen P, Alho O. Prognostic factors in laryngeal carcinoma: the role of apoptosis, p53, proliferation (Ki-67) and angiogenesis. APMIS. 2003;111:451–7.
Rodrigo JP, Cabanillas R, Chiara MD, Garcia Pedrero J, Astudillo A, Suarez Nieto C. Prognostic significance of angiogenesis in surgically treated supraglottic squamous cell carcinomas of the larynx. Acta Otorrinolaringol Esp. 2009;60:272–7.
Hagedorn HG, Nerlich AG. Microvessel density and endothelial basement membrane composition in laryngeal squamous cell carcinomas. Acta Otolaryngol. 2000;120:891–8.
Gumina RJ, Kirschbaum NE, Rao PN, vanTuinen P, Newman PJ. The human PECAM1 gene maps to 17q23. Genomics. 1996;34:229–32.
Jong JS. De, van Diest PJ, Baak JP. Heterogeneity and reproducibility of microvessel counts in breast cancer. Lab Investig. 1995;73:922–6.
Rubio L, Burgos JS, Morera C, Vera-Sempere FJ. Morphometric study of tumor angiogenesis as a new prognostic factor in nasopharyngeal carcinoma patients. Pathol Oncol Res. 2000;6:210–6.
Sion-Vardy N, Fliss DM, Prinsloo I, Shoham-Vardi I, Benharroch D. Neoangiogenesis in squamous cell carcinoma of the larynx - biological and prognostic associations. Pathol Res Pract. 2001;197:1–5.
Kyzas PA, Stefanou D, Batistatou A, Agnantis NJ. Prognostic significance of VEGF immunohistochemical expression and tumor angiogenesis in head and neck squamous cell carcinoma. J Cancer Res Clin Oncol. 2005;131:624–30.
Yla-Herttuala S, Rissanen TT, Vajanto I, Hartikainen J. Vascular endothelial growth factors: biology and current status of clinical applications in cardiovascular medicine. J Am Coll Cardiol. 2007;49:1015–26.
Sawatsubashi M, Yamada T, Fukushima N, Mizokami H, Tokunaga O, Shin T. Association of vascular endothelial growth factor and mast cells with angiogenesis in laryngeal squamous cell carcinoma. Virchows Arch. 2000;436:243–8.
Chen G, Liu Y, Wang J, et al. Expression of vascular endothelial growth factor and cyclooxygenase-2 in laryngeal squamous cell carcinoma and its significance. J Huazhong Univ Sci Technolog Med Sci. 2006;26:105–7.
Denhart BC, Guidi AJ, Tognazzi K, Dvorak HF, Brown LF. Vascular permeability factor/vascular endothelial growth factor and its receptors in oral and laryngeal squamous cell carcinoma and dysplasia. Lab Investig. 1997;77:659–64.
Neuchrist C, Quint C, Pammer A, Burian M. Vascular endothelial growth factor (VEGF) and microvessel density in squamous cell carcinomas of the larynx: an immunohistochemical study. Acta Otolaryngol. 1999;119:732–8.
Unal ZN, Unal M, Bagdatoglu OT, Polat G, Atik U. Genetic polymorphism of VEGF-1154 (a/G) in laryngeal squamous cell carcinoma. Arch Med Res. 2008;39:209–11.
Chen Z, Malhotra PS, Thomas GR, et al. Expression of proinflammatory and proangiogenic cytokines in patients with head and neck cancer. Clin Cancer Res. 1999;5:1369–79.
Bernier J. Head and neck Cancer: multimodality management. New York: Springer; 2011.
Kupisz K, Chibowski D, Klatka J, Klonowski S, Stepulak A. Tumor angiogenesis in patients with laryngeal cancer. Eur Arch Otorhinolaryngol. 1999;256:303–5.
Teknos TN, Cox C, Barrios MA, et al. Tumor angiogenesis as a predictive marker for organ preservation in patients with advanced laryngeal carcinoma. Laryngoscope. 2002;112:844–51.
Wang Z, Chen Y, Li X, et al. Expression of VEGF-C/VEGFR-3 in human laryngeal squamous cell carcinomas and its significance for lymphatic metastasis. Asian Pac J Cancer Prev. 2012;13:27–31.
Bonhin RG, Rocha VBC, De Carvalho GM, et al. Correlation between vascular endothelial growth factor expression and presence of lymph node metastasis in advanced squamous cell carcinoma of the larynx. Braz J Otorhinolaryngol. 2015;81:58–62.
Pignataro L, Carboni N, Midolo V, et al. Clinical relevance of microvessel density in laryngeal squamous cell carcinomas. Int J Cancer. 2001;92:666–70.
Gleich LL, Biddinger PW, Duperier FD, Gluckman JL. Tumor angiogenesis as a prognostic indicator in T2-T4 oral cavity squamous cell carcinoma: a clinical-pathologic correlation. Head Neck. 1997;19:276–80.
Chaudhury TK, Lerner MP, Nordquist RE. Angiogenesis by human melanoma and breast cancer cells. Cancer Lett. 1980;11:43–9.
Frank R, Saclarides TJ, Leurgans S, Speziale NJ, Drab EA, Rubin DB. Tumor angiogenesis as a predictor of recurrence and survival in patients with node-negative Colon Cancer. Ann Surg. 1995;222(6):695–9.
Gleich LL, Biddinger PW, Pavelic ZP, Gluckman JL. Tumor angiogenesis in T1 oral cavity squamous cell carcinoma: role in predicting tumor aggressiveness. Head Neck. 1996;18:343–6.
Laitakari J, Nayha V, Stenback F. Size, shape, structure, and direction of angiogenesis in laryngeal tumour development. J Clin Pathol. 2004;57:394–401.
Akdeniz O, Akduman D, Haksever M, Ozkarakas H, Muezzinoglu B. Relationships between clinical behavior of laryngeal squamous cell carcinomas and expression of VEGF, MMP-9 and E-cadherin. Asian Pac J Cancer Prev. 2013;14:5301–10.
Baek S, Jung K, Lee S, et al. Prognostic significance of vascular endothelial growth factor-C expression and lymphatic vessel density in supraglottic squamous cell carcinoma. Laryngoscope. 2009;119:1325–30.
Sullu Y, Gun S, Atmaca S, Karagoz F, Kandemir B. Poor prognostic clinicopathologic features correlate with VEGF expression but not with PTEN expression in squamous cell carcinoma of the larynx. Diagn Pathol. 2010;5:35.
Hinojar-Gutierrez A, Fernandez-Contreras M, Gonzalez-Gonzalez R, et al. Intratumoral lymphatic vessels and VEGF-C expression are predictive factors of lymph node relapse in T1-T4 N0 laryngopharyngeal squamous cell carcinoma. Ann Surg Oncol. 2007;14:248–57.
Williams JK, Carlson GW, Cohen C, DeRose PB, Hunter S, Jurkiewicz MJ. Tumor angiogenesis as a prognostic factor in oral cavity tumors. Am J Surg. 1994;168:373–80.
Murray JD, Carlson GW, McLaughlin K, et al. Tumor angiogenesis as a prognostic factor in laryngeal cancer. Am J Surg. 1997;174:523–6.
Rajeev S, Shevde LA. Recent advances in anti-Angiogenic therapy of Cancer. Oncotarget. 2011;2(3):122–34.
Acknowledgements
The authors wish to thank Petra Altenhoff (Department of Otorhinolaryngology, University Hospital Essen) for excellent technical support and Ulrike Krahn (University Hospital Essen, IMIBE = Institute of medical informatics, biometry and epidemiology) for support with the statistical analyses.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The funding body had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
Submission of a manuscript to a BioMed Central journal implies that materials described in the manuscript, including all relevant raw data, will be freely available to any scientist wishing to use them for non-commercial purposes, without breaching participant confidentiality. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. There is no conflict of interest.
Author information
Authors and Affiliations
Contributions
Conception and design: SB. Provision of study materials or patients: AB, SZ, ND, JA, MM, SL. Collection and assembly of data: AS, PW, OK, LH, PH, BH. Data analysis and interpretation: AS; IN, PW, SB. Manuscript writing: AS, PW, IN, BAS, SB. Final approval of manuscript: all authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the local ethics committee of the Medical Faculty of the University Duisburg-Essen (12–5192-BO) and was performed according to Declaration of Helsinki. Based on the retrospective and anonymous character of the study the approval contained a waiver for written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Schlüter, A., Weller, P., Kanaan, O. et al. CD31 and VEGF are prognostic biomarkers in early-stage, but not in late-stage, laryngeal squamous cell carcinoma. BMC Cancer 18, 272 (2018). https://doi.org/10.1186/s12885-018-4180-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-018-4180-5