Abstract
Background
Gene expression can be employed for the discovery of prognostic gene or multigene signatures cancer. In this study, we assessed the prognostic value of a 35-gene expression signature selected by pathway and machine learning based methods in adjuvant therapy-linked glioblastoma multiforme (GBM) patients from the Cancer Genome Atlas.
Methods
Genes with high expression variance was subjected to pathway enrichment analysis and those having roles in chemoradioresistance pathways were used in expression-based feature selection. A modified Support Vector Machine Recursive Feature Elimination algorithm was employed to select a subset of these genes that discriminated between rapidly-progressing and slowly-progressing patients.
Results
Survival analysis on TCGA samples not used in feature selection and samples from four GBM subclasses, as well as from an entirely independent study, showed that the 35-gene signature discriminated between the survival groups in all cases (p<0.05) and could accurately predict survival irrespective of the subtype. In a multivariate analysis, the signature predicted progression-free and overall survival independently of other factors considered.
Conclusion
We propose that the performance of the signature makes it an attractive candidate for further studies to assess its utility as a clinical prognostic and predictive biomarker in GBM patients. Additionally, the signature genes may also be useful therapeutic targets to improve both progression-free and overall survival in GBM patients.
Similar content being viewed by others
Background
Glioblastoma multiforme (GBM) is the most common and highly aggressive brain tumour. Patients with GBM have very poor prognosis, with the median OS time of 14.5 months [1]. Chemotherapy and radiotherapies are intended to improve patient survival, but are, however, hampered by development of resistance. Methylation of the promoter of the MGMT gene, which encodes O-6-methylguanine-DNA methyl-transferase, a DNA-repair enzyme that removes alkylating groups at the O6 of guanine residues, is a predictor of treatment response in GBM. Most studies that considered progression-free survival assessed only the prognostic value of MGMT promoter methylation [2–4]. Tumours with hypermethylated MGMT promoters are expected to benefit from temozolomide, an alkylating agent used for treating GBM, but reports regarding the prognostic value of this biomarker have been conflicting [5, 6].
Several gene expression prognostic and predictive signatures have been translated into clinical applications for cancer treatment. Oncotype DX is a 21-gene qRT-PCR assay used to predict likelihood of recurrence in women with estrogen receptor positive breast cancer [7, 8]. Mammostrat is prognostic immunohistochemical test that uses antibodies specific for SLC7A5, p53, HTF9C, NDRG1, and CEACAM5 to classify ER-positive, lymph node negative breast cancer cases into low-, moderate- or high-risk groups [9, 10]. Mammaprint is a 70-gene microarray-based test for predicting risk of metastasis in breast cancer [11].
In light of the lack of standardised prognostic biomarkers for GBM, we aimed to identify a mRNA expression derived prognostic signature using data from the Cancer Genome Atlas (TCGA - http://cancergenome.nih.gov/). As current prognostic feature selection approaches lack reproducibility and do not take chemoradioresistant pathways into consideration, we used a combination of pathway enrichment analysis and Support Vector Machine based Recursive Feature Elimination (SVM-RFE) to ensure that the genes selected as having predictive potential would also be biologically relevant to the phenoptype. We here describe a multigene signature that successfully predicts both progression-free and overall survival in glioblastoma multiforme.
Methods
Gene-centric expression data
Five hundred fifty eight GBM gene expression profiles generated by the Cancer Genome Atlas (TCGA) were downloaded from the NCI Genomic Data Commons Data Portal (https://portal.gdc.cancer.gov/projects/TCGA-GBM). Five hundred forty eight of the these profiles were obtained from GBM patients, and ten were from non-neoplastic patients. One profile was selected for each of the samples profiled two or more times. Five hundred twenty nine profiles left after removing those of non-neoplastic samples were used in this study (Additional file 1). The expression were profiled on Affymetrix HT HG-U133A platform. As gene expression of the TCGA samples was profiled in batches which could introduce bias in classification analysis [12], the statistical significance of batch effect was assessed as a function of the selected genes using guided Principal Component Analysis (gPCA) from the R package gPCA [13]. The approach used by TCGA (2008) [14] and Verhaak et al. (2011) [15] was employed to generate gene-centric expression data. The probe sequences of HT HG-U133A downloaded from Affymetrix were mapped against a database composed of RefSeq version 41 and GenBank 178 complete coding sequences using SpliceMiner [16]. Only perfect matches were considered and probes mapping to more than one gene were excluded. The output file from SpliceMiner and the HT HG-U133A chip definition file (cdf) were passed to the alternate cdf-generating function makealtcdf of AffyProbeMiner [17]. Probe sets with less than five probes were excluded from the resulting alternative cdf, which was then converted to an R package using makecdfenv. The cdf was used to perform Robust Multi-array Average normalization and summarization of the gene expression data, resulting in gene-centric data for 12161 genes.
An independent validation data set (GSE7696) profiled on HG-U133 Plus 2 Affymetrix platform and downloaded from the NCBI Gene Expression Omnibus (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE7696) was equivalently treated. This data set contained gene expression data for 80 GBM and four non-neoplastic samples, and was chosen because of the availability of patients’ treatment information.
Sample selection
To ensure that treatment did not introduce confounding effects, samples from patients that received adjuvant chemotherapy and radiation and had uncensored days to death or progression were selected. Figure 1 shows sample selection for the identification of genes with prognostic value. Four hundred fifteen patients received the standard GBM treatment. Semantically, tumour progression is a radiologically documented increase in tumour size after a subtotal surgical excision [18]. The time for this to occur is known as time to progression, which is the same as uncensored progression-free survival (PFS) [19]. Two hundred one patients had associated uncensored progression-free survival (PFS) times, and 380 had overall survival OS times (censored or uncensored).
Clinical data for all the patients used in this study were obtained from TCGA. PFS times for patients who experienced tumour progression within the follow-up period were obtained from the TCGA file for new tumour events. The GBM subtypes of samples used in our study were obtained from the supplementary clinical file provided by Brennan et al., (2013) [20].
There is no standard for classifying patients as rapid and slow GBM progressors after standard treatment. While the median PFS after treatment could be used as a separation point, it does not provide a ’buffer zone’ to filter out borderline samples close to the median that may fall in the incorrect group due to unknown confounding factors. Rather than defining an arbitrary exclusion range, we used the first (Q1) and third (Q3) quartiles, 120 and 341 days respectively, as boundaries to divide patients into three classes, since they are still dependent on the median and not influenced by extreme outliers. Class 1 contained 48 patients having PFS times between 6 and 120 days (rapidly-progressing) and class 2 contained 35 patients having PFS times between 358 and 720 days (slow progressing). Classes 1 and 2 were used in feature selection and the 118 remaining samples (Class 3) that fell within the inter-quartile range were used in PFS and OS analysis.
Selection of genes discriminating between rapidly and slowly progressing GBM patients
In this present study, genes in the cancer-related pathways were considered in our feature selection because of their known roles in chemoradiation resistance, and to reduce the likelihood of selecting genes related to survival by chance. Studies have identified pathways and processes that drive resistance to chemotherapy and radiotherapy in cancer. Several of these genes are found in known cancer pathways [21–28]. Several genes in the NF- κB and PI3K/Akt signaling pathways are associated with chemoresistance development in cancer [29, 30]. Also, genes involved in drug inactivation and efflux, DNA repair, and epithelial-mesenchymal transition have been shown to enhance drug resistance mechanisms [26, 31]. Pathway enrichment analysis was performed on the genes with high expression variance (median absolute deviation ≥ 0.5) across the 529 samples using the Set Analyser web service provided by the Comparative Toxicogenomics Database [32]. Genes were selected from the pathway categories related to cancer signaling pathways, reactive oxygen species metabolism, DNA repair, and drug transport and metabolism. A set of genes that discriminated between the rapidly-progressing and slowly-progressing groups were selected using a modified Support Vector Machine-Recursive Feature Elimination (SVM-RFE). SVM-RFE, proposed by [33], was modified by introducing 5-fold cross-validation into the SVM classifier step and capturing the error rate generated at this step (the figure showing the workflow for SVM-RFE is attached as Additional file 2).
Survival analysis
The 118 Class 3 patients not used in the feature selection step were used to calculate regression coefficients (β) for the selected genes using univariate Cox proportional hazards analysis. The β’s were computed for the genes using coxph from the R survival package. Prognostic index, PI, was then calculated for each of the patients who received adjuvant chemotherapy and radiation and had PFS and/or OS data using the equation
where β g and gene g are the regression coefficient and the gene expression value for gene g, respectively. Patients in Class 3 were classified into low-risk and high-risk groups by choosing a value between the highest and lowest PI that ensured proper patients distribution based on PI. Patients with PI scores greater or equal than the chosen value were assigned to the high-risk group, whereas those with PI scores less than the value were assigned to the low-risk group. 380 patients with OS times were also classified into low-risk and high-risk groups in the same way.
Assessment of signature prognostic value in GBM subtypes
Verhaak et al. (2010) [15] identified four subtypes of GBM, namely proneural, neural, classical and mesenchymal, using gene expression data from 200 GBM samples. Brennan et al. (2013) [20] assigned additional 342 TGCA samples into the four subtypes using single-sample gene set enrichment analysis. A summarised clinical file provided by the authors was used in our study to assign patients to GBM subtypes. 95, 60, 105 and 120 of the 380 patients with available OS times were assigned to proneural, neural, classical and mesenchymal subtypes, respectively. 51, 33, 51 and 66 of the 201 patient group having associated PFS times were assigned to proneural, neural, classical and mesenchymal subtypes, respectively. We further categorised patients in each subtype into low-risk and high-risk groups.
Assessment of signature prognostic value in an independent dataset
The prognostic value of the selected gene signature was validated with the data from patients in the Murat et al. [34] validation dataset who had primary tumours and received adjuvant chemo- and radiotherapy. PI was calculated for the patients using the β’s obtained from the TCGA training set and the expression values of the selected genes in the samples from the patients. They were classified into low-risk and high-risk groups in such a manner as to ensure proper patient distribution between the two groups. Survival of the low-risk and high-risk groups were determined for both the TCGA and validation cohorts using the Kaplan-Meier method. Differences in survival between the risk groups were estimated statistically by log rank test. Survival differences between groups was said to be statistically significant if p<0.05. Hazard ratios (HR) between risk groups were determined by Cox proportional hazards regression model.
Mutivariate survival analysis to assess independent prognostic value
A multivariate Cox survival model was built using three variables: our prognostic index, MGMT promoter methylation, and age. Ages of patients at diagnosis were obtained from the clinical file provided by TCGA. MGMT promoter methylation status data were obtained from the clinical file provided by Brennan et al. [20] The univariate Cox analysis was first carried out on each variable followed by multivariate Cox analysis on all the variables. The coxph function in the R survival package was used for the analysis. Using the median PI value, the patients were assigned into low-risk or high-risk groups. Those with PI values lower than the median were assigned to low-risk groups, and those with PI to high-risk groups. The low-risk and the MGMT methylated promoter groups were used as references for prognostic index and MGMT promoter methylation status, respectively. Correlation of variables with PFS and OS was considered statistically significant at p(Wald)<0.05.
Identifying functional interactions between signature genes
We used the STRING database of known and predicted protein-protein interactions (https://string-db.org/) [35] to construct an interaction network for the signature genes and to perform KEGG pathway enrichment analysis on the derived subnetwork.
Results and discussion
In this present study, pathway-based and modified SVM-RFE-based methods were used to select a set of genes that discriminated between rapidly- and slowly-progressing GBM patients and combined into a signature. The prognostic value of the signature in predicting PFS and OS was accessed in the risk groups of GBM patients and validated on data set from an independent study. The independence of the signature in predicting PFS and OS was assessed by a multivariate Cox’s proportional hazards analysis. Studies on the identification of protein-coding multigene prognostic signatures in GBM focused on OS [7–9]. Overall survival (OS) is dependent on other factors besides gene expression. Progression-free survival, on the other hand, is expected to be a function of the expression of certain key genes. Genes whose expression across a cohort of patients correlated with OS were selected for survival analysis in these previous studies. This method has be shown to produce inconsistent signature genes in different data sets [36, 37].
genes discriminate between rapidly- and slowly-progressing GBM patients
GBM is a highly aggressive brain tumour, and the median survival of patients with GBM is 14.6 months [38]. We hypothesized that the tumour’s pre-treatment expression of genes in pathways associated with chemoradioresistance in cancer would be predictive of how rapidly a GBM patient would experience progression after standard treatment. Signaling pathways (MAPK, JAK/STAT, WNT, NOTCH, Hedgehog, PIK3/AKT), cell cycle, drug transporters, reactive oxygen species metabolism and DNA repair system are known to be involved in chemoradioresistance in cancer [29, 39–41]. We also reasoned that PFS times were more appropriate than OS times in grouping patients. PFS times were expected to be more closely related to expression of key genes, while other factors including age and treatment after disease progression are also associated with OS.
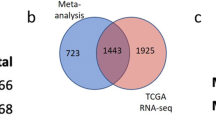
Pathway enrichment analysis was performed on 3899 genes (Additional file 2) that had varied expression (MAD≥0.5) across 529 GBM samples. 18 of the 159 gene sets from the enrichment analysis were annotated for the known chemoradioresistance-associated pathways (Table 1). Assessment of batch effect in TGCA expression data set from 529 GBM samples as a function of the 356 genes extracted from the pathways (Additional file 3) showed that the data set did not have significant batch effect (p=0.118). Inspection of the unguided principal component analysis plot of the first two principal components also showed that no batch effect was present (Additional file 4). The extracted genes were used in gene selection by the modified SVM-RFE. Our modified SVM-RFE was used to identify genes that discriminated between 48 rapidly-progressing patients (between 6 and 120 days PFS) and 35 slowly-progressing patients (between 358 and 720 days PFS). Figure 2 shows the plot of 5-fold cross-validation error rate against number of genes at each recursive step, starting with the 356 genes extracted from the pathways. The CV error rate decreased with decreasing number of genes until it reached 35 genes, which discriminated between rapidly- and slowly-progressing GBM patients at 100% accuracy. Further decreases in the number of genes resulted in increasing error rate.
The PFS times and expression levels of selected genes in the 118 Class 3 patients were used in multivariate Cox regression analysis to compute β’s for the genes. Table 2 shows the β’s calculated for the 35 selected genes. PI scores were calculated for all patients who received adjuvant chemotherapy and radiation (380) by substituting β’s and expression levels of selected genes into the prognostic index formula. The scores were then used to classify samples into low- and high-risk groups in survival analysis.
All the seed pathways in Table 1 except mismatch repair had at least one representative in the signature. Cell cycle had the highest number of genes (eight), followed by WNT pathway, which had five. The expression of four of the selected genes were significantly correlated with PFS (p<0.05): DKK1, FZD7, and PPARGC1A showed positive correlation (β>0), and CCNE1 displayed negative correlation (β<0) (Table 2).
Several signature genes are linked to survival in other cancers
Several genes in the signature have been reported to be associated with progression-free and/or overall survival in other cancers. DKK1, FZD3, FZD7, SFRP1, and SFRP4 are regulators of the Wnt/ β pathway. Overexpression of DKK1 is predictive of unfavourable overall survival and time to recurrence in intrahepatic cholangiocarcinoma patients [42]. Overexpression of FZD3 in colorectal patients was correlated with poor survival [43]. Underexpression of SFRP1 is associated with poor survival and may be an independent predictive and prognostic factor for prostate cancer [44]. SFRP4 increased the sensitivity of ovarian cancer cell lines to cisplatin, suggesting it is a predictive marker of chemoresistance in the cancer [45]. CCNA1, CCND1, CCNE1, CDC6, CDK2, CDKN1C and CDKN2A regulate the cell cycle. CCND1 amplication was associated with poor prognosis in estrogen receptor positive breast cancer [46] and [47] found it to be an independent prognostic factor in primary tumours and metastases as well as an independent prognostic factor in metastasis. CDC6 expression was correlated with overall and recurrence survival in non-small cell lung cancer patients [48]. CDKN2A promoter methylation was correlated with poor prognosis of colorectal cancer patients [49, 50]. CDK2, regulated by CDKN2A, is a known oncogene and regulator of the cell cycle. Its regression coefficient (β<0) in our study, however, showed that it was positively associated with progression-free survival. Its overexpression was associated with shorter survival in oral cancer [51]. GADD45G is implicated in stress signaling responses to physiological or environmental stressors, resulting in cell cycle arrest, DNA repair, cell survival and senescence, or apoptosis [52, 53]. GADD45G methylation and protein expression were independently associated with survival of gastric cardia adenocarcinoma patients [54] and esophageal squamous cell carcinoma patients [55].
The 35-gene signature predicts progression-free and overall survival in both TCGA and independent dataset
The 35 genes that discriminated between rapidly- and slowly-progressing patients were combined into a signature and its prognostic value first assessed in the patients that were not used in the feature selection step (Class 3). The prognostic index (PI) scores of these patients were standardized and used to split the patients into low- and high-risk groups. Figures 3a and 3b show the PFS and OS Kaplan Meier plots, respectively, for the two prognostic groups. The median PFS and OS times for the low-risk group (256 days, 95% CI = 232 - 299 days and 635 days, 95% CI = 502 - 1024 days) were significantly higher than those of the high-risk group (175 days, 95% CI = 158 - 204 days and 393 days, 95% CI = 345 - 454 days) (p<0.05).
Kaplan-Meier plots for low-risk and high-risk groups of GBM patients that received adjuvant chemotherapy and radiotherapy. The patients were classified based on PI score. a PFS plots and b OS plots of risks groups from 118 TCGA patients not used in the feature selection. c OS plots of risk groups from 380 TCGA patients with OS times. d OS plots of risks groups from the Murat et al. data set used for validation. The two numbers in the topright corner of each plot represents the total number of patients in each risk group and the number of patients who experienced progression or death within the follow-up periods, respectively
Two hundred seventy nine of the 380 patients who received adjuvant chemotherapy and radiotherapy died before the end of the follow-up period. The remaining 101 patients were alive at the end of follow-up or were lost to follow-up. The 380 patients were split into low- and high-risk groups. Figure 3c shows the OS plots for these prognostic groups. There was a statistically significant difference in OS between the groups (p<0.05). The median OS time (548 days, 95% CI = 486 - 646) of the low-risk group was significantly higher than that (442 days, 95% CI = 394 - 476) of the high-risk group (p<0.05).
Thirty nine patients in the validation cohort received adjuvant chemotherapy and radiation. The β’s computed with the TCGA cohort and the expression levels of the signature genes in the validation cohort were used to calculate PI scores for the patients in the validation cohort. The patients were then split into low- and high-risk groups. The median OS of the low-risk group was higher than that of the high-risk group, and the difference in OS between the groups was statistically significant (p<0.05) (Fig. 3d).
The results show that the 35-gene signature identified from the TCGA dataset may be a generically applicable predictor of progression-free and overall survival in GBM, since prognostic value in the prediction of overall survival was validated in an independent cohort.
The 35-gene signature predicts progression-free and overall survival in four GBM subtypes
The prognostic value of the signature in predicting PFS and OS in subtypes of GBM was assessed. 51, 51, 3 and 66 patients belonged to the classical, proneural, neural, and mesenchymal subtypes, respectively. Figure 4 shows the results of the PFS survival analysis in the subtypes. There was statistically significant difference in survival between low- and high-risk groups in all the subtypes (p<0.05). In the classical subtype, the median PFS times of low- and high-risk groups were 256 and 186 days respectively. In the mesenchymal subtype, the median PFS times were 269 and 146 days respectively. In the neural subtype, the median PFS times were 358 and 172 days, respectively. In the proneural subtype, the median PFS times were 304 and 172 days, respectively.
Kaplan-Meier progression-free survival plots for risk groups of patients in each subtype of GBM. The patients were classified based on PI score. The two numbers in the topright corner of each plot represents the total number of patients in each risk group and the number of patients who experienced progression or death within the follow-up periods, respectively
One hundred five classical, 95 proneural, 60 neural and 120 mesenchymal subtype patients were used for subtype-specific OS analysis. Figure 5 shows the Kaplan-Meier OS plots for high-risk and low-risk groups in each subtype. The low- and high-risk groups differed significantly in OS in all the subtypes (p<0.05). In the classical subtype, the median OS times of low- and high-risk groups were 544 and 452 days respectively. In the mesenchymal subtype, the median OS times were 485 and 394 days respectively. In the neural subtype, the median OS times were 476 and 435 days, respectively. In the proneural subtype, the median OS times were 748 and 395 days, respectively. Reports from previous studies show that the prognostic value of MGMT promoter methylation in GBM patients is controversial. Zhang et al. [56] showed that MGMT promoter methylation was associated with better PFS and OS in patients with GBM regardless of therapeutic intervention, and associated with longer OS in GBM patients treated with alkylating agents. Costa et al. [5] did not find significant association between MGMT promoter methylation and the outcome of Portuguese GBM patients treated with temozolomide. Brennan et al. [20] however reported that MGMT promoter methylation was only correlated with OS in the GBM classical subtypes. The possible explanation for these conflicting reports on the prognostic value of MGMT promoter methylation could thus be due to differences in the GBM subtype distribution which was not considered in most previous studies. Our 35-gene signature, however, predicted PFS and OS regardless of the subtype, suggesting that it may be a more effective predictor of overall and progression-free survival in GBM.
Kaplan-Meier overall survival plots for risk groups of patients in each subtype of GBM. The patients were classified based on PI score. The two numbers in the topright corner of each plot represents the total number of patients in each risk group and the number of patients who experienced progression or death within the follow-up periods, respectively
The 35-gene signature is an independent predictor of PFS and OS in GBM patients
A multivariate Cox regression model analysis involving the prognostic index, age and MGMT promoter methylation was carried to assess the independence of the gene signature to predict PFS and OS. 79 TCGA GBM patients had associated days to progression, and age and MGMT promoter methylation status (38 methylated and 41 unmethylated) data. Two hundred sixty nine patients had days to death and age and MGMT promoter methylation (135 methylated and 134 unmethylated) data. The results from the univariate and multivariate analyses on the three variable are shown in Table 3. MGMT promoter methylation was not correlated with PFS in both univariate and multivariate Cox analyses (p>0.05). Prognostic index, age and MGMT promoter methylation were significantly correlated with OS in the univariate and multivariate analyses (p<0.05). The univariate Cox’s proportional hazard analysis showed that age and the prognostic index based on the 35-gene signature were both significantly correlated with PFS (p<0.05), but only the prognostic index was significantly correlated with PFS in the multivariate analysis (p<0.05). This showed that the expression signature is an independent predictor of PFS and OS in GBM patients.
Post-treatment tumour progression depends largely on alterations in classical cancer and chemotherapy/radiation resistance-related pathways. This is supported by findings from the multivariate Cox’s proportional hazard analysis findings as only the 35-gene prognostic index was significantly associated with PFS and was an independent predictor of PFS. Overall survival, on the other hand, is determined by many factors. Age at diagnosis is one of the most important factors associated with overall survival in cancer and has been demonstrated in GBM [57–59]. While the prognostic value of MGMT promoter methylation in GBM remains controversial, our findings showed that prognostic index, age and MGMT promoter methylation are all independent prognostic factors for overall survival.
Signature genes belong to a functional interaction subnetwork enriched for known cancer pathways
A subnetwork generated from the interactions between the signature genes had significantly more interactions than would be expected for a random set of proteins of similar size (PPI enrichment p=1.11×10−16) (Fig. 6). The network was also significantly enriched (p<0.01) for KEGG cancer pathways and pathways known to drive tumour initiation and progression, such as the cell cycle and PI3K-Akt, Wnt, p53 and Ras signaling [60, 61].
A subset of the signature genes may be relevant to GBM biology and may have utility in drug discovery
Combinatorial medicine have been proposed for the treatment of tumour recurrence. It involves therapeutically targeting as many genomic alterations responsible for a disease in a patient as possible and has strong implications for overcoming the challenge of tumour progression and drug resistance [62, 63]. One of the ways to overcome this challenge is to prioritise combinations of genes to be targeted based on their unique roles in tumour progression. Of the signature genes, only ABL1, CCND1, CCNE1, PDGFRA, PIK3CA were found to be linked to predisposition to at least one cancer by the Online Mendelian Inheritance in Man (OMIM) database [64]. However, CCNA1, CDK2, CDKN1C, CDKN2A, FZD3, HSPA1B, IGFBP3, PDGFRA, PIK3CA, PLA2G5, THBS2 and VEGFA all have gene ontology annotations related to apoptosis, while ABL1, FZD7, PDGFRA, PIK3CA, SFRP1, THBS2, and VEGFA are annotated as being involved in angiogenesis (data not shown). Collectively this may indicate differential gene expression explicitly directed towards towards resisting induced cell death by both intrinsic and extrinsic factors and optimising the tumour microenvironment for maximum fitness. This, combined with the knowledge that the signature genes are involved in classical pathways implicated in cancer drug resistance, suggests that the highlighted genes should be further validated and assessed as drug targets in designing novel combinatorial therapies for GBM in future studies.
Conclusion
We propose that the performance of the signature makes it an attractive candidate for further studies to assess its utility as a clinical prognostic and predictive biomarker in GBM patients, and that its component genes may also have utility as therapeutic targets for improving both progression-free and overall survival.
References
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, Kros JM, Hainfellner JA, Mason W, Mariani L, Bromberg JEC, Hau P, Mirimanoff RO, Cairncross JG, Janzer RC, Stupp R. MGMT Gene Silencing and Benefit from Temozolomide in Glioblastoma. N Engl J Med. 2005; 352(10):997–1003. https://doi.org/10.1056/NEJMoa043331.
Kim YS, Kim SH, Cho J, Kim JW, Chang JH, Kim DS, Lee KS, Suh CO. MGMT gene promoter methylation as a potent prognostic factor in glioblastoma treated with temozolomide-based chemoradiotherapy: a single-institution study. Int J Radiat Oncol Biol Phys. 2012; 84(3):661–7. https://doi.org/10.1016/j.ijrobp.2011.12.086.
Shen D, Liu T, Lin Q, Lu X, Wang Q, Lin F, Mao W. MGMT Promoter Methylation Correlates with an Overall Survival Benefit in Chinese High-Grade Glioblastoma Patients Treated with Radiotherapy and Alkylating Agent-Based Chemotherapy: A Single-Institution Study. PLoS ONE. 2014; 9(9):107558. https://doi.org/10.1371/journal.pone.0107558.
Melguizo C, Prados J, González B, Ortiz R, Concha A, Alvarez PJ, Madeddu R, Perazzoli G, Oliver JA, López R, Rodríguez-Serrano F, Aránega A. MGMT promoter methylation status and MGMT and CD133 immunohistochemical expression as prognostic markers in glioblastoma patients treated with temozolomide plus radiotherapy. J Transl Med. 2012; 10(1):250. https://doi.org/10.1186/1479-5876-10-250.
Costa BM, Caeiro C, Guimarães I, Martinho O, Jaraquemada T, Augusto I, Castro L, Osório L, Linhares P, Honavar M, Resende M, Braga F, Silva A, Pardal F, Amorim J, Nabiço R, Almeida R, Alegria C, Pires M, Pinheiro C, Carvalho E, Lopes JM, Costa P, Damasceno M, Reis RM. Prognostic value of MGMT promoter methylation in glioblastoma patients treated with temozolomide-based chemoradiation: a Portuguese multicentre study. Oncol Rep. 2010; 23(6):1655–62.
Yin A-a, Zhang L-h, Cheng J-x, Dong Y, Liu B-l, Han N, Zhang X. The Predictive but Not Prognostic Value of MGMT Promoter Methylation Status in Elderly Glioblastoma Patients: A Meta-Analysis. PLoS ONE. 2014; 9(1):85102. https://doi.org/10.1371/journal.pone.0085102.
Goldstein LJ, Gray R, Badve S, Childs BH, Yoshizawa C, Rowley S, Shak S, Baehner FL, Ravdin PM, Davidson NE, Sledge GW, Perez EA, Shulman LN, Martino S, Sparano JA. Prognostic Utility of the 21-Gene Assay in Hormone Receptor–Positive Operable Breast Cancer Compared With Classical Clinicopathologic Features. J Clin Oncol. 2008; 26(25):4063–71. https://doi.org/10.1200/JCO.2007.14.4501.
Paik S, Shak S, Tang G, Kim C, Baker J, Cronin M, Baehner FL, Walker MG, Watson D, Park T, Hiller W, Fisher ER, Wickerham DL, Bryant J, Wolmark N. A Multigene Assay to Predict Recurrence of Tamoxifen-Treated, Node-Negative Breast Cancer. N Engl J Med. 2004; 351(27):2817–26. https://doi.org/10.1056/NEJMoa041588.
Acs G, Kiluk J, Loftus L, Laronga C. Comparison of Oncotype DX and Mammostrat risk estimations and correlations with histologic tumor features in low-grade, estrogen receptor-positive invasive breast carcinomas. Mod Pathol. 2013; 26(11):1451–60. https://doi.org/10.1038/modpathol.2013.88.
Ring BZ, Seitz RS, Beck R, Shasteen WJ, Tarr SM, Cheang MCU, Yoder BJ, Budd GT, Nielsen TO, Hicks DG, Estopinal NC, Ross DT. Novel prognostic immunohistochemical biomarker panel for estrogen receptor-positive breast cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2006; 24(19):3039–47. https://doi.org/10.1200/JCO.2006.05.6564.
van ’t Veer LJ, Dai H, van de Vijver MJ, He YD, Hart AAM, Mao M, Peterse HL, van der Kooy K, Marton MJ, Witteveen AT, Schreiber GJ, Kerkhoven RM, Roberts C, Linsley PS, Bernards R, Friend SH. Gene expression profiling predicts clinical outcome of breast cancer. Nature. 2002; 415(6871):530–6. https://doi.org/10.1038/415530a.
Soneson C, Gerster S, Delorenzi M. Batch Effect Confounding Leads to Strong Bias in Performance Estimates Obtained by Cross-Validation. PLoS ONE. 2014; 9(6):100335. https://doi.org/10.1371/journal.pone.0100335.
Reese SE, Archer KJ, Therneau TM, Atkinson EJ, Vachon CM, de Andrade M, Kocher J-PA, Eckel-Passow JE. A new statistic for identifying batch effects in high-throughput genomic data that uses guided principal component analysis. Bioinformatics. 2013; 29(22):2877–83. https://doi.org/10.1093/bioinformatics/btt480.
TCGA: Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature. 2008; 455(7216):1061–8. https://doi.org/10.1038/nature07385.
Verhaak RGW, Hoadley KA, Purdom E, Wang V, Qi Y, Wilkerson MD, Miller CR, Ding L, Golub T, Mesirov JP, Alexe G, Lawrence M, O’Kelly M, Tamayo P, Weir BA, Gabrie S, Winckler W, Gupta S, Jakkula L, Feiler HS, Hodgson JG, James CD, Sarkaria JN, Brennan C, Kahn A, Spellman PT, Wilson RK, Speed TP, Gray JW, Meyerson M, Getz G, Perou CM, Hayes DN. An integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR and NF1. Cancer Cell. 2010; 17(1):98. https://doi.org/10.1016/j.ccr.2009.12.020.
Kahn AB, Ryan MC, Liu H, Zeeberg BR, Jamison DC, Weinstein JN. SpliceMiner: a high-throughput database implementation of the NCBI Evidence Viewer for microarray splice variant analysis. BMC Bioinformatics. 2007; 8(1):75. https://doi.org/10.1186/1471-2105-8-75.
Liu H, Zeeberg BR, Qu G, Koru AG, Ferrucci A, Kahn A, Ryan MC, Nuhanovic A, Munson PJ, Reinhold WC, Kane DW, Weinstein JN. AffyProbeMiner: a web resource for computing or retrieving accurately redefined Affymetrix probe sets. Bioinformatics. 2007; 23(18):2385–90. https://doi.org/10.1093/bioinformatics/btm360.
Iacob G, Dinca E. Current data and strategy in glioblastoma multiforme. J Med Life. 2009; 2(4):386–93.
Tang PA, Bentzen SM, Chen EX, Siu LL. Surrogate end points for median overall survival in metastatic colorectal cancer: Literature-based analysis from 39 randomized controlled trials of first-line chemotherapy. J Clin Oncol. 2007; 25(29):4562–8. https://doi.org/10.1200/JCO.2006.08.1935.
Brennan CW, Verhaak RGW, McKenna A, Campos B, Noushmehr H, Salama SR, Zheng S, Chakravarty D, Sanborn JZ, Berman SH, Beroukhim R, Bernard B, Wu CJ, Genovese G, Shmulevich I, Barnholtz-Sloan J, Zou L, Vegesna R, Shukla SA, Ciriello G, Yung W, Zhang W, Sougnez C, Mikkelsen T, Aldape K, Bigner DD, Van Meir EG, Prados M, Sloan A, Black KL, Eschbacher J, Finocchiaro G, Friedman W, Andrews DW, Guha A, Iacocca M, O’Neill BP, Foltz G, Myers J, Weisenberger DJ, Penny R, Kucherlapati R, Perou CM, Hayes DN, Gibbs R, Marra M, Mills GB, Lander E, Spellman P, Wilson R, Sander C, Weinstein J, Meyerson M, Gabriel S, Laird PW, Haussler D, Getz G, Chin L. The Somatic Genomic Landscape of Glioblastoma. Cell. 2013; 155(2):462–77. https://doi.org/10.1016/j.cell.2013.09.034.
Shtivelman E, Hensing T, Simon GR, Dennis PA, Otterson GA, Bueno R, Salgia R, Shtivelman E, Hensing T, Simon GR, Dennis PA, Otterson GA, Bueno R, Salgia R. Molecular pathways and therapeutic targets in lung cancer. Oncotarget. 2014; 5(6):1392–433. https://doi.org/10.18632/oncotarget.1891.
Bagnyukova TV, Serebriiskii IG, Zhou Y, Hopper-Borge EA, Golemis EA, Astsaturov I. Chemotherapy and signaling: How can targeted therpies supercharge cytotoxic agents?Cancer Biol Ther. 2010; 10(9):839–53. https://doi.org/10.4161/cbt.10.9.13738.
Riedel RF, Porrello A, Pontzer E, Chenette EJ, Hsu DS, Balakumaran B, Potti A, Nevins J, Febbo PG. A genomic approach to identify molecular pathways associated with chemotherapy resistance. Mol Cancer Ther. 2008; 7(10):3141–9. https://doi.org/10.1158/1535-7163.MCT-08-0642.
Fojo T. Cancer, DNA repair mechanisms, and resistance to chemotherapy. J Natl Cancer Inst. 2001; 93(19):1434–6. https://doi.org/10.1093/jnci/93.19.1434.
Sherman-Baust CA, Becker KG, Wood III WH, Zhang Y, Morin PJ. Gene expression and pathway analysis of ovarian cancer cells selected for resistance to cisplatin, paclitaxel, or doxorubicin. J Ovarian Res. 2011; 4:21. https://doi.org/10.1186/1757-2215-4-21.
Long J, Zhang Y, Yu X, Yang J, LeBrun D, Chen C, Yao Q, Li M. Overcoming Drug Resistance in Pancreatic Cancer. Expert Opin Ther Targets. 2011; 15(7):817–28. https://doi.org/10.1517/14728222.2011.566216.
Pritchard JR, Lauffenburger DA, Hemann MT. Understanding resistance to combination chemotherapy. Drug Resist Updat. 2012; 15(5):249–57. https://doi.org/10.1016/j.drup.2012.10.003.
Humphrey RW, Brockway-Lunardi LM, Bonk DT, Dohoney KM, Doroshow JH, Meech SJ, Ratain MJ, Topalian SL, Pardoll DM. Opportunities and challenges in the development of experimental drug combinations for cancer. J Natl Cancer Inst. 2011; 103(16):1222–6. https://doi.org/10.1093/jnci/djr246.
Reuter S, Gupta SC, Chaturvedi MM, Aggarwal BB. Oxidative stress, inflammation, and cancer: How are they linked?Free Radic Biol Med. 2010; 49(11):1603–16. https://doi.org/10.1016/j.freeradbiomed.2010.09.006.
West KA, Castillo SS, Dennis PA. Activation of the PI3k/Akt pathway and chemotherapeutic resistance. Drug Resist Updat Rev Commentaries Antimicrob Anticancer Chemother. 2002; 5(6):234–48.
Housman G, Byler S, Heerboth S, Lapinska K, Longacre M, Snyder N, Sarkar S. Drug Resistance in Cancer: An Overview. Cancers. 2014; 6(3):1769–92. https://doi.org/10.3390/cancers6031769.
Davis AP, Murphy CG, Johnson R, Lay JM, Lennon-Hopkins K, Saraceni-Richards C, Sciaky D, King BL, Rosenstein MC, Wiegers TC, Mattingly CJ. The Comparative Toxicogenomics Database: update 2013. Nucleic Acids Res. 2013; 41(Database issue):1104–14. https://doi.org/10.1093/nar/gks994.
Guyon I, Weston J, Barnhill S, Vapnik V. Gene Selection for Cancer Classification using Support Vector Machines. Mach Learn. 2002; 46(1-3):389–422. https://doi.org/10.1023/A:1012487302797.
Murat A, Migliavacca E, Gorlia T, Lambiv WL, Shay T, Hamou MF, de Tribolet N, Regli L, Wick W, Kouwenhoven MCM, Hainfellner JA, Heppner FL, Dietrich PY, Zimmer Y, Cairncross JG, Janzer RC, Domany E, Delorenzi M, Stupp R, Hegi ME. Stem cell-related “self-renewal” signature and high epidermal growth factor receptor expression associated with resistance to concomitant chemoradiotherapy in glioblastoma. J Clin Oncol Off J Am Soc Clin Oncol. 2008; 26(18):3015–24. https://doi.org/10.1200/JCO.2007.15.7164.
Szklarczyk D, Morris JH, Cook H, Kuhn M, Wyder S, Simonovic M, Santos A, Doncheva NT, Roth A, Bork P, Jensen LJ, von Mering C. The STRING database in 2017: quality-controlled protein–protein association networks, made broadly accessible. Nucleic Acids Res. 2017; 45:362–8. https://doi.org/10.1093/nar/gkw937.
Zhao X, Rødland EA, Sørlie T, Naume B, Langerød A, Frigessi A, Kristensen VN, Børresen-Dale AL, Lingjærde OC. Combining gene signatures improves prediction of breast cancer survival. PLoS ONE. 2011; 6(3):17845. https://doi.org/10.1371/journal.pone.0017845.
Lau SK, Boutros PC, Pintilie M, Blackhall FH, Zhu CQ, Strumpf D, Johnston MR, Darling G, Keshavjee S, Waddell TK, Liu N, Lau D, Penn LZ, Shepherd FA, Jurisica I, Der SD, Tsao MS. Three-gene prognostic classifier for early-stage non small-cell lung cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2007; 25(35):5562–9. https://doi.org/10.1200/JCO.2007.12.0352.
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJB, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO. European Organisation for Research and Treatment of Cancer Brain Tumor and Radiotherapy Groups, National Cancer Institute of Canada Clinical Trials Group. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005; 352(10):987–96. https://doi.org/10.1056/NEJMoa043330.
Jiang BH, Liu LZ. Role of mTOR in anticancer drug resistance. Drug Resist Updat Rev Commentaries Antimicrob Anticancer Chemother. 2008; 11(3):63–76. https://doi.org/10.1016/j.drup.2008.03.001.
Niero EL, Rocha-Sales B, Lauand C, Cortez BA, de Souza MM, Rezende-Teixeira P, Urabayashi MS, Martens AA, Neves JH, Machado-Santelli GM. The multiple facets of drug resistance: one history, different approaches. J Exp Clin Cancer Res CR. 2014; 33(1):37. https://doi.org/10.1186/1756-9966-33-37.
Martin HL, Smith L, Tomlinson DC. Multidrug-resistant breast cancer: current perspectives. Breast Cancer Targets Ther. 2014; 6:1–13. https://doi.org/10.2147/BCTT.S37638.
Shi RY, Yang XR, Shen QJ, Yang LX, Xu Y, Qiu SJ, Sun YF, Zhang X, Wang Z, Zhu K, Qin WX, Tang ZY, Fan J, Zhou J. High expression of Dickkopf-related protein 1 is related to lymphatic metastasis and indicates poor prognosis in intrahepatic cholangiocarcinoma patients after surgery. Cancer. 2013; 119(5):993–1003. https://doi.org/10.1002/cncr.27788.
Wong SCC, He CW, Chan CML, Chan AKC, Wong HT, Cheung MT, Luk LLY, Au TCC, Chiu MK, Ma BBY, Chan ATC. Clinical Significance of Frizzled Homolog 3 Protein in Colorectal Cancer Patients. PLoS ONE. 2013; 8(11):79481. https://doi.org/10.1371/journal.pone.0079481.
Zheng L, Sun D, Fan W, Zhang Z, Li Q, Jiang T. Diagnostic Value of SFRP1 as a Favorable Predictive and Prognostic Biomarker in Patients with Prostate Cancer. PLoS ONE. 2015; 10(2):0118276. https://doi.org/10.1371/journal.pone.0118276.
Saran U, Arfuso F, Zeps N, Dharmarajan A. Secreted frizzled-related protein 4 expression is positively associated with responsiveness to Cisplatin of ovarian cancer cell lines in vitro and with lower tumour grade in mucinous ovarian cancers. BMC Cell Biol. 2012; 13(1):25. https://doi.org/10.1186/1471-2121-13-25.
Roy PG, Pratt N, Purdie CA, Baker L, Ashfield A, Quinlan P, Thompson AM. High CCND1 amplification identifies a group of poor prognosis women with estrogen receptor positive breast cancer. Int J Cancer. J Int Du Cancer. 2010; 127(2):355–60. https://doi.org/10.1002/ijc.25034.
Seiler R, Thalmann GN, Rotzer D, Perren A, Fleischmann A. CCND1/CyclinD1 status in metastasizing bladder cancer: a prognosticator and predictor of chemotherapeutic response. Mod Pathol. 2014; 27(1):87–95. https://doi.org/10.1038/modpathol.2013.125.
Allera-Moreau C, Rouquette I, Lepage B, Oumouhou N, Walschaerts M, Leconte E, Schilling V, Gordien K, Brouchet L, Delisle MB, Mazieres J, Hoffmann JS, Pasero P, Cazaux C. DNA replication stress response involving PLK1, CDC6, POLQ. RAD51 and CLASPIN upregulation prognoses the outcome of early/mid-stage non-small cell lung cancer patients. Oncogenesis. 2012; 1(10):30. https://doi.org/10.1038/oncsis.2012.29.
Xing X, Cai W, Shi H, Wang Y, Li M, Jiao J, Chen M. The prognostic value of CDKN2a hypermethylation in colorectal cancer: a meta-analysis. Br J Cancer. 2013; 108(12):2542–8. https://doi.org/10.1038/bjc.2013.251.
Maeda K, Kawakami K, Ishida Y, Ishiguro K, Omura K, Watanabe G. Hypermethylation of the CDKN2A gene in colorectal cancer is associated with shorter survival. Oncol Rep. 2003; 10(4):935–8. https://doi.org/10.3892/or.10.4.935.
Mihara M, Shintani S, Nakahara Y, Kiyota A, Ueyama Y, Matsumura T, Wong DT. Overexpression of CDK2 is a prognostic indicator of oral cancer progression. Jpn J Cancer Res Gann. 2001; 92(3):352–60.
Cretu A, Sha X, Tront J, Hoffman B, Liebermann DA. Stress sensor Gadd45 genes as therapeutic targets in cancer. Cancer Ther. 2009; 7(A):268–76.
Zerbini LF, Libermann TA. GADD45 Deregulation in Cancer: Frequently Methylated Tumor Suppressors and Potential Therapeutic Targets. Clin Cancer Res. 2005; 11(18):6409–13. https://doi.org/10.1158/1078-0432.CCR-05-1475.
Guo W, Dong Z, Guo Y, Chen Z, Kuang G, Yang Z. Methylation-mediated repression of GADD45a and GADD45g expression in gastric cardia adenocarcinoma. Int J Cancer J Int Du Cancer. 2013; 133(9):2043–53. https://doi.org/10.1002/ijc.28223.
Guo W, Zhu T, Dong Z, Cui L, Zhang M, Kuang G. Decreased expression and aberrant methylation of Gadd45g is associated with tumor progression and poor prognosis in esophageal squamous cell carcinoma. Clin Exp Metastasis. 2013; 30(8):977–92. https://doi.org/10.1007/s10585-013-9597-2.
Zhang K, Wang X-q, Zhou B, Zhang L. The prognostic value of MGMT promoter methylation in Glioblastoma multiforme: a meta-analysis. Familial Cancer. 2013; 12(3):449–58. https://doi.org/10.1007/s10689-013-9607-1.
Scott JG, Suh JH, Elson P, Barnett GH, Vogelbaum MA, Peereboom DM, Stevens GHJ, Elinzano H, Chao ST. Aggressive treatment is appropriate for glioblastoma multiforme patients 70 years old or older: a retrospective review of 206 cases. Neuro-Oncol. 2011; 13(4):428–36. http://dx.doi.org/10.1093/neuonc/nor005.
Thumma SR, Fairbanks RK, Lamoreaux WT, Mackay AR, Demakas JJ, Cooke BS, Elaimy AL, Hanson PW, Lee CM. Effect of pretreatment clinical factors on overall survival in glioblastoma multiforme: a Surveillance Epidemiology and End Results (SEER) population analysis. World J Surg Oncol. 2012; 10:75. https://doi.org/10.1186/1477-7819-10-75.
Bozdag S, Li A, Riddick G, Kotliarov Y, Baysan M, Iwamoto FM, Cam MC, Kotliarova S, Fine HA. Age-Specific Signatures of Glioblastoma at the Genomic. Genetic, and Epigenetic Levels. PLoS ONE. 2013; 8(4):62982. https://doi.org/10.1371/journal.pone.0062982.
Feitelson MA, Arzumanyan A, Kulathinal RJ, Blain SW, Holcombe RF, Mahajna J, Marino M, Martinez-Chantar ML, Nawroth R, Sanchez-Garcia I, Sharma D, Saxena NK, Singh N, Vlachostergios PJ, Guo S, Honoki K, Fujii H, Georgakilas AG, Amedei A, Niccolai E, Amin A, Ashraf SS, Boosani CS, Guha G, Ciriolo MR, Aquilano K, Chen S, Mohammed SI, Azmi AS, Bhakta D, Halicka D, Nowsheen S. Sustained proliferation in cancer: mechanisms and novel therapeutic targets. Semin Cancer Biol. 2015; 35:25–54. https://doi.org/10.1016/j.semcancer.2015.02.006.
Zhang J, Chen YH, Lu Q. Pro-oncogenic and anti-oncogenic pathways: opportunities and challenges of cancer therapy. Futur Oncol. 2010; 6(4):587–603. https://doi.org/10.2217/fon.10.15.
Al-Lazikani B, Banerji U, Workman P. Combinatorial drug therapy for cancer in the post-genomic era. Nat Biotechnol. 2012; 30(7):679–92. https://doi.org/10.1038/nbt.2284.
Tang J, Karhinen L, Xu T, Szwajda A, Yadav B, Wennerberg K, Aittokallio T. Target inhibition networks: predicting selective combinations of druggable targets to block cancer survival pathways. PLoS Comput Biol. 2013; 9(9):1003226. https://doi.org/10.1371/journal.pcbi.1003226.
Amberger JS, Bocchini CA, Schiettecatte F, Scott AF, Hamosh A. OMIM.org: Online mendelian inheritance in man (OMIM®;), an online catalog of human genes and genetic disorders. 2015; 43:789–98. https://doi.org/10.1093/nar/gku1205.
Acknowledgements
Not applicable.
Availability of data and materials
The datasets supporting the conclusions of this article are available in the NCI Genomic Data Commons Data Portal (https://portal.gdc.cancer.gov/projects/TCGA-GBM) and in the NCBI Gene Expression Omnibus (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE7696).
Authors’ information
Not applicable.
Author information
Authors and Affiliations
Contributions
AAF conceived and designed the experiments, and analyzed the data. AAF wrote the paper under JG’s guidance. JG supervised all aspects of this work, and read, edited and approved the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1
Workflow of the modified SVM-RFE used for selecting a set of genes that discriminated between rapidly-progressing and slow-progressing GBM patients. (XLSX 66.7 kb)
Additional file 2
Genes with high expression variance used in pathway enrichment analysis. (PDF 23.5 kb)
Additional file 3
Unguided principal component analysis to identify batch effect in the TCGA data set as a function of genes from chemoradioresistance-associated pathways. p=0.118, indicating absence of significant batch effect in the data. Samples in each batch are denoted by a different colour and symbol. (TXT 2.05 kb)
Additional file 4
Unguided principal component analysis to assess batch effect. (PDF 161 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License(http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver(http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Fatai, A., Gamieldien, J. A 35-gene signature discriminates between rapidly- and slowly-progressing glioblastoma multiforme and predicts survival in known subtypes of the cancer. BMC Cancer 18, 377 (2018). https://doi.org/10.1186/s12885-018-4103-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-018-4103-5