Abstract
Background
We investigated whether GSTT1 (“null” allele), GSTM1 (“null”allele), GSTP1 (A313G), RFC1 (G80A), MTHFR (C677T), TS (2R/3R) polymorphisms were associated with toxicity and survival in patients with early breast cancer (EBC) treated with adjuvant chemotherapy (CT).
Methods
This prospective trial included patients with stage I–III BC subjected to CT with CMF or FEC regimens. PCR-RFLP was performed for MTHFR, RFC1 and GSTP1, while PCR for TS, GSTT1 and GSTM1 genes.
Results
Among the 244 patients consecutively enrolled, 48.7% were treated with FEC and 51.3% with CMF. Patients with TS2R/3R genotype showed less frequently severe neutropenia (G3/G4) than those with TS2R/2R and 3R/3R genotype (p = 0.038). Patients with MTHFRCT genotype had a higher probability of developing severe neutropenia than those with MTHFR CC genotype (p = 0.043). Patients with RFC1GG or GSTT1-null genotype or their combination (GSTT1-null/RFC1GG) were significantly associated with a shorter disease free survival (DFS) (p = 0.009, p = 0.053, p = 0.003, respectively) and overall survival (OS) (p = 0.036, p = 0.015, p = 0.005, respectively). Multivariate analysis confirmed the association of RFC1GG genotype with a shorter DFS (p = 0.018) and of GSTT1-null genotype of a worse OS (p = 0.003), as well as for the combined genotypes GSTT1-null/RFC1GG, (DFS: p = 0.004 and OS: p = 0.003).
Conclusions
Our data suggest that TS2R/2R and 3R/3R or MTHFR CT genotypes have a potential role in identifying patients with greater risk of toxicity to CMF/FEC and that RFC1 GG and GSTT1-null genotypes alone or in combination could be important markers in predicting clinical outcome in EBC patients.
Similar content being viewed by others
Background
Breast cancer (BC) currently accounts for 20% of all female cancers worldwide and is the most frequent malignancy occurring in women [1]. There is convincing evidence that adjuvant systemic chemotherapy (AC) increases survival of patients with BC [2]. AC imparted a statistically significant reduction in the risk of BC relapse and death at 5 years of follow-up (with a hazard reduction of approximately 25%), and combination chemotherapy was found to be significantly more effective than single-agent therapy [3]. Trials included more than 15 years of follow-up and led to the conclusion that AC conferred benefit to both premenopausal and postmenopausal patients and also to node-positive and node-negative patients [4]. In general, approximately one of every four recurrences and one of seven deaths is avoided annually by adjuvant chemotherapy [5].
Among the treatments used in this adjuvant setting, the combination of cyclophosphamide (CP), methotrexate (MTX) and 5-fluorouracil (5-FU) (CMF treatment) or the combination of 5-FU, anthracycline-based chemotherapy (adriamycin or its analogue epirubicin) and CP (FAC/FEC treatment) are the most commonly used. Although the benefit of BC chemotherapy has been demonstrated, these drugs have shown the ability to induce DNA damage in eukaryotic cells [6, 7] and, consequently, chemotherapy treatment involves a risk of provoking DNAdamage even in proliferative non-cancer cells [8] therefore leading to a marked toxicity state. Adverse events represent an important physical, psychological and financial burden for the patient and society since up to 15% of the patients receiving FEC will experience at least one serious adverse event [9, 10]. Besides toxicity, another major clinical problem encountered during adjuvant CMF or FEC treatments is BC recurrence of therapeutically resistant disease and thus affecting the long-term outcome of the patient. Significant variability in drug response may occur among cancer patients treated with the same medications [11].
Germline genetic variation in drug metabolizing enzymes and transporters is thought to contribute to the observed inter-individual variation in treatment toxicity and/or efficacy [12]. Recently, pharmacogenomic studies have elucidated the inherited nature of these differences in drug disposition and effects, thereby providing a stronger scientific basis for optimizing drug therapy according to each patient’s genetic constitution. Candidate genes are thymidylate synthase (TS), 5, 10-methylenetetrahydrofolate reductase (MTHFR), the reducer folate carrier (RFC1) and glutathione-S-transferases (GSTs), involved in CMF or FEC adjuvant chemotherapies transport and/or metabolism, or being targets of such drugs, as it is shown in Fig. 1. TS is an enzyme implicated in the conversion of deoxyuridine monophosphate (dUMP) into deoxythymidine monophosphate (dTMP), which is essential in DNA synthesis. The human TS gene (hTS) is polymorphic with either double (2R) or triple (3R) tandem repeats of a 28 base-pair sequence downstream of the cap site in the 5′ terminal regulatory region [13]. In vitro studies, the activity of a reporter gene linked to the 5′ terminal fragment of the hTS gene with triple (3R) tandem repeats was 2.6 times higher than that with double (2R) tandem repeats [14]. Thus, this polymorphic region TS 2R/3R appears to be functional and may modulate TS gene expression. MTHFR is an enzyme responsible for the metabolization of vitamin B9 (folate), which is required for DNA synthesis. A known MTHFR gene polymorphism consists of a 677C > T transition, in exon 4, which results in an alanine to valine substitution in the predicted catalytic domain of MTHFR. This substitution renders the enzyme thermolabile, and homozygotes and heterozygotes have about 70 and 35% reduced enzyme activity, respectively [15]. RFC1 is a major MTX transporter whose impaired function has been recognized as a frequent mechanism of antifolate resistence [16]. Different gene alterations affecting RFC1 transport properties were found in cell lines selected for antifolate resistance [17]. A polymorphism G > A at position 80 in exon 2 of RFC1 gene which replaces His by Arg at position 27 of the RFC1 protein was identified. A recent study implied an effect of G > A80 in combination with C > T677 in MTHFR on plasma folate levels and homocysteine pools [18]. It is known that the mechanism of cytotoxicity with chemotherapy is through the generation of reactive oxygen species (ROS) and their by-products. The reactive molecules responsible for cytotoxicity of these therapies are subject to enzymatic removal, and variability of cells in sensitivity to therapy could depend, at least in part, on the availability and activity of specific metabolizing enzymes. GSTs enzymes are an important cellular defence system that protects cells from chemical injury by catalyzing conjugation of reactive electrophilic molecules with glutathione (GSH). GSTs catalyze the detoxification of some alkylating agents used in chemotherapy and detoxification of products of reactive oxidation [19]. GSTs M1 and T1 have been shown to have activity toward lipid hydroperoxides [20], and individuals lacking each of these enzymes (null allele) may have reduced removal of secondary organic oxidation products produced by cancer therapy and thus may have better prognoses. The pi-class human GST (GSTP1) besides playing a role in protection from oxidative damage was shown to catalyze GSH conjugation of reactive cyclophosphamide metabolites in vitro assays [21]. The present study aimed at investigating the association between TS 2R/3R, MTHFR C677T, RFC1 G80A and GSTT1 null, GSTM1 null or GSTP1 A313G polymorphisms with toxicity, disease free survival (DFS) and overall survival (OS) in Caucasian patients with early BC treated with CMF or FEC regimens.
Metabolism of chemotherapeutic drugs-related gene polymorphisms. In cancer cells 5-FU is converted to 5-fluorodeoxyuridine monophosphate (5-FdUMP). 5-FdUMP inhibits the DNA synthesis by competing with deoxyuridine monophosphate (dUMP) for binding to thymidylate synthase (TS) in a complex that is stabilized by the reduced folate 5,10-methylene tetrahydrofolate. 5-FU can also inhibit RNA synthesis in a pathway that involves its metabolism to 5-fluorouridinemonophosphate (5-FUMP) and subsequent conversion to 5-fluorouridine triphosphate (5-FUTP) via 5-fluorouridine diphosphate (5-FUDP). The main effect of cyclophosphamide is due to its metabolite phosphoramide mustard that forms DNA crosslinks both between and within DNA strands at guanine N-7 positions (known as interstrand and intrastrand crosslinkages, respectively). This is irreversible and leads to cell apoptosis. Anthracyclines inhibit DNA and RNA synthesis by intercalating between base pairs of the DNA/RNA strand, thus preventing the replication of rapidly growing cancer cells. In addition, they can generate reactive oxygen species (ROS) damaging DNA, proteins and cell membranes. Glutathione S-transferases (GSTs) catalyse the detoxification of alkylating agents used in chemotherapy and/or ROS
Methods
Study population
This prospective study was conducted in patients with a histological diagnosis of stage I-III BC treated with conservative surgery or mastectomy, and subjected to adjuvant chemotherapy with CMF or FEC regimens. Tumor staging followed the TNM-AJCC classification [22] and the pTNM was obtained after classical pathological examination. Patients with metastatic disease and with other previous tumors were excluded from this study. Recorded clinical and pathological features for each patient included: age, menopausal status, histology, grade, stage, estrogen receptors (ER) and progesterone receptor (PgR) status, Ki67, p53, HER2 and medical adjuvant therapy. ER, PgR, Ki67, p53 and HER2 status were assessed at the time of surgery on formalin-fixed paraffin-embedded tissue blocks of the primary tumor in the Pathology Department of the University of Perugia. We used the following cut-off for considering Ki 67 positive >14%, [23] p53 positive ≥ 1%, Her2 positive IHC 3+ or IHC 2+ and FISH amplified. Written informed consent was obtained by all patients and the study was reviewed and approved by the institution’s Ethics Committee in accordance with the principles established in the Helsinki declaration.
Chemotherapy regimen
Treatment combined regimen was as follows: CMF (cyclophosphamide 600 mg/m2, MTX 40 mg/m2 and 5-fluorouracil 600 mg/m2) administered on day 1 and 8 each 4 weeks, for 6 cycles; FEC (5-fluorouracil 600 mg/m2, 4-epirubicin 90 mg/m2 and cyclophosphamide 600 mg/m2) administered on day 1, every 21 days, for 6 cycles. Physical examination and a full blood counts were performed after each chemotherapy cycle. Hepatic and renal function tests were assessed at baseline and repeated before each cycle of treatment. All patients who had received at least one course of chemotherapy were evaluated for toxicity. Toxicity was scored every 3 weeks according to the Common Toxicity Criteria of the National Cancer Institute (NCI-CTC, version 2.0) [24].
We defined “severe toxicity” as hematological or gastrointestinal toxicity of grade 3–4.
Genotyping analysis
Genomic DNA was extracted from 200 μL of whole blood using the Qiamp blood kit (Qiagen, Milan, Italy) according to the manufacturer’s instructions. Polymorphisms were characterized using the PCR-RFLP for genotyping analyses of MTHFR, RFC1 and GSTP1, while PCR was used for TS polymorphism determination. Multiplex PCR was used to simultaneously amplify GSTT1 and GSTM1, with albumin as a control gene. All primers used in this study were designed by using Primer express 2.0 software (Applied Biosystems, Italy). The primer sequences, restriction enzymes and PCR conditions used in the study are shown in Additional file 1: Table S1.
Statistical analysis
Allele and genotype frequencies for each polymorphism were calculated and tested as to whether they were distributed according to the Hardy-Weinberg equilibrium. A chi-square test for deviation from Hardy-Weinberg equilibrium was used to estimate differences in allele frequencies. The association of each polymorphism and clinical-pathological features of the patients was assessed by means of a chi-square test. A univariate logistic regression model was used to assess the effect of the same variables, included as dummy variables on incidence of toxicity (0–1-2 grade vs. 3–4), expressing results as odds ratios (OR) and relative 95% confidence intervals (95% CIs). Disease free survival (DFS) was defined as the time from the treatment start up to the date of first progression or death from any cause, whichever came first. Patients who had not died or had disease progression at the date of analysis were censored at the last available information on status. Overall survival (OS) was defined as the time from the treatment start to the date of death from any cause. Time-to-event data were described by the Kaplan-Meier curves. Cox proportional hazards models were used for univariate and multivariate analyses to estimate and test clinical-pathological features and polymorphisms for their associations with DFS and OS. Variables statistically significant at univariate analysis (at a level of p < 0.10) were included in the multivariate models. Results were expressed as hazard ratio (HRs) and their 95% CIs. Due to the explorative nature of the study, no adjustment of the significance level to make allowance for multiple tests has been made. Statistical significance was set at p < 0.05. All statistical analyses were carried out using SAS version 9.2 (SAS Institute, Cary, NC).
Results
Patient characteristics
From June 2000 to September 2005 a total of 244 consecutive Caucasian patients with conservative surgery or mastectomy for primary BC, referred to the Breast Unit Surgical Department of the University of Perugia, Italy, were recruited. Histological diagnosis was confirmed by a pathologist at the Institute of Pathology, University of Perugia. The main clinical-pathological characteristics of the patients are summarized in Table 1.
Frequencies and associations among the polymorphisms and clinical-pathological features
The associations between genetic polymorphisms and the patient clinical-pathological features are reported in Additional file 2: Table S2.
The frequencies of genotypes GSTT1-null e GSTM1-null were 20.5% and 54.1%, respectively and GSTM1-null allele was significantly higher in stage I than the GSTM1-present allele (p = 0.042). The frequencies of the genotypes GSTP1 AA, AG, and GG were 59.4%, 39.3%, and 1.2%, respectively. GSTP1 AA genotype was significantly higher in stage III, in positive lymph nodes and in negative p53, than the GSTP1 AG or GG genotype (p = 0.006, p = 0.027 and p = 0.033, respectively). For MTHFR the frequencies of CC, CT, and TT were 27.5%, 47.5%, and 25.0%, respectively and the MTHFR CT or TT genotypes were significantly higher in stage III or in positive lymph nodes than the MTHFR CC genotype (p = 0.025 and p = 0.011, respectively). For the RFC1 polymorphism, the frequencies of GG, GA, and AA were 30.3%, 46.3%, and 23.4%, respectively. The frequencies of TS tandem repeat genotype distribution were 32.8% in 3R3R, 35.2% in 3R2R, and 32.0% in 2R2R. There was no statistically significant association among genotype distributions and tumor size, grading, ER, PgR, Ki67 and HER2 status. The genotype distribution observed was similar to that expected under Hardy-Weinberg equilibrium.
Toxicity and effect of polymorphisms in whole BC group
All 244 patients were evaluable for toxicity. Hematological and non-hematological toxicities to CMF/FEC regimen were evaluated and are summarized in Additional file 3: Table S3. Among patients with BC who developed toxicity the prevalence of hematologic and non-hematologic toxicities of any grade was as follows: 63 neutropenia (25.8%), 58 leucopenia (23.7%), 13 anemia (5.2%), 46 mucositis (18.8%) and 35 hepatic toxicity (14.3%). Among BC patients treated with CMF (n = 124) the prevalence of hematologic and non-hematologic toxicities of any grade was as follows: 28 neutropenia (22.5%), 27 leucopenia (21.7%), 6 anemia (4.8%), 27 mucositis (21.7%) and 18 hepatic (14.5%) toxicity. Among BC patients treated with FEC (n = 120) the prevalence of hematologic and non-hematologic toxicities of any grade was as follows: 24 neutropenia (20.0%), 20 leucopenia (16.6%), 8 anemia (6.6%), 18 mucositis (15.0%) and 15 hepatic (12.5%) toxicity. There were no statistically significant differences between Table S4:CMF and FEC regimens in terms of toxicity (Additional file 3: Table S3). Grade 3/4 toxicity was observed overall in 14.3% (35/244) of patients: 10% (24/244) for hematological toxicity, 4.5% (11/244) for non-hematological toxicity (alopecia not included). A few patients experienced cycle delay (n.5 patients) or dose reduction (n.8 patients). No toxic deaths were observed in this study. Associations between genotypes and toxicities are reported in Table 2. A significant association was detected between the number of 28-bp tandem repeats in the 5′-untranslated region of the TS gene and the severity of toxicity. The patients with 2R/3R TS genotype showed less frequently severe (G3/G4) neutropenia than patients with 2R/2R TS genotype (OR = 0.25, 95% CI: 0.06–0.93p = 0.038). The patients with CT MTHFR genotype had a higher probability of developing severe neutropenia than patients with CC MTHFR genotype (OR = 8.32 95% CI: 1.06–65.2, p = 0.043). When considering toxicity of any grade (G1–4), patients with 2R/3R TS genotype had a lower probability of developing oral mucositis (OR = 0.36 95% CI: 0.16–0.82, p = 0.015, Additional file 4: Table S4). No other statistically significant differences in toxicity were found with respect to the other polymorphisms.
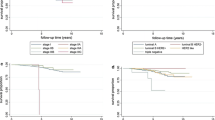
Survival analysis
At a median follow-up of 9.2 years (interquartile range: 8.2–10.6), we observed 38 (15.6%) disease recurrences, 16 (6.6%) second tumors and 41 (16.8%) deaths. Overall the patients with recurrence and/or second tumor and/or deaths were 85 (34.8%). Loco-regional recurrence was observed in 13 patients (34.2%) and metastatic disease in 25 patients (65.8%): dominant site was visceral in 28 of 38 patients (76.7%). Results of univariate analysis for DFS and OS are reported in Table 3.Both patients with genotype RFC1 GG and genotype RFC1 GA had a shorter DFS in comparison to those with genotype AA (HR = 2.89, 95% CI: 1.31–6.38, p = 0.009; HR = 2.35, 95% CI: 1.09–5.07, p = 0.029 for GG and GA, respectively (Fig. 2a- DFS curves for RFC1). Patients with genotype RFC1 GG had a shorter OS in comparison to those with genotype AA (HR = 2.90, 95% CI: 1.07–7.88, p = 0.036) while patients with genotype RFC1 GA did not show a different survival when compared with genotype AA (HR = 1.95, 95% CI: 0.79–5.22, p = 0.184) (Fig. 2b- OS curves for RFC1). DFS was also shorter in patients with genotype GSTT1-null when compared to patients with genotype GSTT1-present (HR = 1.68, 95% CI: 0.99–2.86, p = 0.05) (Fig. 2c- DFS curves for GSTT1). OS was also shorter in patients with genotype GSTT1-null when compared to patients with genotype GSTT1-present (HR = 2.22, 95% CI: 1.17–4.24, p = 0.015). (Fig. 2d- OS curves for GSTT1). The multivariate model (including age, ER/PgR positive, stage, the genotypes GSTT1 and RFC1) for DFS and OS showed that the genotype RFC1 GG confirmed a shorter DFS when compared to RFC1 AA genotype (HR = 2.64, 95% CI: 1.18–5.90, p = 0.018), while genotype GSTT1-null was confirmed as a independent prognostic factor for a worse OS (HR = 2.82, 95% CI: 1.41–5.64, p = 0.003) (Table 4).
Kaplan Meier curves by RFC1 and GSTT1 status. Disease-Free Survival by RFC1 polymorphism a. GSTT1 status c. and combined genotype groups e. Overall Survival by RFC1 polymorphism b. GSTT1 status d. and combined genotype groups f. Combined genotype groups were as follows: group1: GSTT1-present and RFC1-AA; group2: GSTT1-present and RFC1-GA/RFC1-GG or GSTT1-null and RFC1-GA/RFC1-AA; group3: GSTT1-null and RFC1-GG
According to genotypes of GSTT1 and RFC1 genes we classified patients in three groups: the first with GSTT1-present and RFC1-AA (group1), the second with GSTT1-present and RFC1-GA/RFC1-GG or GSTT1-null and RFC1-GA/RFC1-AA (group2), and the third with GSTT1-null and RFC1-GG (group3).
Kaplan-Meier curves for DFS and OS are reported in Fig. 2e and f, respectively. At univariate analysis, confirmed at multivariate analysis (Table 4) both for DFS and OS, group2 showed a worse prognosis compared with group1 (HR = 4.20, 95% CI 1.52–11.56, P = 0.006; HR = 4.54, 95% CI 1.09–18.92, P = 0.038 for DFS and OS respectively). A greater difference was detected when compared group3 with group1 (HR = 6.61, 95% CI 1.93–22.59, P = 0.003; HR = 10.12, 95% CI 2.04–50.19, P = 0.005 for DFS and OS respectively).
Discussion
In the present study, we demonstrated that among BC patients who received CMF or FEC, those possessing the TS 2R/3R variant showed a significantly lower risk of severe toxicity (grade 3–4) for neutropenia and, when considering toxicity of any grade (G1–4), the same variant conferred a lower probability of developing oral mucositis. Our data are in agreement with previously published studies [25,26,27] confirming a significant inverse association of TS 2R/3R polymorphism and severity toxicity. However, whereas in the study by Lecomte et al. patients with the 2R/2R genotype were 20 times more likely to have severe toxicity compared with 3R/3R carriers, this effect was much less pronounced in our study and more similar to the results of Schwab’s study [28]. However, the role of other 5-FU catabolism-involved polymorphisms, such as dihydropyrimidine dehydrogenase (DPYD), should be explored to improve prediction of 5-FU toxicity [29]. At present, the real predictive value of MTHFR C677T polymorphism on MTX and 5-FU toxicity is not completely established. In our study, we found that the patients with MTHFR CT genotype had a higher probability of developing severe neutropenia than patients with MTHFR CC genotype. Some recent studies have shown increased toxicity in 677 T–carriers treated with methotrexate [30,31,32], although other studies did not confirm such an association [33, 34]. Different methotrexate doses and schemes as well as diverse nutritional/folate status might account, at least in part, for these discrepant results. Probably, the heterozygous effects of MTHFR CT and TS 2R/3R genotypes as compared to each homozygous effect might be justified by considering that exogen factors, environmental conditions, dietary habits and lifestyle might play an important role [25,26,27, 35, 36]. No other significant differences in toxicity were found with respect to the other polymorphisms. There are a few studies on the role of GSTs isoenzymes on mortality in BC survivors drawn from community practice. The majority of these studies have small sample sizes, are based on participants diagnosed prior to 1999 and on women undergoing chemotherapy and/or radiotherapy. In addition, most of them examined only one GST gene (usually GSTP1). In our study, we showed that genotype GSTT1-null was associated with worse DFS and OS in EBC patients. This association was maintained in the multivariate model only for OS independently of age and other traditional predictors of prognosis. Our results are based on the assumption that the individuals with GSTT1-null genotype, that is associated with an absence of enzyme activity, are considered to be at increased risk for malignancies due to reduced efficiency in protection against environmental carcinogens [37, 38]. Conversely, Ambrosone et al. [39], showed that GSTM1-null and GSTT1-null genotypes predicted significantly better DFS and OS, both individually or in combination. Our results on GSTM1genotype are in agreement with those of Lizard-Nacol et al. [40] who, showed no effect of GSTM1-null genotype on DFS or OS among 92 women with advanced BC who had received cyclophosphamide, doxorubicin, and 5-FU. Whereas, Kristensen et al. [41] found that patients with GSTM1-null allele had a significantly shorter OS. Moreover, Yu Ke-Da et al. [42] showed a more complicated role for GSTM1 that should be considered in breast cancer risk prediction. The results of this study indicated a U-shaped association of GSTM1 with breast cancer, which challenges the linear gene-dosage effect of GSTM1 that was previously proposed. This effect was due to a new SNP, rs412543 (−498C > G) located in the promoter region that decreased gene transcription by 30–40% via reducing the DNA-binding affinity of AP-2. In contrast to these previous studies, our study is the only one to examine adjuvant therapy in a population of patients with a relatively uniform recurrence risk, with a longer follow-up (9.2 years), providing a homogeneous patient population in which to study treatment related genotypes and outcomes. Genetic background differences among races account for differences in the frequencies of allelic variants so that the association of polymorphic variants with a disease risk can significantly vary among populations. As far as we know, scanty information is available on the association of chemotherapeutic drug-related gene polymorphisms on toxicity and survival of breast cancer patients in non Caucasian populations. The results of Yang et al. showed no association between any of the GSTM1 or GSTT1 genotypes in patients with breast carcinoma who were treated with chemotherapy [43].
RFC1 genotypes, as predictors of BC treatment efficacy, have not been previously reported. Recent evidence suggests that G80A polymorphism in RFC1 is associated with altered folate/antifolate levels and may influence the efficacy of therapy with MTX [39]. Data suggest that subjects carrying the homozygous mutant AA genotype tend to have higher plasma folate and MTX levels and higher erythrocyte polyglutamate levels compared with those with the wild type or heterozygous genotype. In our study, for the first time to our knowledge, we showed that patients with RFC1 GG genotype had a shorter DFS and OS than carriers of the AA genotype. These observations are in keeping with previous studies on rheumatoid arthritis (RA). The work of Drozdzik et al. [44] showed that patients with RFC1 AA genotype responded to the therapy more effectively than carriers of AG and GG genotypes. The remission of RA symptoms was significantly higher (3.32-fold) in AA carriers in comparison to GG individuals. In contrast to RA patients, the study on acute lymphoblastic leukemia of Laverdiere et al. [45] showed children with AA genotype had worse prognoses than patients with GG genotype, and AA genotype was associated with higher plasma levels of MTX than other genotypes. Moreover, we showed, in an explorative analysis, that the combined genotypes (GSTT1-null/RFC1-GG) had a negative prognostic effect on DFS and OS. This subgroup of tumors could have a more aggressive clinical course and the availability of a non-invasive, repeatable and reproducible technique to detect polymorphisms in the blood appears to be a useful tool for identifying high-risk BC patients. Therefore, further large sample size and well designed studies are greatly needed to confirm these preliminary results. Limitations of our study include relatively small sample size and low number of events, thus we were not able to evaluate the association with outcome by subgroups, such as menopausal status. Nevertheless, the association between GST polymorphisms and BC survival, showed by our results seems to be in agreement with those of the literature [39, 40].
The cohort was established before some current treatments, such as aromatase inhibitors, and Her2/neu targeted therapies were available. Therefore, we cannot estimate what associations GST isoenzymes might have with survival in women using these treatments. However, our study has a larger sample size than most prior studies examining the association between GST polymorphisms and survival and it is the first study to evaluate RFC1 genotypes as predictors of BC treatment efficacy.
Conclusions
In conclusion, our study provides important novel information about the potential role of drug-transporter enzyme polymorphisms in the outcome after adjuvant therapy for EBC. Confirmation of these findings in a large sample size and well designed studies and supportive mechanistic data will ultimately allow the potential for drug-transporter genotyping to be realized in the clinic to individualize and optimize EBC therapy.
References
Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108.
Guarneri V, Conte PF. The curability of breast cancer and the treatment of advanced disease. Eur J Nucl Med Mol Imaging. 2004;31:S149–61.
The Ludwig Breast Cancer Study Group. Combination adjuvant chemotherapy for node-positive breast cancer inadequacy of a single erioperative cycle. N Engl J Med. 1988;319:677–83.
Early Breast Cancer Trialists’ Collaborative Group. Systemic treatment of early breast cancer by hormonal cytotoxic or immune therapy 133 randomised trials involving 31000 recurrences and 24000 deaths among 75000 women. Lancet. 1992;339:1–15.
Early Breast Cancer Trialists’ Collaborative Group. Polychemotherapy for early breast cancer: an overview of the randomised trials. Lancet. 1998;352:930–42.
Anderson D, Bishop JB, Colin Garner R, Ostrosky-Wegman P, Selby PB. Cyclophosphamide: review of its mutagenicity for an assessment of potential germ cell risks. Mutat Res. 1995;330:115–81.
Longley DB, Harkin DP, Johnston PG. 5-fluorouracil: mechanisms of action and clinical strategies. Nat Rev Cancer. 2003;3:330–8.
Kopjar N, Garaj-Vrhovac V, Milas I. Assessment of chemotherapy-induced DNA damage in peripheral blood leukocytes of cancer patients using the alkaline comet assay. Teratog Carcinog Mutagen. 2002;22:13–30.
Roché H, Fumoleau P, Spielmann M, Canon JL, Delozier T, Serin D, Symann M, Kerbrat P, Soulié P, Eichler F, Viens P, Monnier A, Vindevoghel A, Campone M, Goudier MJ, Bonneterre J, Ferrero JM, Martin AL, Genève J, Asselain B. Sequential adjuvant epirubicin-based and docetaxel chemotherapy for node-positive breast cancer patients the FNCLCC PACS 01. Trial J Clin Oncol. 2006;24:5664–71.
Hasset MJ, O’Malley AJ, Pakes JR, Newhouse JP, Earle CC. Frequency and cost of chemotherapyrelated serious adverse effects in a population sample of women with breast cancer. J Natl Cancer Inst. 2006;98:1108–17.
Choi JY, Nowell SA, Blanco JG, Ambrosone CB. The role of genetic variability in drug metabolism pathways in breast cancer prognosis. Pharmacogenomics. 2006;7:613–24.
Gonzalez-Neira A. Pharmacogenetics of chemotherapy efficacy in breast cancer. Pharmacogenomics. 2012;13(6):677–90.
Horie N, Aiba H, Ogura K, Hojo H, Takeishi K. Functional analysis and DNA polymorphism of the tandemly repeated sequences in the 59-terminal regulatory region of the human gene for thymidylate synthase. Cell Struct Funct. 1995;20:191–7.
Horie N, Chimoto M, Nozawa R, Takeishi K. Characterization of the the Pharmacogenomics journal regulatory sequences and nuclear factors that function in cooperation with the promoter of the human thymidylate synthase gene. Biochem Biophys Acta. 1993;1216:409–16.
Frost P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG, Boers GJ, den Heijer M, Kluijtmans LA, van den Heuvel LP, Rozen R. A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolatereductase. Nat Genetics. 1995;10:111–3.
Gorlick R, Goker E, Trippett T, Waltham M, Banerjee D, Bertino JR. Intrinsic and acquired resistance to methotrexate in acute leukemia. N Engl J Med. 1996;335(14):1041–8.
Moskow JA. Reduced folate carrier gene (RFC1) expression and anti-folate resistance in transfected and non-selected cell lines. Int J Cancer. 1997;72:184–90.
Chango A, Emery-Fillon N, de Courcy GP, Lambert D, Pfister M, Rosenblatt DS, Nicolas JP. A polymorphism (80G/a) in the reduced folate carrier gene and its associations with folate status and homocysteinemia. Mol Genet Metab. 2000;70:310–5.
Hayes JD, Pulford DJ. The glutathione S-transferase supergene family: regulation of GST and the contribution of the isoenzymes to cancer chemoprotection and drug resistance. Crit Rev Biochem Mol Biol. 1995;30:445–600.
Hurst R, Bao Y, Jemth P, Mannervik B, Williamson G. Phospholipid hydroperoxide glutathione peroxidase activity of human glutathione transferases. Biochem J. 1998;332:97–100.
Dirven HA, Van Ommen B, Van Bladeren PJ. Involvement of human glutathione S-transferaseisoenzymes in the conjugation of cyclophosphamide metabolites with glutathione. Cancer Res. 1994;54:6215–20.
Singletary SE, Allred C, Ashley P, Bassett LW, Berry D, Bland KI, Borgen PI, Clark G, Edge SB, Hayes DF, Hughes LL, Hutter RV, Morrow M, Page DL, Recht A, Theriault RL, Thor A, Weaver DL, Wieand HS, Greene FL. Revision of the American joint committee on cancer staging system for breast cancer. J Clin Oncol. 2002;20:3628–36.
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thürlimann B, Senn HJ. Panel members. Strategies for subtypes--dealing with the diversity of breast cancer: highlights of the St. Gallen international expert consensus on the primary therapy of early breast cancer 2011. Ann Oncol. 2011;22(8):1736–47. doi:10.1093/annonc/mdr304. Epub 2011 Jun 27
Common Terminology Criteria for Adverse Events v2.0 (CTCAE) Available at: ctepcancergov/reporting/ctchtml [Last Accessed 1 January 2010].
Pullarkat ST, Stoehlmacher J, Ghaderi V, Xiong YP, Ingles SA, Sherrod A, Warren R, Tsao-Wei D, Groshen S, Lenz HJ. Thymidylate synthase gene polymorphism determines response and toxicity of 5-FU chemotherapy. Pharmacogenomics J. 2001;1:65–70.
Adleff V, Hitre E, Köves I, Orosz Z, Hajnal A, Kralovánszky J. Heterozygote deficiency in thymidylate synthase enhancer region polymorphism genotype distribution in Hungarian colorectal cancer patients. Int J Cancer. 2004;108:852–6.
Lecomte T, Ferraz JM, Zinzindohoué F, Loriot MA, Tregouet DA, Landi B, Berger A, Cugnenc PH, Jian R, Beaune P, Laurent-Puig P. Thymidylate synthase gene polymorphism predicts toxicity in colorectal cancer patients receiving 5-fluorouracil-based chemotherapy. Clin Cancer Res. 2004;10:5880–8.
Schwab M, Zanger UM, Marx C, Schaeffeler E, Klein K, Dippon J, Kerb R, Blievernicht J, Fischer J, Hofmann U, Bokemeyer C, Eichelbaum M. German 5-FU toxicity study group: role of genetic and nongenetic factors for fluorouracil treatment-related severe toxicity: a prospective clinical trial by the German 5-FU toxicity study group. JCO. 2008;26(13):2131–8.
Van Kuilenburg AB. Dihydropyrimidine dehydrogenase and the efficacy and toxicity of 5-fluorouracil. Eur J Cancer. 2004;40:939–50.
Ulrich CM, Yasui Y, Storb R, Schubert MM, Wagner JL, Bigler J, Ariail KS, Keener CL, Li S, Liu H, Farin FM, Potter JD. Pharmacogenetics of methotrexate toxicity among marrow transplantation patients varies with the methylenetetrahydrofolatereductase C677T polymorphism. Blood. 2001;98:231–4.
Chiusolo P, Reddiconto G, Casorelli I, Laurenti L, Sorà F, Mele L, Annino L, Leone G, Sica S. Preponderance of methylenetetrahydrofolatereductase C677T homozygosity among leukemia patients intolerant to methotrexate. Ann Oncol. 2002;13:1915–9.
Toffoli G, Russo A, Innocenti F, Corona G, Tumolo S, Sartor F, Mini E, Baiocchi M. Effect of methylenetetrahydrofolatereductase 677C→T polymorphism on toxicity and homocysteine plasma level after chronic methotrexate treatment of ovarian cancer patients. Int J Cancer. 2003;103:294–9.
Kishi S, Griener J, Cheng C, Das S, Cook EH, Pei D, Hudson M, Rubnitz J, Sandlund JT, Pui CH, Relling MV. Homocysteinepharmacogenetics and neurotoxicity in children with leukemia. J Clin Oncol. 2003;21:3084–91.
Seidemann K, Book M, Zimmermann M, Meyer U, Welte K, Stanulla M, Reiter A. MTHFR 677 (C→T) polymorphism is not relevant for prognosis or therapy-associated toxicity in pediatric NHL: results from 484 patients of multicenter trial NHL-BFM 95. Ann Hematol. 2006;85:291–300.
Sidoti A, Antognelli C, Rinaldi C, D'Angelo R, Dattola V, Girlanda P, Talesa V, Amato A. Glyoxalase I A111E, paraoxonase 1 Q192R and L55M polymorphisms: susceptibility factors of multiple sclerosis? Mult Scler. 2007;13(4):446–53.
Antognelli C, Del Buono C, Ludovini V, Gori S, Talesa VN, Crinò L, Barberini F, Rulli A. CYP17, GSTP1, PON1 and GLO1 gene polymorphisms as risk factors for breast cancer: an Italian case-control study. BMC Cancer. 2009;9:115.
McIlwain CC, Townsend DM, Tew KD. Glutathione S-transferasepolymorphisms: cancer incidence and therapy. Oncogene. 2006;25:1639–48.
Gao LB, Pan XM, Li LJ, Liang WB, Bai P, Rao L, Su XW, Wang T, Zhou B, Wei YG, Zhang L. Null genotypes of GSTM1 and GSTT1 contribute to risk of cervical neoplasia: an evidence-based meta-analysis. PLoS One. 2001;6(5):e20157. doi:10.1371/journal.pone.0020157.
Ambrosone CB, Sweeney C, Coles BF, Thompson PA, McClure GY, Korourian S, Fares MY, Stone A, Kadlubar FF, Hutchins LF. Polymorphisms in glutathione S-transferases (GSTM1 and GSTT1) and survival after treatment for breast cancer. Cancer Res. 2001;61(19):7130–5.
Lizard-Nacol S, Coudert B, Colosetti P, Riedinger JM, Fargeot P, Brunet-Lecomte P. Glutathione S-transferase M1 null genotype: lack of association with tumour characteristics and survival in advanced breast cancer. Breast Cancer Res. 1999;1:81–7.
Nedelcheva Kristensen V, Andersen TI, Erikstein B, Geitvik G, Skovlund E, Nesland JM, Børresen-Dale AL. Single tube multiplex polymer-ase chain reaction genotype analysis of GSTM1 GSTT1 and GSTP1: relation of genotypes to TP53 tumor status and clinicopathological variables in breast cancer patients. Pharmacogenetics. 1998;8:441–7.
Yu KD, Di GH, Fan L, Wu J, Hu Z, Shen ZZ, Huang W, Shao ZM. A functional polymorphism in the promoter region of GSTM1 implies a complex role for GSTM1 in breast cancer. FASEB J. 2009;23(7):2274–87.
Yang G, Shu XO, Ruan ZX, Cai QY, Jin F, Gao YT, Zheng W. Genetic polymorphisms in glutathione-S-Transferase genes (GSTM1, GSTT1, GSTP1) and survival after chemotherapy for invasive breast carcinoma. Cancer. 2005;103(1):52–8.
Drozdzik M, Rudas T, Pawlik A, Gornik W, Kurzawski M, Herczynska M. Reduced folate carrier-1 80G>A polymorphism Yu KD, Di GH, Fan L, Wu J, Hu Z, Shen ZZ, Huang W, Shao ZM. A functional polymorphism in the promoter region of GSTM1 implies a complex role for GSTM1 in breast cancer. FASEB J. 2009 Jul;23(7):2274–87affects methotrexate treatment outcome in rheumatoid arthritis. Pharmacogenomics J. 2007;7:404–7.
Laverdiere C, Chiasson S, Costea I, Moghrabi A, Krajinovic M. Polymorphism G80A in the reduced folate carrier gene and its relationship to methotrexate plasma levels and outcome of childhood acute lymphoblastic leukemia. Blood. 2002;100(10):3832–4.
Acknowledgements
The authors would like to remember Irene Floriani for her technical support and to dedicate this work to her, who deceased. She was head of the Clinical Research Laboratory of Mario Negri institute in Milan, Italy. They also want to remember her commitment, dedication and professionalism as well as the human talent that she had and which led us to reallocate many oncological research projects. Her loss is tremendous to our Society and especially to our hearts. The authors also express their gratitude to the patients who participated in this study.
Funding
This work was supported in part (reagents for gene polymorphism analysis) by Consiglio Nazionale delle Ricerche (CNR), by the Umbria Association Against Cancer (AUCC) and by “Conoscere per Vincere” charities.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
Conception and design: VL, SG; MT; Manuscript writing: VL; Statistical analysis: ER, IF; Patient management/enrolment: AR, JF, EL, SG, LC; genotyping analysis: LP, GN, FRT, SP; Histological diagnosis and biomolecular characterization: AS; Review of the manuscript: VL, CA, VNT. All authors approved the final version of this article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study is in compliance with the Helsinki declaration. Ethical approval has been granted by the Institutional Review Board of the Comitato Etico Aziende Sanitarie (CEAS) Umbria (reference-number: 9440). Upon inclusion, a written informed consent is obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1: Table S1.
Characteristics of the studied polymorphisms. (DOC 46 kb)
Additional file 2: Table S2.
Association among gene polymorphisms and clinical-pathological features. (DOC 99 kb)
Additional file 3:Table S3.
CMF/FEC treatment-related toxicity graded according to the NCI- CTC v.2.0. (DOC 55 kb)
Additional file 4: Table S4.
Association among gene polymorphisms and risk of toxicity of any grade (grade1–2–3-4 vs 0). (DOC 83 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ludovini, V., Antognelli, C., Rulli, A. et al. Influence of chemotherapeutic drug-related gene polymorphisms on toxicity and survival of early breast cancer patients receiving adjuvant chemotherapy. BMC Cancer 17, 502 (2017). https://doi.org/10.1186/s12885-017-3483-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-017-3483-2