Abstract
Background
To study the association between Apelin expression and the clinical features and postoperative prognosis in patients with gastric cancer (Int J Cancer 136:2388-2401, 2015).
Methods
Tumor samples and matched adjacent normal tissues were collected from 270 patients with GC receiving surgical resection. The tumor and serum Apelin levels were determined by immunohistochemistry and ELISA methods, respectively. GC cell lines were cultured for migration and invasive assays.
Results
Our data showed that tumor Apelin expression status, instead of serum Apelin level, was closely associated with more advance clinical features including tumor differentiation, lymph node and distant metastases. Moreover, patients with high tumor Apelin level had a significantly shorter overall survival period compared to those with low Apelin expression and those with or negative Apelin staining. Our in vitro study revealed that the Apelin regulated the migration and invasion abilities of GC cell lines, accompanied by up-regulations of a variety of cytokines associated with tumor invasiveness.
Conclusion
Our data suggest that tumor Apelin can be used as a marker to evaluate clinical characteristics and predict prognosis in GC patients.
Similar content being viewed by others
Background
Gastric cancer is among the leading causes of global cancer-related mortality [1]. Despite of the recent advances in diagnosis and therapy, the prognosis of GC patients is still poor. Usually, the 5-year survival rates are less than 20 % [2–4]. Currently, there is no specific marker for early diagnosis and prognosis prediction, although a number of proteins have been previously reported to be associated with the outcome of GC patients [5–8].
Apelin is a member of the endogenous ligand of the human G protein receptor, known as APJ [9]. Both Apelin and APJ are extensively expressed in blood vasculature and stimulate angiogenesis by prompting endothelial cell growth [10–12]. Also, Apelin induces the maturation of tumor blood capillaries and prompts tumor vascularization [13]. Moreover, Apelin is upregulated in human cancers and its association with cancer outcomes were reported as well [14–17]. In addition, recent studies show that Apelin has lymphangiogenic potential and it is related to tumor growth and lymph node metastasis in vivo [18, 19].
However, the association of Apelin and gastric cancer remain largely unknown. A recent study reported a higher serum Apelin in patients with gastroesophageal cancer (GEC) compared to healthy controls [20]. Moreover, there is a weak positive correlation between serum Apelin concentrations and tumor Apelin expression levels [20]. In this study, we enrolled GC patients to further investigate the role of tumor and serum Apelin in the clinical features, in particular, disease characteristics and prognosis in GC patients.
Methods
Samples
Tumor samples and matched adjacent non-tumorous tissues were collected from 270 patients with GC receiving surgical resection between 1 January 2009 and 31 December 20013. None of the patients with carcinomas underwent either chemotherapy or radiotherapy before surgery. The tumor stage of patients was determined by the UICC-TNM classification. All the tissue samples were identified by clinical pathologist and then were fixed by formaldehyde and embedded by paraffin for further study. We also collected tissue samples from 81 patients with chronic gastritis as control. All patients were followed by consulting their documents, or through clinic visit or telephone interviews. Overall survival (OS) period was defined as the time interval between the date of surgery and date of death or last follow-up.
Immunohistochemistry
GC tissues sections fixed by formalin and embedded by paraffin were dewaxed in xylene and rehydrated with gradient ethanol. The sections were incubated with rabbit anti-Apelin monoclonal antibody (1:150, Abcam, USA) at 4 °C overnight. The immune complex was detected by a standard avidin-biotin detection system (Dako, USA). The sections were evaluated by three pathologists who were blinded to clinicopathologic information. Apelin staining score = positive cell score + staining intensity score. The percentage of positive cells was classified by four grades (percentage scores): 0 [21], <1/3 [21], 1/3-2/3 [22] and >2/3 [22]. The intensity of staining was also divided into four grades (intensity scores): no staining [21], weak staining [21], moderate staining [22] and strong staining [22]. The overall scores 0, 1–2, 3–4, and 5–6 were defined as negative (−), weak positive (±), moderate positive (+), and strong positive (++) respectively.
Serum apelin level detection
The peripheral blood samples were collected from all participants after 12-h overnight fast. The serum Apelin concentration was measured by an ELISA kit (Apelin-12, Phoenix pharmaceuticals, Belmont, USA) according to manufacturer’ protocol. The sensitivity was 0.05 ng/mL, and intra- and inter-assay variations were <5 and <10 %, respectively.
Cell lines and cell culture
Three GC cell lines, namely, SGC-7901, MKN-45, AGS and an immortalized normal gastric epithelial cell line GES-1, were purchased from Cell Bank of Type Culture Collection (Shanghai China). Cells were maintained in Dulbecco’s Modified Eagle’s medium (DMEM, Gibco) containing 10 % fetal bovine serum (FBS), 100 U/ml penicillin, and 100 ug/ml streptomycin.
Gene silencing of APJ with siRNA
GC cell lines were transfected with 200 nmol/L APJ or nonspecific siRNA (Ambion, USA) in culture medium for 48 h. The medium was then replaced with fresh DMEM and the cells were incubated at 37 °C for an additional 24 h. The cells were collected and stored at −80 °C until assayed for protein expression by Western blotting as detailed below.
Proliferation assay
The effect of hypoxia on the viability of cultured cells was evaluated by 2-(2-methoxy-4-nitrophenyl)-3-(4-nitrophenyl)-5-(2,4-disulfophenyl)-2H-tetrazolium, a monosodium salt (WST-8) assay (Dojindo Molecular Technologies, Japan). Briefly, cells are treated with Apelin (50 and 100 ng/mL) and seeded (cell density of 5 × 103 per well) in 96-well microplates and cultured in the hypoxic incubator for 8 h, followed by addition of 10 ul WST-8 solution to each well. After 4 h of incubated at 37 °C, absorbance was measured at 450 nm using a microplate reader (Benchmark Microplate Reader, BIO-RAD) with a reference wavelength of 490 nm.
Cell migration and invasion analysis
Cells were treated with Apelin (50 and 100 ng/mL) for cell migration and invasion assay by using Transwell chamber (Corning, NY, USA), which coated with Matrigel (BD Bioscience) in invasion assays. 5 × 104 cells were collected and seeded in the upper chamber without serum. 10 % fetal bovine serum was used as a chemoattractant in lower chamber. After 8 h of incubation, cells that did not invade through the pores were wiped out with cotton wool. Invaded cell was stained with 20 % methanol and 0.2 % crystal violet and counted with an inverted microscope (Olympus, Japan).
Western blot analysis
Cells were lysed with RIPA lysis buffer and the lysates protein concentration was measured by a BCA Protein Assay Kit (Pierce, Rockford, USA). The protein samples (10 μg/well) were loaded onto 10 % SDS-PAGE and then transferred onto PVDF membranes. After blocked by skim milk, the membranes were incubated in the primary antibodies for overnight at 4 °C and then in the HRP-conjugated secondary antibody for 2–3 h at room temperature. The primary antibodies used in the experiments were anti-Apelin, anti-APJ (both 1:1000; Abcam, USA), anti- Matrix metalloproteinases1 (MMP1) and MMP9 (both 1:1000; Santa Cruz, USA), anti-Bone morphogenetic protein 2 (BMP2, 1:1000; Santa Cruz, USA), anti-interleukin1 and 6 (IL1 and IL6, both1:1000; Santa Cruz, USA), Finally the protein band images were captured by ECL reagent (Thermo, USA).
Statistical analysis
All data were analyzed using the SPSS 19.0 software (SPSS Inc., Chicago, USA) and GraphPad Prism (Version 6.02 for Windows, Graphpad Software, USA). Qualitative variables were analyzed using either the Chi Square Test or the Fisher’s test. Correlations between Apelin expression and clinical features of GC patients were determined by chi-square test. Survival analysis was performed using the Kaplan-Meier method. COX analysis was used to determine the independent prognostic factor for GC patients. Unless otherwise noted, P < 0.05 was accepted as significant.
Results
The demographical information of patients with GC and patients with chronic gastritis listed in Table 1. There is no significant difference in mean age, gender distribution, smoking status and Helicobacter Pylori infection status between two groups.
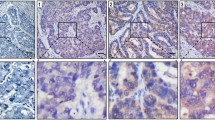
The representative images about Apelin immunohistochemical stainings are shown in Fig. 1a. Apelin is expressed in cytoplasma and also in vascular endothelial cells in the tumor tissue. Cytoplasmic Apelin staining was identified in 112 of 270 normal gastric mucosa samples and 36 of 81 samples with chronic gastritis (41.2 % vs.44.4 %, P = 0.635). The GC patients with strong Apelin staining (show as “++” in Table 1) are 120, with moderate Apelin staining are 99 (show as “+” in Table 1), and only 51 patients had weak or no Apelin staining in this group (show as “±/-” in Table 1). There are a significant difference in Apelin expression status between patients with GC and with chronic gastritis (Table 2).
a shows the representative images about Apelin immunohistochemical stainings. Left, high Apelin expression sample. Apelin is expressed in cytoplasma and also in vascular endothelial cells in the tumor tissue. Right, low Apelin expression sample, Apelin are dominately expressed in vascular endothelial cells. b The serum Apelin levels between patients with GC and chronic gastritis. There is no significant difference in serum Apelin levels between two groups (2.84 ± 1.13 vs.2.52 ± 0.78, ng/mL, P = 0.453)
In contrast, the serum Apelin levels remains similar among GC and Chronic gastritis groups (2.84 ± 1.13 vs.2.52 ± 0.78, ng/mL, P = 0.453, Fig. 1).
We next investigated the relationship between tumor Apelin expression status and clinical characteristics of GC patients. As shown in Table 3, high expression of Apelin in GC cancer samples was associated with poor differentiation, tumor stage, lymph node metastases, and distant metastases. However, there were no significant associations between Apelin expression levels and gender, age, or histology type and tumor size was found (Table 3). When the serum Apelin is studied, we only found that GC patients with lymph node metastasis had a higher serum Aplein level compared to those without (P = 0.043). However, serum Apelin levels are not associated with the other clinical characteristics in GC patients (All P > 0.05, Table 3).
We further analyzed the relation of tumor Apelin expression status with the survival of GC patients in this study. As shown in Fig. 2a, patients with high tumor Apelin staining had a significantly shorter overall survival period compared to those with low Apelin expression and those with weak or negative Apelin staining (22.6 ± 4.9, 29.1 ± 3.7 and 30.4 ± 6.4, months, P < 0.001 by log-rank test, Fig. 2a). We used the mean serum Apelin value (2.84 ng/mL) as a cut-off value to subgroup all GC patients: those with equal or higher than 2.84 ng/mL were assigned into high serum Apelin group (n = 160) and those with lower than 2.84 ng/mL were assigned into low serum Apelin group (n = 110). We found these two groups had similar overall survival period (26.9 ± 5.2 vs. 26.4 ± 2.9, months, P = 0.187 by log-rank test, Fig. 2b).
The relation of tumor Apelin expression status with the survival of GC patients by Kaplan-Miere curves. a Patients with strong Apelin staining had significantly shorter overall survival period 22.6 ± 4.9 months) compared to those with low Apelin expression (29.1 ± 3.7, months) and those with weak or negative Apelin staining (30.4 ± 6.4 months). b GC patients with high and low serum Apelin had similar overall survival period (26.9 ± 5.2 vs. 26.4 ± 2.9, months, P = 0.187 by log-rank test, Fig. 2b)
Subsequently, as shown in Table 4, the univariate COX analysis revealed that the prognosis of GC patients were associated with lymph node metastasis (P = 0.004), tumor differentiation (P = 0.034) and tumor Apelin expression (P = 0.002), but not with serum Apelin level (P = 0.332). Furthermore, the multivariate mode of COX analysis revealed that tumor Apelin expression level wasn a independent prognostic factor for the overall survival in GC patients (P = 0.003).
In our in vitro study, we observed that all GC cell lines, including SGC-7901, MKN-45 and AGS had a 1.5 to 2 folds higher expression levels of Apelin compared to non-cancer cell line GES-1 (Fig. 3a). Similarly, the APJ expression level is higher in GC cell lines than in normal cell line GES-1 (Fig. 3a).
a SGC-7901, MKN-45 and AGS had a higher Apelin expression levels compared GES-1 by western blot assay. b Apelin treatment (50 and 100 ng/mL) for 8 h did not affect the proliferation rates in GC cell lines and non-cancer cell line GES-1. c and d The migration and invasion abilities of GC cell lines were significantly increased by Apelin treatment (50 and 100 ng/mL for 8 h, respectively)
When these cells are treated with Apelin (50 and 100 ng/mL) for 8 h, we observed that proliferation rates remain similar between GC cell lines and non-cancer cell line GES-1 (Fig. 3b). However, the migration and invasion abilities of GC cell lines were significantly increased by Apelin treatment (Fig. 3c-d).
Notably, we observed that Apelin treatment induced the protein expression of a variety of cytokines, such as APJ, MMP1, MMP9, BMP-2, IL1 and IL6 (Fig. 4a). All these cytokines are reported associated with tumor invasive or metastasis.
When these cells are transfected with Apelin receptor APJ si-RNA, an 85 % reduction of APJ was observed and Apelin expression was not affected (Fig. 4b). When the scramble and si-APJ RNA transfected cells were treated with Apelin (100 ug/mL for 24 h), We observed that there is a reduced migration and invasion abilities in GC cell lines (Fig. 4c and d, respectively).
Discussion
In the present study, we studied the correlation between tissue and serum Apelin level with the clinical characteristics and prognosis of GC patients. Our data show that tissue Apelin expression status, instead of serum Apelin level, is closely associated with more advance clinical features and poorer outcome. Our in vitro data further reveals that GC cell lines over-expression Aplein and its receptor APJ, together with the other cytokines which are known to facilitate tumor metastasis and progression, including IL-1, IL6, MMP1, MMP9 and BMP-2. The inhibition of Apelin receptor APJ, reduces the cellular migration and invasion abilities in vitro. Our data suggest that tumor Apelin is a protein marker to evaluate the clinical features and to predict post-operative prognosis in GC patients.
Apelin is a peptide expressed in various tissues, including gastrointestinal tract, heart, lung, liver, and bone [23]. Previous experimental and clinical studies suggest that Apelin is a mitogenic factor for the endothelial cells and stimulates tumor angiogenesis. Recent studies show that Apelin was found to be up-regulated in a variety of human cancers. The Apelin/APJ pathway induces arteriogenesis in samples of poorly-differentiated hepatocellular carcinoma (HCC) [24]. Using Apelin as a marker to monitor tumor vessel normalization window during anti-angiogenic therapy was reported [17]. Co-expression of Apelin and APJ in tumor is the basis of an autocrine loop involved in the growth of colon adenocarcinomas [25]. A clinical study showed that Apelin up-regulation is associated with a poor prognosis in oral squamous cell carcinoma patients [24]. However, the role of Apelin in GC is not adequately studied to date.
A recent study detected the serum Apelin level in gastroesophageal cancer (GEC) patients and found that serum Apelin was significantly higher in cachectic patients than in the controls. Serum Apelin is positively correlated with hypersensitive C reactive protein level, suggesting that suggest that Apelin production in serum is probably related to systemic inflammatory response in GEC patients [20]. However, this study did not investigate the prognostic role of Apelin in GC patients. Given serum marker could be easily affected by external condition, such as inflammation and stress, it is of interest to study the effect of tumor Aplein in tumor tissues in GC patients. In our study, we found that GC patients had a significantly higher percentage of having strong Apelin staining than samples from chronic gastritis. However, the serum Apelin levels remains similar among GC and Chronic gastritis groups. Moreover, high expression of Apelin in GC cancer samples was associated with poor differentiation, lymph node metastases and distant metastases. However, serum Apelin levels are not associated with the other clinical characteristics in GC patients.
In this study, we detected several cytokines, including IL-1, IL6, MMP1, MMP9 and BMP-2. There factors are known to be correlated with tumor invasiveness and metastasis in gastric cancer [25–29]. We observed GC cell lines had a higher expression of these factor and their expression can be further increased by Apelin treatment. We postulate that Apelin may prompt tumor invasiveness through up-regulation of these factors.
Recent animal studies indicated that lymphatic vessels interact extensively with malignant cells. Moreover, lymphangiogenesis is associated with lymph node metastasis. Apelin overexpression induces intratumoral lymphangiogenesis and promotes lymphatic metastasis. Apelin increases lymphatic endothelial cells (LEC) spheroid numbers and stimulates capillary-like cord formation of LECs in vitro and promotes the growth of lymph vessels [18]. Consistent with these findings, in this study, we found that tumor Apelin was associated with lymph node metastases.
A previous study suggest that tumor patients had higher Apelin levels compared with healthy controls, and Apelin is closely related to the disease stages and progression independently of other potential confounders [30]. Apelin was expressed in cultured lung cancer cell lines both at the mRNA and protein levels [30]. We observed similar phenomena in cultured GC cell lines. Increased Apelin protein level is associated with elevated microvessel densities and predicts poor overall survival, suggesting Apelin as a novel angiogenic factor in human lung cancer cell [31]. In our study we observed that GC patients with strong Apelin staining had significantly shorter overall survival period compared to those with low Apelin expression and those with weak or negative Apelin staining.
Several limitation should be addressed it this study. Firstly, the sample size is relatively small and only Chinese patients were enrolled. Secondly, the signal pathway under which Apelin/APJ pathway affects cellular biological behavior of gastric cell lines was not included in this study.
Conclusion
In the present study, we reported that tissue Apelin status, rather than serum Apelin level, is closely associated with clinical features and prognosis of GC patietns. in vitro study indicated in GC cell lines inhibition of APJ reduced cellular proliferation rate, migration and invasion ability in vitro, suggesting the involvement of Apelin/APJ pathway in GC progression.
Abbreviations
- BMP:
-
Bone morphogenetic protein
- FBS:
-
Fetal bovine serum
- GC:
-
Gastric cancer
- MMP:
-
Matrix metalloproteinases
- OS:
-
Overall survival
- TNF-α:
-
Tumornecrosisfactor-a
- VEGF:
-
Vascular endothelial growth factor
References
Heine-Broring RC, et al. Dietary supplement use and colorectal cancer risk: a systematic review and meta-analyses of prospective cohort studies. Int J Cancer. 2015;136(10):2388–401.
Msika S, et al. Population-based study of diagnosis, treatment and prognosis of gastric cancer. Br J Surg. 1997;84(10):1474–8.
Zhang XF, et al. Surgical treatment and prognosis of gastric cancer in 2,613 patients. World J Gastroenterol. 2004;10(23):3405–8.
Shen W, et al. Meta-analysis of prognosis after surgical treatment in gastric cancer patients with liver metastasis. Zhonghua Wei Chang Wai Ke Za Zhi. 2014;17(2):128–32.
Liu H, et al. GPRC5A overexpression predicted advanced biological behaviors and poor prognosis in patients with gastric cancer. Tumour Biol. 2016;37(1):503–510.
Bian Y, et al. Elevated rictor expression is associated with tumor progression and poor prognosis in patients with gastric cancer. Biochem Biophys Res Commun. 2015;464(2):534–40.
Cheng G, et al. Expression of Tim-3 in gastric cancer tissue and its relationship with prognosis. Int J Clin Exp Pathol. 2015;8(8):9452–7.
Jiang W, et al. High co-expression of Sp1 and HER-2 is correlated with poor prognosis of gastric cancer patients. Surg Oncol. 2015;24(3):220–5.
He L, et al. Apelin/APJ signaling in hypoxia-related diseases. Clin Chim Acta. 2015;451(Pt B):191–8.
Kojima Y, Quertermous T. Apelin-APJ signaling in retinal angiogenesis. Arterioscler Thromb Vasc Biol. 2008;28(10):1687–8.
Masri B, et al. Apelin signalisation and vascular physiopathology. J Soc Biol. 2009;203(2):171–9.
Peltonen T, et al. Apelin and its receptor APJ in human aortic valve stenosis. J Heart Valve Dis. 2009;18(6):644–52.
Kalin RE, et al. Paracrine and autocrine mechanisms of apelin signaling govern embryonic and tumor angiogenesis. Dev Biol. 2007;305(2):599–614.
Hong L, Han Y, Brain L. The role of epidermal growth factor receptor in prognosis and treatment of gastric cancer. Expert Rev Gastroenterol Hepatol. 2014;8(1):111–7.
Kawahara H, et al. Tumor endothelial cell-specific drug delivery system using apelin-conjugated liposomes. PLoS One. 2013;8(6):e65499.
Kidoya H, et al. The apelin/APJ system induces maturation of the tumor vasculature and improves the efficiency of immune therapy. Oncogene. 2012;31(27):3254–64.
Zhang L, et al. Apelin as a marker for monitoring the tumor vessel normalization window during antiangiogenic therapy. Cancer Sci. 2016;107(1):36–44.
Berta J, et al. Apelin promotes lymphangiogenesis and lymph node metastasis. Oncotarget. 2014;5(12):4426–37.
Rayalam S, et al. Emerging role of apelin as a therapeutic target in cancer: a patent review. Recent Pat Anticancer Drug Discov. 2011;6(3):367–72.
Diakowska D, et al. Serum levels of resistin, adiponectin, and apelin in gastroesophageal cancer patients. Dis Markers. 2014;2014:619649.
Zhang. A comprehensive modular map of molecular interactions in RB/E2F pathway. Mol Syst Biol. 2008;4:173.
Cherra 3rd SJ, Dagda RK, Chu CT. Review: autophagy and neurodegeneration: survival at a cost? Neuropathol Appl Neurobiol. 2010;36(2):125–32.
Sorli SC, et al. Apelin is a potent activator of tumour neoangiogenesis. Oncogene. 2007;26(55):7692–9.
Heo K, et al. Hypoxia-induced up-regulation of apelin is associated with a poor prognosis in oral squamous cell carcinoma patients. Oral Oncol. 2012;48(6):500–6.
Xia Y, et al. Piperine inhibits IL-1beta-induced IL-6 expression by suppressing p38 MAPK and STAT3 activation in gastric cancer cells. Mol Cell Biochem. 2015;398(1–2):147–56.
Kang MH, et al. BMP2 accelerates the motility and invasiveness of gastric cancer cells via activation of the phosphatidylinositol 3-kinase (PI3K)/Akt pathway. Exp Cell Res. 2010;316(1):24–37.
Han J, et al. Additive effects of EGF and IL-1beta regulate tumor cell migration and invasion in gastric adenocarcinoma via activation of ERK1/2. Int J Oncol. 2014;45(1):291–301.
Zhao G, et al. IL-6 mediates the signal pathway of JAK-STAT3-VEGF-C promoting growth, invasion and lymphangiogenesis in gastric cancer. Oncol Rep. 2016;35(3):1787–95.
Chang X, et al. NDRG1 controls gastric cancer migration and invasion through regulating MMP-9. Pathol Oncol Res. 2016;22:789–96.
Lacquaniti A, et al. Apelin beyond kidney failure and hyponatremia: a useful biomarker for cancer disease progression evaluation. Clin Exp Med. 2015;15(1):97–105.
Berta J, et al. Apelin expression in human non-small cell lung cancer: role in angiogenesis and prognosis. J Thorac Oncol. 2010;5(8):1120–9.
Acknowledgments
This work was supported by National Natural Science Funds of China (Grant No. 81302058). This work was also supported by 2015 Harbin applied technology research and development projects (No. 2015RAXYJ059) and Haiyan Research Fund of The Affiliated Tumor Hospital of Harbin Medical University (No. JJZD2016-02). The funding body plays no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
Primary data are available on request.
Authors’ contributions
MF, HY, YQ and GY carried out the data collection, participated in the immunohistochemistry, cell culture and biological behavior analysis. KW and MF designed this study, performed the statistics and draft the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
N/A.
Ethics approval and consent to participate
Written consent was acquired from all participants who were fully informed of the experimental procedures during the period of research. The study protocol was approved by the ethics committee of the Affiliated Tumor Hospital of Harbin Medical University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Feng, M., Yao, G., Yu, H. et al. Tumor apelin, not serum apelin, is associated with the clinical features and prognosis of gastric cancer. BMC Cancer 16, 794 (2016). https://doi.org/10.1186/s12885-016-2815-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-016-2815-y