Abstract
Background
BRCA1 is a main component of homologous recombination and induces resistance to platinum in preclinical models. It has been studied as a potential predictive marker in lung cancer. Several proteins modulate the function of BRCA1. The E3 ubiquitin ligase HERC2 facilitates the assembly of the RNF8-UBC13 complex to recruit BRCA1 to DNA damage sites. The combined analysis of multiple components of the pathway leading to the recruitment of BRCA1 at DNA damage sites has the potentiality to improve the BRCA1 predictive model.
Methods
We retrospectively analyzed 71 paraffin-embedded tumor samples from advanced non-small-cell lung cancer patients treated with first-line platinum based chemotherapy and measured the mRNA expression levels of BRCA1, RNF8, UBC13 and HERC2 using real-time PCR. The mRNA expression was categorized using median value as cut-off point.
Results
The median progression-free survival of all 71 patients was 7.2 months whereas the median overall survival of the study population was 10.7 months. Among patients with low BRCA1 expression, the median PFS was 7.4 months in the presence of low HERC2 levels and 5.9 months for patients expressing high HERC2 levels (p = 0.01). The median OS was 15.3 months for patients expressing low levels of both genes and 7.4 months for those with low BRCA1 but high HERC2 (p = 0.008). The multivariate analysis showed that among patients with Eastern Cooperative Oncology Group performance status 0–1, the combined low expression of both BRCA1 and HERC2 clearly reduced the risk of progression (p = 0.03) and of death (p = 0.004).
Conclusions
These findings confirm the potentiality of integrated DNA repair components analysis in predicting the sensitivity to platinum in lung cancer. The study indicates a predictive role for HERC2 mRNA expression and paves the way for further refinement of the BRCA1 predictive model.
Similar content being viewed by others
Background
Platinum-based chemotherapy is currently the first-line treatment of choice for patients with advanced non-small-cell lung cancer (NSCLC) in the presence of wild-type epidermal growth factor receptor and non-rearranged ALK. However, no reliable predictive biomarkers of platinum resistance are currently available for routine clinical use. Breast cancer susceptibility gene 1 (BRCA1) plays a pivotal role in the repair of platinum-induced DNA damage and has been associated with cell resistance to platinum in preclinical models [1–3]. From the biological point of view, BRCA1 is involved in two main mechanisms of repair of platinum-induced DNA damage. The first one is nucleotide excision repair (NER), being the main pathway for the repair of helix-distorting DNA lesions [4, 5]. The second one is homologous recombination, an error-free mechanism for the repair of DNA double-strand breaks [6].
In clinical retrospective series, low mRNA expression of BRCA1 was associated with longer survival in NSCLC patients treated with cisplatin-based neoadjuvant chemotherapy [7], while the clinical feasibility of prospectively assessing BRCA1 mRNA expression was later demonstrated in a prospective phase II trial in advanced NSCLC patients [8]. Despite these encouraging preliminary results, a phase III randomized trial (NCT00617656/GECP-BREC) comparing non-biomarker-directed therapy with treatment based on the mRNA expression levels of BRCA1 and receptor-associated protein 80 (RAP80) was recently closed prematurely, since the interim analysis showed a detrimental effect in terms of progression free survival (PFS) in patients allocated to the experimental arm (hazard ratio [HR], 1.35; p = 0.03) [9, 10]. The protein RAP80 is a component of one of the BRCA1 complexes at DNA damage sites and may be essential in the assembly of the BRCA1-A complex at DNA damage sites [11]. Retrospective analyses had demonstrated that RAP80 mRNA expression could affect the predictive capacity of BRCA1 [8, 12].
However, several other DNA repair components are required for the recruitment and the function of BRCA1 in DNA repair [13, 14]. In particular, post-translational protein modification called ubiquitination is fundamental for the assembly of effector proteins complexes. After the phosphorylation of mediator of DNA damage checkpoint 1 (MDC1), RING finger ubiquitin ligase 8 (RNF8) is recruited at DNA damage sites and creates a complex with ubiquitin conjugating enzyme 13 (UBC13). This complex induces the formation of Lys 63-linked ubiquitin chains, which are essential for the assembly of BRCA1 complexes at double-strand breaks [15–17]. Recently, HECT domain and RCC1-like domain-containing protein 2 (HERC2), which functions as an E3-ubiquitin ligase, was shown to facilitate the formation of the RNF8-UBC13 complex [18] (Fig. 1). The protein HERC2 is also involved in regulating the stability of BRCA1 at DNA damage sites, since HERC2 ubiquitinates BRCA1 and targets it for degradation when BRCA1 is not in a complex with BRCA1-associated RING domain protein 1 (BARD1). The BRCA1-BARD1 heterodimer is required for BRCA1 stability, nuclear localization and E3 ligase function [19, 20]. This role of HERC2 is enhanced in the S-phase of the cell cycle, thus contributing to the modulation of BRCA1 function throughout the cell cycle and to the role of BRCA1 at the G2-M checkpoint [21].
The protein BRCA1 is recruited at DNA damage through a recognition mechanism implying the phosphorylation of histone H2AX and leading to the assembly of a protein complex that induces histones post-translational modification called ubiquitination. This protein complex includes the RING finger ubiquitin ligase 8 (RNF8), the conjugating enzyme 13 (UBC13) and the E3 ubiquiting ligase HECT domain-containing protein 2 (HERC2). The biological model of BRCA1 recruitment at DNA damage sites was used to select the genes to evaluate as potential predictive markers of platinum sensitivity in lung cancer
On the basis of this biological model, we hypothesized that RNF8, UBC13 and HERC2, being the main protagonists of ubiquitination process leading to BRCA1 recruitment at DNA damage sites, could modulate the predictive model based on BRCA1 expression.
Methods
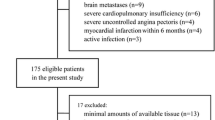
We retrospectively analyzed a series of 71 patients diagnosed with advanced NSCLC and treated with cisplatin or carboplatin plus gemcitabine or pemetrexed in the first-line setting (Table 1). Patients were selected according to first-line treatment, not including taxanes or vinca alkaloids, and availability of adequate tumor samples. No further clinical selection was performed. Radiological response was assessed using the Response Evaluation Criteria for Solid Tumor (RECIST) v 1.0 [22]. Progression free survival (PFS) was calculated from the beginning of first-line treatment until demonstrated radiological progression or death from any cause. The overall survival (OS) was calculated from the start of platinum-based chemotherapy to death from any cause.
Paraffin-embedded tumor specimens were collected before beginning chemotherapy and patients who had previously received radiotherapy were excluded. Tumor samples were evaluated by the pathologist to ensure a minimum of 90 % of tumor cells in analyzed samples. After mRNA extraction and retro transcription, the mRNA expression levels of BRCA1, RNF8, UBC13 and HERC2 were quantified using real-time PCR with a comparative method, as previously described [8]. mRNA levels were considered as categorical variables and dichotomized using the median value as cut-off point (Additional file 1: Supplementary Methods).
The median PFS and OS were estimated using the Kaplan-Meier method and compared with a two-sided log-rank test. Multivariate analyses were performed with the Cox regression method, with Eastern Cooperative Oncology Group (ECOG) performance status (PS) as covariate. All statistical analyses were performed using Statistical Package for Social Science (SPSS) for Windows version 17 (Chicago, IL, USA). Significance was set at p < 0.05.
Results and discussion
The clinical features of the study population are summarized in Table 1. Patients were mainly male (76 %), asymptomatic or poorly symptomatic at diagnosis (ECOG PS 0–1, 75 %), and current or former smokers (85 %). The prevalent histology was adenocarcinoma (60 %). First-line treatment was chosen according to standard clinical practice and did not include taxanes or vinca alkaloids (Table 1).
The expression of each gene was successfully analyzed in 87-96 % of patients (Additional file 2: Table S1).
The median PFS for all 71 patients was 7.2 months (95 % confidence interval, CI = 5.8-8.5) and the median OS was 10.7 months (95 % CI = 9.2-12.2) (Additional file 3: Figure S1). No differences in PFS or OS were observed according to the individual expression levels of any of the four genes.
Based on our previous experience [23], we then examined the potential predictive value of a two-gene model and analyzed PFS and OS according to the combination of BRCA1 with each of the three other genes. No significant differences were observed according to the combination of BRCA1 and UBC13 or of BRCA1 and RNF8 expression levels. However, the combination of BRCA1 and HERC2 identified subgroups of patients with different outcomes. Reliable quantification of mRNA was available for 55 patients. Among patients expressing low levels of BRCA1, the median PFS was 7.4 months (95 % CI = 4.5-10.4) for those expressing low HERC2 levels, compared to 5.9 months (95 % CI = 4.8-7.1) for patients with high HERC2 levels (p = 0.01) (Fig. 2a). The median OS was 15.3 months (95 % CI = 5.5-25.8) for patients expressing low BRCA1 and HERC2 and 7.4 months (95%CI = 5.1-9.7) for those with low BRCA1 but high HERC2 levels (p = 0.008) (Fig. 2b). Consistently, response rates were 42.9 % in patients expressing low levels of both BRCA1 and HERC2 and 28.6 % in those with low BRCA1 but high HERC2 levels. Progressive disease was recorded as best radiological response in 23.8 % and 42.9 % of patients, respectively (Additional file 4: Table S2). In contrast, HERC2 expression levels did not affect the outcome of patients expressing high levels of BRCA1 (Additional file 5: Figure S2).
To confirm the predictive value of this model, we assessed multivariate analysis and selected a more homogeneous population according to performance status (PS). Multivariate analyses showed that among patients with ECOG PS 0–1, high levels of either BRCA1 or HERC2 were associated with an increased risk of progression (HR, 1.4; 95 % CI = 1.1-4.73; p = 0.03) and death (HR, 3.7; 95 % CI = 1.54-9.1; p = 0.004) (Table 2), while among patients with PS 2, no significant differences according to BRCA1 and HERC2 levels were observed.
The identification of predictive markers of platinum sensitivity in lung cancer can help optimize the chemotherapy approach in advanced NSCLC patients. While a defective DNA damage repair capacity is associated with increased sensitivity to platinum, the translational application of this concept is rather difficult due to the complicated interplay among DNA repair pathways [13, 14]. The potential predictive roles of BRCA1 and excision repair cross-complementing 1 (ERCC1) have been widely studied in NSCLC [14, 24]. ERCC1 is a main component of NER, and low ERCC1 protein and mRNA expression have been associated with improved outcome in platinum-treated NSCLC patients, both in early-stage and in metastatic disease [14, 24]. However, neither BRCA1 nor ERCC1 expression was confirmed as a predictive marker in phase III studies [9, 25]. Nevertheless, our knowledge of DNA repair pathways is increasing, and a pivotal role has been demonstrated for post-translational modification in the response to double-strand breaks. In particular, the proteins UBC13 and RNF8, and more recently HERC2, are known to be essential for the recruitment of BRCA1 at DNA damage sites [13, 15–18].
The present study examined the hypothesis that the BRCA1 predictive model in advanced NSCLCs could be improved through the analysis of genes involved in the recruitment of BRCA1 at DNA damage sites through post-translational modifications (Fig. 1). In a retrospective, clinically homogeneous series of patients, we have demonstrated that HERC2 mRNA expression provides additional predictive information when analyzed in conjunction with BRCA1. The outcome of patients expressing low BRCA1 mRNA was significantly different according to HERC2 mRNA expression and the median OS in patients expressing low levels of both BRCA1 and HERC2 was 15.3 months, which is greatly superior to that observed in unselected patients treated with platinum-based therapy (rarely exceeding 10 months) [26]. Moreover, a significantly increased risk both of progression and of death was associated with high expression of either BRCA1 or HERC2 with Cox regression analysis.
These findings lend support to the integrated analysis of several DNA repair components, which can provide enhanced results compared to the analysis of one component alone. Moreover, our results show the important role of HERC2 in determining platinum sensitivity in patients with low BRCA1 expression, which is consistent with its known role in the recruitment of BRCA1 at DNA damage sites [18].
The main limitations of the study are its retrospective nature and the relatively small number of patients with mRNA expression data available for both BRCA1 and HERC2. Due to the number of patients, we cannot draw definitive conclusions about the absence of predictive value of UBC13 and RNF8 in combination with BRCA1 or of each gene when considered in isolation. In addition, mRNA expression data could not able to mirror the protein function and a validation through analyses of these markers at protein level could further increase the interest of these data. However, mRNA analysis is one of the most used surrogate marker of DNA repair capacity, taking into account the great difficulties in measuring DNA repair capacity at functional level. From the practical point of view, the need of highly experienced laboratories is one main limitation to the use of mRNA quantitative expression, while the possibility of testing more candidate markers is one strength point that could be particularly useful when studying a complex molecular pathway and the interplay of different components of the pathway.
Further development of this research would be the validation of the findings in a larger series of patients and the inclusion of a validation set of patients treated without platinum in order to test the hypothesis of a prognostic effect for the studied model. Finally the data should be confirmed prospectively.
Conclusions
In our study population, integrated mRNA analysis of BRCA1 and HERC2 shows a predictive role in advanced NSCLC patients treated with first-line platinum-based chemotherapy. The patients expressing low levels of both genes achieved better outcome to platinum, while isolated analysis of BRCA1 does not carry predictive value. Despite the limitations of the study, our results identify a new potential predictive marker, HERC2, and further refine the BRCA1 predictive model. Importantly, our findings support and pave the way for additional biomarker analyses, potentially useful for customizing chemotherapy in lung cancer.
Ethics approval and consent to participate
Ethical approval has been obtained at each Institution participating in the trial. In particular, patients from Sant Pau Hospital, Alicante General Hospital and Cluzeau Hospital were enrolled in EURTAC clinical trail, all the included patients signed informed consent approved both by the coordinating center of the prospective trial and by each local ethics committee (Sant Pau Hospital, Alicante General Hospital, Cluzeau Hospital). The consent forms used for patients treated at the Istituto Oncologico Veneto were presented and approved by the Ethics Committee of Azienda Ospedaliera in Padova and the local Institutional Review Board (IRB) has reviewed the study and waived the need for formal ethic approval.
All the patients have signed a written informed consent form, approved at each local IRB.
Abbreviations
- BARD1:
-
BRCA1-associated RING domain protein 1
- BRCA1:
-
breast cancer susceptibility gene 1
- CI:
-
confidence interval
- ECOG:
-
Eastern Cooperative Oncology Group
- ERCC1:
-
excision repair cross complementing 1
- HERC2:
-
HECT domain and RCC1-like domain-containing protein 2
- HR:
-
hazard ratio
- MDC1:
-
mediator of DNA damage checkpoint 1
- NER:
-
nucleotide excision repair
- NSCLC:
-
non-small-cell lung cancer
- OS:
-
overall survival
- PFS:
-
progression-free survival
- PS:
-
performance status
- RAP80:
-
receptor-associated protein 80
- RNF8:
-
RING finger ubiquitin ligase 8
- UBC13:
-
ubiquitin conjugating enzyme 13
References
Bhattacharyya A, Ear US, Koller BH, Weichselbaum RR, Bishop DK. The breast cancer susceptibility gene BRCA1 is required for subnuclear assembly of Rad51 and survival following treatment with the DNA cross-linking agent cisplatin. J Biol Chem. 2000;275(31):23899–903.
Husain A, He G, Venkatraman ES, Spriggs DR. BRCA1 up-regulation is associated with repair-mediated resistance to cis-diamminedichloroplatinum(II). Cancer Res. 1998;58(6):1120–3.
Quinn JE, Kennedy RD, Mullan PB, Gilmore PM, Carty M, Johnston PG, Harkin DP. BRCA1 functions as a differential modulator of chemotherapy-induced apoptosis. Cancer Res. 2003;63(19):6221–8.
Le Page F, Randrianarison V, Marot D, Cabannes J, Perricaudet M, Feunteun J, Sarasin A. BRCA1 and BRCA2 are necessary for the transcription-coupled repair of the oxidative 8-oxoguanine lesion in human cells. Cancer Res. 2000;60(19):5548–52.
Abbott DW, Thompson ME, Robinson-Benion C, Tomlinson G, Jensen RA, Holt JT. BRCA1 expression restores radiation resistance in BRCA1-defective cancer cells through enhancement of transcription-coupled DNA repair. J Biol Chem. 1999;274(26):18808–12.
Kennedy RD, Quinn JE, Johnston PG, Harkin DP. BRCA1: mechanisms of inactivation and implications for management of patients. Lancet. 2002;360(9338):1007–14.
Taron M, Rosell R, Felip E, Mendez P, Souglakos J, Ronco MS, Queralt C, Majo J, Sanchez JM, Sanchez JJ, et al. BRCA1 mRNA expression levels as an indicator of chemoresistance in lung cancer. Hum Mol Genet. 2004;13(20):2443–9.
Rosell R, Perez-Roca L, Sanchez JJ, Cobo M, Moran T, Chaib I, Provencio M, Domine M, Sala MA, Jimenez U, et al. Customized treatment in non-small-cell lung cancer based on EGFR mutations and BRCA1 mRNA expression. PLoS One. 2009;4(5), e5133.
Moran T, Cobo M, Domine M, Sanchez-Ronco M, Bover I, Provencio M, Massutti B, Vergnenegre A, Lopez-Vivanco G, Robinet G, et al. Interim analysis of the Spanish Lung Cancer Group (SLCG) BRCA1-RAP80 Expression Customization (BREC) randomized phase III trial of customized therapy in advanced non-small cell lung cancer (NSCLC) patients (p) (NCT00617656/GECP-BREC). J Clin Oncol. 2013;31(suppl; abstr):LBA8002.
Moran T, Wei J, Cobo M, Qian X, Domine M, Zou Z, Bover I, Wang L, Provencio M, Yu L, et al. Two biomarker-directed randomized trials in European and Chinese patients with nonsmall-cell lung cancer: the BRCA1-RAP80 Expression Customization (BREC) studies. Ann Oncol. 2014;25(11):2147–55.
Yan J, Kim YS, Yang XP, Li LP, Liao G, Xia F, Jetten AM. The ubiquitin-interacting motif containing protein RAP80 interacts with BRCA1 and functions in DNA damage repair response. Cancer Res. 2007;67(14):6647–56.
Bonanno L, Costa C, Majem M, Favaretto A, Rugge M, Rosell R. The predictive value of BRCA1 and RAP80 mRNA expression in advanced non-small-cell lung cancer patients treated with platinum-based chemotherapy. Ann Oncol. 2013;24(4):1130–2.
Harper JW, Elledge SJ. The DNA damage response: ten years after. Mol Cell. 2007;28(5):739–45.
Bonanno L. Predictive models for customizing chemotherapy in advanced non-small cell lung cancer (NSCLC). Transl Lung Cancer Res. 2013;2(3):160–71.
Kolas NK, Chapman JR, Nakada S, Ylanko J, Chahwan R, Sweeney FD, Panier S, Mendez M, Wildenhain J, Thomson TM, et al. Orchestration of the DNA-damage response by the RNF8 ubiquitin ligase. Science. 2007;318(5856):1637–40.
Mailand N, Bekker-Jensen S, Faustrup H, Melander F, Bartek J, Lukas C, Lukas J. RNF8 ubiquitylates histones at DNA double-strand breaks and promotes assembly of repair proteins. Cell. 2007;131(5):887–900.
Huen MS, Grant R, Manke I, Minn K, Yu X, Yaffe MB, Chen J. RNF8 transduces the DNA-damage signal via histone ubiquitylation and checkpoint protein assembly. Cell. 2007;131(5):901–14.
Bekker-Jensen S, Rendtlew Danielsen J, Fugger K, Gromova I, Nerstedt A, Lukas C, Bartek J, Lukas J, Mailand N. HERC2 coordinates ubiquitin-dependent assembly of DNA repair factors on damaged chromosomes. Nat Cell Biol. 2010;12(1):80–6. sup pp 81–12.
Joukov V, Chen J, Fox EA, Green JB, Livingston DM. Functional communication between endogenous BRCA1 and its partner, BARD1, during Xenopus laevis development. Proc Natl Acad Sci U S A. 2001;98(21):12078–83.
Brzovic PS, Keeffe JR, Nishikawa H, Miyamoto K, Fox 3rd D, Fukuda M, Ohta T, Klevit R. Binding and recognition in the assembly of an active BRCA1/BARD1 ubiquitin-ligase complex. Proc Natl Acad Sci U S A. 2003;100(10):5646–51.
Wu W, Sato K, Koike A, Nishikawa H, Koizumi H, Venkitaraman AR, Ohta T. HERC2 is an E3 ligase that targets BRCA1 for degradation. Cancer Res. 2010;70(15):6384–92.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
Bonanno L, Costa C, Majem M, Sanchez JJ, Gimenez-Capitan A, Rodriguez I, Vergnenegre A, Massuti B, Favaretto A, Rugge M, et al. The predictive value of 53BP1 and BRCA1 mRNA expression in advanced non-small-cell lung cancer patients treated with first-line platinum-based chemotherapy. Oncotarget. 2013;4(10):1572–81.
Martin LP, Hamilton TC, Schilder RJ. Platinum resistance: the role of DNA repair pathways. Clin Cancer Res. 2008;14(5):1291–5.
Bepler G, Williams C, Schell MJ, Chen W, Zheng Z, Simon G, Gadgeel S, Zhao X, Schreiber F, Brahmer J, et al. Randomized International Phase III Trial of ERCC1 and RRM1 Expression-Based Chemotherapy Versus Gemcitabine/Carboplatin in Advanced Non-Small-Cell Lung Cancer. J Clin Oncol. 2013;31(19):2404–12.
Schiller JH, Harrington D, Belani CP, Langer C, Sandler A, Krook J, Zhu J, Johnson DH. Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N Engl J Med. 2002;346(2):92–8.
Acknowledgements
Work in Dr. Rafael Rosell’s laboratory was partially supported by a grant from “La Caixa Foundation”. The Foundation had no role in the design of the study, the interpretation of the data or decision for publication.
We thank Renée O’Brate, assistant of Dr. Rosell, for reviewing the language of the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
The authors have no competing interests to declare. The study was performed in collaboration with Pangaea Biotech as part of an internship with no commercial implications, and Pangaea Biotech played no part in study design or choice of publication.
Authors’ contributions
LB and RR conceived the research, interpreted the data and wrote the manuscript; LB, CC and AGC designed and performed molecular analyses; LB, MM, AV, BM, AF and CP treated patients and provided clinical data; JJS and IR performed the statistical analyses; MA M-V and MT supervised the molecular analyses; MR provided tumor samples and pathological revision. All the authors have read and approved the final manuscript.
Additional files
Additional file 1:
Supplementary Methods. Additional information on gene expression analyses. (DOCX 21 kb)
Additional file 2: Table S1.
Results of gene expression analyses in the study population (71 patients). (DOCX 11 kb)
Additional file 3: Figure S1.
The median progression-free and overall survival for all 71 patients. (DOCX 108 kb)
Additional file 4: Table S2.
Best radiological response in patients expressing low levels of BRCA1 according to HERC2 levels. (DOCX 10 kb)
Additional file 5: Figure S2.
The effect of HERC2 mRNA expression on the outcome of patients expressing high levels of BRCA1. (DOCX 198 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Bonanno, L., Costa, C., Majem, M. et al. Combinatory effect of BRCA1 and HERC2 expression on outcome in advanced non-small-cell lung cancer. BMC Cancer 16, 312 (2016). https://doi.org/10.1186/s12885-016-2339-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-016-2339-5