Abstract
ᅟ
The overall purpose of this study is to provide proof of concept for introducing the anthracycline epirubicin as an effective, biomarker-guided treatment for metastatic colorectal cancer (mCRC) patients who are refractory to treatment with oxaliplatin-based chemotherapy and have TOP2A gene amplification in their tumor cells.
Background
Epirubicin is an anthracycline that targets DNA topoisomerase 2-α enzyme encoded by the TOP2A gene. It is used for treatment of several malignancies, but currently not in CRC. TOP2A gene amplifications predict improved efficacy of epirubicin in patients with breast cancer and thus could be an alternative option for patients with CRC and amplified TOP2A gene. We have previously analysed the frequency of TOP2A gene aberrations in CRC and found that 46.6 % of these tumors had TOP2A copy gain and 2.0 % had loss of TOP2A when compared to adjacent normal tissue. The TOP2A gene is located on chromosome 17 and when the TOP2A/CEN-17 ratio was applied to identify tumors with gene loss or amplifications, 10.5 % had a ratio ≥ 1.5 consistent with gene amplification and 2.6 % had a ratio ≤ 0.8 suggesting gene deletions. Based on these observations and the knowledge gained from treatment of breast cancer patients, we have initiated a prospective clinical, phase II protocol using epirubicin (90 mg/m2 iv q 3 weeks) in mCRC patients, who are refractory to treatment with oxaliplatin.
Methods/Design
The study is an open label, single arm, phase II study, investigating the efficacy of epirubicin in patients with oxaliplatin refractory mCRC and with a cancer cell TOP2A/CEN-17 ratio ≥ 1.5. TOP2A gene amplification measured by fluorescence in situ hybridization. A total of 25 evaluable patients (15 + 10 in two steps) will be included (Simon’s two-stage minimax design). Every nine weeks, response is measured by computed tomography imaging and evaluated according to RECIST 1.1. The primary end-point of the study is progression-free survival.
Trial registration
Eudract no. 2013-001648-79.
Similar content being viewed by others
Background
Colorectal cancer (CRC) is a major health problem since it is among the five most prevalent cancers [1, 2]. Over the last decade, the use of novel treatment modalities and complex treatment strategies in terms of optimized surgery, adjuvant chemotherapy, and novel targeted biological agents have contributed to significant improvement of outcome of the entire population of patients with CRC. However, only three cytotoxic drugs (fluorouracil (5-FU), oxaliplatin and irinotecan) are recommended as standard treatment in patients with metastatic CRC (mCRC). In Europe, the routine clinical management of patients with primary CRC involves adjuvant treatment with 5-FU/Leucovorin (LV) and oxaliplatin (FOLFOX, FLOX or XELOX) given to high-risk patients [3–6]. In the treatment of mCRC, patients who have yet not received oxaliplatin will often be offered FOLFOX, FLOX or XELOX, followed by 5-FU/LV and irinotecan (FOLFIRI, FLIRI or XELIRI) at progression, or vice versa [7–10]. Chemotherapy may be combined with the EGF-receptor targeting antibodies cetuximab or panitumumab in patients with RAS wild type tumors [11–14], while patients with RAS mutated tumors often will receive the VEGF targeting antibody bevacizumab [15, 16]. The objective response rate to first-line systemic treatment of mCRC patients approximates 50 % [10, 17]. However, only 10 % of mCRC patients will obtain objective response during second-line treatment [10], suggesting that there is a high degree of cross-resistance between the used drugs. Improvements in mCRC treatment may be achieved through the development of novel drugs with new molecular mechanisms of action and thus lack of cross-resistance with currently used drugs. However, drug development is expensive (estimated cost is 1 Bill USD per drug), takes a long time (12–15 years) and the risk of failure in late stage clinical trials is extremely high. An alternative to the drug development approach is to search for novel predictive biomarkers that can guide personalized treatment and thereby select the right drug for the right patient at the right time. Using predictive biomarkers will increase the therapeutic index and avoid side effects among the many patients who will not benefit from the treatment. A third way to address these medical problems is to test whether drugs being used in some other cancer types might have beneficial effects also in CRC. However, with an expected relatively low response rate, such drugs should only be used together with companion diagnostics allowing for a pre-treatment selection of patients with the highest likelihood of obtaining benefit from the treatment. This third approach is called biomarker guided repurposing and is the foundation for the present protocol, where we investigate whether epirubicin has a beneficial effect in oxaliplatin resistant mCRC patients with TOP2A gene amplification.
Epirubicin and TOP2A
The anthracycline epirubicin exerts its antitumor effects by interference with the synthesis and function of DNA and is most active in the S-phase of the cell cycle [18]. It is metabolized in the liver and primarily eliminated in the bile. The main molecular target of epirubicin is the DNA topoisomerase 2-α enzyme (Top2α) that plays a key role in maintaining the topological status of chromosomes during DNA replication and transcription. During DNA transcription, Top2α removes DNA supercoiling, and at the end of DNA replication, Top2α is essential for chromosome condensation and segregation. In this process, Top2α reversibly binds and cleaves both complementary DNA strands forming what is called a Top2 cleaving complex (Top2cc). Epirubicin leads to entrapment of Top2α in the Top2CC and thereby prevents religation of the cleaved DNA strands, which ultimately leads to DNA damage. Apart from this, epirubicin also interferes with a broad range of DNA processes through DNA intercalation [19].
TOP2A amplification predicts improved efficacy to epirubicin in patients with breast cancer [20, 21] and thus could be an alternative option to irinotecan-based therapy in patients with CRC and TOP2A amplification who relapsed on oxaliplatin containing chemotherapy. We have previously established irinotecan (SN-38, the active metabolite of irinotecan) resistant CRC cell lines, and these CRC cells were also resistant to epirubicin [22]. In contrast, our SN-38 resistant CRC cells were also resistant to epirubicin whereas our oxaliplatin resistant CRC cell lines retained sensitivity to epirubicin [Niel Frank Jensen et al. Unpublished observations]. In another study we analysed the frequency of TOP2A aberrations in CRC tissue from 153 primary stage III CRC tumors and found that 46.6 % had TOP2A copy gain and 2.0 % TOP2A loss, when compared to adjacent normal tissue [23]. When the TOP2A/CEN-17 ratio was applied to identify tumors with gene loss or amplifications, 16 (10.5 %) had a ratio ≥ 1.5, consistent with gene amplification and 4 (2.6 %) had a ratio ≤ 0.8, suggesting gene deletion.
Design/methods
Design
The study is an open label, single arm, phase II study, investigating the efficacy of epirubicin in patients with oxaliplatin refractory mCRC and a cancer cell TOP2A/CEN-17 ratio ≥ 1.5. A second aim is the collection of relevant tumor and blood material for subsequent biomarker studies.
Inclusion criteria
To be eligible for inclusion, patients must provide written informed consent. All patients must be above the age of 18 years, have WHO performance status 0–2, and a life expectancy of at least 3 months. Furthermore, patients must have histologically verified, non-resectable, oxaliplatin resistant mCRC i.e. progression during or after oxaliplatin-based therapy (at least 2 months of oxaliplatin-based palliative therapy or at least 4 months of adjuvant oxaliplatin-based therapy). Moreover, FFPE tumor tissue blocks (primary tumor biopsy/resection specimen or biopsy/resection specimen from a metastatic lesion) must be available for fluorescence in situ hybridization (FISH) analysis of the TOP2A/CEN-17 ratio and this ratio has to be ≥ 1.5.
Treatment
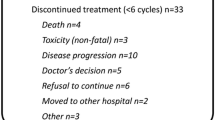
Drug/dosage: Epirubicin 90 mg/m2 day 1 administration via fast running infusion of 0.9 % sodium chloride every 21-day. Treatment will continue until maximum cumulative dose of Epirubicin = 900 mg/m2, unacceptable toxicity, progressive disease at computer tomography (CT) scan according to RECIST version 1.1 or patients wish of ending treatment. Before start of treatment a baseline CT scan will be performed, and a new CT scan will be performed after every third series of epirubicin to monitor treatment response.
Ethics
The study will be conducted in compliance with the protocol and in accordance with the ethical principles put forward in the second Declaration of Helsinki and in accordance with good clinical practice (GCP) rules. The trial was approved by the Ethics Committee of Region Syddanmark (2013-001648-79/ S-20130042) and by the Danish Medical Authority (Eudract no. 2013-001648-79).
Study objectives
The primary end-point of the study is progression-free survival (PFS), defined as time from the first infusion of epirubicin to the first documented disease progression, according to RECIST version 1.1. Secondary end-points include overall survival (OS), response rate (RR), toxicity, and validation of tissue inhibitor of metalloproteinase-1 (TIMP-1) measured in plasma and immunohistochemically in tumor tissue, as biomarker for anthracycline sensitivity/resistance [24]. Additionally, the relationship between TOP2A and TOP1 gene amplifications will be studied [25].
Statistics
The number of evaluable patients (the sample size) is based on Simon’s two stages Mini-max design [26]. This design ensures early study termination if there is insufficient effect. Patients will be evaluated with CT scans every 9 weeks. In randomized trials on second-line therapy, PFS is around 4 months. A tumor control rate less than 10 % after 4 months (at the time of the second evaluation CT scan) is not clinically relevant. Assuming a significance level at 0.05 (α = 0.05) and a power at 80 % (β = 0.20) it can be calculated, that 15 patients should be included in the first part of the study. The enrolment will continue until 15 patients have completed the second CT scan or experienced progressive disease. If none out of the first 15 consecutive patients achieve stable disease at the second CT scan (i.e. after 6 courses of epirubicin), we will reject our hypotheses and close the study after the first stage of accrual. If one or more patients achieve tumor control (partial response or stable disease) at the second scan, an additional 10 patients will be accrued in the second stage. If 5 out of 25 patients achieve tumor control after six courses of therapy, a tumor control rate of 30 % cannot be rejected, and it will be concluded that the treatment is effective enough to continue with future studies.
We will use non-parametric methods for calculation of patient characteristics, side effects and disease control. PFS and OS will be calculated and reported as median survival (Kaplan-Meier method).
Methods
The TOP2A FISH pharmDx™ Kit (Dako, Glostrup, Denmark) will be used according to the manufacturer’s instructions, as previously reported [23]. For every patient tumor sample, TOP2A and CEN-17 signals will be counted in 60 non-overlapping malignant cells, and a TOP2A/CEN-17 ratio will be calculated as the total counted number of TOP2A signals divided by the total counted number of CEN-17 signals. TOP2A FISH analysis will be performed on archived FFPE tumor tissues obtained from either the primary tumor (at time of diagnosis or obtained from the surgical resection specimen) or from a metastatic lesion (biopsy or resection specimen).
Discussion
The number of treatment options in patients with mCRC is still very limited. Response rates decrease dramatically with time, while the patients proceed in the treatment lines. New and non-cross resistant treatment options are urgently needed, and biomarkers predictive of response to chemotherapeutic treatments are totally lacking. Studies on breast cancer patients indicate that amplification and possibly deletion of TOP2A is predictive of response to epirubicin [20, 21]. Data on TOP2A aberrations in CRC are sparse, with reported TOP2A amplification rates ranging from 2.2 to 46.6 % in studies using different analytical methods [23, 27, 28]. In a study of the frequency of TOP2A gene aberrations in CRC tissue, we found that a total of 10.5 % of the patients had a TOP2A/CEN-17 ratio ≥ 1.5, which is compatible with TOP2A amplification [23]. Previous studies have investigated the effect of epirubicin in the entire unselected group of patients with mCRC, but found that this treatment had lower impact than oxaliplatin- or irinotecan-based treatment options [18, 29–31]. Taken together, those data led to the hypothesis that re-purposing epirubicin to patients with mCRC and TOP2A gene amplification may represent a valid treatment offer to a subset of mCRC patients. Hence, the aim of this clinical study is to take a further step towards personalized mCRC treatment. If epirubicin should prove to be effective in patients with increased TOP2A gene copy numbers, this may lead to a novel personalized treatment option for patients with mCRC.
This study differs from the standard treatment strategy for mCRC, where the patients often will be offered irinotecan-based therapy after failure to oxaliplatin-based therapy or vice versa. Median PFS of this standard treatment is approximately 2 months, and 75 % of the patients will experience progressive disease after 4 months of treatment [10]. In the present phase II protocol with pre-selected patients, we expect that 30 % will have objective response after the first 4 months of treatment, thereby achieving an increased median PFS. All patients will be evaluated every 9 weeks, enabling a quick change in treatment strategy if a patient experiences disease progression during epirubicin treatment [32, 33]. Carefully planned and closely monitored “window of opportunity” phase II studies are feasible and ethically acceptable in mCRC patients, and may have the advantage to determine potential efficacy of novel agents without placing the patients at risk. In the present study, close monitoring of efficacy every 9 weeks will ensure that this novel treatment line with epirubicin will be offered without further delay in case of progression during epirubicin treatment, with respect to any future treatment option.
The statistical basis for the protocol is based on the fact that we expect a response rate of 30 % in this sub-population of patients with TOP2A aberrations, which is significantly better than the typical second line treatment these patients will be offered, which usually has response rates of 10 %. In conclusion, if the objectives of this study protocol are met, the expected 10 % of mCRC patients with a TOP2A/CEN-17 ratio ≥ 1.5 will be offered an extra line of effective treatment, which may lead to an overall improved survival in this subgroup of mCRC patients.
Trial status
A total of 120 patients have been screened for TOP2A levels and we have found 14 patients (12 %) to have a TOP2A/CEN-17 ratio ≥ 1.5 in primary tumor, a metastatic lesion or both. To date 3 patients have been included and initiated treatment with epirubicin.
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127(12):2893–917.
Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013;49(6):1374–403.
Andre T, Boni C, Mounedji-Boudiaf L, Navarro M, Tabernero J, Hickish T, et al. Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med. 2004;350(23):2343–51.
Andre T, Boni C, Navarro M, Tabernero J, Hickish T, Topham C, et al. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol. 2009;27(19):3109–16.
Haller DG, Tabernero J, Maroun J, de Braud F, Price T, Van Cutsem E, et al. Capecitabine plus oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J Clin Oncol. 2011;29(11):1465–71.
Kuebler JP, Wieand HS, O’Connell MJ, Smith RE, Colangelo LH, Yothers G, et al. Oxaliplatin combined with weekly bolus fluorouracil and leucovorin as surgical adjuvant chemotherapy for stage II and III colon cancer: results from NSABP C-07. J Clin Oncol. 2007;25(16):2198–204.
Douillard JY, Cunningham D, Roth AD, Navarro M, James RD, Karasek P, et al. Irinotecan combined with fluorouracil compared with fluorouracil alone as first-line treatment for metastatic colorectal cancer: a multicentre randomised trial. Lancet. 2000;355(9209):1041–7.
Kohne CH, van Cutsem E, Wils J, Bokemeyer C, El-Serafi M, Lutz MP, et al. Phase III study of weekly high-dose infusional fluorouracil plus folinic acid with or without irinotecan in patients with metastatic colorectal cancer: European Organisation for Research and Treatment of Cancer Gastrointestinal Group Study 40986. J Clin Oncol. 2005;23(22):4856–65.
Saltz LB, Cox JV, Blanke C, Rosen LS, Fehrenbacher L, Moore MJ, et al. Irinotecan plus fluorouracil and leucovorin for metastatic colorectal cancer. Irinotecan Study Group. N Engl J Med. 2000;343(13):905–14.
Tournigand C, Andre T, Achille E, Lledo G, Flesh M, Mery-Mignard D, et al. FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GERCOR study. J Clin Oncol. 2004;22(2):229–37.
Douillard JY, Siena S, Cassidy J, Tabernero J, Burkes R, Barugel M, et al. Randomized, phase III trial of panitumumab with infusional fluorouracil, leucovorin, and oxaliplatin (FOLFOX4) versus FOLFOX4 alone as first-line treatment in patients with previously untreated metastatic colorectal cancer: the PRIME study. J Clin Oncol. 2010;28(31):4697–705.
Tveit KM, Guren T, Glimelius B, Pfeiffer P, Sorbye H, Pyrhonen S, et al. Phase III Trial of Cetuximab With Continuous or Intermittent Fluorouracil, Leucovorin, and Oxaliplatin (Nordic FLOX) Versus FLOX Alone in First-Line Treatment of Metastatic Colorectal Cancer: The NORDIC-VII Study. J Clin Oncol. 2012;30(15):1755–62.
Van Cutsem E, Kohne CH, Hitre E, Zaluski J, Chang Chien CR, Makhson A, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med. 2009;360(14):1408–17.
Van Cutsem E, Kohne CH, Lang I, Folprecht G, Nowacki MP, Cascinu S, et al. Cetuximab plus irinotecan, fluorouracil, and leucovorin as first-line treatment for metastatic colorectal cancer: updated analysis of overall survival according to tumor KRAS and BRAF mutation status. J Clin Oncol. 2011;29(15):2011–9.
Arnold D, Andre T, Bennouna J, Sastre J, Oesterlund PJ, Greil R, Van Cutsem E, Von Moos R, Reyes-Rivera I, Bendahmane B, Kubicka S: Bevacizumab (BEV) plus chemotherapy (CT) continued beyond first progression in patients with metastatic colorectal cancer (mCRC) previously treated with BEV plus CT: Results of a randomized phase III intergroup study (TML study). ASCO abstract CRA3503 2012.
Saltz LB, Clarke S, Diaz-Rubio E, Scheithauer W, Figer A, Wong R, et al. Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol. 2008;26(12):2013–9.
Schmoll HJ, Van Cutsem E, Stein A, Valentini V, Glimelius B, Haustermans K, et al. ESMO Consensus Guidelines for management of patients with colon and rectal cancer. A personalized approach to clinical decision making. Ann Oncol. 2012;23(10):2479–516.
Plosker GL, Faulds D. Epirubicin. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic use in cancer chemotherapy. Drugs. 1993;45(5):788–856.
Pommier Y, Leo E, Zhang HL, Marchand C. DNA Topoisomerases and Their Poisoning by Anticancer and Antibacterial Drugs. Chem Biol. 2010;17(5):421–33.
Di Leo A, Desmedt C, Bartlett JMS, Piette F, Ejlertsen B, Pritchard KI, et al. HER2 and TOP2A as predictive markers for anthracycline-containing chemotherapy regimens as adjuvant treatment of breast cancer: a meta-analysis of individual patient data. Lancet Oncol. 2011;12(12):1134–42.
Du YY, Zhou Q, Yin WJ, Zhou LH, Di GH, Shen ZZ, et al. The role of topoisomerase II alpha in predicting sensitivity to anthracyclines in breast cancer patients: a meta-analysis of published literatures. Breast Cancer Res Treat. 2011;129(3):839–48.
Jensen NF, Stenvang J, Beck MK, Hanakova B, Belling KC, Do KN, et al. Establishment and characterization of models of chemotherapy resistance in colorectal cancer: Towards a predictive signature of chemoresistance. Mol Oncol. 2015.
Nygard SB, Christensen IJ, Smith DH, Nielsen SL, Jensen NF, Nielsen HJ, et al. Underpinning the repurposing of anthracyclines towards colorectal cancer: assessment of topoisomerase II alpha gene copy number alterations in colorectal cancer. Scand J Gastroenterol. 2013;48(12):1436–43.
Ejlertsen B, Jensen MB, Nielsen KV, Balslev E, Rasmussen BB, Willemoe GL, et al. HER2, TOP2A, and TIMP-1 and responsiveness to adjuvant anthracycline-containing chemotherapy in high-risk breast cancer patients. J Clin Oncol. 2010;28(6):984–90.
Sonderstrup IM, Nygard SB, Poulsen TS, Linnemann D, Stenvang J, Nielsen HJ, et al. Topoisomerase-1 and -2A gene copy numbers are elevated in mismatch repair-proficient colorectal cancers. Mol Oncol. 2015;9(6):1207–17.
Simon R. Optimal two-stage designs for phase II clinical trials. Control Clin Trials. 1989;10(1):1–10.
Al-Kuraya K, Novotny H, Bavi P, Siraj AK, Uddin S, Ezzat A, et al. HER2, TOP2A, CCND1, EGFR and C-MYC oncogene amplification in colorectal cancer. J Clin Pathol. 2007;60(7):768–72.
Coss A, Tosetto M, Fox EJ, Sapetto-Rebow B, Gorman S, Kennedy BN, et al. Increased topoisomerase IIalpha expression in colorectal cancer is associated with advanced disease and chemotherapeutic resistance via inhibition of apoptosis. Cancer Lett. 2009;276(2):228–38.
Alberola V, Garcia Conde J, Jimeno J, Fernandez Martos C, Herranz C, Macheng I, et al. Phase II study with high doses of epirubicin in patients with advanced rectal cancer. Tumori. 1990;76(5):503–4.
Cersosimo RJ, Hong WK. Epirubicin: a review of the pharmacology, clinical activity, and adverse effects of an adriamycin analogue. J Clin Oncol. 1986;4(3):425–39.
Molinaro P, Lafleur F, Blum RH. A phase III randomized trial of epirubicin versus 5-fluorouracil in metastatic rectal/sigmoid adenocarcinoma. Am J Clin Oncol. 1989;12(4):332–4.
Glimelius B, Lahn M, Gawande S, Cleverly A, Darstein C, Musib L, et al. A window of opportunity phase II study of enzastaurin in chemonaive patients with asymptomatic metastatic colorectal cancer. Ann Oncol. 2010;21(5):1020–6.
Glimelius B, Spindler KL, Frodin JE, Berglund A, Bystrom P, Qvortrup C, et al. Long-term follow-up of chemonaive patients with asymptomatic metastatic colorectal cancer treated with enzastaurin in a window of opportunity phase II study. Ann Oncol. 2010;21(5):1127–8.
Acknowledgment
The staffs at The Department of Oncology and Pathology at Odense University Hospital are thanked for excellent assistance, and all the patients are thanked for their willingness to participate.
Funding
This work was supported by The Danish Cancer Society, grant number R72-A4686-I3-S2 (900.000 Danish kroner).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
LST, CQ, SBN, SLN, NFJ, JS, NB and PP collected the data underlying the study protocol. LST, CQ, SBN, JS, SD, NB and PP designed the study. LST, JS, NB and PP wrote the protocol. LST and PP handled ethics approval. LST, CQ, SD and PP are trial coordinators, responsible for evaluating FISH data and the daily running of the trial. LTS, CQ, SLN, DRA, JS, SD, NB and PP are responsible for inclusion and analyses of eligible patients. All authors contributed to and approved the final version of the manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tarpgaard, L.S., Qvortrup, C., Nygård, S.B. et al. A phase II study of Epirubicin in oxaliplatin-resistant patients with metastatic colorectal cancer and TOP2A gene amplification. BMC Cancer 16, 91 (2016). https://doi.org/10.1186/s12885-016-2124-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-016-2124-5