Abstract
Background
Globally, young women deliver at home, often under unhygienic conditions and without skilled birth attendants. This study identified the determinants of health facility delivery among young mothers in Ghana.
Methods
We analysed secondary data from the 2014 Ghana Demographic and Health Survey, which collected data across the former ten administrative regions of Ghana. This study analysed data from the ‘women file’ by adjusting for the sample weight. STATA/SE version 16 was employed to analyse the data by computing descriptive statistics, Chi-square, and Binary Logistic Regression.
Results
Seven in ten young mothers gave birth in a health facility. Young mothers who had secondary school education were over three-fold more likely to deliver in a health facility (AOR = 3.5, 95% CI: 1.33–9.23) compared with young mothers with no formal education. Young mothers who resided in rural areas had lower odds (73%) of delivering in a health facility (AOR = 0.27; 95% CI: 0.14–0.514) compared with those in urban areas. Young mothers within the richest wealth quintile also had higher odds (8 times) of delivering in a health facility (AOR = 8.24; 95% CI: 0.95–71.77) compared with those within the poorest wealth quintile. Young mothers who obtained four to seven antenatal visits (AOR = 0.53; 95% CI: 0.27–1.03) had lower odds of delivering in a health facility compared with those who obtained eight or more antenatal visits.
Conclusion
The majority of young mothers in Ghana gave birth in a health facility. The likelihood of delivering in a health facility was influenced by socio-demographic factors, economic factors and utilization of antenatal care services. Therefore, interventions aimed at increasing utilization of skilled delivery among young women should focus on promoting girl child education, economic status and antenatal care visits.
Similar content being viewed by others
Introduction
Maternal and newborn deaths are global health problems, but common in sub-Saharan Africa (SSA) [1, 2]. For instance, about two-thirds of global maternal deaths occur in SSA [1,2,3]. Reducing maternal and newborn mortalities remains a global health priority. For example, the Sustainable Development Goals, especially Target 3.1 seeks to reduce the global Maternal Mortality Rate (MMR) to less than 70 per 100,000 live births by 2030, while Target 3.2 seeks to end preventable deaths of newborns by 2030 [4]. Studies across the globe have shown that younger age is a major risk factor for maternal and newborn deaths [5, 6]. Young mothers (10–24 years) are at a higher risk of severe complications during childbirth, including infections and eclampsia [7]. Globally, pregnancy and childbirth complications are the top causes of mortality among mothers aged 15–19 years [8, 9]. Also, children born to young mothers are at a higher risk of death and severe neonatal conditions, preterm delivery, and being underweight [8, 10].
Health facility delivery or skilled birth attendance has proven to be an effective intervention in reducing maternal and newborn deaths. Health facilities have professional birth attendants (i.e. nurses, doctors, and midwives), infrastructure, logistics, and referral systems to help in the provision of quality health services during labour, delivery, and the postpartum period [11]. In addition, skilled birth attendants are trained to manage obstetric complications [12]. Yet, the utilization of skilled birth attendance among young mothers remains low in low and middle-income countries [13, 14]. For instance, a cross-sectional study in the Northern region of Ghana revealed that 22.1% of young women in rural areas and 36.7% of those in urban areas used skilled delivery services [15]. Factors associated with the utilization of skilled delivery include educational status, health insurance status, optimal antenatal care visits, and socioeconomic status. Other correlates include the place of residence, previous delivery, exposure to mass media, religion, and partners’ educational status [7, 16].
In Ghana, the maternal mortality rate in 2017 was estimated at 309 per 100,000 live births [17]. which is higher than the global target of less than 70 per 100,000 by 2030. In addition, teenage pregnancy remains a serious public health concern. In 2020 alone, 109,888 Ghanaian girls between the ages of 10–19 years were impregnated [18]. However, little is known about their place of delivery. Existing studies on skilled birth attendance focused on all women of reproductive age without age-specific estimates [19, 20]. However, young people have different healthcare needs and health-seeking behaviours, hence limiting the generalizability of findings from the adult population to the young population. The objectives of this study were to assess the prevalence of health facility delivery, and associated factors among mothers aged 15–24 years in Ghana, using national representative data. Findings from this study will help inform maternal health policies and programming, which can help reduce the burden of maternal and neonatal mortalities. We hypothesize that young mothers from poor households and rural areas are less likely to give birth in a health facility compared with their counterparts.
Methods
Source of data
This study analysed data from the 2014 Ghana Demographic and Health Survey (GDHS). The survey collected data across the former ten administrative regions of Ghana, using structured questionnaires, from both men and women in rural and urban areas. Women between the ages of 15–49 years were the target population. The study participants were selected using a two-stage sampling procedure. First, 427 clusters were selected from the updated version of the 2010 Population and Housing Census sampling frame. Second, about 30 households were selected from each cluster using a systematic sampling technique proportional to size. In all, 3150 women aged 15–24 years participated in the 2014 GDHS. This present study focused on women aged 15–24 years who had delivered in the last five years to the survey. Therefore, women who fell outside this criterion were excluded from the analysis. A weighted sample of 864 women aged 15–24 years was included in this analysis. The 2014 GDHS obtained written informed consent from the caregivers of minors (15–17 years) and adults. The survey received approval from the Ghana Health Service Ethics Review Committee. Further information about the 2014 GDHS is provided in the full report [21].
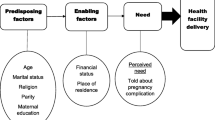
Measures
In this study, the main outcome was the place of delivery (where did you give birth?). This variable was recoded as (1 = health facility and 0 = home). The exposure variables found in the literature included socio-demographic factors, insurance coverage, utilization of antenatal care, exposure to mass media (frequency of reading newspaper/magazine, listening to radio, and watching television), and barriers to accessing healthcare. The socio-demographic variables included the following: age, educational status, marital status, wealth index, place of residence, geographical region, religion, employment status, partner’s educational status, health insurance coverage and distance to a health facility.
Statistical analysis
STATA/SE, version 16 (StataCorp, College Station, Texas, USA) was employed to analyse the data. Before the analysis, some variables (i.e. religion, age, marital study, employment status, and ANC visits) were recorded. The sampling weights, clustering, and stratification (complex survey design) were taken into consideration during the analysis by using the ‘svy’ STATA command, which fits statistical models for complex survey data by adjusting the results of a command for survey settings identified through ‘svyset’ [22]. Both descriptive statistics and inferential statistics were computed. At the univariate level, frequency and percentage were computed, while Chi-square analysis was computed at the bivariate level. Adjusted odds ratios were computed at the multivariable level employing binary logistic regression analysis. All statistical significance was reported at the 0.05 significance level.
Results
Descriptive statistics
The majority of the participants were aged 20–24 years (79%), married (63%), and resided in rural areas (61%). More than half of the participants professed Christianity (78%). Also, six in ten participants were employed and 62% were covered by health insurance. Exactly, 71% had no distance-related problem in accessing health services. Regarding exposure to mass media, the majority of the participants did not read a newspaper (90%), 19% did not listen to radio and 27% did not watch television. In addition, the majority of the participants obtained between 4 to 7 antenatal visits (60%). Exactly, 75% of the participants delivered in a health facility, while 25% delivered at home (Table 1).
Association between participant characteristics and health facility delivery
A statistically significant association was found between educational status, wealth quintile and area of residence, and health facility delivery (p < 0.05). In addition, geographical region, religion, health insurance status, partner’s educational status and distance to health facility were associated with health facility delivery (p < 0.05). Exposure to mass media was associated with health facility delivery (p < 0.05). Young mothers in the Upper East Region had the highest prevalence of health facility delivery (91%). Home delivery was common among participants in the Northern Region (60%), those who professed Traditional religion (72%), and those who obtained zero ANC visit (84%) (Table 2).
Predictors of health facility delivery
Participants who had secondary school education had higher odds of giving birth in a health facility (AOR = 3.5, 95% CI: 1.33–9.23) compared to participants with no formal education. Participants residing in rural areas (AOR = 0.27; 95% CI: 0.14–0.514) had lesser odds of giving birth in a health facility compared with participants in urban areas. We also found that participants in the richest wealth quintile (AOR = 8.24; 95% CI: 0.95–71.77) had higher odds of giving birth in a health facility compared with those within the poorest wealth quintile. Also, participants who obtained zero ANC visits (AOR = 0.00; 95% CI: 0.00–0.01) had lesser odds of accessing skilled delivery services compared with those who obtained 8 or more ANC visits. Participants in the Upper East region (AOR = 8.44; 95% CI: 2.33–30.55) had higher odds of giving birth in a health facility compared with those in the Western region (Table 3).
Discussion
The results showed that 75% of the participants gave birth in a health facility. The prevalence of health facility delivery in this study is higher than what previous studies found in Nigeria (33.7%) [23] and rural India (46%) [24]. The difference in findings can be attributed to the implementation of the Free Maternal Health Care Policy in Ghana. With this policy, pregnant women can enrol on the National Health Insurance Scheme (NHIS) free of charge. Subscribers of the NHIS can access maternal health services, including skilled delivery services, free of charge [25]. Further, persons below the age of 18 years are exempted from paying the NHIS premium. There is evidence to show that the implementation of the NHIS has led to an improvement in the utilization of maternal health services [26].
Notwithstanding, a considerable proportion (25%) of young mothers delivered at home. Home delivery predisposes the mother and the new born to a high risk of infections and death during and after delivery. Home delivery is also associated with late initiation of breastfeeding and inadequate postnatal checks for the mother and the child [27]. Although skilled delivery service is free in Ghana, young mothers may still face some financial constraints, such as transportation costs. Also, evidence shows that insured persons in Ghana make unapproved payments when accessing health services (including maternal and child care services) in NHIS accredited health facilities, which may pose as barriers to accessing skilled delivery services [28]. Moreover, adolescent mothers are at a higher risk of intrapartum mistreatment during childbirth [29]. These factors may explain why some young mothers deliver at home. This finding calls for urgent attention from stakeholders, including the Ministry of Health, Ghana Health Services, and Non-Governmental Organizations that are interested in promoting the health and wellbeing of women.
In addition, it was found that health facility delivery was associated with higher maternal education and higher socioeconomic status. Also, young mothers residing in rural areas had reduced odds of utilizing skilled delivery services. All the above findings have been supported by similar studies in India [24], Nigeria [23], and Bangladesh [30]. For instance, a systematic review of similar studies across low-and middle-income countries confirms that adolescents’ utilization of maternal health services is influenced by educational status, wealth index, and place of residence [31]. These findings are understandable since women with higher education are literates and can access information about pregnancy and childbirth complications from the electronic and print media. Moreover, women from wealthy households are more likely to afford health services compared with those from poor households. In Ghana, the majority of the health facilities are concentrated in urban areas, hence women in these areas are more likely to have access to skilled delivery services. Further, young mothers in the Upper East region had the highest odds of giving birth in a health facility. Available evidence shows that the Upper East region has the highest coverage of maternal health services, including antenatal and skilled delivery [17]. Further, this study demonstrated that utilization of skilled delivery was associated with adequate ANC visits. Nigerian adolescent mothers who accessed full antenatal care visits were seven times more likely to give birth in a facility compared with their counterparts [23]. There is substantial literature to show that ANC visits and skilled delivery are positively correlated [31].
The findings from this study have implications for maternal health policy and programming.
This study highlights the socio-economic and geographic disparities in the utilization of skilled delivery services among young mothers. Utilization of skilled delivery services was low among young mothers with low educational status, those from poorer households and those residing in rural areas. This implies that these young mothers are at a higher risk of pregnancy and childbirth complications as well as negative birth outcomes. It is, therefore, imperative for stakeholders, including the Ministry of Health and Ghana Health Services, to prioritize maternal health interventions among young women from low socio-economic backgrounds. Interventions that focus on increasing ANC coverage, promoting girl child education, and bridging the socio-economic gap between the rich and the poor will help increase the utilization of skilled delivery services among young women in Ghana. Stakeholders must ensure equity in the distribution of health care resources, including infrastructure and health workforce, between rural and urban areas.
Strength and limitations
To the best of the authors’ knowledge, this is the maiden study in Ghana to assess the utilization of skilled delivery services among young mothers, using national representative data. Therefore, these findings can be generalized to the young population in Ghana. However, this study is not without limitations. This study employed a cross-sectional design, therefore, the findings cannot explain the reasons behind young mothers’ choice of place of delivery. Hence, studies that employ qualitative designs to explore in-depth the intricate views of adolescent and young mothers regarding the choice of place of delivery will be valuable. The associations found in this study, as with surveys in general, do not mean causation. Thus, the findings must be interpreted with caution.
Conclusion
The findings of this study showed that the majority of young mothers in Ghana utilized skilled delivery services. Yet, a substantial proportion of young mothers delivered at home, despite efforts to increase the utilization of maternal health services. Health facility delivery was influenced by socio-demographic factors, socio-economic factors, and adequate utilization of ANC. Going forward, interventions that seek to increase the utilization of skilled delivery services among young women should focus on addressing the socio-economic disparities. Stakeholders can leverage these findings to help reduce maternal and neonatal mortalities as well as promote the health and wellbeing of young women in Ghana.
Availability of data and materials
The data used in this study is owned by The DHS Program, therefore, the authors cannot share the data. Interested persons can contact The DHS Program for the data (https://dhsprogram.com/data/available-datasets.cfm). The authors confirm they did not have any special access or privileges to the data that other researchers would not have.
Abbreviations
- GDHS:
-
Ghana Demographic and Health Survey
- ANC:
-
Antenatal care
- NHIS:
-
National Health Insurance Scheme
- SSA:
-
Sub-Sahara Africa
- MMR:
-
Maternal Mortality Rate
- FMHCP:
-
Free Maternal Health Care Policy
References
WHO. The global health observatory; explore a world of health data-maternal and reproductive health. 2021. https://www.who.int/data/gho. Accessed 21 Sept 2021.
WHO. Newborns: improving survival and well-being-key facts. 2021. https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality. Accessed 24 Sept 2021.
WHO. Global maternal mortality; fact sheets. 2021. https://www.who.int/news-room/fact-sheets/detail/maternal-mortality. Accessed 26 Sept 2021.
Yamey G, Shretta R, Binka FN. The 2030 sustainable development goal for health. BMJ. 2014;349. https://doi.org/10.1136/bmj.g5295
WHO. Adolescent pregnancy: key fact. 2021. https://www.who.int/news-room/fact-sheets/detail/adolescent-pregnancy. Accessed 27 Sept 2021.
Mweteni W, Kabirigi J, Matovelo D, Laisser R, Yohani V, Shabani G, Shayo P, Brenner J, Chaput K. Implications of power imbalance in antenatal care seeking among pregnant adolescents in rural Tanzania: a qualitative study. PLoS One. 2021;16(6):e0250646.
Singh PK, Singh L, Kumar C, Rai RK. Correlates of maternal healthcare service utilisation among adolescent women in Mali: analysis of a nationally representative cross-sectional survey, 2006. J Public Health. 2013;21(1):15–27.
Adolescent pregnancy [https://www.who.int/news-room/fact-sheets/detail/adolescent-pregnancy]. Accessed 10 Sept 2021.
Adolescents: health risks and solutions [https://www.who.int/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions]. Accessed 23 Sept 2021.
WHO. WHO, “Adolescents: health risks and solutions 2018,.” 2018. https://www.who.int/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions. Accessed 23 Sept 2021.
Bhowmik J, Biswas R, Woldegiorgis M. Antenatal care and skilled birth attendance in Bangladesh are influenced by female education and family affordability: BDHS 2014. Public Health. 2019;170:113–21.
Munabi-Babigumira S, Nabudere H, Asiimwe D, Fretheim A, Sandberg K. Implementing the skilled birth attendance strategy in Uganda: a policy analysis. BMC Health Serv Res. 2019;19(1):1–15.
GMHS. 2017 Ghana Maternal Health Survey: fact sheet. 2017. https://dhsprogram.com/pubs/pdf/GF42/GF42.pdf. Accessed 25 Sept 2021.
WHO. WHO recommendations on antenatal care for a positive pregnancy experience: World Health Organization; 2016. https://apps.who.int/iris/bitstream/handle/10665/250796/9789241549912-eng.pdf?sequence=1. Accessed 9 Oct 2021.
Saaka M, Akuamoah-Boateng J. Prevalence and determinants of rural-urban utilization of skilled delivery services in northern Ghana. Scientifica. 2020. https://doi.org/10.1155/2020/9373476.
Singh P, Singh KK, Singh P. Maternal health care service utilization among young married women in India, 1992–2016: trends and determinants. BMC Pregnancy Childbirth. 2021;21(1):1–13.
Ghana Statistical Service. Ghana Maternal Health Survey 2017. Ghana: GSS, GHS, the DHS program; 2018. https://dhsprogram.com/pubs/pdf/FR340/FR340.pdf. Accessed 12 Oct 2021.
Ghanaweb. Ghana Health Service Teenage Pregnancy Update 2021. https://www.google.com/search?q=Ghana+Health+Service%3A+Ghana+Health+Service+Teenage+Pregnancy+Update+2021&oq=Ghana+Health+Service%3A+Ghana+Health+Service+Teenage+Pregnancy+Update+2021&aqs=chrome..69i57.943j0j15&sourceid=chrome&ie=UTF-8. Accessed 25 Oct 2021.
Abor PA, Abekah-Nkrumah G, Sakyi K, Adjasi CK, Abor J. The socio-economic determinants of maternal health care utilization in Ghana. Int J Soc Econ. 2011;38(7):628–48.
Ebu NI, Gross J. Factors influencing access to antenatal services and delivery care in sub-Saharan Africa. Afr J Midwifery Womens Health. 2015;9(2):58–65.
Ghana Statistical Service, Ghana Health Service, Macro, ICF International. Ghana Demographic and Health Survey 2014. Accra; 2015. https://dhsprogram.com/pubs/pdf/fr307/fr307.pdf. Accessed 23 Oct 2021.
Williams R. Analyzing complex survey data: Some key issues to be aware of. University of Notre Dame; 2015. https://www3.nd.edu/~rwilliam/stats2/SvyCautions.pdf. Accessed 11 Oct 2021.
Alex-Ojei CA, Odimegwu CO, Akinyemi JO. Patterns of delivery assistance among adolescent mothers in Nigeria. Midwifery. 2020;82:102619.
Singh PK, Rai RK, Alagarajan M, Singh L. Determinants of maternity care services utilization among married adolescents in rural India. PLoS One. 2012;7(2):e31666.
Azaare J, Akweongo P, Aryeetey GC, Dwomoh D. Impact of free maternal health care policy on maternal health care utilization and perinatal mortality in Ghana: protocol design for historical cohort study. Reprod Health. 2020;17(1):1–17.
Brugiavini A, Pace N. Extending health insurance in Ghana: effects of the National Health Insurance Scheme on maternity care. Heal Econ Rev. 2016;6(1):1–10.
Ahinkorah BO, Seidu A-A, Budu E, Agbaglo E, Appiah F, Adu C, Archer AG, Ameyaw EK. What influences home delivery among women who live in urban areas? Analysis of 2014 Ghana Demographic and Health Survey data. PLoS One. 2021;16(1):e0244811.
Akweongo P, Aikins M, Wyss K, Salari P, Tediosi F. Insured clients out-of-pocket payments for health care under the national health insurance scheme in Ghana. BMC Health Serv Res. 2021;21(1):1–14.
Habib HH, Torpey K, Maya ET, Ankomah A. Promoting respectful maternity care for adolescents in Ghana: a quasi-experimental study protocol. Reprod Health. 2020;17(1):1–10.
Kamal SM. Factors affecting utilization of skilled maternity care services among married adolescents in Bangladesh. Asian Popul Stud. 2009;5(2):153–70.
Banke-Thomas OE, Banke-Thomas AO, Ameh CA. Factors influencing utilisation of maternal health services by adolescent mothers in Low-and middle-income countries: a systematic review. BMC Pregnancy Childbirth. 2017;17(1):1–14.
Acknowledgements
The authors would like to thank Measure DHS for making the dataset available to us. Additionally, EAA is receiving funding as a PhD candidate from the HRP Alliance, part of the UNDP-UNFPA-UNICEF-WHO-World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), a cosponsored programme executed by the World Health Organization (WHO), to complete his studies. This article represents the views of the named authors only and does not represent the views of the World Health Organization.
Funding
The author did not receive any funding for this study.
Author information
Authors and Affiliations
Contributions
EAA and SKA conceptualized the topic and wrote the original draft. DOA and EJM obtained the data. AM and EAA performed the analysis. AAL, DOA, EJM, AM and KT supervised, reviewed and edited the paper. All authors contributed extensively to the work presented in this paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ghana Health Service Ethics Review Committee approved the protocols for the 2014 Ghana Demographic and Health Survey. Informed consent was obtained from all adult participants and informed assent from minors. A formal request to use the raw data was made to The DHS Program through their website (https://dhsprogram.com/data/available-datasets.cfm). The study was performed in accordance with relevant regulations and guidelines. Data used in this study were anonymised before use.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Anaba, E.A., Alangea, D.O., Addo-Lartey, A. et al. Determinants of health facility delivery among young mothers in Ghana; insights from the 2014 Ghana Demographic and Health Survey. BMC Pregnancy Childbirth 22, 656 (2022). https://doi.org/10.1186/s12884-022-04985-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-04985-5