Abstract
Background
Obstetric infections are the third most common cause of maternal mortality, with the largest burden in low and middle-income countries (LMICs). We analyzed causes of infection-related maternal deaths and near-miss identified contributing factors and generated suggested actions for quality of care improvement.
Method
An international, virtual confidential enquiry was conducted for maternal deaths and near-miss cases that occurred in 15 health facilities in 11 LMICs reporting at least one death within the GLOSS study. Facility medical records and local review committee documents containing information on maternal characteristics, timing and chain of events, case management, outcomes, and facility characteristics were summarized into a case report for each woman and reviewed by an international external review committee. Modifiable factors were identified and suggested actions were organized using the three delays framework.
Results
Thirteen infection-related maternal deaths and 19 near-miss cases were reviewed in 20 virtual meetings by an international external review committee. Of 151 modifiable factors identified during the review, delays in receiving care contributed to 71/85 modifiable factors in maternal deaths and 55/66 modifiable factors in near-miss cases. Delays in reaching a GLOSS facility contributed to 5/85 and 1/66 modifiable factors for maternal deaths and near-miss cases, respectively. Two modifiable factors in maternal deaths were related to delays in the decision to seek care compared to three modifiable factors in near-miss cases. Suboptimal use of antibiotics, missing microbiological culture and other laboratory results, incorrect working diagnosis, and infrequent monitoring during admission were the main contributors to care delays among both maternal deaths and near-miss cases. Local facility audits were conducted for 2/13 maternal deaths and 0/19 near-miss cases. Based on the review findings, the external review committee recommended actions to improve the prevention and management of maternal infections.
Conclusion
Prompt recognition and treatment of the infection remain critical addressable gaps in the provision of high-quality care to prevent and manage infection-related severe maternal outcomes in LMICs. Poor uptake of maternal death and near-miss reviews suggests missed learning opportunities by facility teams. Virtual platforms offer a feasible solution to improve routine adoption of confidential maternal death and near-miss reviews locally.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Obstetric infections are the third most common cause of maternal mortality, with the largest burden in low and middle-income countries (LMICs) (10·7%) compared with high-income countries (HICs) (4·7%) [1]. The true proportion of infection-related maternal deaths is most probably higher, as the estimates do not include deaths due to abortion-related or non-obstetric infections. The Global Maternal Sepsis Study (GLOSS), led by the World Health Organization (WHO), estimated that about 70 women per 1000 live births were admitted or already hospitalized with a maternal infection [2]. Among those, 11 women per 1000 live births had infection-related severe maternal outcomes (SMO: death or near-miss). The most common infections identified in the GLOSS study were urinary tract infections, endometritis, chorioamnionitis, abortion-related infections, and infections of the skin and soft tissue, in line with previous studies [3,4,5].
Infection-related maternal mortality and severe morbidity can have many contributing factors, including delays in the decision to seek care, arrival at the appropriate health facility, and provision of adequate and timely management [6]. Maternal and Perinatal Death Surveillance and Response (MPDSR), a process aimed at improving identification, reporting, and review of maternal deaths, is key for addressing health system issues and inadequacies to end preventable maternal mortality [6, 7]. Individual maternal death review is one of the cornerstones of MPDSR to assess the causes of death during pregnancy, around the time of childbirth, post-partum, or post-abortion, identify missed opportunities within the health system, and facilitate appropriate response, in a continuous surveillance cycle. However, it is crucial not only to avert future similar deaths but also to prevent acute severe complications and longer-term sequelae associated with experiencing a maternal near-miss (women who nearly died but survived a life-threatening complication that occurred during pregnancy, childbirth or 6 weeks postnatally [3]). Review of maternal near-miss cases may provide additional information on factors associated with occurrence of adverse outcomes, as they occur much more frequently than maternal deaths [8, 9].
Maternal deaths and near-miss reviews, when timely implemented with accurate and complete data [10], and in an environment of confidentiality, no-blame and professionalism, are useful in identifying contributing factors and formulating recommendations to improve services and quality of care [7, 11,12,13], and ultimately reduce all cause or cause-specific mortality and severe morbidity [14, 15], such as maternal infections [16, 17].
Considering the significance of infection-related maternal deaths and near-misses, and paucity of studies reporting on in-depth explorations of their causes and the surrounding circumstances in LMICs, this study sought to contribute to current knowledge on factors affecting the survival of pregnant or recently pregnant women after infection, using the GLOSS study [2].
This manuscript describes the results of an international, virtual confidential enquiry into maternal deaths and near-miss cases identified within the frame of the GLOSS study. The international external review committee analyzed causes of infection-related maternal deaths and near miss, identified clinical and non-clinical modifiable factors from before admission until death or discharge and generated suggested actions for facility level care improvement to avoid preventable infection-related maternal deaths and near-miss.
Methods
Study design and participants
The Global Maternal Sepsis Study (GLOSS) was a facility-based, prospective, inception cohort study implemented in health care facilities located in pre-specified geographical areas in 52 countries [18]. During a seven-day period (November 28 to December 04, 2017), all women admitted to or already hospitalized in participating facilities with suspected or confirmed infection during any stage of pregnancy through to 42 days after abortion or childbirth were included in the study. Participants were followed during their stay in the facilities until hospital discharge, transfer to another health facility not included in the study, or death. Among 2466 women recruited (Fig. 1) from 43 low- and middle-income countries (LMICs), a total of 26 infection-related maternal deaths and 351 infection-related near-miss cases were reported.
This is an extension of the GLOSS protocol, that includes additional data collection, and where all maternal deaths and near-miss cases from health facilities reporting at least one infection-related death were eligible for inclusion. A total of 16 countries, out of 17 eligible, expressed interest to participate in this study. Therefore, 25 infection-related maternal deaths and 53 near-miss cases from 25 health facilities were considered for inclusion. Cause of deaths were classified using the WHO ICD-MM (The WHO application of ICD-10 to deaths during pregnancy, childbirth, and puerperium: ICD-Maternal Mortality) system [19]. Near-miss cases were defined using the WHO criteria as a woman who nearly died but survived a life-threatening condition during pregnancy, childbirth, post-partum or post-abortion periods [3].
Ethical approvals were obtained from the WHO ethics review committee and as required by national or local entities.
Data collection
Health facility information was available from the GLOSS study [18, 20]. As part of the preparation for facility inclusion for this study, we requested baseline data on facility characteristics related to local maternal death review processes and characteristics of the local committees shown in Additional file 1: Table S1, including existing systems to review deaths and near-miss, composition of the committee, organization of the meetings, documentation used to review or produced after the review process, findings dissemination channels and mechanism to follow up on the committee recommendations.
During the GLOSS study, information was collected from individual facility medical records on sociodemographic and obstetric characteristics of the woman; source of infections and management in the health facility; and maternal, perinatal, and neonatal outcomes. However, given that the design and initial objectives of the GLOSS study did not include a review component for maternal deaths and/or near-miss, comprehensive information for such reviews was not specifically collected. Additional data for this extended phase of the GLOSS study were requested using the form in Fig. S1, Additional file 1, from the facilities on: antenatal care received, mode of transport to the hospital, prior hospital admissions and referral including vital signs and laboratory measurement during hospital stay, timing of antimicrobials, additional diagnoses or management, managing multidisciplinary team composition, detailed information on cause of death and use of ICD-10 coding in case of death or near-miss. Data collection forms, the research protocol, and a manual of operation were translated from English into French and Spanish. Anonymized index case data collection forms were completed manually, scanned and transferred by the participating facility study coordinators, then entered into and managed using REDCap (Research Electronic Data Capture) electronic data capture tools [21, 22] by the WHO coordination team.
Index case anonymized available documents were collected from health facilities or local review committees, including anonymized copies of death certificates, autopsy reports, reports from local death reviews, or other documents relevant to each case.
Virtual maternal and near-miss case review process
An external multi-country review committee was formed and tasked to perform independent assessments virtually of all included infection-related maternal deaths and near-miss cases. The external review committee consisted of 30 experts from 12 countries who indicated interest in taking part in the reviews, including GLOSS regional and country coordinators, and members of the country teams. All participants were health care providers, including gynecologists and obstetricians, internists and cardiologists, non-specialist medical doctors, nurses, and midwives. About half of the participants reported having extensive experience in review meetings, while half reported having little experience. Participants were divided into five multi-country review committees based on their preferred languages (English, French, and Spanish) and time zones. Five internationally recognized expert facilitators of maternal death and near-miss reviews and MPDSR were invited to serve as meeting moderators and were paired to the review committee groups. A team of WHO staff and consultants coordinated logistics for the review meetings.
Case summaries were prepared for each maternal death and near-miss case by the WHO coordination team using the template in Fig. S2, Additional file 1, that was adapted from the International Federation of Gynecology and Obstetrics (FIGO) Maternal Death Review clinical summary form [23]. Case summaries presented a main diagnosis, timing and chain of events, a narrative of the case management, outcomes, and facility characteristics. Distinct from the source clinical form, the case summary form used in this study contained questions that were specific to the management of an infection, for example, the date and time of the first antibiotic and the date and time of suspicion or diagnosis of infection. The case summary form also investigated the use of the International Classification of Disease (ICD) codes by facility review teams to classify cases of maternal deaths.
To assess gaps in management from before admission until death or discharge and document the review findings, a note-taking form in Fig. S3, Additional file 1, was adapted from Borchert et al. and Menéndez, et al. [24, 25]. The form provided an objective way to evaluate the severity of modifiable factors/gaps as minor, intermediate, or major, evaluate the severity of diagnosis discrepancies, and help review committee members think through the gaps as they read the cases before the meetings.
Over a three-month period, between August 31, 2020, and November 11, 2020, 20 virtual external review meetings were conducted. Each review meeting was scheduled for 75 minutes and facilitated by one of the international moderators. Maternal deaths and near-miss cases were grouped into three geographical groups based on the review languages and numbered sequentially. Using the numbers, the index cases were randomly allocated to committees outside the geographical area where the cases occurred. Two deaths and one near-miss cases were assigned for each meeting and the review committees were sent case summaries 10 to 14 days before the meeting. Individual members of the committees were tasked to prepare a presentation on one case to be presented at the virtual meetings and a facilitated discussion followed to build consensus. In cases where a team was unable to review all three cases assigned per session, the remaining case was reviewed in the subsequent meeting. Two assigned individuals from the coordination team took notes at the meetings to document the cause of death, missed opportunities and recommendations discussed.
Analysis
We described the numbers and proportions of maternal demographic, obstetric and clinical characteristics, as well as complications, and outcomes for maternal deaths and near-miss cases.
The meeting notes for each case were reviewed by the coordination team and modifiable factors were identified and categorized following a structured process of thematic analysis [26], informed by themes defined in previously published work [24]. Factors that occurred prior to hospital admission, at admission, diagnosis, treatment, and discharge were included. New sub-themes were created where existing ones were not adequate. These included information on the circumstances that preceded maternal presentation to the GLOSS health facility such as antenatal care history and pre-existing comorbidities, the adequacy of the managing team at the GLOSS facility, and whether or not a facility review was conducted.
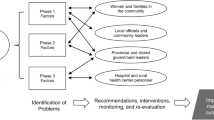
Modifiable factors identified during the external review meetings were then organized into the following categories using the three delays framework [27] - (1) deciding to seek appropriate medical help for an obstetric emergency; (2) reaching an appropriate facility; and (3) receiving adequate care when a facility is reached. Gaps that did not directly result from a delay to seek, reach, or receive adequate care were categorized under other clinical and non-clinical factors as per Table 2. Other clinical factors included antibiotics resistance and unexplained prolonged hospitalization. Non-clinical factors were related to the managing team (composition, mobilization, and collaboration), and local contextual factors and policies.
Recommendations were classified into five thematic areas following the three delays framework and consolidated across all reviews to avoid repetition. Recommendations addressing delays 1 and 2 were combined into a single thematic area due to the paucity of data for these delays. Recommendations related to delay 3 (receiving adequate care when a facility is reached) and other clinical factors were sub-divided into three thematic areas namely clinical and laboratory examination, diagnosis, and treatment. A fifth thematic area addressed the gaps related to the managing team.
Preliminary results and summary of the recommendations formulated during the review meetings were shared with the members of the five review committees in two joint virtual meetings providing an opportunity to discuss the relevance of findings and feasibility of recommendations across various local contexts.
Results
There were 25 infection-related maternal deaths and 53 near-miss cases from 25 health facilities in 16 countries eligible for inclusion. However, only 11 countries submitted the necessary additional data on 13 out of 15 maternal deaths and 19 out of 47 near-misses (Fig. 1). Five country study teams were unable to submit their data due to factors including inability to trace the case folders, a demanding data collection process, staff changes that affected country study teams, and difficulty obtaining additional local ethical approvals. Three of the 11 countries submitted death certificates, and three submitted additional documentation. Only one country submitted both death certificates and additional documentation.
From the documented information available, most women with severe maternal outcomes (SMO) related to infection were between ages 20 and 35 (n = 7/13 maternal deaths and n = 14/19 near-miss) (Table 1). Two-thirds of SMOs occurred in the post-partum period (n = 6/13 deaths and n = 10/19 near-miss) and to multiparous women (n = 8/13 deaths and n = 12/19 near-miss). Close to a third of deaths (n = 4/13) and near-miss (n = 5/19) were from post-abortion complications. Among SMOs, at least one in every five had delivered by cesarean section with near-miss cases (n = 8/19) occurring almost twice as often in this group compared to maternal deaths (n = 3/13). Just over half of the women who died (n = 7/13) or had a near-miss (n = 10/19) were managed in intensive care (ICU) or in a high dependency unit (HDU). More than a third of women (n = 5/13) died within the first 48 hours of admission to the health facility. Two thirds of near-miss cases required more than a week of hospital admission (n = 13/19). Perinatal outcome was very poor – only 3/15 survived when there was a maternal death and 8/19 in the case of a near-miss. The results presented from the virtual review meetings are from 12 of the 13 maternal deaths as one death occurred within the first hour of presentation before the managing team commenced clinical management, and data was not sufficient to conduct a review of the case. Facility audits were conducted for only 2/13 maternal deaths and 0/19 near-miss cases (See Table S1, Additional file 1).
The external review committee identified 151 modifiable factors from the available information, among which 85 were from death reviews and 66 were from near-miss reviews (Table 2) - the most common modifiable factors were related to delays in receiving adequate care in the facility. Between three and 12 factors were identified per maternal death, and between zero and seven factors per near-miss (See Table S2, Additional file 1).
The delay in receiving care (delay 3) was considered by the committee to have contributed to 71 of the 85 modifiable factors for maternal deaths (Fig. 2), and 55 of the 66 modifiable factors for near-miss cases. Among maternal deaths, five of the 85 modifiable factors were associated with a delay in reaching a GLOSS facility in a timely manner (delay 2) compared to one of the 66 factors in near-miss cases. A delay in the decision to seek care (delay 1) was documented in two of the 85 modifiable factors identified for maternal deaths compared to three of the 66 modifiable factors in near-miss cases. Other clinical and non-clinical factors contributed each to seven of 85 modifiable factors for maternal deaths and 66 near-miss cases.
Number of modifiable factors identified in the review of 12 maternal deaths and 19 near-miss. Note. Bold numbers are total. Other clinical factors include antimicrobial resistance and unexplained prolonged hospitalization. Non-clinical factors include incomplete multidisciplinary team, delayed mobilization of the managing team, restrictive abortion policies and legislation, stigma of preexisting condition as a potential care barrier, discharge against medical advice
Inadequate or delayed treatment made up 32 of 71 modifiable factors related to a delay in receiving care (delay 3) for maternal deaths compared to 18 of 55 factors for near-miss cases (Fig. 2). Clinical and laboratory examination issues contributed to 20 of 71 modifiable factors in maternal deaths and 17 of 55 factors in near-miss cases. Diagnosis-related problems were higher in near-miss cases at 12 of 55 modifiable factors than maternal deaths with 13 of 71 factors. Table 2 details the modifiable factors identified during the review.
Table S3, Additional file 1 compares the causes of death reported in the facility records with re-assigned causes of death after review by the GLOSS coordination team. A cause of death was not recorded in 2 of the 13 deaths reviewed. For 4 of the 11 deaths, the review committee agreed with the reported underlying cause of death as an infection but provided a more detailed cause of death. At the facility level, only 4 of the 13 deaths were assigned a cause of death using the ICD coding system, 2 using ICD-10 and 2 using ICD-MM.
Based on the review findings, the external review committee generated a broad set of recommendations for improved prevention and management of maternal infections and sepsis presented in Table 3.
Discussion
This global virtual review, of 13 infection-related maternal deaths and 19 near-miss cases from 11 LMICs, highlights important gaps in quality standards of care related to delays in establishing diagnosis and appropriate management, including clinical and laboratory examinations. Information on care prior to presentation at the health facilities was often lacking or incomplete. Missed opportunities were exacerbated by antenatal care interventions not fully implemented, delayed referrals to higher level facilities, incomplete multidisciplinary teams as well as gaps in conducting reviews and disseminating findings to health facilities and staff involved in care.
Delays in the recognition of early warning signs of clinical deterioration, diagnosis, and prompt management of maternal infection and sepsis were common findings for both deaths and near-miss cases reviewed, in line with findings from previous infection-related deaths reviews in settings with limited resources [16, 28]. Utilization of clinical early warning systems globally, characterized by abnormal clinical observations of consciousness level, temperature, pulse rate, respiratory rate and blood pressure, have been shown to be an important tool for prompt diagnosis [29], better monitoring, and improved management of pregnant or recently pregnant women admitted with infection [30]. The external review committee recommended the use of early warning signs systems as part of the essential quality monitoring to evaluate the severity of maternal infection and assess the need for higher level care at admission or during hospital stay.
Gaps in diagnosis and management of maternal infections and sepsis could have resulted from delayed or absent microbiological cultures and relevant laboratory tests and imaging. Notably, among maternal deaths and near-miss cases with delayed or absent culture results, the sources of infection were likely incorrectly identified in two deaths and three near-miss cases and unidentified in one death. Similarly, others have reported lack of cultures in up to 25% of sepsis-related maternal deaths [16, 28]. While the reasons behind absent microbiology cultures were not documented in our study, others cite rapid deterioration of the woman’s clinical condition, lost samples, missing results from medical records, and out of pocket costs [16], as some of the reasons. While reiterating the importance of collecting blood culture samples prior to antibiotic treatment in all suspected maternal sepsis cases, the external review committee recommended that imaging and other relevant laboratory tests are also essential to enable diagnosis and support adequate monitoring and management.
Suboptimal use of antibiotics was a significant contributor to gaps in treatment identified for most of the maternal deaths and near-miss cases. Early administration of appropriate antimicrobial agents provide the most benefit in sepsis when accompanied by high quality supportive care – e.g. fluid resuscitation [30]. However, antimicrobial use with unsupported frequent and erratic changes without microbiological or clinical indication and removal of the infection source can be detrimental and contribute to the emergence of antimicrobial resistance [31]. While the external review committee agreed that ideally an antibiotic sensitivity profile ought to guide the choice of and switch between antimicrobial agents, they also recognized situations where the administration is justified when such a sensitivity profile is not possible or poses substantial delay in cases of severe infections or sudden deterioration in the clinical presentation. In those instances, adequate documentation of the reasons in medical records was encouraged. Members of the external review committee who had noted similar findings related to provision of quality care in their local maternal death audits highlighted a potential connection with health system gaps. For instance, a correlation between misdiagnosis and the absence or limitations of good laboratory facilities such as in primary level birthing centers; or delay in administration of antibiotics linked to a shortage of antimicrobial agents in the hospital pharmacy.
Significantly increased risk of fetal and neonatal deaths have been reported in countries where systemic infections/ sepsis are among the leading causes of maternal morbidity and mortality [32, 33]. Extremely low survival rates of the babies among the reviewed cases of maternal deaths (3/15) and maternal near-miss (8/19) support the association between SMO and poor perinatal outcomes [34]. Beyond coverage of essential interventions, delays in quality care implementation and lack of comprehensive supportive care are hypothesized contributors to maternal outcomes, and in turn, perinatal survival [32]. Linking maternal and fetal records with maternal and perinatal death surveillance and response can strengthen the provision of comprehensive supportive care to the mother-baby dyad.
We were also able to identify issues in the process of conducting reviews. At the facility level, the cases we reviewed demonstrated that there was no documented evidence that the majority of deaths/ near-miss cases had been reviewed, despite an established maternal death review processes reported in two-thirds of the included facilities. A majority of countries have policies in place for maternal death notification and review, yet a gap remains when examining the steps beyond this, including reviewing and reporting at an aggregate level, disseminating findings and recommendations, and involving civil society and communities [35]. While an understanding of the MPDSR process is fundamental to conducting reviews, the external review committee stressed that experience is not needed to get started. As reflected by the range of experience among members, the committee underscored that capacity building occurs through an iterative process of learning that occurs as teams participate in and incorporate the review meetings into the clinical management of cases and self-evaluation. The committee also stressed that a no-blame culture is critical to the successful implementation of reviews and response [7, 36], and noted that the inclusion of a near-miss case among the regular death reviews boosted the morale of the team.
Among the reviewed cases, the committee recognized a need to involve the referral facilities and staff in the review and dissemination process. Through the virtual platform, reviewers would be able to participate from any location, mitigating distance and manpower constraints which are barriers to maternal deaths audits [37].
Recommendations from our study are particularly relevant given the shortage of written protocols specific to the prevention or management of infection related SMO in LMIC contexts. Consistent with existing standard sepsis guidelines [30], the proposed recommendations reiterate the main issues continue to be prompt identification, monitoring, initial resuscitation with intravenous fluids, diagnosis using appropriate routine microbiologic cultures, early treatment with appropriate antimicrobials and rapid control of the source of infection. Close collaboration with other medical disciplines [16] especially in cases of non-obstetric causes of sepsis, competent and motivated staff [10] as well as a more thorough implementation of the review process by managing and referral facilities and staff are also important to optimize maternal outcomes.
Strengths and limitations
To our knowledge, this is the first multi-country virtual maternal deaths and near-miss review case series. Due to the multinational composition of the external review committees and random assignments of anonymized cases to each committee, the committee members rarely encountered cases from their countries. Consequently, the nature of the review meetings enabled compliance with the basic principles of good practice of clinical audits including the confidentiality of information and the principles of no name, no shame, and no blame [8, 38]. Multi-country participation led to very rich discussions on how management differs between contexts and strong cross-country learning. One of such new learning for some was a minute of silence observed at each review meeting to humanize and honor the memories of the women that died. Interactions with members of other country teams and the experience of internationally recognized moderators enabled capacity strengthening.
Although the cases had originally been identified for the GLOSS research study, medical records information on care at the GLOSS facilities and prior to presentation were often lacking or incomplete and may explain why the majority of our recommendations focus on delay in receiving care. Efforts to obtain additional information on the missing data from other sources were unsuccessful. Incomplete or inadequate routine patient case notes documentation affects not only this study but is the reality in many settings, impeding clinical decision making and opportunities for audit and quality improvement efforts. Our study demonstrated the urgency to invest so that “Every woman and newborn has a complete, accurate, standardized medical record during labour, childbirth and the early postnatal period” ([10], p.41). Similar challenges with poor record keeping and lost records are reported in other obstetric audits [16, 37, 38]. Records for two maternal deaths and 18 near-miss cases were not found in the facility and there was a lack of consensus on the circumstances surrounding one maternal death. Such shortcomings in record keeping may undermine the quality of the information and review conclusions [39], as cases were analyzed and classified by the expert committee based on available information from medical records.
One of the study objectives was to compare findings and recommendations of local committee reviews and those from an external review committee. An extensive comparison was impossible given the low rates of internal audits conducted at the facilities.
Lastly, external reviewers may not have been completely familiar with the context and the facility managing teams were not available for clarifications during the review which could have affected interpretation of events by the reviewers. In addition, the confidential nature of the reviews limited the ability of the reviewers to probe further into the local context, therefore the ensuing recommendations were not specific to each death or near-miss or to the facility or country involved.
Conclusion
The lack of precision in management due to limited continuous clinical assessment, use of clinical skills and laboratory examinations contribute to missed opportunities in the provision of high-quality care to prevent and manage infection related SMO, and shortfalls in maternal death and near-miss review processes in facilities in LMICs. Poor uptake of maternal deaths and near-miss reviews suggests missed learning opportunities by facility teams. Routine confidential enquiries and review meetings should be incentivized at the facility level as part of quality improvement efforts. This study confirms the feasibility of multinational maternal death and near-miss reviews using a virtual platform. While locally conducted reviews would allow for more detailed and context specific recommendations, virtual review meetings allow for a confidential approach to reviewing deaths across a diverse number of settings. The authors recognize the need for additional evaluations to assess the quality of the review process, compare and validate findings, assess the feasibility of implementing and adapting actionable recommendations to different contexts.
Availability of data and materials
The data used for this analysis can be made available upon reasonable request, in accordance with the GLOSS research group data sharing policy and WHO policy of data use and data sharing. For further information, contact the corresponding author.
Abbreviations
- LMICS:
-
Low-and Middle-Income Countries
- HICs:
-
High Income Countries
- GLOSS:
-
The Global Maternal Sepsis Study
- WHO:
-
World Health Organization
- SMO:
-
Severe Maternal Outcomes
- MPDSR:
-
Maternal and Perinatal Death Surveillance and Response
- WHO ICD-MM:
-
The WHO application of ICD-10 to deaths during pregnancy, childbirth, and puerperium: ICD-Maternal Mortality
- REDCap:
-
Research Electronic Data Capture
- FIGO:
-
The International Federation of Gynecology and Obstetrics
- ICD:
-
International Classification of Disease
- ICU:
-
Intensive care
- HDU:
-
High dependency unit
References
Say L, Chou D, Gemmill A, Tunçalp Ö, Moller A-B, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2:e323–33.
Bonet M, Brizuela V, Abalos E, Cuesta C, Baguiya A, Chamillard M, et al. Frequency and management of maternal infection in health facilities in 52 countries (GLOSS): a 1-week inception cohort study. Lancet Glob Health. 2020;8:e661–71.
Souza JP, Gülmezoglu AM, Vogel J, Carroli G, Lumbiganon P, Qureshi Z, et al. Moving beyond essential interventions for reduction of maternal mortality (the WHO multicountry survey on maternal and newborn health): a cross-sectional study. Lancet Lond Engl. 2013;381:1747–55.
Oud L. Pregnancy-associated severe Sepsis: contemporary state and future challenges. Infect Dis Ther. 2014;3:175–89.
Barton JR, Sibai BM. Severe Sepsis and septic shock in pregnancy. Obstet Gynecol. 2012;120:689–706.
WHO. Maternal death surveillance and response: technical guidance. Information for action to prevent maternal death. Geneva: World Health Organization; 2013. http://apps.who.int/iris/bitstream/handle/10665/87340/9789241506083_eng.pdf. Accessed 5 May 2021
WHO. Maternal and perinatal death and surveillance and response: materials to support implementation. Geneva: World Health Organization; 2021. https://www.who.int/publications-detail-redirect/9789240036666. Accessed 4 Dec 2021
WHO. Beyond the numbers: reviewing maternal deaths and complications to make pregnancy safer. Geneva: World Health Organization; 2004. https://apps.who.int/iris/handle/10665/42984. Accessed 12 Jun 2021
WHO. Evaluating the quality of care for severe pregnancy complications: the WHO near-miss approach for maternal health. Geneva: World Health Organization; 2011. https://apps.who.int/iris/handle/10665/44692. Accessed 16 Aug 2021
WHO. Standards for improving quality of maternal and newborn care in health facilities. Geneva: World Health Organization; 2016. https://www.who.int/docs/default-source/mca-documents/advisory-groups/quality-of-care/standards-for-improving-quality-of-maternal-and-newborn-care-in-health-facilities.pdf. Accessed 9 Sept 2021
Knight M, Acosta C, Brocklehurst P, Cheshire A, Fitzpatrick K, Hinton L, et al. Beyond maternal death: improving the quality of maternal care through national studies of ‘near-miss’ maternal morbidity. Southampton (UK): NIHR Journals Library; 2016.
Institut National de la Santé et de la Recherche Médicale, SANTÉ PUBLIQUE FRANCE. Les morts maternelles en France : mieux comprendre pour mieux prévenir. 5e rapport de l’Enquête nationale confidentielle sur les morts maternelles (ENCMM), 2010–2012. France; 2017. https://www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-cardiovasculaires-et-accident-vasculaire-cerebral/maladies-vasculaires-de-la-grossesse/documents/rapport-synthese/les-morts-maternelles-en-france-mieux-comprendre-pour-mieux-prevenir.-5e-rapport-de-l-enquete-nationale-confidentielle-sur-les-morts-maternelles. Accessed 15 Feb 2021.
Willcox ML, Price J, Scott S, Nicholson BD, Stuart B, Roberts NW, et al. Death audits and reviews for reducing maternal, perinatal and child mortality. Cochrane Database Syst Rev. 2020. https://doi.org/10.1002/14651858.CD012982.pub2.
Lewis G. Saving mothers’ lives: the continuing benefits for maternal health from the United Kingdom (UK) confidential enquires into maternal deaths. Semin Perinatol. 2012;36:19–26.
Dumont A, Fournier P, Abrahamowicz M, Traoré M, Haddad S, Fraser WD, et al. Quality of care, risk management, and technology in obstetrics to reduce hospital-based maternal mortality in Senegal and Mali (QUARITE): a cluster-randomised trial. Lancet Lond Engl. 2013;382:146–57.
Kodan LR, Verschueren KJC, Kanhai HHH, van Roosmalen JJ, Bloemenkamp KWM, Rijken MJ. The golden hour of sepsis: an in-depth analysis of sepsis-related maternal mortality in middle-income country Suriname. PLoS One. 2018;13:e0200281. https://doi.org/10.1371/journal.pone.0200281.
Knight M, Bunch K, Cairns A, Cantwell R, Cox P, MBRRACE-UK, et al. Saving Lives, Improving Mothers’ Care Rapid Report: Learning from SARS-CoV-2-related and associated maternal deaths in the UK. Oxford: National Perinatal Epidemiology Unit, University of Oxford; 2020. https://www.npeu.ox.ac.uk/assets/downloads/mbrrace-uk/reports/MBRRACE-UK_Maternal_Report_2020_v10_FINAL.pdf. Accessed 16 Nov 2020
Bonet M, Souza JP, Abalos E, Fawole B, Knight M, Kouanda S, et al. The global maternal sepsis study and awareness campaign (GLOSS): study protocol. Reprod Health. 2018;15:16. https://doi.org/10.1186/s12978-017-0437-8.
WHO. The WHO application of ICD-10 to deaths during pregnancy, childbirth and puerperium: ICD MM. Geneva: World Health Organization; 2012. https://apps.who.int/iris/bitstream/handle/10665/70929/9789241548458_eng.jsessionid=141094E2EBE05E4C9EBFEDD5EF7E506B?sequence=1. Accessed 15 Feb 2021
Brizuela V, Cuesta C, Bartolelli G, Abdosh AA, Malham SA, Assarag B, et al. Availability of facility resources and services and infection-related maternal outcomes in the WHO global maternal Sepsis study: a cross-sectional study. Lancet Glob Health. 2021;9:e1252–61.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. https://doi.org/10.1016/j.jbi.2019.103208.
De Brouwere V, Zinnen V, Delvaux T. How to conduct maternal death reviews (MDR). Guidelines and tools for health professionals. London: International Federation of Gynecologists and Obstetricians; 2013.
Borchert M, Goufodji S, Alihonou E, Delvaux T, Saizonou J, Kanhonou L, et al. Can hospital audit teams identify case management problems, analyse their causes, identify and implement improvements? A cross-sectional process evaluation of obstetric near-miss case reviews in Benin. BMC Pregnancy Childbirth. 2012;12:109. https://doi.org/10.1186/1471-2393-12-109.
Menéndez C, Quintó L, Castillo P, Fernandes F, Carrilho C, Ismail MR, et al. Quality of care and maternal mortality in a tertiary-level hospital in Mozambique: a retrospective study of clinicopathological discrepancies. Lancet Glob Health. 2020;8:e965–72.
Braun V, Clarke V. Thematic analysis. In: APA handbook of research methods in psychology, Vol 2: research designs: quantitative, qualitative, neuropsychological, and biological. Washington, DC: American Psychological Association; 2012. p. 57–71.
Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994;38:1091–110.
Cebekhulu S, Cornelissen L, Pattinson RC. Too little, too late : the recurrent theme in maternal deaths due to sepsis. Obstet Gynaecol Forum. 2018;28:9–12.
Umar A, Ameh CA, Muriithi F, Mathai M. Early warning systems in obstetrics: a systematic literature review. PLoS One. 2019;14:e0217864. https://doi.org/10.1371/journal.pone.0217864.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving Sepsis campaign: international guidelines for Management of Sepsis and Septic Shock: 2016. Crit Care Med. 2017;45:486–552.
Greer O, Shah NM, Johnson MR. Maternal sepsis update: current management and controversies. Obstet Gynaecol. 2020;22:45–55.
Vogel JP, Souza JP, Mori R, Morisaki N, Lumbiganon P, Laopaiboon M, et al. Maternal complications and perinatal mortality: findings of the World Health Organization multicountry survey on maternal and newborn health. BJOG Int J Obstet Gynaecol. 2014;121:76–88.
The Alliance for maternal and newborn health improvement (AMANHI) mortality study group. Population-based rates, timing, and causes of maternal deaths, stillbirths, and neonatal deaths in South Asia and sub-Saharan Africa: a multi-country prospective cohort study. Lancet Glob Health. 2018;6:e1297–308.
Baguiya A, Bonet M, Cecatti JG, Brizuela V, Curteanu A, Minkauskiene M, et al. Perinatal outcomes among births to women with infection during pregnancy. Arch Dis Child. 2021;106:946–53.
Bandali S, Thomas C, Hukin E, Matthews Z, Mathai M, Ramachandran Dilip T, et al. Maternal death surveillance and response systems in driving accountability and influencing change. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. 2016;135:365–71.
Kinney M, Louise T, Francesca P, Animesh B, Debra J, Nathalie R, et al. Overcoming blame culture: key strategies to catalyze maternal and perinatal death surveillance and response. Authorea. 2021. https://doi.org/10.22541/au.163251970.03568586/v1.
van Hamersveld KT, den Bakker E, Nyamtema AS, van den Akker T, Mfinanga EH, van Elteren M, et al. Barriers to conducting effective obstetric audit in Ifakara: a qualitative assessment in an under-resourced setting in Tanzania. Tropical Med Int Health. 2012;17:652–7.
Kongnyuy EJ, van den Broek N. The difficulties of conducting maternal death reviews in Malawi. BMC Pregnancy Childbirth. 2008;8:42. https://doi.org/10.1186/1471-2393-8-42.
Combs Thorsen V, Sundby J, Meguid T, Malata A. Easier said than done!: methodological challenges with conducting maternal death review research in Malawi. BMC Med Res Methodol. 2014;14:29. https://doi.org/10.1186/1471-2288-14-29.
Acknowledgements
The World Health Organization Global Maternal Sepsis Study (GLOSS) is a research project implemented by the WHO in a global network of health facilities between 2017 and 2018. This project is part of the WHO response to the Sepsis resolution adopted by the 70th World Health Assembly (2017). We sincerely thank the women who participated in this study. WHO is grateful to the extensive network of institutions and individuals who contributed to the project design and implementation, including researchers, study coordinators, data collectors, data clerks, and other partners including the staff from the Ministries of Health and WHO offices. We would like to thank Allisyn Moran (Scientist at the World Health Organization (WHO) in the Department of Maternal, newborn, Child, and Adolescent Health (MCA)) and Marian Knight for their comments on this manuscript.
WHO Global Maternal Sepsis Study- Maternal Death and Near-miss Review Working Group.
Benin: Sourou Goufodji Keke, Pascal Sedami. Burkina Faso: D. Vincent Batiene, Kadari Cisse, Evelyne Béwendin Komboigo, Henri Gautier Ouedraogo. Ethiopia: Abdulfetah Abdulkadir Abdosh, Rahel Demissew, Biruck Gashawbeza, Ayalew Mariye, Thomas Mekuria, Filagot Tadesse, Fikremelekot Temesgen, Alula M. Teklu, Dawit Worku. Ghana: Richard Adanu, Kwame Adu-Bonsaffoh, Philip Govule, Charles Noora Lwanga, Ama Asantewa Tamatey. Guatemala: William Enrique Arriaga Romero, María Guadalupe Flores Aceituno, Ligia María Palma Guerra. Honduras: Carolina Bustillo, Rigoberto Castro, Carlos Alberto Ochoa Fletes, Bredy Lara. Kenya: George Gwako, Alfred Osoti, Zahida Qureshi. Malawi: Luis Gadama. Morocco: Zaynab Alaoui, Bouchra Assarag, Hassan Chrifi, Rachid Moulki, Iatimad Moutaouadia. Myanmar: Hla Mya Thway Einda, Thae Maung, Myint Moh Soe, Khaing Nwe Tin. Nigeria: Olubukola Adesina, Chris Aimakhu, Olufemi Aworinde, Bukola Fawole. Philippines: Zenaida Dy Recidoro. Sri Lanka: Hemali Jayakody, Kapila Jayaratne, Dhammica Rowel, Hemantha Senanayake. Zimbabwe: Mugove Madziyire, Thulani Magwali, Stephen Munjanja. External Review Committee Chairs: Luc de Bernis, Louise Tina Day, Matthews Mathai, Edgar Ivan Ortiz, Priya Soma-Pillay. Coordinating Unit: Mercedes Bonet, Obiageli Okafor, Nathalie Roos.
Funding
This study is financially supported by the UNDP–UNFPA–UNICEF–WHO–World Bank Special Programme of Research, Development and Research Training in Human Reproduction, Department of Sexual and Reproductive Health and Research, WHO, Geneva, Switzerland (project A65787). The GLOSS study also received support from Merck Sharp & Dohme, a wholly owned subsidiary of Merck (Kenilworth, NJ, USA), through its Merck for Mothers programme, and the United States Agency for International Development (grant GHA-G-00-09-00003). The views of the funding bodies have not influenced the content of this manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
MB conceptualized the study and developed the study protocol with inputs from OO, NR and the GLOSS research group. AAA, WAR, OAw, BA, RC, HC, PG, ZQ, MGM, HGO, KNT, KJ and DR led the acquisition of data. OO managed the data collection. OO, NR and MB planned and coordinated the external review meetings, OO and NR drafted the manuscript with substantial input from MB. LdB, LTD, MM, EO, and PSP led the external review meetings and commented on previous versions of the manuscript. AAA, OA, ZA, WAR, BA, OAw, RD, MGFA, LG, BG, SGK, GG, KJ, EK, BL, MGM, RM, IM, SM, CAOF, ZQ, ZDR, HS, KNT, PS, and DW participated in the external review meetings and commented on previous versions of the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the World Health Organization Ethical Review Committee on May 23, 2019 and obtained all required authorizations at country and institutional level. The study was performed in accordance with the ethical standards of the institutional and/or national research committee and principles of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary appendix to “International virtual confidential reviews of infection-related maternal deaths and near-miss in 11 low- and middle-income countries – Case report series and suggested actions. Study forms used for data collection and during the external review meetings. Results of a baseline assessment of maternal death review (MDR) committees and practices in participating GLOSS facilities. Additional information on the causes of deaths and distribution of modifiable factors described in this study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Okafor, O., Roos, N., Abdosh, A.A. et al. International virtual confidential reviews of infection-related maternal deaths and near-miss in 11 low- and middle-income countries – case report series and suggested actions. BMC Pregnancy Childbirth 22, 431 (2022). https://doi.org/10.1186/s12884-022-04731-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-04731-x