Abstract
Background
Home postpartum care is a major part of midwifery care in Germany. The user perspective plays an increasingly important role in the evaluation of health services, but there is a lack of valid and theoretically based measuring instruments, especially in midwifery care. The aim of this study was to develop and validate an instrument for measuring quality of midwifery care in the postpartum period from the perspective of women.
Methods
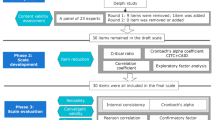
The following steps were taken to achieve this: (1) definition of the goals of midwifery work; (2) literature-based item development; (3) item selection based on a pre-test (n = 16); (4) item reduction and investigation of factor structure by means of explorative factor analysis (EFA; n = 133);(5) second EFA (n = 741) and confirmatory factor analysis (CFA; n = 744) based on a split representative sample survey; (6) hypothesis-based testing of correlations to sociodemographic characteristics of women and to characteristics of care.
Results
Measurement of Midwifery quality postpartum (MMAYpostpartum) consists of three scales with a total of 17 items which were found to have acceptable internal consistency: Personal Control (Cronbach’s alpha = .80), Trusting Relationship (Cronbach’s alpha = .87) and Orientation and Security (Cronbach’s alpha = .78). CFA verified and confirmed three factors: CFI = .928, TLI = .914, RMSEA = 0.073.
Conclusion
MMAYpostpartum is a predominantly valid, reliable short tool for evaluating the quality of midwifery care postpartum. It can be used to evaluate midwifery care, to compare different care models and in intervention research. It thus supports the orientation of midwives’ work towards the needs of women and their families.
Similar content being viewed by others
Background
In Germany, midwives support women from the beginning of pregnancy until the end of breastfeeding. During pregnancy, they have a secondary role compared to obstetricians. During childbirth, a midwife must be present by law. In most cases, gynecologists are also present and delivery rooms are supervised by gynecologists. Most women go home 3 to 5 days after giving birth. Postpartum home care is exclusively offered by midwives.
Women can receive up to 36 home visits postnatally and during the breastfeeding period [1]. In Germany, 92.8% of women use home-based care provided by a midwife in the postpartum period, with lower use in vulnerable groups.
It typically involves an average of 12 visits (SD ± 5.7), of 38.8 min duration (SD ± 17.4) and continues for up to 9 weeks after birth (SD ± 3.7) or until the end of the breastfeeding period [2]. Care during this period is offered by freelance midwives. It is currently not subjected to formal evaluation (or quality control).
The user’s perspective plays an increasingly important role in the evaluation of health services [3]. Evaluation from the user’s perspective appears to be particularly important in the area of home postnatal care. There is an explicit public health expectation in Germany that women and their families receive postpartum care. It is intended to support breastfeeding and help at risk women and families, as this phase of life is particularly important for the later health of the child [4]. Allowing home visits necessitates a special relationship of trust between women, families and the midwife, however.
Several instruments involving the user perspective to measure the level of satisfaction or the experience of midwifery care have already been developed [5,6,7,8,9,10]. A number of problems have been identified with these tools, however. For example, they are not very sensitive [11, 12], and satisfaction depends on the expectations of the user and tends to be measured on an emotional-affective level, and midwifery care evaluated from a “consumer experience” perspective [11, 13].
In contrast, very few instruments have been developed to measure the quality of midwifery care from a users’ perspective. In the field of midwifery, there is one instrument for measuring quality in antenatal care (QPCQ [11];, and one for measuring quality during pregnancy and childbirth (PCQ) [14]. No instrument for measuring quality in postpartum care was found in a scoping review [15].
Quality is understood here as the extent to which objectives are achieved in various defined dimensions of a health service [16, 17]. The dimensions of midwifery care are understood comprehensively. Topics such as disrespect and abuse/respectful care are just as important as health and medical topics or to give orientation for women and families in a potentially challenging life situation.
The measurement of quality can be used by professionals to evaluate, develop and professionalize their own work. It can also be used to compare different models of care or for evaluation within intervention research. In addition, midwives in Germany are required to evaluate their work, however no validated instrument is available yet [18].
A theory-based, valid and reliable assessment tool for quality in postpartum midwifery care from the point of view of women as users is needed.
Method
The aim of this study is to develop and validate an instrument for measuring quality of midwifery care in the postpartum period from the perspective of women. For this purpose, the usual steps for questionnaire development and validation were followed.
The validation of the questionnaire took place as part of the study HebAB.NRW - Midwifery Care in North Rhine-Westphalia. The study was funded by the Landeszentrum für Gesundheit, NRW (LZG.NRW; funding code: LZG TG 72001/2016) [2]. The Ethics Committee of the University of Applied Sciences, Hochschule für Gesundheit in Bochum, approved the study. The authors are midwifery scientists and health scientists. Two of the authors have worked as midwives in the past.
An instrument for quality assessment during birth has also been developed and is currently under review.
Phase one: Theoretical foundation
In this work quality was defined as the extent to which objectives are achieved. In order to be able to measure this, the objectives of midwifery were first defined. To this end, a systematic literature search was carried out on the objectives and concepts of midwifery and on the needs and wishes of women regarding midwifery care. The Walker and Avant method of theory construction [19] was used to develop a theory on the aims and purpose of midwifery. The procedure and results have been published in detail elsewhere [20].
Phase two: item generation and selection
Items were developed for each of the midwifery goals defined in phase one. The wording of the items was guided by the literature on women’s needs for midwifery care. The literature from Phase 1 was used for this purpose.
A pre-test of the item list was performed with nine new mothers, five midwifery scientists and two midwives. The items were evaluated for clarity, relevance, acceptability, importance and freedom of overlap. Where appropriate, items were reformulated or removed.
Items were scored on a five-point Likert scale with a neutral centre in order to avoid systematic distortion by undecided or neutral participants. Due to the potential for ambiguous research results, a “not sure” category was omitted. The possible answers were as evenly distributed as possible and were as follows: “not applicable at all”, “not applicable”, “neither”, “applicable” and “fully applicable” [21].
Phase three: item reduction and investigation of factor structure
Sampling
Since there were no prior assumptions about the data structure on which to base a power analysis and due to the small number of expected factors, a minimum sample size of 100 women was aimed for [22].
For this purpose, a convenience sample was used, with recruitment via a freely accessible link on social media. This allowed uncomplicated and low-threshold access to a diverse sample. Included were women over 18 years of age who had given birth to a child in the last 12 months, had taken advantage of postnatal midwifery care and given informed consent to participate. The items were presented in a randomized order to exclude sequence effects. The survey was conducted online with the software Unipark.
Data analysis: exploratory factor analysis (EFA)
Exploratory factor analysis (EFA) was used to reduce the number of items. A principal axis factoring analysis with Varimax rotation was performed using SPSS 24.0. The suitability of the data for a factor analysis was checked for using the Kaiser-Meyer-Olkin criterion (KMO > .5) and the significance of the Bartlett test of sphericity. Factors with an eigenvalue greater than 1 were selected.
Items whose level of difficulty was judged too low (<.20) or too high (>.80) were viewed critically, as were items which did not sufficiently load on the primary factor (< .50), or whose crossloadings were too high (> .45). In addition, attention was paid not only to the statistical parameters, but also to how well the item’s content fit the factors during selection. The internal consistency of the scales was evaluated using Cronbach’s Alpha (α), with an internal consistency of α < .75 being considered unacceptable.
The factor structure of the reduced number of items was examined using the principal axis factoring analysis with Varimax rotation.
Phase four: questionnaire validation and determination of psychometric properties
Sampling
Phase four was conducted as part of a comprehensive study of the accessibility of midwifery care for women in North Rhine-Westphalia which took place between 01.02.2018 and 15.06.2018. In a retrospective cohort study, 45 of the 146 obstetric departments in North Rhine-Westphalia (NRW) were randomly selected. Twenty-seven clinics gave their consent to recruitment. North Rhine-Westphalia is the most populous state in Germany (17.9 mill. Inhabitants; ranked 7th in GDP per capita; ranked 11th in unemployment rate in Germany) [23].
Participants were asked about utilization, access, continuity and availability of midwifery care, as well as empowerment, self-rated health and use of e-health. The survey took place four to 12 months after birth. This period was chosen in order to generate a sufficiently large sample. The survey was started only 4 months after childbirth, so that an retrospective assessment of the quality of care in the postpartum and breastfeeding period was possible.
The women could participate online or by mail. It was also possible to participate online via open access for women who fulfilled the inclusion criteria but gave birth in a non-participating hospital. This opportunity was offered because the recruitment rates were lower than expected and there was also public interest in participation. Inclusion criteria were the provision of informed consent, having given birth in NRW during the survey period, age over 18 years and the use of midwifery postpartum care. The online survey was conducted with Unipark software.
Data analysis: confirmatory factor analysis (CFA)
Based on the existing data it was assumed that the implementation of the first EFA was not sufficiently stable due to the small sample size. Therefore the second large sample was divided into two subsamples to perform a cross-validation [24, 25]. An EFA was carried out on the first sub-sample andhe CFA on the second subsample.
Questionnaires with more than two missing items per scale were removed. In those missing one item it was replaced by the scale mean.
The final scale was then tested using Confirmatory Factor Analysis (CFA) using R 3.5.3. to test the relationship between the manifest variables and the underlying latent construct. The following quality criteria were used to ensure the construct validity (range in literature):
Comparative Fit Index (CFI > .90; .97), Tucker-Lewis Index (TLI > .90), goodness of fit index (GFI > .90; .95), adjusted goodness of fit index (AGFI > .85; .90), Standardized Root Mean Square Residual (SRMR <..10; .05), Root Mean Square Error of Approximation (RMSEA <.08; .05), Chi2/df < 3,0; 2,0, Factor Reliability (FR > 0.6), Average Variance Extracted (AVE > 0.5) [26, 27].
The internal consistency was determined using Cronbach’s alpha for the subscales and the overall scale, as well as Cronbach’s alpha if item deleted from subscale. There was no way to determine the criterion validity, as there is no gold standard for measuring quality of midwifery care in the postpartum period from the perspective of women.
Phase five: construct/convergent validity
Whether there are differences between specific characteristics of women and maternity care and the MMAYpostpartum score was examined. For this purpose, the cases were dichotomized into those below the 25th and those above the 75th percentile of the MMAYpostpartum score.
It was hypothesized that the MMAY score would not correlate to the personal characteristics of the woman or child or with the number or duration of postpartum visits. In contrast, it was hypothesized that the MMAY score would correlate positively with satisfaction regarding the number of visits. Furthermore, the women were classified according to whether they had made negative comments on postpartum care in a free text section of the questionnaire. Negative comments were expected to correlate negatively with the MMAY score.
The entire sample of the second survey was therefore used. Variables of interest were dichotomized. Odds ratios were calculated and Pearsons Chi2 was used to test the significance of the correlations.
The following variables were included in the analysis. Characteristics of the woman/child: Urban/rural resident, born in Germany, German native speaker, vocational training, university entrance qualification, annual income above 2.500 € (~ 2.718 US$), multipara, spontaneous vaginal birth, twins, premature birth, breastfeeding, self-rated health (SF-1 [28]), self-rated health of child, self-rated mental health postpartum, self-rated physical health postpartum.
Characteristics of care: place of birth, antenatal care by a midwife, satisfaction with the number of postpartum visits, number of postpartum visits, duration of care in weeks, and private health insurance.
Results
The results of the six phases are presented below.
Phase one: development of a theoretical foundation
The theory of the goals and purpose of midwifery work is described in a three-level model. On the first level, the aim is to establish a Trusting relationship. This promotes the three goals on the second level: Security, Personal control and Orientation. These serve the purpose of midwifery on the third level, the Promotion of the reproductive capabilities of women and families. The theory thus shows a total of four goals of midwifery care (see Fig. 1).
Hierarchical model of the means and targets of midwifery from [20] [Picture quote]
Phase two: item generation and selection based on a pre-test
On the basis of phase one, 145 items were developed. These were then revised based on comments made in the pre-test and reduced to 90.
Phase three: item reduction and investigation of factor structure
Sample I
One hundred thirty-three women met inclusion criteria and took part in the online random sample (convenience sample). Sociodemographic and anamnestic data are shown in Table 1. It is noticeable that there is a small proportion of women with a migrant background and a small proportion of first-time mothers. The proportions of twin births and premature births do not reflect those in statistical routine data.
Data analysis: EFA
The results of the KMO criterion (0.91) and the Bartlett test (p < 0.00) were considered suitable for conducting the initial EFA for item reduction. There were 12 factors with an eigenvalue > 1. This solution explains a variance of 78.1%, with the first factor explaining 56.79% of the total variance. Items were reduced from 90 to 17 as described above.
A further EFA was carried out to investigate the factor structure. The EFA of the remaining 17 items showed a KMO criterion of 0.93 and a significant Bartlett test (p < 0.00). Three factors with an eigenvalue > 1 yielded a variance explanation of 65.63%, with the first factor explaining 50.97% of the total variance. The factor loadings are shown in Table 2.
This solution primarily shows the theoretically postulated factors. In the factor analysis it was not possible to distinguish between the two theoretically separate factors safety and orientation. The factors Personal Control (FPC) and Trusting Relationship (FTR) contain five items each and demonstrate good internal consistency (FPC: α. =.89; FTR: α. =.86). The factor Security and Orientation (FSO) contains seven items and displays good internal consistency of α. =.84. The internal consistency of the entire scale was rated very good (α. = .93).
Phase four: questionnaire validation and determination of psychometric properties
Sampling
Three thousand one hundred one women gave their consent to participate in the HebAB.NRW study between 01.02.2018 and 15.07.2018. One thousand eight hundred seventy-three women completed the questionnaire, 1649 received postpartum care and 1485 (79.25%) could be included in the analysis of the scale.
The sample contains a relatively high proportion of women with high socioeconomic status (income, education) and with no migrant background. The two sub-samples do not differ significantly in sociodemographic and obstetric characteristics [Table 1].
Data analysis: EFA
The data (n = 741) was deemed suitable for EFA, based on the KMO criterion of 0.90 and a significant Bartlett-Test (p < 0.00). Three factors with an eigenvalue > 1 were found, showing a variance explanation of 55.09%; the first factor has a variance explanation of 23.65%. The results are shown in Table 2.
On the basis of the EFA and content aspects, the allocation of items to the scales Personal Control and Trusting Relationship was revised. Items 15 and 16 had very low loadings on all factors. Item 15 asked whether the midwife took into account the culture or religion of the woman. This item was retained because of its importance in terms of content. Item 16 asked whether the woman was able to choose a midwife. It was removed as a factor because of the loads and the difficulty of fitting the content to a factor.
Data analysis: CFA
The 16 item model and the revised factor structure were verified using a CFA with a sample of n = 744. The CFA confirmed an adequate model of fit. The fit indices for the final model were CFI = 0.928, TLI = 0.914, GFI = 0.94, AGFI = 0.91, RMSEA = 0.073, SRMR = 0.053, Chi2/df = 4.951, FR = 0.82 to 1.39 and AVE = 0.33 to 0.40. The model fit is therefore above the limit of < 2.5 and the AVE is too low. All other quality criteria are fulfilled.
Phase five: construct/convergent validity
The data were examined for correlations between extreme values of the MMAYpostpartum score (<25th; >75th percentile) and characteristics of women/children and maternity care (n = 704; Table 3).
Women who were satisfied with the number of postpartum visits were significantly less likely to rate the care as poor. Women who had made negative comments in free text fields were more likely to rate the midwifery care as poor. This difference was not significant, but also had low cell occupancy.
As hypothesized, for most variables no significant correlations were found. Contrary to the assumptions made, there was a correlation between mother tongue (significant) and country of birth (not significant) and the assessment of the quality of care in the postpartum period. Women of a migrant background were less likely to rate the quality as poor. Contradictory and non-significant tendencies were found with regard to university entrance qualification and professional training and the assessment of quality. There was also a non-significant tendency for women who had given birth in a hospital to report poorer quality than women who had not.
Characteristics of final scale
Measurement of Midwifery quality – MMAYpostpartum measures the quality of midwifery care with 16 items in three scales. Trusting Relationship measures whether the midwife is empathetic and respects the individual situation of the woman so that a trusting relationship can develop. This also includes good communication and organizational aspects. Orientation and Security measures the practical assistance and information provided in a potentially new and challenging life situation. In addition, it measures whether the midwife provides security by protecting and promoting the mental and physical health of the woman and her child. The subscale Personal Control measures the involvement of women in decision-making and the feeling that their own sovereignty and integrity are respected.
The scales and their properties are shown in Table 4. The scale Trusting Relationship is the only scale in which the possible range is not completely filled by the observed data. The internal consistency of the subscales and the total scale, with Cronbach’s Alpha ranging from α. =.78 to α. =.87, is acceptable to good. The properties of the individual items are described in Table 5. Two items were kept for content reasons, although deleting the item from the subscale would have improved Cronbach’s alpha.
Discussion
This study aimed to develop the first reliable and valid instrument for the assessment of the quality of home midwifery care postpartum. The MMAYpostpartum contains 16 items in three scales: Trusting Relationship, Orientation and Security, and Personal Control.
Overall, MMAYpostpartum demonstrates good reliability and validity with small weaknesses.
The content validity is estimated to be very high. Thus, a literature-based theory on the aims and purpose of midwifery work was carefully prepared especially for the development of the quality scale. The scales and items were then developed on the basis of this theory. In addition, the items and scales were evaluated by midwives and midwifery scientists before the pre-test. The face validity is supported by the item evaluation, which was carried out by mothers in the pre-test.
Exploratory and confirmatory factor analysis was performed to investigate construct validity and the internal relationship of the data. Differences in the assignment of items to the factors Trusting Relationship and Personal Control were found between the first and the second sample. The first sample was not representative and had a rather small number of participants, so it is thought that this could be responsible for the differences. The factor structure should therefore be investigated in further studies. The low values in AVE and slightly too high values in model fit could represent variances in the empirical data that are unexplained by the model. It is noted that these values were worse [6] or were not reported [11, 12, 14] in previous instruments developed to measure satisfaction, experience or quality from women’s points of view.
Two theoretically postulated factors (Orientation and Security) could not be separated empirically. This may indicate that this is a professional distinction made by midwives in their work, but that women do not distinguish between these two factors.
However, the data analyses clearly support the existence of three factors in overwhelming agreement with the theory, and the usual quality criteria, such as CFI, TLI and RMSEA, turned out well and support the construct validity of MMAYpostpartum.
Criterion validity was examined on the basis of postulated correlations to other items of the HebAB.NRW study, which were collected in connection with the MMAYpostpartum Score. The hypotheses were largely confirmed, so that the MMAY postpartum score predominantly shows no correlation with personal characteristics or with characteristics of care. Instead, it measures a construct of its own. As hypotheses, there is a logical connection between the assessment of quality of care and satisfaction with the quantity of care. However, a non-postulated connection between characteristics of a migrant background and the evaluation of quality was found. This should be investigated further. A non-significant trend was shown by the fact that women who had given birth in hospital more often rated the quality of postpartum care as poor than women who had given birth outside the hospital. This could be due to the fact that women in Germany who do not give birth in hospital are more likely to receive continuity of care or carer than women who give birth in hospital. In some cases, the cell populations were too small to make valid statements.
Good reliability in terms of internal consistency is supported by good Cronbach Alpha values.
Our study also has limitations. The questions are adapted to the German health system and were evaluated in Germany. The sample was not fully representative in sociodemographic terms. In addition, it was not possible to test the correlations with existing instruments. And no test-retest measurement to support reliability over time was possible due to the study design. The main strengths are to be found in the careful theoretical work done in advance, and in the rigorous execution of the statistical analyses.
Conclusion
The 16 item MMAYpostpartum questionnaire is a predominantly valid, reliable short tool for evaluating the quality of midwifery care postpartum. It can be used to evaluate the work of midwives (or midwifery teams), to compare different care models and in intervention research. It thus supports the orientation of midwives’ work towards the needs of women and their families.
Availability of data and materials
Raw data of the Scala MMAYpostpartum can be requested from MP.
Abbreviations
- AGFI:
-
Adjusted Goodness of Fit Index
- AVE:
-
Average Variance Extracted
- CFA:
-
Confirmative Factor Analysis
- CFI:
-
Comparative Fit Index
- df:
-
Degrees of freedom
- EFA:
-
Explorative Factor Analysis
- FR:
-
Factor Reliability
- FPC:
-
Factor Personal Control
- FTR:
-
Factor Trusting Relationship
- FOS:
-
Factor Orientation and Security
- GFI:
-
Goodness of Fit Index
- KMO:
-
Kaiser-Meyer-Olkin
- LZG.NRW:
-
Landeszentrum für Gesundheit, NRW
- NRW:
-
North Rhine-Westphalia
- RMSEA:
-
Root Mean Square Error of Approximation
- SRMR:
-
Standardized Root Mean Square Residual
- SD:
-
Standard deviation
References
Anlage 1.3 Vergütungsverzeichniszum Vertrag nach § 134a SGB V; 2020. Available from: URL: https://www.gkv-spitzenverband.de/media/dokumente/krankenversicherung_1/ambulante_leistungen/hebammen/aktuelle_dokumente/Hebammen_Anlage_1.3_Verguetungsverzeichnis_ab_01.01.19.pdf. [cited 2020 Feb 26].
Peters M, Villmar A, Hering T, Bauer NH, Schäfers R. Einfluss von Migrationshintergrund und niedrigem sozioökonomischen Status auf die Nutzung von aufsuchender Wochenbettbetreuung in Deutschland; 2020.
Geraedts M, Drösler SE, Döbler K, Eberlein-Gonska M, Heller G, Kuske S, et al. DNVF-Memorandum III “Methoden für die Versorgungsforschung”, Teil 3: Methoden der Qualitäts- und Patientensicherheitsforschung. Gesundheitswesen. 2017;79(10):e95–e124. https://doi.org/10.1055/s-0043-112431 .
Kooperationsverbund gesundheitsziel.de. Nationales Gesundheitsziel: Gesundheit rund um die Geburt; 2017.
Shaban I, Mohammad K, Homer C. Development and validation of women’s satisfaction with hospital-based Intrapartum care scale in Jordan. J Transcult Nurs. 2016;27(3):256–61. https://doi.org/10.1177/1043659614550486 .
Sjetne IS, Iversen HH, Kjøllesdal JG. A questionnaire to measure women's experiences with pregnancy, birth and postnatal care: instrument development and assessment following a national survey in Norway. BMC Pregnancy Childbirth. 2015;15(1):182. https://doi.org/10.1186/s12884-015-0611-3 .
Thomas LH, McColl E, Priest J, Bond S, Boys RJ. Newcastle satisfaction with nursing scales: an instrument for quality assessments of nursing care. Qual Health Care. 1996;5(2):67–72. https://doi.org/10.1136/qshc.5.2.67 .
Panth A, Kafle P. Maternal satisfaction on delivery service among postnatal mothers in a government hospital, Mid-Western Nepal. Obstet Gynecol Int. 2018;2018:4530161.
Lomas J, Dore S, Enkin M, Mitchell A. The labor and delivery satisfaction index: the development and evaluation of a soft outcome measure. Birth. 1987;14(3):125–9. https://doi.org/10.1111/j.1523-536X.1987.tb01472.x .
Janssen PA, Dennis C-L, Reime B. Development and psychometric testing of the care in obstetrics: measure for testing satisfaction (COMFORTS) scale. Res Nurs Health. 2006;29(1):51–60. https://doi.org/10.1002/nur.20112 .
Heaman MI, Sword WA, Akhtar-Danesh N, Bradford A, Tough S, Janssen PA, et al. Quality of prenatal care questionnaire: instrument development and testing. BMC Pregnancy Childbirth. 2014;14(1):188. https://doi.org/10.1186/1471-2393-14-188 .
Camacho FT, Weisman CS, Anderson RT, Hillemeier MM, Schaefer EW, Paul IM. Development and validation of a scale measuring satisfaction with maternal and newborn health care following childbirth. Matern Child Health J. 2012;16(5):997–1007. https://doi.org/10.1007/s10995-011-0823-8 .
Vinagre MH, Neves J. The influence of service quality and patients’ emotions on satisfaction. Int J Health Care Qual Assur. 2008;21(1):87–103. https://doi.org/10.1108/09526860810841183 .
Truijens SEM, Pommer AM, van Runnard Heimel PJ, Verhoeven CJM, Oei SG, Pop VJM. Development of the pregnancy and childbirth questionnaire (PCQ): evaluating quality of care as perceived by women who recently gave birth. Eur J Obstet Gynecol Reprod Biol. 2014;174:35–40. https://doi.org/10.1016/j.ejogrb.2013.11.019 .
Peters M, Schäfers R. Systematic literature research on instruments for quality measurement of midwifes. Bochum; 2018. (Scientific Conference)
Deutsches Institut für Normung e.V. (Hrsg.). DIN EN ISO 9000ff - Qualitätsmanagementsysteme - Anforderungen: DIN EN ISO 9000ff. Beuth Verlag GmbH; 2016.
Petzold T, Walther F, Schmitt J. Wie ist Qualität im deutschen Gesundheitssystem definiert? Eine systematische Analyse deutscher Gesetzestexte und Richtlinien. Gesundh ökon Qual manag. 2018;23(04):194–204.
Sozialgesetzbuch V (SGB V). §134a: Versorgung mit Hebammenhilfe.
Walker LO, Avant KC. Strategies for theory construction in nursing. 5th ed. Boston: Prentice Hall; 2011.
Peters M, Kolip P, Schäfers R. A theory of the aims and objectives of midwifery practice: a theory synthesis. Midwifery. 2020;84:102653. https://doi.org/10.1016/j.midw.2020.102653 .
Menold N, Bogner K. Gestaltung von Ratingskalen in Fragebögen; 2014.
Jung S, Lee S. Exploratory factor analysis for small samples. Behav Res Methods. 2011;43(3):701–9. https://doi.org/10.3758/s13428-011-0077-9 .
Lexas: Wirtschaftsdaten der 16 Deutschen Länder. Online verfügbar unter https://www.laenderdaten.de/europa/deutschland/bundeslaender/wirtschaftsdaten.aspx. Accessed 18 Feb 2021.
Fabrigar LR, Wegener DT, MacCallum RC, Strahan EJ. Evaluating the use of exploratory factor analysis in psychological research. Psychol Methods. 1999;4(3):272–99. https://doi.org/10.1037/1082-989X.4.3.272 .
Worthington RL, Whittaker TA. Scale development research. Couns Psychol. 2006;34(6):806–38. https://doi.org/10.1177/0011000006288127.
Schermelleh-Engel K, Moosbrugger H, Müller H. Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Methods Psychol Res. 2003;8(2):23–74.
Little TD, Kline RB. Principles and practice of structural equation modeling. 4th ed. New York, London: The Guilford Press; 2016. (Methodology in the social sciences)
Bullinger M. Erfassung der gesundheitsbezogenen Lebensqualität mit dem SF-36-Health Survey. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2000;43(3):190–7. https://doi.org/10.1007/s001030050034 .
Acknowledgments
We are very grateful to all participants in the study who made the development possible and to all hospitals and midwives who collaborated in recruitment.
Funding
The study HebAB.NRW, where part of the data collection took place, was funded by the Landeszentrum für Gesundheit, NRW (LZG.NRW) (funding code: LZG TG 72 001/2016). The LZG.NRW is part of the German national health system. The authors received no specific funding for this study. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
MP did the planning, data collection and analysis and wrote the manuscript. RS and PK provided advice and evaluated the planning, data collection and analysis and the manuscript. All authors have read and approved the final manuscript.
Authors’ information
Mirjam Peters, Midwife, B.Sc. Psychology, M.Sc. Public Health, phD student Public Health.
Midwifery Research Associate, with a focus on client-centred health care and digitalization in the field of midwifery. Previous projects: Aims and purpose of midwifery, Quality measurement of midwifery, Human Rights in Childbirth, Early Pregnancy Loss, Supply situation in Germany, digitalization in midwifery.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of the University of Applied Sciences, Hochschule für Gesundheit in Bochum, and informed consent was obtained from all patients before inclusion. The consent to participate was given by signing the paper and pencil version and by clicking a checkbox in the online version.
Consent for publication
Not applicable.
Competing interests
The authors declare that no competing interests exist.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Peters, M., Kolip, P. & Schäfers, R. A questionnaire to measure the quality of midwifery care in the postpartum period from women’s point of view: development and psychometric testing of MMAYpostpartum. BMC Pregnancy Childbirth 21, 412 (2021). https://doi.org/10.1186/s12884-021-03857-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-021-03857-8