Abstract
Background
The prevalence of the World Health Organization (WHO) recommended infant feeding practices for HIV exposed infants is low in developing countries. There is no nationwide representative study was done in Ethiopia. Therefore, this study aimed to assess the pooled prevalence of WHO-recommended infant feeding practices among HIV-positive mothers in Ethiopia.
Methods
EMBASE, PubMed, Google Scholar, CINHAL, Web of Science, Cochrane library, and hand searches of references were extensively searched to find out the primary articles. This study was included in all primary articles published in peer review journals regarding the recommended infant feeding practices in Ethiopia. Reviewers were used a standardized Microsoft Excel format to extract the data and analyzed it with Stata 11 version software. The pooled prevalence of recommended infant feeding practices among HIV exposed infants was estimated by a random-effect model. The sources of variation between the studies were identified by the I 2 statistics test. Furthermore, the source of heterogeneity was checked by subgroup and meta-regression analyses. Sensitivity analysis was also carried out for included articles to identify extreme values that affect the outcome of pooled results.
Results
A total of twenty-one articles were included in this study. The random effect pooled prevalence of WHO-recommended infant feeding practices in Ethiopia was 82.76% (95% Confidence Interval [CI]: 75.4, 90.11) with the heterogeneity of I2 = 93.7 with a value of p < 0.001. The subgroup analysis result showed that the highest prevalence of WHO-recommended infant feeding practices was observed in the retrospective cohort study design, 89.45%, and the lowest prevalence was found in cross-sectional studies, 80.67%. Mothers who disclosed their HIV serostatus to their spouses OR = 2.88(2.27, 3.66) and attended antenatal care visits OR = 4.62(3.13, 6.83) were more likely to follow the WHO-recommended infant feeding practices than their counterparts.
Conclusion
Two out of ten HIV exposed infants received mixed feeding in Ethiopia. Health professionals should support and counsel HIV positive mothers to disclose their HIV serostatus to their spouses and advertisements in general or community health workers can get this message out to encourage using antenatal care services during the pregnancy period were recommended to increase the adoption of WHO recommended infant feeding practices and decrease their infant’s risk of morbidity, including HIV infection.
Similar content being viewed by others
Background
More than 37.9 million people are living with HIV in the globe and 1.7 million of them are children. A majority of these children are living in sub-Saharan Africa [1] and over one-hundred thousand children are living in Ethiopia [2]. The majority (90%) of the children have acquired HIV infection through vertical transmission and breastfeeding is the main route of transmission when there was no PMTCT care given to the exposed ones [1]. The magnitude of vertical HIV infection in Ethiopia due to breastfeeding to 18–24 months was 28% [2].
WHO has forwarded recommendations for the HIV-exposed infants to feed either exclusive breastfeeding or replacement feeding for the first 6 months of life with highly maternal antiretroviral therapy (ART) and ART prophylaxis for exposed neonates, followed by complementary feeding with continued breastfeeding through 12–24 months of age [3]. Although there is a risk of HIV infection through breastfeeding, the risk of mortality or morbidity also high if infants are taking replacement feedings [3]. In many resource-limited settings, infants who were not breastfed were up to six times more likely to die from diarrheal illnesses, malnutrition, and pneumonia [3]. Thus, breastfeeding is important for protection against other child infections, mal-occlusion helps to increase intelligence, prevent early childhood obesity and diabetes [4].
Different studies have assessed the prevalence of WHO-recommended infant feeding practices and associated factors among HIV exposed infants in Ethiopia [5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22]. The highest adoption of WHO-recommended infant feeding practices was found from research done in Addis Ababa, 98.5% [10] while the lowest level of practice was from Wolega, 36.4% [21]. These findings showed that there is great variability in the prevalence of WHO-recommended infant feeding practices across the country. Antenatal care visits [5,6,7,8,9,10,11,12,13,14,15,16,17,18], disclosure of HIV status to her spouse [5,6,7, 9, 11, 14, 15, 18], husband support [5,6,7], occupational status [5,6,7], place of delivery [4,5,6], insufficient milk [4], knowledge of mothers on infant feeding options [7, 10, 11], educational status of mothers [5,6,7, 9], being on ART [6], were some of the factors associated with the adoption of WHO-recommended infant feeding practices. Among these factors, antenatal care visits and disclosure of their HIV status to their spouses have selected due to the variability of their odds ratio in different study areas. Antenatal care visits odds ratio was high in a study done in Northwest Ethiopia OR = 11.2(5.34, 25.26), while lower odds ratio was seen in Debre Markos, OR = 2.12(1.12, 4.01) [6, 14]. Besides, the association of disclosure of mothers HIV status to their spouses and recommended infant feeding practices were supported with studies were done in [5, 6, 9, 14, 15], while studies were done in Addis Ababa and the southern part of Ethiopia did not support this finding [10, 18].
Although many different studies were done regarding the adoption of WHO-recommended infant feeding practices, there are fragmented and no representative study was done which determined the pooled prevalence of WHO-recommended infant feeding practices and its association with antenatal care visits and disclosure of mothers’ HIV status to their spouses in Ethiopia. Thus, this study was aimed to estimate the pooled prevalence of WHO-recommended infant feeding practices and its association with antenatal visits and disclosure of status to their spouse in the context of Ethiopia. This study finding would be an input for program planners and policymakers working on the area of PMTCT.
Method
Databases and searching strategy
The preferred reporting item for systematic reviews (PRISMA) guidelines was followed for this review [23]. All studies that reported recommended infant feeding practices were searched through CINAHL, PubMed, Google Scholar, EMBASE, and Cochrane library. The searching terms were “Exclusive breastfeeding”, “Exclusive replacement feeding”, “prevalence “Incidence”, “Burden”, Factors”, “Predictors”; “Recommended infant feeding practices”, “Determinants”, “HIV exposed infants”, Formula feeding and “Ethiopia”. The key words and the boolean operators term such as “OR” or “AND” or AND/NOT or AND, NOT were used in combination and separate manner. The initial search was done on October 19, 2019. The search was re-done on February 16, 2021, and no further papers were found.
Inclusion and exclusion criteria
Studies have been done on the prevalence of WHO recommended infant feeding practices and its associations with disclosure of mother’s HIV status to spouse and antenatal visits in Ethiopia, with cross-sectional, cohort study designs, and having full texts were included in this review. But, studies reported on single case study designs, published in books, and qualitative studies were excluded.
Operational definitions
WHO recommended infant feeding practices: HIV-positive mothers must practices either exclusive breastfeeding with maternal ART and appropriate ART prophylaxis for children or exclusive replacement feeding until the child reaches to the age of six-months old [5].
Data extractions and quality assessment
Joanna Briggs Institute Meta-Analysis of Statistics Assessment and Review Instrument (JBI-MAStARI) was used to critically appraise the quality of paper [24]. Clear definition criteria were included for the inclusion of the selection of the study participants, sample, outcome interest, confounding factors, statistical analysis methods, and consistent measurement of outcome variables [24]. The criteria were dealing before the extraction of the data. The quality of included studies was taken a mean score value of two independent reviewers. Components used to extract the data were primary author, year of the publication, study area, sample size, study design, region of the study, prevalence of recommended infant feeding practices, age of child, and response rate. Article inclusion, data extraction, and compared results were independently carried out by the reviewers. Finally, the disagreement was resolved by a consensus of the reviewer.
Data analysis
Data were extracted using Microsoft Excel and exported to Stata version 11 software for analysis. The variation between studies was assessed by the I2 statistic test [25]. Laird’s random-effects model was used to estimate the pooled prevalence of WHO-recommended infant feeding practices among HIV exposed infants in Ethiopia [26]. Subgroup analysis was done by study design to minimize the random variations between the point estimates of the primary studies. Furthermore, univariate meta-regression analysis was undertaken using sample size, study setting, study design, region, and publication date. The Logs odd’s ratio was used to determine the association between WHO recommended infant feeding practices with antenatal visits and disclosure of HIV status to her spouses.
Publication bias
Fill trim analysis and Egger tests were done for assessing publication bias [27].
Results
A total of 852 research articles with regard to WHO recommended infant feeding practices in Ethiopia were retrieved through SCOPUS, PubMed, Google Scholar, Web of Science, Cochrane library, and African journal of health sciences. Of this, 821 were excluded due to duplication and irrelevant and 10 articles were excluded after reviewing the abstract and title of the study. Finally, 21 studies were included in this review (Fig. 1).
Characteristics of the original studies
As described in Table 1, a total of 6575 HIV positive mothers enrolled in the prevention of mother to child transmission (PMCT) were included to estimate the pooled prevalence of WHO recommended infant feeding practices. Almost all (99.31%) mothers practiced WHO-recommended infant feeding practices from a study done in Oromiya and Amhara regions [29, 30] whereas the lowest prevalence (34.6%) was reported from a study done in the Oromia region [21]. In this meta-analysis, five out of nine regions of the country and 21 studies were included. From included studies, seven studies were from the Amhara region [5, 6, 8, 14, 22, 28, 30], six studies were from the Oromia region [6, 9, 13, 19, 21, 29], four studies were from Addis Ababa city [10,11,12, 17], three studies were from the SNNP region [15, 18, 20], and the remaining one study was from Tigray region [16]. A total of sixteen studies with cross-sectional and five studies with cohort study designs were included in this review (Table 1).
Publication bias
The publication bias was assessed by the Egger test. The result was − 0.20 (95% CI = 0.33, −.07) p = 0.06 which indicates there was not a statistically significant publication bias (Fig. 2).
Overall pooled prevalence of the adoption of WHO recommended infant feeding practices
A total of twenty-one studies were included in this review and the overall pooled prevalence of WHO-recommended infant feeding practices in Ethiopia was 82.76% (CI: 75.4, 90.11). A severe heterogeneity was observed across the studies (I2 =93.5, p-value = < 0.001). Subgroup analysis was done by region, sample size, and publication year and none of them showed statically significance except study design. Accordingly, a slightly higher level of WHO recommended infant feeding practices was observed in cohort studies (89.45%) while lower in cross-sectional studies (80.67%) (Fig. 3).
Meta-regressions
The univariate meta-regression analysis was done with study design, publication date, sample size, region, and study design to identify the source of heterogeneity between the studies. But, none of them were statistically significant (Table 2).
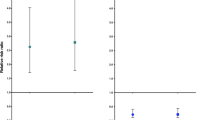
Association between antenatal care visits and safe infant feeding practice
Six studies were included to examine the association between antenatal care visits and WHO recommended infant feeding practices [6, 11, 14,15,16, 18]. The result showed that there is a significant association between antenatal care visits and WHO-recommended infant feeding practices. HIV positive pregnant mothers who attended antenatal care visits were 4.62 times more likely to adopt or follow WHO-recommended infant feeding practices (OR: 4.62, 95% CI: 3.13, 6.83) than counterparts. Moderate heterogeneity (I = 62.7% and p-value< 0.02) was observed across the included studies. The result of the Egger test indicated that there was a statistically significant publication bias (p < 0.001) (Fig. 4).
Association between disclosure of HIV status and WHO recommended infant feeding practices
Seven studies were included to determine the association between disclosure of mother’s HIV serostatus to their spouses and WHO-recommended infant feeding practices [5, 6, 9, 11, 14, 15, 18]. The result indicated that the pooled odds ratio of disclosure of HIV status was significantly associated with the WHO-recommended infant feeding practices (OR = 2.88 (2.27, 3.66). Due to the presence of severe heterogeneity across the studies (I2 = 78.1% and p-value =0.000), a random-effects model was employed to estimate the pooled effect. Moreover, Egger’s test was done to assess publication bias and it showed that not statistically significant, P = 0.149.
Discussion
Though the World Health Organization has recommended HIV positive mothers to practice either exclusive breastfeeding or replacement feeding for their exposed infant for the first 6 months of life, the practice was not satisfactory. The overall pooled prevalence practice of HIV positive mothers towards the adoption of WHO-recommended infant feeding practices in this study was 82.76% (CI: 75.4, 90.11). This finding is similar with studies done in Uganda, 79.4% [31], Nigeria, 87% [32], and Kenya, 88.1% [33]. However, it is higher than studies done in India, 67.1% [34], and Singapore, 62.02% [35]. The possible explanation might be due to difference in socio-demographic characteristics, study design, and cultural variability between the studies.
The result of this finding is lower than studies done in South Africa, 90% [36], Lesotho 97% [37], and South Sudan, 96% [38]. This difference might be due to culture variation related to feeding practices, socio-economic variation, knowledge gaps regarding exclusive breastfeeding, quality or time spent with mothers; duration or frequency of counseling by health care workers, and provider training or interest in providing infant-feeding option counseling services.
In sub-group analysis, the pooled prevalence of recommended infant feeding practice varies with study designs. Studies done with cohort study design show a slightly higher prevalence of recommended infant feeding practices, 89.45% compared to those conducted with cross-sectional study designs, 80.67%. This difference could be the cohort study design may better estimate the prevalence of recommended infant feeding practices.
The WHO recommended infant feeding practices were influenced by different factors. Mothers who attended antenatal care visits (> = 4) were 4.62 times more likely to practice recommended infant feeding practices than their counterparts. This finding is in line with studies done in Rwanda [39], Odisha [40], Botswana [41], and other sub-Saharan Africa countries [42]. This may be due to mothers receiving information and knowledge regarding infant feeding options during their ANC visits. Besides, the close interaction of mothers with health workers may increase psychosocial support regarding infant feeding practices.
Disclosure of the mother’s HIV serostatus to their spouse is also another determining factor of WHO-recommended infant feeding practices. Mothers who disclosed their HIV serostatus to their spouses were 2.28 times more likely to practice WHO recommended infant feeding practices than those who did not disclose. This finding is consistent with studies done in Nigeria [43] and South Africa [44, 45]. This might be due to mothers who disclosed their HIV serostatus to their spouses are more likely to receive comfort, support from their husbands, and feel relieved [46]. Additionally, it might have psychological benefits as they do not hide while formula feeding; disclosure may enable them to have a favorable attitude towards exclusive breastfeeding practice. Hence, mothers can practice freely when feeding their infant without fear and helps to reduce the practice of mixed feeding.
Strengths and limitations
Since it is the first review study, it may be used as a baseline to do further experimental research studies. The magnitude of outcome may be affected by other confounding variables because of recall bias and age-group of the children assessed.
Conclusions
Approximately two out of ten HIV positive mothers did not adopt WHO recommended infant feeding practice in Ethiopia. Health professionals should support and counsel HIV positive mothers to disclose their HIV serostatus to their spouses and encourage them to visit antenatal care services. Therefore, adopt WHO recommended infant feeding practices help to save their infants from the risk of morbidity as well as for the free survival of viral infections.
Availability of data and materials
Data will be available upon request of the corresponding author.
Abbreviations
- ANC:
-
Antenatal Care
- EDHS:
-
Ethiopian Demographic and Health Survey
- HIV:
-
Human Immune Deficiency Virus
- MTCT:
-
Mother to Child Transmission
- OR:
-
Odds Ratio
- PMTCT:
-
Prevention of Mother to Child Transmission
- WHO:
-
World Health Organization
References
World Health Organization. HIV/AIDS factsheet. WHO; 2019. https://www.who.int/docs/default-source/searo/myanmar/factsheet-hiv-aids-wad-2019.pdf?sfvrsn=ffebd469_0.3pm/2019.
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia demographic and health survey 2016: HIV report. Addis Ababa and Rockville: CSA and ICF; 2018.
World Health Organization. Guidelines on HIV and infant feeding 2010: principles and recommendations for infant feeding in the context of HIV and a summary of evidence. World Health Organization; 2010.
Victora CG, Bahl R, Barros AJ, França GV, Horton S, Krasevec J, Murch S, Sankar MJ, Walker N, Rollins NC, Group TL. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475–90.
Muluye D, Woldeyohannes D, Gizachew M, Tiruneh M. Infant feeding practice and associated factors of HIV positive mothers attending prevention of mother to child transmission and antiretroviral therapy clinics in Gondar town health institutions, Northwest Ethiopia. BMC Public Health. 2012;12(1):240.
Wakwoya EB, Zewudie TA, Gebresilasie KZ. Infant feeding practice and associated factors among HIV positive mothers in Debre Markos referral hospital east Gojam zone, north West Ethiopia. Pan African Med J. 2016;24.
Mengistu YG, Kedir M. Assessment of infant feeding practice among HIV positive mothers and HIV status of their infants in Adama hospital, Oromia regional state, Ethiopia, 2016. J Preg Child Health. 2017;4(346):2.
Sendo EG, Mequanint FT, Sebsibie GT. Infant feeding practice and associated factors among HIV positive mothers attending ART Clinic in governmental health institutions of Bahir Dar town, Amhara regional state, Ethiopia. J AIDS Clin Res. 2018;9:1.
Ejara D, Mulualem D, Gebremedhin S. Inappropriate infant feeding practices of HIV-positive mothers attending PMTCT services in Oromia regional state, Ethiopia: a cross-sectional study. Int Breastfeed J. 2018;13(1):37.
Maru Y, Haidar J. Infant feeding practice of HIV positive mothers and its determinants in selected health institutions of Addis Ababa, Ethiopia. Ethiopian J Health Dev. 2009;23(2).
Mukerem M, Haidar J. Assessment of the prevalence and factors influencing adherence to exclusive breast feeding among HIV positive mothers in selected health institution of Addis Ababa, Ethiopia. Ethiopian J Health Dev. 2012;26(3):169–75.
Mirkuzie AH. Correction: implementation and outcomes of guideline revisions for the prevention of mother-to-child HIV transmission in mother support Programme, Addis Ababa, Ethiopia. PloS one. 2018;13(7):e0200687.
Obsa S, Dabsu R, Ejeta E. Rate of mother to child transmission of HIV and factors associated among HIV exposed infants in Oromia regional state, Ethiopia: retrospective study. Egyptian Pediatric Association Gazette. 2018;66(3):61–5.
Esubalew F, Atenafu A, Abebe Z. Feeding practices according to the WHO-recommendations for HIV exposed children in Northwest Ethiopia: a cross-sectional study. Clin Nutr ESPEN. 2018;28:114–20.
Modjo KE, Amanta NW. Attitude and practice towards exclusive breast feeding and its associated factors among HIV positive mothers in southern Ethiopia. Am J Health Res. 2015;3(2):105–15.
Girma Y, Aregay A, Biruh G. Infant feeding practice and associated factors among HIV positive mothers enrolled in governmental health facilities in Mekelle town, Tigray Region, North Ethiopia. J HIV/AIDS Infect Dis. 2014;2(401):1–8.
Negash TG, Ehlers VJ. An assessment of the outcomes of prevention of mother-to-child transmission of HIV services in Addis Ababa, Ethiopia. Curationis. 2016;39(1):1–9.
Mengstie A, Tadese T. Assessment of factors associated with infant and young child feeding practices of human immunodeficiency virus (HIV) positive mothers in selected hospitals of southern nations, nationalities, and peoples region (SNNPR) Ethiopia. J AIDS HIV Res. 2016;8(6):80–92.
Wudineh F, Damtew B. Mother-to-child transmission of HIV infection and its determinants among exposed infants on care and follow-up in Dire Dawa City, eastern Ethiopia. AIDS Res Treatment. 2016;2016:3262746.
Tadele T, Tamiso A, Tadele T. Incidences and predictors of HIV positivity among infants who born from HIV positive mother who have follow up at two hospitals of southern Ethiopia, 2014. Sci J Public Health. 2014;2(5):431–9.
Bayissa ZB. Exclusive breast feeding status and its determinant among HIV positive women in West showa zone Oromia region Ethiopia. J AIDS Clin Res. 2017;8(1).
Berhan Z, Abebe F, Gedefaw M, Tesfa M, Assefa M, Tafere Y. Risk of HIV and associated factors among infants born to HIV positive women in Amhara region, Ethiopia: a facility based retrospective study. BMC research notes. 2014;7(1):876.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. https://doi.org/10.1136/bmj.b2700BMJ.
Munn Z, Moola S, Lisy K, Riitano D. The Joanna Briggs institute reviewers’ manual 2014. The systematic review of prevalence and incidence data. Adelaide: The Joanna Briggs Institute; 2014.
Rücker G, Schwarzer G, Carpenter JR, Schumacher M. Undue reliance on I 2 in assessing heterogeneity may mislead. BMC Med Res Methodol. 2008;8:79. https://doi.org/10.1186/1471-2288-8-79.
Jackson D, Bowden J, Baker R. How does the DerSimonian and Laird procedure for random effects meta-analysis compare with its more efficient but harder to compute counterparts? J Stat Plann Infer. 2010;140(4):961–70.
Borenstein M, Hedges LV, Higgins J, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. https://doi.org/10.1002/jrsm.12.
Dagnew AB, Tewabe T, Birhie A, Birehanu M, Alehegn T, Simachew A, Tsegaw A. Factors associated with compliance with World Health Organization-recommended infant-feeding practices by mothers with HIV infection in Northwest Ethiopia. Curr Ther Res. 2019;91:100568.
Demissie DB, Tadesse F, Bezabih B, Chala A, Kebede Y, Obsa G, Negewo J. Infant feeding practice and associated factors of HIV positive mothers attending prevention of mother to child transmission and antiretroviral therapy clinics in Shashemene Referal hospital. J Health Med Nurs. 2016;30:2422–8419.
Moges NA, Kassa GM, Boneya DJ. Rate of HIV transmission and associated factors among HIV-exposed infants in selected health facilities of east and west Gojjam zones, Northwest Ethiopia; retrospective cohort study. BMC Infect Dis. 2017;17(1):475.
Nabirye Z, Kiwanuka F, Nakaye Z, Kamurasi I, Tolulope AA. Mothers’ adherence to optimal infant and young child feeding practices in Uganda: a cross-sectional study. F1000Research. 2018;7:877.
Aishat U, David D, Olufunmilayo F. Exclusive breastfeeding and HIV/AIDS: a crossectional survey of mothers attending prevention of mother-to-child transmission of HIV clinics in southwestern Nigeria. Pan Afr Med J. 2015;22(1).
Lang’at PC, Ogada IA, Steenbeek A, Odinga G, Mwachiro MM. Do the feeding practices and nutrition status among HIV-exposed infants less than 6 months of age follow the recommended guidelines in Bomet County, Kenya? BMC Nutr. 2016;2(1):43.
Suryavanshi N, Jonnalagadda S, Erande AS, Sastry J, Pisal H, Bharucha KE, Shrotri A, Bulakh PM, Phadke MA, Bollinger RC, Shankar AV. Infant feeding practices of HIV-positive mothers in India. J Nutr. 2003;133(5):1326–31.
Leow TY, Ung A, Qian S, Nguyen JT, An Y, Mudgil P, Whitehall J. Exploring infant feeding practices: cross-sectional surveys of South Western Sydney, Singapore, and Ho Chi Minh City. BMC Pediatr. 2017;17(1):145.
Doherty T, Sanders D, Goga A, Jackson D. Implications of the new WHO guidelines on HIV and infant feeding for child survival in South Africa. Bull World Health Organ. 2011;89:62–7.
Olorunfemi SO, Dudley L. Knowledge, attitude and practice of infant feeding in the first 6 months among HIV-positive mothers at the Queen Mamohato Memorial hospital clinics, Maseru, Lesotho. Afr J Primary Health Care Family Med. 2018;10(1):1–2.
Lasuba AY. Infant feeding methods among HIV-positive mothers in Yei County, South Sudan. South Sudan Med J. 2016;9(3):56–9.
Påfs J, Musafili A, Binder-Finnema P, Klingberg-Allvin M, Rulisa S, Essén B. ‘They would never receive you without a husband’: paradoxical barriers to antenatal care scale-up in Rwanda. Midwifery. 2015;31(12):1149–56.
Basudev SA. Infant feeding practices among HIV positive women in selected health facilities of Odisha; 2015.
Ndubuka J, Ndubuka N, Li Y, Marshall CM, Ehiri J. Knowledge, attitudes and practices regarding infant feeding among HIV-infected pregnant women in Gaborone, Botswana: a cross-sectional survey. BMJ Open. 2013;3(11):e003749.
Horváth H, Taylor K. Couples HIV testing and counseling (CHTC): A review of national policies, programs and practices in 22 high-priority countries of sub-Saharan Africa since the 2012 publication of WHO’s CHTC guidance.
Aliyu MH, Blevins M, Audet CM, Kalish M, Gebi UI, Onwujekwe O, Lindegren ML, Shepherd BE, Wester CW, Vermund SH. Integrated prevention of mother-to-child HIV transmission services, antiretroviral therapy initiation, and maternal and infant retention in care in rural north-Central Nigeria: a cluster-randomised controlled trial. Lancet HIV. 2016;3(5):e202–11.
Doherty T, Chopra M, Jackson D, Goga A, Colvin M, Persson LA. Effectiveness of the WHO/UNICEF guidelines on infant feeding for HIV-positive women: results from a prospective cohort study in South Africa. Aids. 2007;21(13):1791–7.
Doherty T, Chopra M, Nkonki L, Jackson D, Greiner T. Effect of the HIV epidemic on infant feeding in South Africa: “when they see me coming with the tins they laugh at me”. Bull World Health Organ. 2006;84:90–6.
Aishat U, Olufunmilayo F, David D, Gidado S. Factors influencing infant feeding choices of HIV positive mothers in southwestern, Nigeria. Am J Public Health Res. 2015;3(5A):72–9.
Acknowledgements
Not applicable.
Funding
No specific funding was received for this study.
Author information
Authors and Affiliations
Contributions
AB: Conception of research protocol, study design, literature review, data extraction, data analysis, interpretation and drafting the manuscript. MD: Data analysis and reviewing the manuscript. AB, MD: Data extraction and quality assessment. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
I declared that we have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dagnew, A.B., Teferi, M.D. A systematic review and meta-analysis on adoption of WHO-recommended infant feeding practices among HIV positive mothers in Ethiopia. BMC Pregnancy Childbirth 21, 194 (2021). https://doi.org/10.1186/s12884-021-03662-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-021-03662-3