Abstract
Background
The current study aimed to estimate the prevalence of alcohol use identified as a risk factor during pregnancies by the antenatal care providers, resulting in live births in British Columbia (BC) and to examine associations between alcohol use, adverse neonatal outcomes, and pregnancy complications.
Methods
This population-based cross-sectional study utilized linked obstetrical and neonatal records within the BC Perinatal Data Registry (BCPDR), for deliveries that were discharged between January 1, 2015 and March 31, 2018. The main outcome measures were alcohol use identified as a risk factor during pregnancy, associated maternal characteristics, pregnancy complications, and adverse neonatal outcomes. Estimates for the period and fiscal year prevalence were calculated. Chi-square tests were used to compare adverse neonatal outcomes and pregnancy complications by alcohol use during pregnancy identified as a risk factor. Logistic regression was used to examine the association between alcohol use identified as a risk factor during pregnancy and adverse neonatal outcomes and pregnancy complications, after adjusting for identified risk factors.
Results
A total of 144,779 linked records within the BCPDR were examined. The period prevalence of alcohol use during pregnancy identified as a risk factor was estimated to be 1.1% and yearly prevalence was 1.1, 1.1, 1.3 and 0.9% from the 2014/2015 to 2017/2018 fiscal years, respectively.
Alcohol use identified as a risk factor was associated with younger maternal age, fewer antenatal visits, being primiparous, a history of mental illness, substance use and smoking.
Neonates with alcohol use during pregnancy identified as a risk factor had greater odds of being diagnosed with: “low birth weight (1000-2499g)” (ICD-10: P07.1; aOR = 1.25; 95% CI: 1.01, 1.53), “other respiration distress of newborn” (ICD-10: P22.8; aOR = 2.57; 95% CI: 1.52, 4.07), “neonatal difficulty in breastfeeding” (ICD-10: P92.5; aOR = 1.97; 95% CI: 1.27, 2.92) and “feeding problems, unspecified” (ICD-10: P92.9; aOR = 2.06; 95% CI: 1.31, 3.09).
Conclusions
The prevalence of alcohol use during pregnancy identified as a risk factor was comparable to previous estimates within the BCPDR. Identified prenatal alcohol exposure was associated with notable differences in maternal and neonatal characteristics and adverse neonatal outcomes. More consistent, thorough screening and prevention efforts targeting alcohol use in pregnancy are urgently needed in Canada.
Similar content being viewed by others
Background
Maternal consumption of alcohol during pregnancy is a well-known risk factor for adverse neonatal outcomes [1,2,3,4]. Estimated rates of alcohol consumption by women during pregnancy can vary depending on factors such as the population studied and data collection methods; however, overall global prevalence is estimated to be about 10% [5]. In recent years, the prevalence of alcohol use and binge drinking among women of childbearing age have been increasing in the majority of countries globally, including Canada [6].
Prenatal alcohol exposure (PAE) can affect multiple aspects of infant health and development [7,8,9]. Possible adverse neonatal outcomes associated with maternal alcohol consumption include congenital and physical abnormalities such as cardiovascular, musculoskeletal, and craniofacial defects [4, 9]; medical conditions such as respiratory distress and convulsions [10, 11]; and early care challenges such as sleeping and feeding problems [1]. PAE may also have an adverse effect on fetal growth for parameters such as weight, length, and head circumference; however, the research evidence for growth deficits is mixed, especially at low to moderate levels of exposure [12].
PAE does not appear to affect all pregnancies equally, suggesting that a number of additional factors may also be involved in neonatal outcomes. These may include the amount of alcohol consumed by the mother, nutrition, genetic factors, other prenatal exposures (e.g., tobacco, cannabis), pregnancy complications, and maternal attributes such as age, parity or existing health conditions [12, 13].
Data from the 2006 Maternity Experiences Survey suggested that in British Columbia (BC), 38% of pregnant women received prenatal care from obstetricians and gynaecologists, 52% received care from family physicians and general practitioners; and 10% from midwives and nurses [14]. Though health care services are free in Canada, prenatal care from obstetricians may be less accessible to women in rural and remote communities in BC, who often solely receive prenatal care from family physicians [15]. Canadian guidelines (2020) for screening and counselling for alcohol and pregnancy [16] suggest that all women should be screened for alcohol use. However, currently, differences exist between provincial/territorial prenatal care providers in implementing alcohol use screening [17,18,19], which makes the data on the prevalence of PAE incomparable across Canada.
Prenatal services in British Columbia (BC), Canada are administered at a population level by Perinatal Services BC (PSBC), a provincial agency mandated with the coordination of prenatal and newborn screening programs. PSBC collects and analyzes maternal and neonatal information using the British Columbia Perinatal Data Registry (BCPDR), a quality-controlled database containing clinical information on nearly 100% of births throughout the province of BC from all service providers and obstetric facilities. The BCPDR collects standardized data on antenatal, intrapartum, postpartum and neonatal information, including ICD-10 codes indicated at birth and neonatal encounters.
Using population-based data from the BCPDR [17], this study sought to estimate the prevalence of pregnancies in which maternal alcohol use was identified as a risk factor and examine possible associations between alcohol use in pregnancy, adverse neonatal outcomes, and pregnancy complications. In addition, the study examined maternal attributes and risk factors for alcohol use identified as a risk factor during pregnancy.
Methods
Data source
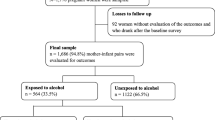
Maternal and neonatal records were obtained from PSBC for discharge dates between January 1, 2015 and March 31, 2018 [17]. Exclusion criteria for neonatal records included therapeutic abortions, stillbirths, unlinked maternal/infant records and records where the sex of the newborn was listed as unidentified.
Prenatal exposures, covariates and outcomes
Maternal alcohol use and binge drinking (four or more drinks per occasion) during pregnancy were recorded during antenatal visits when alcohol use was identified as a risk factor by the antenatal care provider. Alcohol use was initially identified through maternal self-report in most cases, but women only reported on alcohol use following pregnancy recognition. Information on binge drinking was available only among women with alcohol use identified as a risk factor during the respective pregnancy.
Other substance use was recorded during antenatal visits by the antenatal care provider only when it was identified as a risk, during the respective pregnancy. Data on substance use included heroin, methadone, cocaine, marijuana, prescription drugs, solvents, other drug use (such as non-prescription drugs including hallucinogens, stimulants, methylphenidate and designer drugs) and unspecified drug use. Recorded substance use included those used prior to and following pregnancy recognition.
Maternal cigarette smoking status was recorded during antenatal visits through self-report. If smoking was reported throughout or during part of the current pregnancy, the mother was considered a ‘current smoker’.
The following covariates were examined in this study: the maternal variables of prior neonatal death, stillbirths, prior low birthweight newborn and/or major congenital anomalies; maternal history of any mental illness; second-hand smoke exposure; and the neonatal variables of administration of oxygen, intermittent positive pressure ventilation (IPPV) mask and chest compression for resuscitation.
The following adverse neonatal outcomes and pregnancy complications were examined: “Fetal Alcohol Syndrome” (FAS) (ICD-10: Q86.0); “Fetus and newborn affected by maternal use of alcohol” (ICD-10: P04.3); 38 additional adverse neonatal outcomes identified through literature review on prenatal alcohol and other substance-exposed pregnancies (Supplementary File 1); pregnancy complications of bleeding < 20 weeks; antepartum hemorrhaging (bleeding ≥20 weeks); and intrauterine growth restriction (IUGR) (binary variable).
Maternal age during pregnancy was calculated by subtracting the maternal year of birth from the beginning of the fiscal year in which the birth occurred. Please see Supplementary File 2 for further information on data linkage and data cleaning performed in this study.
Statistical analysis
Yearly prevalence of pregnancies in which maternal alcohol use was identified as a risk factor was calculated as a sum of the number of alcohol-exposed births as indicated by alcohol use identified as a risk, divided by the total number of live births in each fiscal year. The period prevalence of pregnancies in which maternal alcohol use was identified as a risk factor was calculated for the entire study population by dividing the number of alcohol-exposed births by the total number of births during the study period (Jan 1, 2015 – Mar 31, 2018).
Statistical analyses were conducted using STATA 16 and R. Descriptive statistics were generated for demographic variables. Chi-square tests were used for testing relationships between categorical variables: alcohol-exposed and non-exposed pregnancies for pregnancy complications and adverse neonatal outcomes. Crude odds ratios were generated for pregnancy complications and adverse neonatal outcomes. Odds ratios (OR) were generated using Chi-square tests and conditional maximum likelihood estimation (Fisher) was used for comparisons where expected cell counts were below 5.
Logistic regression (LR) was used to identify risk factors for alcohol use during pregnancy. Variables in the data such as maternal demographic information, parity, number of living children, prior neonatal death, prior stillbirth, prior low birthweight newborn, prior congenital anomaly, history of mental illness and number of antenatal visits were included in the models. Previous literature has shown that these variables may be associated with adverse maternal and neonatal conditions related to PAE. As such, these variables, as well as maternal smoking status and any substance use, were treated as confounders and were adjusted for in LR models to produce adjusted odds ratios for associations between alcohol use identified as a risk during pregnancy and i.) pregnancy complications; and ii.) adverse neonatal outcomes. Variables below the threshold of α = 0.05 were included in this regression model.
Lastly, logistic regression was used to examine whether there was an association between binge drinking and the three neonatal outcomes with the greatest frequency, controlling for the variables included in the previous regression model.
Results
The final study population included 142,545 maternal records linked to 144,785 neonatal records that were discharged between January 1, 2015 and March 31, 2018 [17]. There were 6 observations that were excluded due to sex of the newborn being undifferentiated (n = 2), parity being unknown (n = 3) and maternal record with no corresponding neonatal record (n = 1), resulting in a final study population of 144,779 neonatal records. The average maternal length of stay in hospital was 61.37 h (2.5 days), there were 65,497 women (45.9%) who were primiparous, and the mean number of antenatal visits was 9.44 (Table 1).
Prevalence of pregnancies in which maternal alcohol use was identified as a risk factor
The prevalence of pregnancies wherein maternal alcohol use was identified as a risk factor by fiscal year in BC was 1.1, 1.1, 1.3 and 0.9% from the 2014/2015 to 2017/2018 fiscal years, respectively. There were 1593 alcohol-exposed neonates during the study period and 144,779 birth records; the resulting period prevalence of alcohol-exposed pregnancies in BC was 1.1 cases per 100 live births between January 1, 2015 and March 31, 2018.
Characteristics of mothers who consumed alcohol during pregnancy versus mothers who did not consume alcohol during pregnancy
Mothers with alcohol use identified as a risk factor during pregnancy were significantly younger, had a longer length of stay in hospital, had a lesser number of antenatal visits and had a greater number of antenatal hospital admissions prior to delivery, had higher rate of a prior neonatal death and a history of any mental illness compared to mothers with no alcohol use identified as a risk factor during pregnancy (Table 1). In addition, mothers with alcohol use identified as a risk factor during pregnancy had a statistically significantly greater proportion of any substance use, current, former and second hand smoking compared to mothers who reported no alcohol use during pregnancy.
Table 2 presents logistic regression output, which demonstrated that being primiparous compared to multiparous, a greater number of living children, and maternal history of any mental illness were all statistically significantly associated with greater odds of maternal alcohol use during pregnancy. Older maternal age and a higher number of antenatal visits were statistically significantly associated with lesser odds of alcohol use identified as a risk factor during pregnancy.
Adverse neonatal outcomes
Table 3 presents characteristics of newborns for the entire study population, stratified by alcohol use being identified as a risk factor by the antenatal care provider. On average, neonates with identified prenatal alcohol exposure were statistically significantly shorter at birth, had smaller head circumference, were less likely to be breastfed within the first hour of life and had higher rates of interventions: resuscitation/stabilization, oxygen for resuscitation, IPPV mask for resuscitation, than those who were alcohol non-exposed.
Table 4 presents overall counts of diagnoses received by newborns and counts stratified by maternal alcohol use identified as a risk factor during pregnancy. The 5 most prevalent ICD-10 diagnoses among all newborns were P07.1: “Other low birth weight (1000-2499g)” (5.5%), P28.5: “Respiratory failure of newborn” (4.3%), P05.9: “Slow fetal growth, unspecified” (2.7%), P92.8: “Other feeding problems of newborn” (1.6%) and P22.9: “Respiratory distress of newborn, unspecified” (1.4%).
There were 5 neonatal records (0.003%) with a diagnosis of “Fetal alcohol syndrome” (FAS; ICD-10: Q86.0) in total among children born in this time period. Interestingly, in 3 of the 5 corresponding pregnancies, alcohol use was not identified as a risk by the antenatal care provider. Additionally, there were 30 neonatal records (0.02%) with a diagnosis of “Fetus and newborn affected by maternal use of alcohol” (ICD-10: P04.3), and 12 out of 30 were not identified as alcohol-exposed based on the same criteria.
Compared to pregnancies without reported alcohol use, pregnancies with alcohol use identified as a risk factor were statistically significantly associated with a greater proportion of the following ICD-10 diagnoses: P04.3: “Fetus and newborn affected by maternal use of alcohol”; P05.9: “Slow fetal growth, unspecified”; P07.1: “Other low birth weight (1000-2499g)”; P22.8: “Other respiration distress of newborn”; P36: “Bacterial sepsis of newborn”; P92.5: “Neonatal difficulty in feeding at breast”; P92.9: “Feeding problems, unspecified”; P96.1: “Neonatal withdrawal symptoms from maternal use of drugs of addiction”; P96.8: “Other specified conditions originating in the perinatal period”; Q86.0: “Fetal alcohol syndrome (dysmorphic)”; and Q89.7: “Multiple congenital malformations, not elsewhere classified” (Table 4).
Table 5 presents the crude and adjusted odds ratios between prenatal alcohol exposure identified as a risk factor and each adverse neonatal outcome, adjusted for maternal age, maternal smoking status, any maternal substance use, parity, prior neonatal deaths, prior stillbirth and prior low birthweight newborn, maternal history of any mental illness and the number of antenatal visits.
After adjustment, neonates with prenatal alcohol exposure identified as a risk factor had 1.25 times greater odds (aOR = 1.25; 95% CI: 1.01, 1.53; p = 0.033) of being diagnosed with P07.1: “Other low birth weight (1000-2499g)”, 2.57 times greater odds (aOR = 2.57; 95% CI: 1.52, 4.07; p < 0.001) of being diagnosed with P22.8: “Other respiration distress of newborn”, 1.97 times greater odds (aOR = 1.97; 95% CI: 1.27, 2.92; p < 0.001) of being diagnosed with P92.5: “Neonatal difficulty feeding at breast”, 2.06 times greater odds (aOR = 2.06; 95% CI: 1.31, 2.92; p < 0.001) of being diagnosed with P92.9: “Feeding problems, unspecified” and 15.63 times greater odds (aOR = 15.63; 95% CI: 1.99, 79.37; p < 0.003) of being diagnosed with Q89.7: “Multiple congenital malformations, not elsewhere classified” compared to neonates without reported prenatal alcohol exposure (Table 5 and Fig. 1).
Forest Plot of adjusted Odds Ratios for the association between selected adverse neonatal outcomes and alcohol use during pregnancy identified as a risk factor. P04.3 - Fetus and newborn affected by maternal use of alcohol; P05.9 - Slow fetal growth, unspecified; P07.1 - Other low birth weight (1000-2499 g); P22.0 - Respiratory distress syndrome; P22.8 - Other respiratory distress of newborns; P22.9 - Respiratory distress of newborn, unspecified; P24.0 - Neonatal aspiration of meconium; P28.5 - Respiratory failure of newborn; P28.9 - Respiratory condition of newborn, unspecified; P29.9 - Cardiovascular disorder originating in perinatal period, unspecified; P36 - Bacterial sepsis of newborn; P90 - Convulsion of Newborn; P92.5 - Neonatal difficulty in feed at breast; P92.8 - Other feeding problems of newborn; P92.9 - Feeding problems, unspecified; P94.1 - Congenital Hypertonia; P96.1 - Neonatal withdrawal symptoms from maternal use of drugs of addiction; P96.8 - Other specified conditions originating in the perinatal period; Q05.9 - Spina bifida, unspecified; Q24.9 - Congenital malformations of heart, unspecified; includes anomaly or disease; Q35.9 - Cleft palate, unspecified; Q36 - Cleft lip without cleft palate; Q37 - Cleft lip with cleft palate; Q89.7 - Multiple congenital malformations, not elsewhere classified; Q89.9 - Congenital Malformation, unspecified; R25.1 - Tremor, unspecified; R62.8 - Other lack of expected normal physiological development; includes: failure to gain weight, failure to thrive, infantilism NOS, lack of growth & physical retardation; R68.1 - Nonspecific symptoms peculiar to infancy; includes: excessive crying of infant & irritable infant
Table 6 presents the adjusted odds ratios for the effects of binge drinking on adverse neonatal outcomes. The three most frequent adverse neonatal outcomes included: P05.9: “Slow fetal growth, unspecified”, P07.1: “Other low birth weight (1000-2499g)” and P28.5: “Respiratory failure of newborn”. Of the three outcomes evaluated, the only statistically significant association was between binge drinking and P28.5: “Respiratory failure of newborn”. Neonates whose mother reported binge drinking during pregnancy had 2.03 times greater odds (aOR = 2.03; 95% CI: 1.02, 4.10; p = 0.044) of being diagnosed with P28.5: “Respiratory failure of newborn” compared to those neonates whose mothers did not report binge drinking (Table 6).
Pregnancy complications
During the study period, there were 2712 (1.9%) pregnancies where bleeding < 20 weeks was reported, 1862 (1.3%) pregnancies where antepartum hemorrhage > 20 weeks was reported and 3460 (2.4%) pregnancies where IUGR was identified as a risk. There were no statistically significant differences in the prevalence or odds of pregnancy complications between prenatally alcohol-exposed and non-exposed pregnancies (Table 7).
Discussion
Main findings
The prevalence of alcohol use identified as a risk factor ranged between 0.9 and 1.3% among BC pregnancies in the years examined. While this is comparable to a prevalence estimate of alcohol use (any amount) of 1.8% from an Ontario birth registry [18], it is notably lower as compared to a regional estimate of alcohol use (any amount) of 10% in 2015 in Manitoba [19]; of which, the latter was based on post-delivery discharge follow-up by public health nurses [19]. This illustrates that provincial birth registries on their own, including PSBC, may be underestimating alcohol use behaviour during pregnancy, and post-partum measures may be able to collect more accurate information. The estimates based solely on birth registry information in BC and ON are remarkably lower compared to the 10% national prevalence estimate of alcohol use during pregnancy across Canada based on a meta-analysis of existing epidemiological studies, which included studies using self-report in survey responses [20]. There is heterogeneity between provinces in how data on alcohol use during pregnancy are collected and recorded, including the alcohol use definition and timing of data collection. Though birth registry data in BC and Ontario generate similar estimates, these data are not comparable: the BCPDR has operationalized alcohol use differently by emphasizing that alcohol use is not only self-reported, but also must be deemed a risk factor in the respective pregnancy [21] and is solely based on that which occurred following pregnancy recognition, captured in a binary data element.
This population-based study found specific maternal risk factors for alcohol use identified as a risk factor during pregnancy that may be useful for targeting education and prevention efforts such as mothers’ age, parity, prior neonatal death, and history of any mental illness. In addition, there was a greater prevalence of other substance use, current and former smoking status, and exposure to second-hand smoke among women with alcohol use identified as a risk factor.
Results also highlighted factors that might identify newborns with prenatal alcohol exposure who are at risk for low birth weight, respiratory distress, and feeding difficulties. Our results did not find any differences between neonates with and without identified prenatal alcohol exposure for the three pregnancy complications examined: bleeding before 20 weeks, antepartum hemorrhaging (bleeding ≥20 weeks) and IUGR. During the neonatal period, however, low birth weight (adjusted), shorter length, and smaller head circumference (unadjusted) were found to be more common for the alcohol-exposed group.
In this study, women with mean ages between 28 and 31 years were at higher risk for alcohol use identified as a risk factor during pregnancy. They were also more likely to be giving birth to their first child and to attend fewer antenatal care visits. Together, these factors indicate that women at risk for consuming alcohol in pregnancy may receive less healthcare support and information during pregnancy due to fewer medical encounters. This suggests that primary healthcare providers may wish to consider greater screening and possible referral to more extensive supports and education for women in this demographic. This is especially important if antenatal alcohol use behaviour in the first pregnancy is predictive of use behaviour while breastfeeding, or during subsequent pregnancies.
Interpretation
During the timeframe of this study, we found a period prevalence of 1.1% for pregnancies where alcohol use was identified as a risk factor. Prevalence for the prior year (2014/2015) in the same jurisdiction was 1.2% [22] and it has ranged over time from 1.3% in 2000/2001 [23] to 0.4% in 2012/2013 [24]. Although some research has suggested a trend towards declining rates of maternal alcohol consumption during pregnancy in both Canada and the United States [25, 26], the data are variable and complex due to factors such as the population studied, data collection methodology, and alcohol use definitions in each study. Globally, however, there is reason to believe that rates of alcohol-exposed pregnancies may be increasing overall [5].
All women who are pregnant or considering pregnancy should be engaged by their primary healthcare providers in discussion regarding substance use, possible harms, and interventions [3]. It may be especially important, however, to provide this guidance and support to first-time mothers, women in particular age-groups, and those with previous mental health issues, based on the findings in the current study. Previous research has reported that women with mental health issues receive less prenatal care than those without mental health issues [27], suggesting a complex relationship between mental health problems, obtaining prenatal care, and alcohol consumption in pregnancy. Women with a history of mental health issues may have an elevated risk for substance use for a number of reasons, including a history of trauma, interpersonal issues, or adverse psycho-social factors [28]. Embedding prenatal education, care, and support into mental health settings may be one possible direction for strategies aimed at reducing PAE and increasing engagement with antenatal healthcare services.
Interestingly, several maternal factors associated with alcohol use identified as a risk factor during pregnancy in this study were similar to those previously reported for cannabis use in pregnancy. Luke et al. [29] noted that a history of mental health issues was more common in women who used cannabis in pregnancy. They also found that the cannabis use group were more likely to use alcohol and tobacco as well, suggesting that much like in the present study, infants exposed to one substance were also frequently exposed to other substances, likely increasing their risk for adverse outcomes. Healthcare providers should therefore be encouraged to consider screening for additional substances if alcohol use is reported or suspected during pregnancy.
These findings may be reflective of the mixed results for growth deficits associated with PAE found in other studies [3, 30] or it may suggest challenges with growth were either not present or undetected in the earlier periods of pregnancy. Coles [2] noted that while some growth deficit can occur in the first and second trimester of alcohol-exposed pregnancies, a more pronounced deficit in weight, length, and head circumference occurs in the third trimester. In the context of this study, it could be that earlier healthcare encounters were less able to identify IUGR and only noted growth deficits at or after birth. As well, given that smoking is well known to influence fetal growth [30, 31] and 29.7% of the women in the study who had alcohol use identified as a risk factor also had concurrent tobacco use, compared to only 5.7% among women for whom alcohol use was not identified as a risk factor; therefore, it is possible that patterns of smoking affected or confounded growth results. Regardless, outcomes from this study suggest that even when growth deficits are not identified early in the pregnancy, primary care providers may wish to consider increased monitoring of fetus development in mothers who are believed to be tobacco and/or alcohol users.
Infants exposed to alcohol identified as a risk factor in this study also showed greater early difficulties with feeding, need for resuscitation, more congenital abnormalities, and longer hospital stays suggesting some important vulnerabilities and risks. Also, these infants were more often administered oxygen or IPPV and more often had problems initiating breastfeeding or were not breastfed at all. Binge drinking during pregnancy was significantly associated with “Respiratory failure of newborn” (ICD-10: P28.5), but not with “Slow fetal growth, unspecified” (ICD-10: P05.9) or “Other low birth weight (1000-2499g)” (ICD-10: P07.1). These results, however, should be interpreted with caution because the measure on binge drinking has not been validated.
Only a small proportion of infants with identified prenatal alcohol exposure as a risk factor, however, received a diagnosis of FAS. As well, many of the mothers of children identified as affected by alcohol at birth did not report alcohol use to their antenatal healthcare providers; this may indicate that alcohol use occurred before pregnancy recognition, it was simply omitted, or was never screened for. This presents a potential challenge for healthcare providers in identifying and channeling infants at risk into early intervention programs for PAE. According to the new Canadian diagnostic guidelines (2016) for Fetal Alcohol Spectrum Disorder (FASD), infants may now be given a designation of “At Risk for FASD” if they have known PAE identified through the three sentinel facial features of FASD or reported by a reliable source, in addition to microcephaly at birth [3]. Having this designation available may provide an important opportunity for early detection of infants not receiving a full FAS diagnosis at birth. As the “At Risk for FASD” designation is a new diagnostic tool only added to the Guidelines recently, it will be of interest for future research studies to establish whether it is effective at directing these at-risk infants and their families into supports and early interventions.
Strengths and limitations
This study has several important strengths. This is a recent, population-based study with a large, representative sample size, and is the first study to examine maternal and neonatal outcomes in relation to alcohol use identified as a risk factor among pregnancies in BC. This study has important findings, which must be understood within the context of several existing limitations. First, alcohol use identified as a risk factor during pregnancy was recorded during antenatal visits by the antenatal care provider, and there may be subjectivity in this identification. It may be the case that these data were ascertained in a biased manner on an individual and/or systemic basis. For example, some women who used alcohol during pregnancy may have not been screened, while other women with medical risk factors or in special sub-populations, for example, may have been screened more heavily for alcohol use. Second, due to the relatively small number of women with alcohol use identified as a risk factor during pregnancy, those with both low and high use were placed into a single group for analysis. As a result, possible dose-dependent outcomes could not be examined. As well, outcomes associated with binge drinking, which is known to produce more damaging results [1, 32], were not examined separately due to low numbers reported. The exact sensitivity of alcohol use screening as collected in the BCPDR is unknown, though it is plausible that higher levels of alcohol use following pregnancy recognition may be more likely to be recorded as being a risk. Binge drinking itself, however, was measured among women with alcohol use identified as a risk factor. The validity of the data on maternal alcohol use in the BCPDR is unknown, though it is not routinely used in surveillance, nor is it mandatory to enter into the information system [33]. Based on the sensitive nature, alcohol use identified as a risk factor during pregnancy may be comparable to maternal smoking status, which was found to have 63.9% sensitivity and 98.2% specificity in a validation study of the BCPDR [33]. Also, as noted above, multi-substance use was high and could have influenced outcomes in this study. In many cases, women who used alcohol in pregnancy also used tobacco, cannabis or other substances, making interpretation of the effect of alcohol alone more difficult. As alcohol consumption was self-reported by women, there is a possibility of social desirability bias influencing both reported usage and amounts consumed. Furthermore, the discrepancy between self-reported alcohol use during pregnancy and identification of alcohol use as a risk factor is unknown; however, all alcohol use during pregnancy is a risk factor for adverse neonatal outcomes. Since maternal self-report of alcohol use was solely based on that which occurred after pregnancy recognition, it is possible that PAE went unrecorded in many cases. This study was not able to examine the timing of pregnancy recognition, and therefore, the role of unplanned pregnancies is unknown. Lastly, FAS is rarely diagnosed at birth, therefore, data from birth registries will always underestimate FAS incidence.
Conclusion
Understanding and describing how PAE is related to fetal growth continues to be challenging. Future research in this area may also wish to examine at what point in the pregnancy various types of growth deficits can be detected, levels of exposure necessary to produce specific deficits, and how multi-substance use contributes to this picture.
Birth registries across country should harmonize the definition and collection of alcohol use data and conduct post-discharge follow-up. Obstetricians and gynaecologists, as well as general practitioners and family physicians, are in a unique first point position, as they can screen childbearing age and pregnant women for alcohol use and identify pregnancies at risk for FASD. All prenatal care providers should consistently be trained to screen for alcohol use during pregnancy in accordance with the 2020 Society of Obstetricians and Gynaecologists of Canada (SOGC) guidelines [16]. Pregnant women with identified alcohol use should be provided with brief interventions, specialized treatment, support programs, and community resources [34]. All these strategies can significantly reduce prevalence of alcohol use during pregnancy and FASD.
Availability of data and materials
The data that support the findings of this study are available from Perinatal Services BC, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Perinatal Services BC.
Abbreviations
- aOR:
-
Adjusted odds ratio
- BC:
-
British Columbia
- BCPDR:
-
British Columbia Perinatal Data Registry
- CI:
-
Confidence interval
- FAS:
-
Fetal Alcohol Syndrome
- FASD:
-
Fetal alcohol spectrum disorder
- ICD-10:
-
The International Classification of Diseases, Version 10
- IPPV:
-
Intermittent positive pressure ventilation
- IUGR:
-
Intrauterine growth restriction
- LR:
-
Logistic regression
- NICU:
-
Neonatal intensive care unit
- NOS:
-
Not otherwise specified
- OR:
-
Odds ratio
- PAE:
-
Prenatal alcohol exposure
- PSBC:
-
Perinatal Services BC
- SD:
-
Standard deviation
- SOCG:
-
Society of Obstetricians and Gynaecologists of Canada
References
Alvik A, Torgersen AM, Aalen OO, Lindemann R. Binge alcohol exposure once a week in early pregnancy predicts temperament and sleep problems in the infant. Early Human Dev. 2011;87(12):827–33.
Coles C. Critical periods for prenatal alcohol exposure: evidence from animal and human studies. Alcohol Res Curr Rev. 1994;18(1):22–9.
Cook JL, Green C, Lilley C, Anderson S, Baldwin ME, Chudley AE, et al. Fetal alcohol spectrum disorder: a guideline for diagnosis across the lifespan. Can Med Assoc J. 2016;188(3):191–7.
Sokol RJ. Alcohol and abnormal outcomes of pregnancy. Can Med Assoc J. 1981;125:143–8.
Popova S, Lange S, Probst C, Gmel G, Rehm J. Estimation of national, regional and global prevalence of alcohol use during pregnancy and fetal alcohol syndrome: a systematic review and meta-analysis. Lancet. 2017;5(3):e290–9.
World Health Organization. Global Status Report on Alcohol and Health. Geneva: World Health Organization; 2018. Available from: https://apps.who.int/iris/bitstream/handle/10665/274603/9789241565639-eng.pdf?ua=1
Abel EL. Prenatal effects of alcohol. Drug Alcohol Depend. 1984;14(1):1–10.
Coles CD, Smith I, Fernhoff PM, Falek A. Neonatal neurobehavioral characteristics as correlates of maternal alcohol use during gestation. Alcohol Clin Exp Res. 1985;9(5):454–60.
Popova S, Lange S, Shield K, Mihic A, Chudley A, Mukherjee RAS, Bekmuradov D, Rehm J. Comorbidity of fetal alcohol spectrum disorder: a systematic review and meta-analysis. Lancet. 2016;387(10022):978–87.
Ioffe S, Chernick V. Maternal alcohol ingestion and incidence of respiratory distress syndrome. Am J Obstet Gynecol. 1987;156(5):1231–5.
Vahidnia F, Eskenazi B, Jewell N. Maternal smoking, alcohol drinking and febrile convulsions. Seizure. 2008;17(4):320–6.
Henderson J, Gray R, Brocklehurst P. Systematic review of effects of low-moderate prenatal alcohol exposure on pregnancy outcomes. Brit J Obstet Gynaecol. 2007;114:243–52.
Coyne KL, de Costa CM, Heazlewood RJ, Newman HC. Pregnancy characteristics of women giving birth to children with fetal alcohol syndrome in far North Queensland. Aust NZ J Obstet Gynaecol. 2008;48:240–7.
Guliani H. Mix of maternity care providers in Canada. Healthc Policy. 2015;11(1):46–60.
Hedden L, Munro S, McGrail KM, Law MR, Bourgeault IL, Barer ML. Is attending birth dying out? Trends in obstetric care provision among primary care physicians in British Columbia. Can Fam Physician. 2019;65(12):901–9.
Graves L, Carson G, Poole N, Patel T, Bigalky J, Green C, et al. Guideline no. 405: screening and counselling for alcohol consumption during pregnancy. J Obstet Gynaecol Can. 2020;42(9):1158–73.
Perinatal Services BC. British Columbia Perinatal Data Registry. Years Provided: (2014/15 to 2017/18). Resource Type: Extract data. Data Provided on (March 27, 2020).
Better Outcomes Registry & Network (BORN). Ontario annual report 2012–2013 and 2013–2014. Ottawa; 2015. Available from: https://www.bornontario.ca/en/publications/resources/Documents/121187%2D%2DFInal%2D%2D-english.pdf
Healthy Child Manitoba. Child and Youth Report. Winnipeg: Healthy Child Manitoba; 2017. Available from: https://www.gov.mb.ca/healthychild/publications/hcm_2017report.pdf
Popova S, Lange S, Probst C, Parunashvili N, Rehm J. Prevalence of alcohol consumption during pregnancy and fetal alcohol spectrum disorders among the general and Aboriginal populations in Canada and the United States. Eur J Med Genet. 2017;60:32–48.
Perinatal Services BC. Perinatal Health Report: Deliveries in British Columbia 2016/17. Vancouver; 2018. Available from: http://www.perinatalservicesbc.ca/Documents/About/AnnualReport/PSBCAnnualReport2016_17.pdf
Perinatal Services BC. Perinatal Health report: deliveries in British Columbia 2014/15. Vancouver: Perinatal Services BC; 2016. Available from: http://www.perinatalservicesbc.ca/Documents/Data-Surveillance/Reports/PHR/PHR_BC_2014_15.pdf
BC Perinatal Health Program. Perinatal Health report 2008: British Columbia. Vancouver: Perinatal Services BC; 2010. Available from: http://www.perinatalservicesbc.ca/Documents/Data-Surveillance/Reports/SurveillanceAnnualReport2008.pdf
Perinatal Services BC. Perinatal Health report 2008–09 to 2012–13: British Columbia. Vancouver: Perinatal Services BC; 2014. Available from: http://www.perinatalservicesbc.ca/Documents/Data-Surveillance/Reports/PerinatalHealthReport2014_FraserHealth.pdf
Dell CA, Roberts G. Alcohol use and pregnancy: an important Canadian public Health and social issue. Ottawa: Public Health Agency of Canada; 2005. p. 100. Cat. no.: HP10-5/2006E
Zelner I, Koren G. Alcohol consumption in women. J Pop Ther Clin Pharm. 2013;20(2):e201–6.
Kim HG, Mandell M, Crandall C, Kuskowski MA, Dieperink B, Buchberger RL. Antenatal psychiatric illness and adequacy of prenatal care in an ethnically diverse inner-city obstetric population. Arch Women Health. 2006;9:103–7.
Greenfield SF, Back SE, Lawson K, Brady KT. Substance abuse in women. Psychiatr Clin North Am. 2010;33(2):339–55.
Luke S, Hutcheon J, Kendall T. Cannabis use in pregnancy in British Columbia and selected birth outcomes. J Obstet Gynaecol Can. 2019;41(9):1311–7.
O’Leary CM, Nassar N, Kurinczuk JJ, Bower C. The effect of maternal alcohol consumption on fetal growth and preterm birth. Brit J Obstet Gynaecol. 2009;116:390–400.
Quelhas D, Kompala C, Wittenbrink B, Han Z, Parker M, Shapiro M, et al. The association between active tobacco use during pregnancy and growth outcomes of children under five years of age: a systematic review and meta-analysis. BMC Public Health. 2018;18(1):1372–17.
Carter RC, Jacobson SW, Molteno CD, Jacobson JL. Fetal alcohol exposure, iron-deficiency anemia, and infant growth. Pediatrics. 2007;120:559–67.
Frosst G, Hutcheon J, Joseph KS, Kinniburgh B, Johnson C, Lee L. Validating the British Columbia Perinatal Data Registry: a chart re-abstraction study. BMC Pregnancy Childbirth. 2015;15:123. Published 2015 May 27. https://doi.org/10.1186/s12884-015-0563-7.
World Health Organization. Guidelines for the identification and management of substance use and substance use disorders in pregnancy. Geneva: World Health Organization; 2014. Available from: http://apps.who.int/iris/bitstream/10665/107130/1/9789241548731_eng.pdf?ua=1
Acknowledgements
Authors thank Perinatal Services BC for providing their data.
Funding
This work was undertaken as part of a larger study supported by Public Health Agency of Canada (Grant #: 1718-HQ-000774). This funding body did not have any role in the design of the study, collection, analysis and interpretation of the data, or in writing this manuscript.
Author information
Authors and Affiliations
Contributions
SP obtained the funding to support this data request, led the development of the design and the conception of this study, and assisted in the acquisition of data by coordinating and supervising the data request process from PSBC. SP supervised statistical data analysis and drafted, reviewed and revised the manuscript. DD assisted in the acquisition of data by initializing and coordinating the data request from PSBC. DD contributed to the conception and design of the study and supervised statistical data analysis. DD contributed to the interpretation of the findings and to manuscript revisions, critically reviewing the manuscript for important intellectual content. GO conducted data linkage, data cleaning, statistical analysis, methods description, and critically reviewed the manuscript for important intellectual content. VT contributed to interpretation of the findings and manuscript writing, critically reviewing and revising the manuscript for important intellectual content. JR contributed to interpretations of the findings and critically reviewed the manuscript for important intellectual content. All authors (SP, DD, GO, VT and JR) have read and approved the final manuscript as it has been submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The release of the dataset for this study from Perinatal Services BC was approved through their Research Review Committee on 25 November 2019. All inferences, opinions, and conclusions drawn in this publication are those of the authors, and do not reflect the opinions or policies of Perinatal Services BC.
This work was undertaken as part of a larger study supported by the Public Health Agency of Canada, for which ethics approval was received from the Centre for Addiction and Mental Health REB on 25 October 2017 (REB#: 014/2017).
Consent for publication
Not applicable.
Competing interests
All authors declare that they do not have any financial, personal, political, intellectual or religious competing interests relevant to this article to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Adverse neonatal outcomes identified through literature review on prenatal alcohol and other substance exposed pregnancies
Additional file 2.
Supporting Information for Methodology
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Popova, S., Dozet, D., O’Hanlon, G. et al. Maternal alcohol use, adverse neonatal outcomes and pregnancy complications in British Columbia, Canada: a population-based study. BMC Pregnancy Childbirth 21, 74 (2021). https://doi.org/10.1186/s12884-021-03545-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-021-03545-7