Abstract
Background
Antenatal care (ANC) is one of the core interventions for improving maternal outcomes. The average annual decline of maternal mortality rate from 1990 to 2013 was 5% in Ethiopia. This figure was below the least expected 5.5% to achieve the targeted 75% by 1990–2015. Moreover, completion of the recommended four or more ANC visits was only 32%. This study was aimed to examine individual, household and community level potential determinants of completing the recommended visits in the country.
Methods
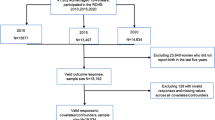
The 2014 Ethiopian Mini Demographic and Health Survey data were used. Among women aged 15–49 years 3694 who had given birth in the 5 years preceding the survey were included in the analysis. The robust standard error method of generalized estimation equations were used for binary outcome variable from the clustered data.
Results
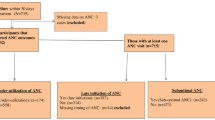
Only 33.0% (95% CI 31. 5% 34.5%) of women completed the recommended visits. Out of the total women, 56.5% had at least one ANC visit. Out of those who had at least one ANC visit, 37.4% visited in their first trimester. Completing the recommended visits was negatively associated with women in the lower educational level, lower economic conditions, higher birth order, and rural residence. But, it was positively associated with the community level high quality ANC services received. Difference in age and region also affected the completion of the recommended visits.
Conclusion
The finding revealed the need for improving the uptake of ANC services, early arrival in the first trimester for services, and motivating mothers that begin ANC to confirm continuity. Strategies to foster completing the recommended visits should focus on upgrading quality of care services at the community level. Women in low economic level, high birth order, rural residence, and low educational status should be given special attention. Early and late age groups should be given special attention regarding the services.
Similar content being viewed by others
Background
Antenatal care (ANC) is one of the core interventions for improving maternal outcomes [1]. ANC services enable early identification of pregnancy related risks and complications; and ensure access of services including health education, vaccines, diagnostic tests and treatments [2]. It also helps to establish good relationship between pregnant women and service providers [3]. Moreover, a pregnant woman visiting health facilities for ANC would get advice and support, and will be more informed about health needs and self-care [4], and consequently leaded to an increased utilization of emergency care services [5, 6].
In Ethiopia the average annual decline of maternal mortality rate was 5% from 1990 to 2013 [7]. This figure was below the least expected 5.5% to achieve the targeted 75% decline between 1990 and 2015 [7]. Out of 289,000 estimated maternal death globally in 2013, 62% were from the Sub-Saharan Africa region alone [7]. In the same 2013 report, Ethiopia was one among ten countries comprising 58% of the global maternal deaths with 420 deaths per 100,000 live births.
According to the WHO report, 83% of pregnant women received ANC at least once in the period 2007–2014 globally. However, in the same report 64% had the recommended four or more ANC visits [8]. In Ethiopia ANC services for women are provided at community health post, health center and hospital. However, in this country, 58% and 32% of the women with live births in the 5 years before the survey had at least one and four or more ANC visits, respectively for services from skilled health personnel [9]. Although the Ethiopian Federal Ministry of Health has been working to improve maternal outcomes, the figures show improving access to and strengthening facility based maternal services is still needed.
Several studies conducted among specific localized areas in Ethiopia examined factors affecting ANC utilization [10,11,12,13], but these were neither representative of the country nor particular about the recommended minimum of four visits. The studies considered only individual and household characteristics associated with the utilization of ANC services. However, literatures suggested that context can influence individual health outcomes [14, 15]. Communities are local contexts and specific localities where individuals reside, share physical and socioeconomic characteristics, and establish social networks that potentially affect individual health and explain the impact of social inequalities in accessing health services [14].
This paper attempted to assess individual, household and community related determinants of completing four or more ANC visits among women of reproductive age in Ethiopia by considering the clustered nature of the data. In order to address this objective, recent data from a large-scale household survey conducted in 2014 provided a valuable opportunity. The analysis of determinants allowed a better identification of women who didn’t utilize ANC services four or more times with a high probability; as a result a more effective and efficient application of interventions was secured.
Methods
Data and variables
The 2014 Ethiopian Mini Demographic and Health Survey (EMDHS) data set was used for this analysis. The survey designed to obtain and provide information on basic indicators, including ANC visits, utilized multi stage sampling technique. The study population comprised of women in Ethiopia aged 15 to 49 years and gave birth at least once in the last 5 years preceding the survey. Out of 8070 individual women surveyed, data on the last live birth for 3694 women with complete information on variables considered under the study were used. The binary response variable considered in this study indicated whether women completed four or more ANC visits or not from skilled health personnel including Doctors, Nurses, Mid-wives and/or Health officer. Selection of several potential factors associated with completing four or more ANC visits was based on related studies conducted on the factors influencing ANC utilization [16,17,18,19,20,21]. Explanatory variables like current age, educational status, residence, region, marital status, sex of household head, birth order, and wealth index were used at individual and household levels. The wealth index variable in the EMDHS included was obtained by using principal component analysis with five quintiles. However, the two low (lowest and lower taken as low) and the upper most two (highest and higher taken as high) categories were merged for the purpose of this analysis. Two categorical variables derived from a self-exclusive proportion were considered, of which the first was a self-exclusive proportion of educated women, showing the community level literacy of women. The second was a self-exclusive proportion of women who took five components of ANC services, showing community related quality of ANC services received [20, 21]. A binary indicator for quality of care was created, distinguishing between proportions less or equal to 5% (low) and proportions more than 5% (high). The five components considered were all of the six components of ANC which the WHO has determined essential for every pregnant woman except weight measurement. Accordingly, the five components considered were measuring blood pressure, taking sample of blood, taking sample of urine, giving iron tablets/syrup, and informing about pregnancy complications. For both the community related variables cut-off points were chosen based on the distribution of cases. Cut-off points were specifically chosen on the basis that could not violate assumptions of the model (cell counts in the covariate pattern used directly for measuring goodness of fit), could enable us to get not small number of categories (important properties for different proportions), and cut-off points were tried to be better practical values (like products of 5, 10, 25, and/or 100).
Statistical analysis
The Statistical software Stata version 11 was used for the whole analysis. Due to the similarity of health facility centers, training, and the similar life style conditions, it was expected that responses from the same enumeration area would behave more alike than those of different enumeration areas. As a result, respondent women were clustered within an enumeration area. Thus, the standard error estimates using independent observations was no longer proper for data sets with cluster structures. This analysis considered the intra-cluster correlation and used the Huber method of robust standard error estimates among the family of generalized estimation equations for clustered data in the binary logistic regression modeling [22, 23].
Results
Characteristics of the sample
Among the 3694 sampled women, only 33.0% (95% CI 31. 5% 34.5%) completed four or more ANC visits (Table 1). Out of the total women considered for this study 56.5% (95% CI 54.8% 58.1%) had at least one ANC visit. Besides, out of those who had at least one ANC, 37.4% (95% CI 35.3% 39.5%) visited in their first trimester.
The result also showed that out of samples taken more than three fourths (80.0%) were rural residents. Only 23.3% of the rural residents completed four or more ANC visits, while 71.6% of the urban residents completed the recommended four or more ANC visits.
Based on the community level quality of received ANC, 54.3% women lived in a community with a low level quality of received ANC, while 45.7% lived in a community with high community level quality of received ANC. Besides, 45.9% of women living in a community with high quality of received ANC completed four or more ANC visits, whereas only 25.6% of those in a community with low quality of received ANC completed the four or more ANC visits. With respect to community level literacy, 24.7% of women lived in a community with low community level literacy of women. This figure was 52.3% and 23.0% for women in the community with medium and high community level literacy of women, respectively. Moreover, 60.9% of the women in the community which had a high level literacy of women completed four or more ANC visits, while the figures were 29.4% and 14.8% for women in low and medium community level literacy of women, respectively.
When considered from the point of view of wealth index, almost half (49.6%) of the women who took part in the study were from poor households, While 15.5% and 34.9% were from medium and rich ones, respectively. Among women who were from poor, medium and rich households, 16.7%, 32.0% and 56.6% completed four or more ANC visits, respectively. At individual levels, 18.7% of the women with their last delivery were first birth order pregnancies. This figure was 29.9%, 25.0%, and 26.4% for 2nd or 3rd, 4th or 5th and above 6th birth orders, respectively. The proportion of those who completed four or more ANC visits decreased as the birth order increased. For instance, 48.2% completed four or more ANC visits among first birth order pregnancies of their last delivery.
Determinants of completing the four or more ANC visits
The result of the bi-variable analysis showed that all explanatory variables were associated with completing four or more ANC visits at 25% level of significance. The final adjusted model, including all considered factors fits the data well (Goodness of fit test p-value = 0.3516). This could also be supported by area under Receiver Operating Curve (ROC) with a value of 0.8044.
The result showed that variables such as age and highest level of education of women, region, residence, and wealth index of the household; birth order of the child and community level quality of received ANC services were significant determinants of completing four or more ANC visits at 5% level of significance (Table 2).
The odds of completing four or more ANC visits for women aged 20–24, 25–30, 30–34, and 35–39 years were 1.71 [OR 1.71, (95% CI 1.12, 2.62)], 2.20 [OR 2.20, (95% CI 1.36, 3.56)], 2.67 [OR 2.67, (95% CI 1.63, 4.40)], and 2.35 [OR 2.35, (95% CI 1.35, 4.07)], times that for women aged 15–19 years, respectively.
Women with primary, and secondary/higher educational levels were 1.86 [OR 1.86, (95% CI 1.56, 2.21)], and 3.67 [OR 3.67, (95% CI: 2.53, 5.31)] times likely to complete four or more ANC visits as compared to un-educated women, respectively.
The result revealed that rural dweller women were 65% [OR 0.35, (95% CI 0.22, 0.53)] less likely to complete four or more ANC visits as compared to urban ones. On the basis of economic status, women in the medium, and rich households were 78% [OR 1.78, (95% CI 1.41, 2.25)], and 84% [OR 1.84, (95% CI 1.41, 2.40)] more likely to complete four or more ANC visits, respectively as compared to their counter parts.
Fourth/fifth, and sixth/above birth order pregnant women were 38% [OR 0.62, (95% CI 0.44, 0.88)], and 36% [OR 0.64, (95% CI 0.42, 0.96)] less likely to complete four or more ANC visits, respectively as compared to 1st birth order pregnant women.
Women in communities with high quality of received ANC were 42% [OR 1.42, (95% CI 1.03, 1.96)] more likely to complete four or more ANC visits as compared to women in communities with low quality of received ANC.
Women in Somali, Afar, and Amhara Regional States were respectively 85% [OR 0.15, (95% CI 0.07, 0.32)], 67% [OR 0.33, (95% CI 0.19, 0.58)] and 44% [OR 0.56, (95% CI 0.34, 0.94)] less likely, while those in Addis Ababa City Administration were 2.56 [OR 2.56, (95% CI 1.32, 4.93)] times likely to complete four or more ANC visits as compared to women in Tigray Regional State.
Discussion
In this study, individual, household, and community level factors were considered as determinants of completing four or more ANC visits in Ethiopia. This study differed from others carried out in Ethiopia [10,11,12,13] to date in that it considered community related variables and used binary logistic regression model with robust standard error estimates. This analysis was helpful to quantify the association of community related variables with completion of four or more ANC visits so as to design more effective policies, define appropriate intervention and reduce community based inequalities in accessing ANC services.
Candidate predictors of the multivariable binary logistic regression model were those significantly associated with completing four or more ANC visits from the bi-variable analysis at 25% level of significance. From the final multivariable model, the variables age and highest level of education of the woman, region, residence and wealth index of the household; birth order of the child and community level quality of received ANC were related with completing the four or more ANC visits in Ethiopia.
The result showed that as women’s educational level increases the likelihood of completing the four or more ANC visits also increases. This result agreed with those of studies conducted abroad, in Vietnam [16], Colombia [19], and Brussels Metropolitan region [18]. This result could be due to the fact that education is an indicator of various other factors associated with health seeking behavior. It could be reasonable to say that educated women as compared to uneducated, have better access to information, possess a level of health literacy that could empower them to exercise their choice, and able to overcome cultural barriers of ANC service utilization [24, 25]. Furthermore, education changes attitude and expectation of a woman and her significant others towards traditional gender norms and roles [26]. Lack of education leads to poor quality interactions between a pregnant and service providers consequently discouraging utilization of ANC services [27]. The study suggested that mothers in Ethiopia should be educated about ANC utilization to raise uptake of services at health facilities [28]. The study also showed the need of strengthening interventions mitigating early drop out of girls from school.
The result also indicated that the likelihood of completing four or more ANC visits decreased as birth order increased as reported consistently by studies in Haiti [20], Nigeria [29], and Brussels Metropolitan region [18]. This result implies that high parity women have less desire to use recommended ANC visits. This could be due to the belief that they do not need services as they have experience with pregnancy and childbirth. Besides, structural barriers related to cost and time raised from higher child dependency ratio prevents seeking ANC services for higher parity women.
Moreover, at individual levels, women aged 20–39 years were more likely to complete the four or more ANC visits as compared to those aged 15–19 years. This finding was consistent with the study conducted in Colombia [19].
Women from Somali, Afar and Amhara Regional States had less chance from severe to slight, respectively to complete the four or more ANC visits. This could be due to the fact that in availability of access to health services, lower economic status, lack of political commitment, hostile and isolated environments, and large number of ethnic minorities in majority of areas of these regions [30, 31].
Rural resident women were less likely to complete the four or more ANC visits as compared to urban dwellers in Ethiopia. Other studies in Nepal [32] and Vietnam [33] found out results consistent with ours.
The likelihood of completing four or more ANC visits increased as household economic status rose. This result was consistent with those of studies in Vietnam [16], Haiti [34], Nigeria [24], and Kenya [35]. Poverty is a structural factor that could affect a woman’s ability to seek ANC through multiple mechanisms, including ability to identify and locate the availability of services, overcoming financial challenges, with standing geographic inaccessibility, possessing knowledge about services, improving attitudes towards services, and improving provider attitudes [36].
Women in the community that received high quality of ANC were more likely to complete four or more ANC visits. This result was consistent with that of a study in Zambia [21] that showed the odds of having three or fewer ANC visits were higher if the quality of ANC received was lower. A related study in Haiti [20] showed that high-quality ANC was associated with increased odds of using skilled birth attendance even after controlling for the number of ANC visits. The number of essential components of care received would show the quality of ANC. In our study these included whether a woman took iron tablets, was informed about the signs of pregnancy complications, and received screening tests like blood pressure measurement, urine sample and blood sample taking during ANC visits.
Limitations
Some social and community level variables, including neighborhood security/safety, dominant ethnic group and religion were not included as they were not captured in the secondary data used for this study. Besides, causality could not be established as the study was derived from cross sectional survey.
Conclusion
The finding highlighted the need to improve the uptake of ANC services, early arrival in the first trimester for ANC services, and motivating mothers that begin ANC to confirm continuity.
Strategies to foster completing four or more ANC visits should focus on upgrading quality of care services at community level. Moreover, women in low economic status, high birth order, rural residence, and low educational level should be given special attention. Early age group and late age group among fertile age group women should be given special attention for the services. Women from Somali, Afar, and Amhara Regions should be given special emphasis.
Abbreviations
- ANC:
-
Antenatal care
- AOR:
-
Adjusted Odds Ratio
- CI:
-
Confidence Interval
- COR:
-
Crude Odds Ratio
- EMDHS:
-
Ethiopian Mini Demographic and Health Survey
- OR:
-
Odds Ratio
- ROC:
-
Receiver Operating Curve
- WHO:
-
world health organization
References
World Health Organization. Maternal mortality. Genava: World Health Organization; 2014.
Gross K, Schellenberg JA, Kessy F, Pfeiffer C, Obrist B. Antenatal care in practice: an exploratory study in antenatal care clinics in the Kilombero Valley, south-eastern Tanzania. BMC Pregnancy Childbirth. 2011;11:36.
Magadi MA, Madise NJ, Rodrigues RN. Frequency and timing of antenatal care in Kenya: explaining the variations between women of different communities. Soc Sci Med. 2000;51:551–61.
World Health Organization. The Partnership for Maternal, Newborn and Child Health. Opportunities for Africa’s newborns: practical data, policy and programmatic support for newborn care in Africa. Geneva: World Health Organization; 2006.
Morse ML, Fonseca SC, Gottgtroy CL, Waldmann CS, Gueller E. Severe maternal morbidity and near misses in a regional reference hospital. Rev Bras Epidemiol. 2011;14:310–22.
Roost M, Altamirano VC, Liljestrand J, Essen B. Does antenatal care facilitate utilization of emergency obstetric care? A case-referent study of near-miss morbidity in Bolivia. Acta Obstetric Gynecol Scand. 2010;89:335–42.
WHO, UNICEF, UNFPA, World Bank, United Nations Population Division. Trends in maternal mortality in 1990 to 2013: estimates by WHO, UNICEF, UNFPA, World Bank and United Nations population division. Geneva: World Health Organization; 2014.
World Health Organization. World Health Statistics 2015. Geneva: WHO; 2015.
Central Statistical Agency[Ethiopia]. Ethiopia Mini Demographic and Health survey 2014. Addis Ababa, Ethiopia: Central Statistics Agency; 2014.
Birmeta K, Dibaba Y, Woldeyohannes D. Determinants of maternal health care utilization in Holeta town, central Ethiopia. BMC Health Serv Res. 2013;13:256.
Tewodros B, G/Mariam A, Dibaba Y. Factors affecting antenatal care utilization in Yem Special Woreda, South Western Ethiopia. Ethiop J Health Sci. 2009;19:1.
Aliy J, Mariam DH. Determinants of equity in utilization of maternal health services in Butajira, Southern Ethiopia. Ethiop J Health Dev. 2012;26(1 special issue): 265-270.
Gedefaw M, Muche B, Aychiluhem M. Current status of antenatal care utilization in the context of data conflict: the case Dembecha District, north West Ethiopia. Open J Epidemiol. 2014;4:208–16.
Kawachi I, Berkman LF. Neighborhoods and health. Oxford: Oxford University Press; 2003.
Shankardass K, Dunn JR. How goes the neighborhood? Rethinking neighborhoods and health research in social epidemiology. In: O’Campo P, Dunn JR, editors. Rethinking social epidemiology: towards a science of change. Dordrecht: Springer; 2012.
Ha BTT, Tac PV, Duc DM, Duong DTT, Thi LM. Factors associated with four or more antenatal care services among pregnant women: a cross-sectional survey in eight south central coast provinces of Vietnam. Int J Women’s Health. 2015;7:699–706.
Barasa SK, Wanjoya KA, Waititu GA. Analysis of determinants of antenatal care services utilization in Nairobi County using logistic regression model. Am J Theor Appl Stat. 2015;4(5):322–8.
Beeckman K, Louckx F, Putman K. Determinants of the number of antenatal visits in a metropolitan region. BMC Public Health. 2010;10:527.
Osorio AM, Tovar LM, Rathmann K. Individual and local level factors and antenatal care use in Colombia: a multilevel analysis. Cad Saúde Pública, Rio de Janeiro. 2014;30(5):1079–92.
Babalola SO. Factors associated with use of maternal health services in Haiti: a multilevel analysis. Rev Panam Salud Publica. 2014;36(1):1–9.
Chama-Chiliba CM, Koch SF. Utilization of focused antenatal care in Zambia: examining individual- and community-level factors using a multilevel analysis. Health Policy Plann. 2015;30:78–87.
Huber PJ, editor The behavior of maximum likelihood estimates under non-standard conditions. The fifth Berkeley symposium on mathematical statistics and probability; 1967.
Fuller WA, Kennedy W, Schnell D, Sullivan G, Park HJ. Carp PC. Ames, IA: Statistical Laboratory, Iowa State University. Ames: Iowa State University; 1986.
Babalola S, Fatusi A. Determinants of use of maternal health services in Nigeria-looking beyond individual and household factors. BMC Pregnancy Childbirth. 2009;9:43.
Greenaway ES, Leon J, Baker DP. Under -standing the association between maternal education and use of health services in Ghana: exploring the role of health knowledge. J Biosoc Sci. 2012;44(6):733–47.
Jejeebhoy SJ. Women’s Education, autonomy, and reproductive behavior: experience from developing countries. Oxford, United Kingdom: Clarendon Press; 1995.
Adamson PC, Krupp K, Niranjankumar B, Freeman AH, Khan M, Madhivanan P. Are marginalized women being left behind? A population-based study of institutional deliveries in Karnataka, India. BMC Public Health. 2012;12:30.
Barasa KS, Wanjoya AK, Waititu AG. Analysis of determinants of antenatal care services utilization in Nairobi County using logistic regression model. Am J Theor Appl Stat. 2015;4(5):322–8.
Aremu O, Lawoko S, Dalal K. Neighbor -hood socioeconomic disadvantage, individual wealth status and patterns of delivery care utilization in Nigeria: a multilevel discrete choice analysis. Int J Women’s Health. 2011;3:167–74.
Galvis LA, Meisel A. Persistencia de las desigualda-des regionales en Colombia: un análisis espacial. Bogotá: Banco de la República; 2010.
Chávez-Martínez DA. Agenda Pacífico XXI: otraoportunidad para el Pacífico colombiano desapro-vechada. Econ Colomb. 2005;311:90–9.
Neupane S, Doku DT. Determinants of time of start of prenatal care and number of prenatal care visits during pregnancy among Nepalese women. J Community Health. 2012;37:865–73.
Tran TK, CTK N, Nguyen HD, Eriksson B, Bondjers G, Gottvall K, et al. Urban-rural disparities in ANC utilization: a study of two cohorts of pregnant women in Vietnam. BMC Health Serv Res. 2011;11:120.
AJ G. Barriers to the utilization of maternal health care in rural Mali. Soc Sci Med 2007;65:1666-1682.
Harun K, Shelmith M, Muia D. Persistent utilization of unskilled birth attendants’ services among Maasai women in Kajiado County, Kenya. Public Health Res. 2012;2(6):213–20.
Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, Rahman MH. Poverty and access to health care in developing countries. Ann N Y Acad Sci. 2008;1136(1):161–71.
Acknowledgements
The author would like to express gratitude to the Central Statistical Agency of Ethiopia for giving the data. I would also like to extend my gratitude to my wife Betelhem Tigabu for her continued support and initiation. Finally, I would like to thank all who directly or indirectly supported me.
Funding
No external fund was received.
Availability of data and materials
Simplified data would be shared upon request.
Author’s contributions
The author contributed to designing of the study, performed the statistical analysis and interpreted the results and prepared the manuscript. The author read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethics committee of the Ministry of Health, Government of Ethiopia, reviewed and approved the survey. All respondents to the survey provided verbal informed consent. The 2014 EMDHS dataset is not available as a public domain. The author requested the Director of Central Statistics Agency of Ethiopia and access was granted to use the data.
Consent for publication
The manuscript does not contain any individual person’s data.
Competing interests
The author declares that he/she has no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Muchie, K.F. Quality of antenatal care services and completion of four or more antenatal care visits in Ethiopia: a finding based on a demographic and health survey. BMC Pregnancy Childbirth 17, 300 (2017). https://doi.org/10.1186/s12884-017-1488-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-017-1488-0