Abstract
Background
Correct measurement and continuous monitoring of exclusive breastfeeding are essential to promote exclusive breastfeeding. Measuring exclusive breastfeeding is a complex issue as rates can vary according to the definition, measurement period, questions asked, and infant’s age. This article reviewed the methodology of reporting exclusive breastfeeding in Nepal, and compared exclusive breastfeeding rates using data from a cohort study undertaken in western Nepal.
Methods
A literature review was first conducted on studies published during 2000–2014. In our cohort study, 735 mother-infant pairs were recruited within the first month postpartum and followed up during the fourth and sixth months.
Results
The majority of studies in Nepal, including national surveys, used the World Health Organization (WHO) recommended definition (only breastmilk with the exception of medicine and vitamin syrup), and the most common measurement period was a 24-h recall. Our data demonstrated that the exclusive breastfeeding rate during the sixth month was 8.9% using the recall-since-birth method but was 18.7% using the 24-h recall method. Substantial differences in rates were also found during the first (66.3% vs 83.9%) and fourth months (39.2% vs 61.1%).
Conclusion
We found that recent studies reporting exclusive breastfeeding in Nepal varied considerably in methodology. The most commonly used measurement, the 24-h recall, leads to over-estimation of the prevalence of exclusive breastfeeding when compared to the recall-since-birth method. A common standard of reporting exclusive breastfeeding is clearly needed for evidence-based decision making.
Similar content being viewed by others
Background
Exclusive breastfeeding offers many short and long-term health and nutrition benefits. In the short term, it is the best source of nutrition, and supports optimum growth and development of the infant [1]. In the long term, exclusive breastfeeding is likely to protect from obesity, type-2 diabetes, and is associated with increased intelligence quotient scores [2, 3]. Exclusive breastfeeding impacts on the infant gut microbiome which in turn may contribute to the programming of infant metabolism and immune function [4]. In low and middle income countries where supply of clean water is limited and hygiene of the mother and child is poor, substituting breastmilk with other fluids or food is likely to introduce pathogens resulting in infection-related infant mortality and morbidity [5]. Furthermore, the introduction of other fluids and foods reduces the frequency of breastfeeding and contributes to reduced milk production, ultimately affecting milk supply [6]. A recent systematic review showed that there were higher rates of infant deaths among 0-5 months infants who were not breastfed, partially breastfed or predominantly breastfed compared to those who were exclusively breastfed [7]. Similarly, Victora et al.[8] projected that the scaling up of optimal breastfeeding practices could save 823000 deaths annually among children under five years of age.
The World Health Organization's (WHO) Comprehensive implementation plan on maternal, infant and young child nutrition was endorsed in 2012 and identified six targets to reduce nutrition-related mortality and mortality [9]. Of these, target 5 was by 2025, to increase the rate of exclusive breastfeeding to 50% in the first six months from 37% for the period 2006–2010 [9]. ‘This would involve a 2.3% relative increase per year and would lead to approximately 10 million more children being exclusively breastfed until six months of age’ ([9], p. 9). To measure the progress of member states in achieving this target it is essential to monitor the practice of exclusive breastfeeding regularly and consistently.
Measuring exclusive breastfeeding however, is a complex issue because the rate can vary with respect to the recall duration, questions asked, age of infant and definition adopted [10–12]. WHO originally defined exclusive breastfeeding as ‘infant has received only breastmilk from his/her mother or wet nurse, or expressed breastmilk, and no other liquids or solids with the exception of drops or syrups consisting of vitamins, mineral supplements or medicine’ [13]. In 2007, this definition was modified to allow a child to receive oral rehydration salts [14]. However, this strict definition of exclusive breastfeeding often is not applied in studies which purport to report levels of exclusive breastfeeding [10, 12, 15], making it difficult to compare the findings of studies both within and between countries.
One of the major issues with measuring exclusive breastfeeding is accounting for prelacteal feeding, which is common practice in countries in South Asia, [16, 17] where babies may receive prelacteal feeds for the first few days of life but after which mothers typically revert to exclusive breastfeeding for several months at least. However, accounting for prelacteal feeding is essential for some purposes due to possible infections in early infancy and the loss of the gut priming effect of colostrum as the first feed [4]. Nevertheless, including prelacteal feeding would dramatically reduce the exclusive breastfeeding rate since birth and suggest that a large proportion of infants had never been exclusively breastfed [12].
The prevalence of exclusive breastfeeding also can vary widely depending on the indicator measure used. The indicator favoured by the WHO employs the 24-h recall methodology to determine the proportion of infants 0–5 months of age who received only breastmilk during the previous day [14]. This method has been adopted in countries where capacity and resources are limited and used in household surveys such as the Demographic and Health Surveys [18]. The 24-h recall method can lead to over-estimation due to its inability to capture prelacteal feeding and intermittent use of complementary feeds. That is, infants who only received breastmilk the previous day may have received other foods before that time [19]. On the other hand, measurements based on recall-since-birth can be affected by recall error. For instance, while maternal recall of initiation and duration of breastfeeding is generally valid and reliable over a short period (≤3 years), recall of the age of introduction of other foods and fluids is less reliable [20]. Therefore, duration of exclusive breastfeeding is best measured prospectively using cohort methodology with short recall intervals [21, 22]. Binns et al. [22] reported wide discrepancies in the rates of exclusive breastfeeding in China and Japan when the results of national and regional cross-sectional surveys which predominantly used the 24-h recall method were compared with data prospectively collected in separate studies using the recall-since-birth method. However, comparison of exclusive breastfeeding rates between the two methods using the same data source is rarely made. Significant differences between the two methods of more than 40 percentage points at two and four months of age were first observed in a study conducted in Sweden [19]. To our knowledge however, there has only been one report of a comparison study from a South Asian country reported in 2009 [23].
One of the strategies to reduce under nutrition in Nepal is promotion of exclusive breastfeeding for the first 6 months [24]. Monitoring of the success of this strategy requires surveillance data on exclusive breastfeeding ‘for six months’. However, the current knowledge of exclusive breastfeeding in Nepal is based almost entirely on cross-sectional studies [25–27] which likely overestimate the true rate of exclusive breastfeeding. The only study that has reported exclusive breastfeeding using prospectively collected data were from the Kaski district of Nepal [28]. To date, there has been no study that specifically addressed issues such as definition of exclusivity, duration of measurement, and age composition of infants, all of which can contribute to the reported rate variations in Nepal and the South Asian region. Further research to critically analyse the existing breastfeeding studies is deemed necessary for accurate monitoring and appropriate reporting of such data in the future. Such critical appraisal would also inform future breastfeeding research in Nepal and other countries in South Asia. The objectives of this study are: (1) to review the definitions and methods of reporting exclusive breastfeeding in Nepal used during the period 2000–2014; and (2) assess the magnitude of differences in exclusive breastfeeding rates between the 24-h recall and recall-since-birth methods using a single data set from a prospective cohort study undertaken recently in western Nepal.
Methods
Our paper presents findings from two different methods; a literature review and a large community-based prospective cohort study. Firstly, we conducted a literature review using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Guidelines [29]. A comprehensive literature search was conducted in PubMed, the Cumulative Index to Nursing and Allied Health Literature, and Web of Science databases, with key words ‘breastfeeding’, ‘breast-feeding’ or ‘breast feeding’ or ‘infant feeding’, and ‘Nepal’. Inclusion criteria were: (1) articles published during 2000–2014; (2) reporting exclusive breastfeeding; (3) study conducted in Nepal; and (4) published in the English language. We excluded those articles reporting qualitative findings, but included data sources which are the major policy informing tools in Nepal, namely: (1) Nepal Demographic and Health Surveys (NDHS 2001, 2006, and 2011); and (2) Multiple Indicator Cluster Survey (MICS) [30]. In addition, we performed a manual reference search of identified articles. Figure 1 describes the process of selecting the articles for the review. Two terms that explain the literature review summary are ‘indicator measure’ and ‘age of the infant’. We defined indicator measure as the methods which were used to measure exclusive breastfeeding such as 24-h recall and recall-since-birth. Age of the infant refers to the infant’s age at which data were collected. This was important as younger infants (e.g. < 3 months) are more likely to be exclusively breastfed than their older counterparts. Such variation in infant’s age affects the reported breastfeeding rates.
Secondly, we used data from a prospective cohort study of infant feeding practices conducted during January-October 2014 in the Rupandehi district of western Nepal. This district is located in the south-western plain areas (Terai) of Nepal bordering India in the south. The methodology of this study has been described previously [31, 32] but briefly 735 mother-infant pairs (rural 378, urban 357) were randomly recruited from 15 rural and 12 urban locations. Mothers were recruited from their communities within 30 days of giving birth and followed up during the fourth (90–120 days) and sixth months (150–180 days) (Fig. 2). The main outcome, exclusive breastfeeding, allowed breastmilk, vitamin or mineral syrups, medicine and oral rehydration salt, but no other liquid or solid/semi-solid food, in accordance with the current WHO definition [14]. We used two methods (24-h recall and recall-since-birth) to estimate the rate of exclusive breastfeeding during the first, fourth, and six months after delivery. For the recall-since-birth method, information was obtained based on recall-since-birth at the first interview, and recall-since-the last interview during the fourth month and sixth month interviews. Information was collected through a questionnaire adapted from the NDHS [25] and an earlier cohort study [28] which were in accordance with the WHO’s Indicators for assessing infant and young child feeding practices part 2: measurement [33]. Pre-testing was done and only a few minor changes were needed to make our questionnaire understandable in our study setting. A list of common food items was read to mothers to help them remember their infant feeding practices. The questionnaire to collect this information is provided as a web appendix (Additional file 1). Data were collected by female enumerators who had vocational training in health science after high school level of education. These enumerators received a one-day orientation on data collection including a data collection exercise in the community and the researcher provided feedback after the pretesting. The enumerators were regularly monitored by the first author to ensure the quality of data. During the follow-up interviews, enumerators again received a brief orientation as most of the questions on infant feeding were repeated. The interviews were conducted in the Nepali language.
We defined exclusive breastfeeding within the last 24-h as: mother did not introduce any food item besides her breastmilk or other women’s milk [33].
A mother was classified as exclusive breastfeeding during the first month using recall-since-birth if (1) she did not introduce any prelacteal feeds (2) responded that she had been feeding only breastmilk since birth and (3) was exclusively breastfeeding based on 24-h recall. A mothers was classified as exclusively breastfeeding during the fourth month using recall-since-birth if (1) she had exclusively breastfed during the first month, (2) did not introduce any complementary food since the last interview (confirmed reading list) and (3) did not introduce any complementary food in the last 24-h (confirmed reading list). Similarly, a mothers would be classified as exclusive breastfeeding during the sixth month based on recall-since-birth if (1) she had been exclusively breastfeeding during the fourth month, (2) did not introduce any complementary food since last interview (confirmed reading list) and (3) did not introduce any complementary food in the last 24-h (confirmed reading list). Any mother who was not breastfeeding at the time of interview was classified as not exclusively breastfeeding.
Ethics approval was obtained from the Human Research Ethics Committee of Curtin University (HR 184/2013) and the Nepal Health Research Council. Mothers provided written consent for themselves and their infants, and personal identifiers were removed before analysis. When mother could not read and write, enumerators read the consent form to them. Mothers provided a thumb print as their initials if they agreed to participate. This method was approved by both ethics committees.
Results
Selection of studies in the review
Our literature review found only 9 articles which reported exclusive breastfeeding in Nepal. In addition, three NDHS, and one MICS were subsequently included. On reviewing the articles in full, it was found that two studies [34, 35] had analysed the same dataset and used the same methods (e.g. indicator measure and definitions) as in the NDHS 2006 [27] therefore, these papers were removed from the review leaving 11 studies (Fig. 1). Of these 11 studies, 10 used unique datasets and one used the NDHS 2006 and 2011 but analysed the data differently from the original NDHS 2006 report using the WHO 2007 definition of exclusive breastfeeding. Only one of them was a cohort study [28] and the rest were cross-sectional studies.
Definitions used in measuring exclusive breastfeeding
Four national surveys (NDHS and MICS) [25–27, 30], one secondary analysis of NDHS 2006 and 2011 [36], and two other studies [37, 38] followed the WHO definition of exclusive breastfeeding of the time. It should be noted that the 2001 and 2011 NDHS defined exclusivity as “only breastmilk”. The 2006 NDHS did not provide the actual definition in the report, but advice from researchers involved confirmed that they followed the WHO 1991 definition [13] (personal communication, Mr. Sujan Karki, March, 2015). Two studies [28, 39] used a slight variant of the WHO definition and described exclusive breastfeeding as ‘nothing else (except medicines) but breast milk’ and ‘given breastmilk only without any other feeds (aside from medications) since birth’, respectively. Two cross-sectional studies [40, 41] did not give any definition.
Indicator measure
There were variations in the indicator measure or methods of reporting exclusive breastfeeding used to estimate prevalence of exclusive breastfeeding. Six studies used the 24-h recall measure [25–27, 30, 36, 41]. One study used recall-since-birth using repeated measures in a prospective cohort study up to 6 months [28], and one used recall-since-birth at two months [39]. Two studies used retrospective recall of mothers of infants aged 6 to 23 months [37] and 9 months postpartum [38], and asked mothers how long they had breastfed exclusively.
Age of infant
Age of infant is another important aspect as younger infants are more likely to be breastfed exclusively than their older counterparts. Whilst most studies reported on infants aged 0–5 months [25–27, 30, 36, 41], one study [40] estimated exclusive breastfeeding rate at the 5th month. On the other hand, the study conducted by Subedi et al. [37] reported on the prevalence of breastfeeding up to six months among infants aged 6 to 23 month, while Chandrashekar et al. [39] considered young infants less than 2 months, and Karkee et al. [28] reported exclusive breastfeeding rates at 1, 4, and 6 months.
Reported exclusive breastfeeding rates in Nepal
In view of the above methodological discrepancies, we found large variations in the rates of exclusive breastfeeding between studies. With the exception of one prospective cohort study which observed a low rate (29.7%) of exclusive breastfeeding at 6 months (22 weeks) using recall-since-birth [28], other studies reported a higher prevalence of greater than 50% amongst infants less than 6 months [37, 39, 40]. Ullak et al. [38] reported 9% exclusive breastfeeding prevalence at 6 months.
Comparison of exclusive breastfeeding rates in a cohort study using 24-h recall and recall-since-birth methods
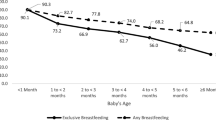
We used data from our cohort study to compare exclusive breastfeeding rates during the first, fourth, and sixth months (Fig. 2); results are presented in Table 1. All infants were breastfed at the time of recruitment. Almost one-third of infants were provided with prelacteal feeds, leaving only 69.4% of them being exclusively breastfed at their first feed. The rates of exclusive breastfeeding are substantially different between the 24-h recall and the recall-since-birth methods at all three time points. During the first month, the prevalence of exclusive breastfeeding based on the 24-h recall method was 83.9% but was 66.3% using recall-since-birth, which accounted for prelacteal feeds. Similarly, the exclusive breastfeeding rate during the sixth month was 18.7% from the 24-h recall method and was half of that (8.9%) using recall-since-birth.
Discussion
This study reviewed and compared the definition and methods of reporting exclusive breastfeeding in Nepal. We found three main issues related to the measurement and reporting of exclusive breastfeeding namely, inconsistent definition of exclusive breastfeeding, indicator measurement and interpretation of the WHO indicator based on 24-h recall.
Data collected from the same participants in our cohort study were used to demonstrate the differences in exclusive breastfeeding rates between methods. Our findings suggest that the extensive use of NDHS data based on 24-h recall would inevitably over-estimate the prevalence of lifelong exclusive breastfeeding. In other words, estimates of exclusive breastfeeding rates in Nepal are probably much lower than those previously reported. Such differences in rates between recall-since-birth and 24-h recall have also been demonstrated by others [19, 22, 23]. As in any observational study which relies on self-reported data there is a potential in our study for recall bias and hence the actual duration of exclusive breastfeeding may differ from that reported. However, our data were collected prospectively with relatively short recall intervals, thereby reducing the likelihood of recall bias.
In surveys such as NDHS and MICS, age group of infants is another concern when 0–5 month old infants are aggregated to be the denominator for the 24-h recall prevalence. In our cohort study, exclusive breastfeeding during the sixth month was 18.7% by 24-h recall. For illustration purposes, let us regard the study as a cross-sectional survey that had similar number of infants in three age groups: (1 (n = 735), 4 (n = 715), and 6 (n = 711) months), i.e. 2,161 infants in total available for interview from Table 1. The number of infants being exclusively breastfed based on 24-h recall in each age group would be 617 + 437 + 133 = 1,187, giving a prevalence of 54.9% which is comparable to those of previous studies in Table 2. This is not however the proportion of infants exclusively breastfed for the entire six month period, which is how cross-sectional data derived by this method often are misinterpreted [11, 12, 23]. This difference has been demonstrated also in two other cross-sectional studies conducted in Nepal and East-Timor [36, 42] where the actual 24-h prevalences of exclusive breastfeeding at the sixth month (33.1% and 24.9%, respectively) was lower than the commonly reported 0–5 month exclusive breastfeeding prevalence of 66.3% and 49%, respectively. If infants should be breastfed for six months according to the WHO recommendation, then the indicator must reflect ‘exclusive breastfeeding for six months’.
Traditionally the use of prelacteal feeds has been a common practice in Nepal, and more recently the use of formula feeding is becoming increasingly prevalent [43]. Previous studies have reported that the introduction of prelacteal feedings or early supplementation of food or fluid is likely to interfere with normal gut microbiome [4], introduce infections [44] and interfere with the duration of breastfeeding. While, it is sometimes claimed that accounting for prelacteal and a few intermittent feeds can greatly under-estimate the rate of exclusive breastfeeding [12], ignoring prelacteal feeding would lead to losing focus on the harmful effects of prelacteal feeds as well as the early supplementation of infant formula. For instance, in our study, if prelacteal feeds were ignored, the rate of exclusive breastfeeding at first feed would be 100% as there was universal breastfeeding initiation [31]. Such interpretation of breastfeeding is also likely to mislead breastfeeding promotion programs providing a false sense of security.
Furthermore, although most studies in the past claimed to adhere to the WHO definition of exclusive breastfeeding [13, 14], we found they did not follow the definition exactly, and particularly with respect to measurement using the 24-h recall and recall-since-birth methods. Consequently, it is difficult to compare rates across studies. Similar comparability problems were also noted in Japan [45] and Australia [15] .
For health policy advocacy and planning, consistency in definition of exclusive breastfeeding and the measurement indicator is necessary in order to monitor and compare the changes in exclusive breastfeeding rates over time, across regions and between population subgroups. In addition, future research in breastfeeding needs to provide the evidence that aligns with the target of the Ministry of Health Nepal [24] and the 2025 Global Targets [9]. As a priority, future research should report both the point-in-time (24-h recall method) and life-long data (recall-since-birth method) [12] to estimate the 24-h prevalence and rate of exclusive breastfeeding for 6 months, respectively and should be used in conjunction with a well-designed cohort study taking repeated measurements. While this method is known to be more resource intensive, some sentinel sites could be established to represent the country, and prospective data could be collected periodically from these chosen sites to measure the rates of exclusive breastfeeding in Nepal [22].
The 24-h recall method is commonly adopted because of its feasibility in large nationally representative studies for evidence-based decision making in developing countries including Nepal [18, 25, 46] and is likely to continue in nationwide Demographic and Health Surveys. However, it should be noted that the statistics generated from these studies do not provide reliable data for monitoring exclusive breastfeeding rates for six months. Therefore, the resulting estimate should be reported as the ‘24-h prevalence of exclusive breastfeeding’ to avoid misinterpretation. It is recommended to increase the sample size in each infant age group from newborn up to six months. This will enable accurate reporting of the 24-h prevalence as well as the proportion of infants being exclusively breastfed according to infant age with a high power to detect any apparent age-related changes and patterns.
Conclusion
This study found that the use of the 24-h-recall measurement indicator significantly over-estimates life-long exclusive breastfeeding rates. To facilitate uniform and accurate reporting of exclusive breastfeeding rates and monitor national targets for breastfeeding, future efforts should be on reporting exclusive breastfeeding based on the recall-since-birth method, using a cohort study design and repeated measurement to collect infant feeding information.
Abbreviations
- MICS:
-
Multiple Indicator Cluster Survey
- NDHS:
-
Nepal Demographic and Health Surveys
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- WHO:
-
World Health Organization
References
Ip S, Chung M, Raman G, Trikalinos TA, Lau J. A summary of the agency for healthcare research and Quality’s evidence report on breastfeeding in developed countries. Breastfeed Med. 2009;4(S1):S-17-S-30.
Horta B, Bahl R, Martines JC, Victora C. Evidence on the long-term effects of breastfeeding: systematic review and meta-analyses. Geneva, Switzerland: WHO; 2007.
Horta BL, Loret de Mola C, Victora CG. Breastfeeding and intelligence: A systematic review and meta-analysis. Acta Paediatr. 2015;104(S467):14–9.
Thompson AL, Monteagudo-Mera A, Cadenas MB, Lampl ML, Azcarate-Peril MA. Milk-and solid-feeding practices and daycare attendance are associated with differences in bacterial diversity, predominant communities, and metabolic and immune function of the infant gut microbiome. Front Cell Infect Microbiol. 2015;5.
Bahl R, Frost C, Kirkwood BR, Edmond K, Martines J, Bhandari N, Arthur P. Infant feeding patterns and risks of death and hospitalization in the first half of infancy: multicentre cohort study. Bull World Health Organ. 2005;83(6):418–26.
Mobbs EJ, Mobbs GA, Mobbs AE. Imprinting, latchment and displacement: a mini review of early instinctual behaviour in newborn infants influencing breastfeeding success. Acta Paediatr. 2016;105(1):24–30.
Sankar MJ, Sinha B, Chowdhury R, Bhandari N, Taneja S, Martines J, Bahl R. Optimal breastfeeding practices and infant and child mortality– A systematic review and meta-analysis. Acta Paediatr. 2015;104:3–13.
Victora CG, Bahl R, Barros AJD, França GVA, Horton S, Krasevec J, Murch S, Sankar MJ, Walker N, Rollins NC. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. The Lancet. 2016;387(10017):475–90.
World Health Organization. Comprehensive implementation plan on maternal, infant and young child nutrition. Geneva: WHO; 2014.
Hector DJ. Complexities and subtleties in the measurement and reporting of breastfeeding practices. Int Breastfeed J. 2011;6:5.
Pullum TW. Exclusive breastfeeding: aligning the indicator with the goal. Glob Health Sci Pract. 2014;2(3):355–6.
Greiner T. Exclusive breastfeeding: measurement and indicators. Int Breastfeed J. 2014;9:18.
WHO. Indicators for Assessing Breastfeeding Practices. Geneva: WHO; 1991.
WHO. Indicators for assessing infant and young child feeding practices : conclusions of a consensus meeting held 6–8 November 2007 in Washington D.C., USA. Washington DC, USA: WHO; 2008.
Binns CW, Fraser ML, Lee AH, Scott J. Defining exclusive breastfeeding in Australia. J Paediatr Child Health. 2009;45(4):174–80.
Khanal V, Adhikari M, Sauer K, Zhao Y. Factors associated with the introduction of prelacteal feeds in Nepal: findings from the Nepal demographic and health survey 2011. Int Breastfeed J. 2013;8:9.
Patel A, Banerjee A, Kaletwad A. Factors Associated with Prelacteal Feeding and Timely Initiation of Breastfeeding in Hospital-Delivered Infants in India. J Hum Lact. 2013;29:572–8.
DHS overview [http://www.dhsprogram.com/What-We-Do/Survey-Types/DHS.cfm]. Accessed 6 Mar 2015.
Aarts C, Kylberg E, Hörnell A, Hofvander Y, Gebre-Medhin M, Greiner T. How exclusive is exclusive breastfeeding? A comparison of data since birth with current status data. Int J Epidemiol. 2000;29:1041–6.
Li R, Scanlon KS, Serdula MK. The validity and reliability of maternal recall of breastfeeding practice. Nutr Rev. 2005;63(4):103–10.
Win NN, Binns CW, Zhao Y, Scott JA, Oddy WH. Breastfeeding duration in mothers who express breast milk: a cohort study. Int Breastfeed J. 2006;1(28):1–5.
Binns C, Lee A, Sauer K, Hewitt K. Reported breastfeeding rates in the Asia-pacific region. Curr Pediatr Rev. 2012;8(4):339–45.
Agampodi SB, Agampodi TC, De Silva A. Exclusive breastfeeding in Sri Lanka: problems of interpretation of reported rates. Int Breastfeed J. 2009;4(14):4358–4.
Department of Health Services, Ministry of Health and Population. Annual Report 2013/2014. Kathmandu: Department of Health Services, Ministry of Health and Population; 2014.
Ministry of Health and Population (MOHP) [Nepal], New ERA, ICF International Inc. Nepal Demographic and Health Survey 2011. Kathmandu, Nepal: Ministry of Health and Population, New ERA, and ICF International, Calverton, Maryland: Ministry of Health and Population (MOHP) [Nepal], New ERA, & ICF International Inc; 2012.
Ministry of Health and Population (MOHP) [Nepal], New ERA, Inc II. Nepal Demographic and Health Survey 2001. Kathmandu, Nepal: Ministry of Health and Population, New ERA, and ICF International, Calverton, Maryland; 2002; 2002.
Ministry of Health and Population (MOHP) [Nepal], New ERA, Macro International Inc. Nepal Demographic and Health Survey 2006. Kathmandu [Nepal]: Ministry of Health and Population (MOHP) [Nepal],New ERA,and Macro International Inc.; 2007.
Karkee R, Lee AH, Khanal V, Binns CW. A community-based prospective cohort study of exclusive breastfeeding in central Nepal. BMC Public Health. 2014;14.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and ElaborationPRISMA: Explanation and Elaboration. Ann Intern Med. 2009;151(4):W-65.
Central Bureau of Statistics, UNICEF. Nepal Multiple Indicator Cluster Survey 2010-Mid and Far western regions. Kathmandu, Nepal: Central Bureau of Statistics, UNICEF,& MICS; 2012.
Khanal V, Scott JA, Lee AH, Karkee R, Binns CW. Factors associated with Early Initiation of Breastfeeding in Western Nepal. Int J Environ Res Public Health. 2015;12(8):9562–74.
Khanal V, Lee A, Karkee R, Binns C. Postpartum breastfeeding promotion and duration of exclusive breastfeeding western Nepal. Birth. 2015;42(4):329-36.
USAID, FANTA, AED, UC DAVIS, IFPRI. Indicators for assessing infant and young child feeding practices part 2: measurement. Geneva: The World Health Organization; 2010.
Dibley MJ, Roy SK, Senarath U, Patel A, Tiwari K, Agho KE, Mihrshahi S, South Asia Infant Feeding Research N. Across-country comparisons of selected infant and young child feeding indicators and associated factors in four South Asian countries. Food Nutr Bull. 2010;31(2):366–75.
Pandey S, Tiwari K, Senarath U, Agho K, Dibley MJ. Determinants of Infant Feeding Practices in Nepal: Analyses of 2006 Demographic and Health Survey Data. Ann Nutr Metab. 2006;2009(55):233–3.
Khanal V, Sauer K, Zhao Y: Exclusive breastfeeding practices in relation to social and health determinants: a comparison of the 2006 and. Nepal Demographic and Health Surveys. BMC Public Health. 2011;2013:13.
Subedi N, Paudel S, Rana T, Poudyal AK. Infant and young child feeding practices in Chepang communities. JNHRC. 2012;10(21):141–6.
Ulak M, Chandyo RK, Mellander L, Shrestha PS, Strand TA. Infant feeding practices in Bhaktapur, Nepal: a cross-sectional, health facility based survey. Int Breastfeed J. 2012;7(1):1.
Chandrashekhar TS, Joshi HS, Binu V, Shankar PR, Rana MS, Ramachandran U. Breast-feeding initiation and determinants of exclusive breast-feeding - a questionnaire survey in an urban population of western Nepal. Public Health Nutr. 2007;10(2):192–7.
Subba SH, Chandrashekhar TS, Binu VS, Joshi HS, Rana MS, Dixit SB. Infant feeding practices of mothers in an urban area in Nepal. KUMJ. 2007;5(1):42–7.
Locks LM, Pandey PR, Osei AK, Spiro DS, Adhikari DP, Haselow NJ, Quinn VJ, Nielsen JN. Using formative research to design a context-specific behaviour change strategy to improve infant and young child feeding practices and nutrition in Nepal. Matern Child Nutr. 2013;11(4):882-96.
Khanal V, da Cruz JL, Karkee R, Lee AH. Factors associated with exclusive breastfeeding in Timor-Leste: findings from Demographic and Health Survey 2009-2010. Nutrients. 2014;6(4):1691–700.
Karkee R, Lee AH, Khanal V, Binns CW. Infant feeding information, attitudes and practices: a longitudinal survey in central Nepal. International breastfeeding journal. 2014;9(1):14.
Debes AK, Kohli A, Walker N, Edmond K, Mullany LC. Time to initiation of breastfeeding and neonatal mortality and morbidity: a systematic review. BMC Public Health. 2013;13 Suppl 3:S19.
Inoue M, Binns CW, Otsuka K, Jimba M, Matsubara M. Infant feeding practices and breastfeeding duration in Japan: A review. Int Breastfeed J. 2012;7(1):15.
Senarath U, Dibley MJ, Agho KE. Factors associated with nonexclusive breastfeeding in five east and Southeast Asian countries: a multilevel analysis. J Hum Lact. 2010;26:248–57.
Acknowledgements
The authors are grateful to the mothers and their families for participation in this study, enumerators who helped with data collection, local social workers who supported data collection, staffs at the District Public Health Office, Rupandehi, and Child Health Division, Kathmandu, for their generous support during recruitment and data collection.
Funding
Authors would like to acknowledge Curtin University for supporting this study as part of VK’s PhD.
Availability of data and material
The datasets supporting the conclusions of this article are available at the institutional repository of Curtin University (http://www.curtin.edu.au). According to the data protection regulation of Curtin University, authors are not permitted to deposit the data elsewhere. A final copy of the thesis will be deposited in the institutional repository of Curtin University Library.
Authors’ contributions
VK contributed to study design, literature review, data collection, data analysis and interpretation, and writing the first draft. CB, JS and AL supervised the project, contributed to study design, data interpretation and revised the manuscript. AL and RK contributed to data analysis and interpretation of findings. All authors revised and agreed on the views expressed in the manuscript.
Competing interests
VK and JS are associate editors for BMC Pregnancy and Childbirth. Both authors do not have any role in review process and final decision.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This research project obtained approval from the Curtin University Human Research Ethics Committee, (approval number: HR 184/2013), and the Nepal Health Research Council (approval number: 773/2014). Mothers provided written consent for themselves and their infants, and personal identifiers were removed before analysis. When mother could not read and write, enumerators read the consent form for them. Mothers provided a thumb print as their initials if they agreed to participate. This method was approved by both ethics committees.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
Web Appendix: Questions asked collect breastfeeding information. (DOCX 23 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Khanal, V., Lee, A.H., Scott, J.A. et al. Implications of methodological differences in measuring the rates of exclusive breastfeeding in Nepal: findings from literature review and cohort study. BMC Pregnancy Childbirth 16, 389 (2016). https://doi.org/10.1186/s12884-016-1180-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-016-1180-9