Abstract
Background
Prognosis after vertebrobasilar stenting (VBS) may differ from that after carotid artery stenting (CAS). Here, we directly compared the incidence and predictors of in-stent restenosis and stented-territory infarction after VBS and compared them with those of CAS.
Methods
We enrolled patients who underwent VBS or CAS. Clinical variables and procedure-related factors were obtained. During the 3 years of follow-up, in-stent restenosis and infarction were investigated in each group. In-stent restenosis was defined as reduction in the lumen diameter > 50% compared with that after stenting. Factors associated with the occurrence of in-stent restenosis and stented-territory infarction in VBS and CAS were compared.
Results
Among 417 stent insertions (93 VBS and 324 CAS), there was no statistical difference in in-stent restenosis between VBS and CAS (12.9% vs. 6.8%, P = 0.092). However, stented-territory infarction was more frequently observed in VBS than in CAS (22.6% vs. 10.8%; P = 0.006), especially a month after stent insertion. HbA1c level, clopidogrel resistance, and multiple stents in VBS and young age in CAS increased the risk of in-stent restenosis. Diabetes (3.82 [1.24–11.7]) and multiple stents (22.4 [2.4–206.4]) were associated with stented-territory infarction in VBS. However, in-stent restenosis (odds ratio: 15.1, 95% confidence interval: 3.17–72.2) was associated with stented-territory infarction in CAS.
Conclusions
Stented-territory infarction occurred more frequently in VBS, especially after the periprocedural period. In-stent restenosis was associated with stented-territory infarction after CAS, but not in VBS. The mechanism of stented-territory infarction after VBS may be different from that after CAS.
Similar content being viewed by others
Introduction
Atherosclerotic stenosis of the carotid and vertebral arteries are major contributors for ischemic stroke [1]. The most important strategies for preventing ischemic stroke in these arteries are thromboembolism risk reduction and cerebral perfusion improvement. With the development of neuro-interventional devices, carotid artery stenting (CAS) has been widely used as an effective endovascular treatment to achieve this goal [2, 3]. Recently, several studies have demonstrated that not only CAS, but vertebrobasilar artery stenting (VBS) also could be acceptable and safe [4,5,6].
Vertebrobasilar artery stenosis is associated with a high risk of ischemic stroke; therefore, prediction for recurrent ischemic stroke and a more active treatment strategy after VBS may be needed for arteries with severe stenosis [7, 8]. However, data showing long-term prognosis including in-stent restenosis or ischemic stroke recurrence after VBS are still controversial, and the factors associated with these events are not clearly verified [9,10,11]. In-stent restenosis is one of the major complications after stent insertion, which was significantly associated with an increased risk of future ischemic stroke after stenting [12, 13]. A considerable proportion of patients show in-stent restenosis after revascularization treatment, and follow-up imaging is performed after stenting to detect in-stent restenosis.
Stroke mechanism and risk factors associated with atherosclerosis differs between ischemic stroke in anterior and posterior circulation [14]. Based on these facts, the incidence and factors associated with in-stent restenosis and stented-territory infarction may differ between VBS and CAS. Here, we investigated the characteristics, long-term incidence, and predictors of in-stent restenosis after VBS and CAS. Moreover, we directly compared the difference in the effect of in-stent restenosis for recurrent infarction between VBS and CAS.
Methods
Study population and clinical data
We retrospectively reviewed data of patients who were admitted to the stroke center of our tertiary hospital and received stent insertion at the cervico-cerebral arteries between September 2013 and May 2021. Patients were included if they fulfilled the following criteria: (1) age > 18 years; (2) symptomatic carotid or vertebrobasilar stenosis ≥50% or asymptomatic stenosis ≥70% diagnosed by digital subtraction angiography (DSA). Patients who had never undergone follow-up neuroimaging after stent insertion were excluded.
Baseline demographics and vascular risk factors were collected from all patients. Laboratory values of hemoglobin A1c (HbA1c) and low-density lipoprotein (LDL) cholesterol were obtained during admission, prior to stenting. All patients received aspirin and clopidogrel for at least 5 days before the procedure. The resistance to antiplatelet treatment was tested and expressed as aspirin reaction units (ARUs), P2Y12 reaction units (PRUs), and percentage of platelet inhibition (%PI). ARUs ≥550, PRUs ≥275, or %PI < 20% was defined as resistance to antiplatelet treatment [15]. Regardless of the resistance, all patients received aspirin and clopidogrel during the periprocedural period. Informed consent was not obtained from patients due to the retrospective nature of this study. The local ethics committee approved this study (IRB No. 2022–0348).
Procedure-related factors
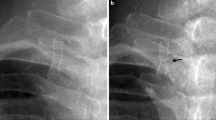
Stenting procedure was performed by neuro-interventionists who were highly experienced in endovascular treatment. The use of catheters, guidewires, and ballooning dilatation was at the discretion of the neuro-interventionist. Wingspan (Boston Scientific), Vision (Abbott Laboratories), and Enterprise (Codman Neuro) stents were used for intracranial stenting, and the Protégé (Covidien), Precise (Cordis), and Acculink (Abbott Laboratories) stents were used for extracranial stenting. The number, location, maximum diameter, and total length of stents, and the ballooning dilatation and pressure were recorded. The degree of stenosis was evaluated according to the North American Symptomatic Carotid Endarterectomy Trial (NASCET) criteria. Stenosis ≥70% was defined as severe and 50–70% as moderate. Symptomatic stenosis was defined as ischemic stroke or transient ischemic attack in a patient within the previous 6 months, resulting from a narrow artery.
Follow-up neuroimaging and clinical outcomes
All patients were followed up with computed tomography angiography (CTA) and carotid duplex ultrasonography (CDU) within 48 hours after the procedure. After discharge, all patients were followed up with CTA and CDU at 1 month after the procedure. After that, patients were followed up with CTA, CDU, magnetic resonance angiography (MRA), or DSA examination at 6 months after the procedure at the discretion of the stroke neurologist. Thereafter, follow-up neuroimaging was performed every 12 months.
The main outcomes were in-stent restenosis and stented-territory infarction. Restenosis higher than 50% of the residual stenosis just after stent insertion at any period during follow-up was considered as in-stent restenosis, regardless of the neuroimaging modality used. Stented-territory infarction was defined as stented-territory ischemic stroke on diffusion-weighted imaging or transient ischemic attack (TIA), associated with the stented artery. Stented-territory infarction was dichotomized according to the event time (periprocedural [≤1 month] vs. long-term [> 1 month]). We additionally obtained any territory infarction, which was defined as any territory ischemic stroke or TIA regardless of the location of stenting. The events were obtained up to 36 months after the procedure, from the outpatient clinic. All images were analyzed by two stroke neurologists (first author and corresponding author) separately, blinded to all the clinical data.
Statistical analysis
First, we compared the baseline characteristics, the incidence of in-stent restenosis, and stented-territory infarction between VBS and CAS. The significance of differences was assessed using the Chi-square test, Mann–Whitney U-test, or t-test, as appropriate. In-stent restenosis and stented-territory infarction during the follow-up were evaluated using the Kaplan–Meier method. Log-rank tests were used to compare the cumulative incidence between VBS and CAS. In subgroup analysis, for the comparison of intra- vs. extra-cranial stenting, in-stent restenosis and stented-territory infarction during the follow-up period between intra- and extracranial VBS were compared using Kaplan-Meier method and log-rank tests. Moreover, in-stent restenosis and stented-territory infarction between intra- and extracranial CAS were also compared using the same methods.
We performed univariable cox proportional analysis for in-stent restenosis in VBS and CAS separately, and for stented-territory infarction in VBS and CAS. In the latter analysis, in-stent restenosis prior to stented-territory infarction was included as a variable. Variables with potential association (P < 0.10) were entered to the multivariable cox proportional analysis. P-value < 0.05 was considered statistically significant. The proportional-hazards assumption was checked by examining the Schoenfeld residuals plot and method against time. All analyses were performed using R Software (version 4.0.5; R Foundation for Statistical Computing, Vienna, Austria).
Results
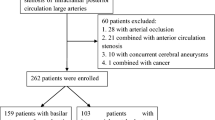
During the study period, 439 patients received stent insertion at the cervico-cerebral arteries. We excluded 5 (1.1%) patients with stent inserted only in the subclavian artery, and 71 (16.2%) patients without any follow-up neuroimaging after stent insertion. Finally, 363 patients who had undergone 417 stent insertions were included (stenting at more than two arteries: 53 patients). The mean age was 66.7 ± 10.1 years, and 341 (81.8%) patients were males. A total of 324 (77.7%) patients underwent CAS and 93 (22.3%) underwent VBS. The follow-up neuroimaging modalities at the last follow-up were CTA (n = 242 [58.3%]), CDU (n = 136 [32.6%]), DSA (n = 26 [6.2%]), and MRA (n = 13 [3.1%]).
Baseline characteristics
The clinical characteristics of patients who underwent VBS and CAS are summarized in Table 1. The mean age was significantly lower in the VBS group than in the CAS group (63.0 ± 11.8 vs. 67.8 ± 9.3 years, P < 0.001). There was less coronary artery disease in the VBS group than in the CAS group (P = 0.010). Procedurally, intracranial stenting was more frequently performed in the VBS group than in the CAS group (P < 0.001). Moreover, the proportion of symptomatic stenosis before stenting was higher (85 [91.4%] vs. 246 [75.9%], P = 0.002), and the maximum diameter and length of stents were smaller and shorter (P < 0.001, P < 0.001, respectively) in the VBS group than in the CAS group. Furthermore, the proportion of post-ballooning dilatation (24 [25.8%], vs. 150 [46.3%], P = 0.001) and maximum balloon pressure (9.5 ± 3.6 atm. vs. 10.7 ± 3.1 atm., P = 0.002) was lower in the VBS group than in the CAS group.
In-stent restenosis and stented-territory infarction
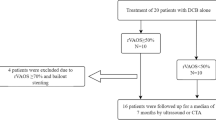
For clinical outcomes, in-stent restenosis was observed in 34 (8.2%) stent insertion cases and stented-territory infarction was observed in 56 (13.4%) stent insertion cases during 3 years of follow-up. There was no difference in in-stent restenosis between VBS and CAS groups (12 [12.9%] vs. 22 [6.8%], P = 0.092). However, stented-territory infarctions were more frequent in the VBS than in the CAS group (21 [22.6%] vs. 35 [10.8%], P = 0.006). Though the occurrence of stented-territory infarction did not differ in the periprocedural period, there was significant difference in long-term stented-territory infarctions between the two groups (15 [16.1%] vs. 11 [3.4%], P < 0.001). Any territory infarctions (23 [24.7%] vs. 43 [13.3%], P = 0.012) also occurred more frequently in- the VBS than in the CAS group.
Kaplan–Meier curve between VBS and CAS is demonstrated in Fig. 1. The incidence of in-stent restenosis in VBS vs. CAS were 10.4% vs. 6.2% at 12 months, 15.7% vs. 8.2% at 24 months, and 18.1% vs. 10.9% at 36 months. There was no significant difference in the occurrence of in-stent restenosis between the two groups (P = 0.130). The cumulative incidences of stented-territory infarction in VBS vs. CAS were 18.6% vs. 9.7% at 12 months, 18.6% vs. 11.1% at 24 months, and 25.3% vs. 11.7% at 36 months. The occurrence of any territory infarction and stented-territory infarction were higher in the VBS than in the CAS group (P = 0.016, and P = 0.006, respectively). In subgroup analysis, there were no statistical differences in the occurrence of in-stent restenosis and stented-territory infarction between intra- and extracranial VBS (P = 0.229 and P = 0.152). Moreover, the occurrences of in-stent restenosis and stented-territory infarction between intra- and extracranial CAS showed no significant differences (P = 0.137 and P = 0.215; Supplemental Fig. 1).
Predictors of in-stent restenosis in VBS and CAS
Multivariable cox proportional analysis showed that HbA1c level (hazard ratio 1.78, 95% confidence interval [1.06–2.98], P = 0.029), %PI < 20% (4.20 [1.09–16.2], P = 0.037), and number of stents ≥2 (46.3 [2.9–749.0], P = 0.007) increased the risk of in-stent restenosis in VBS (Supplemental Table 1).
Univariable cox proportional analysis showed that the age of patients (hazard ratio 0.95, 95% confidence interval 0.91–0.98, P = 0.003), number of stents ≥2 (3.51 [0.82–15.0], P = 0.091), maximum diameter of stents (0.70 [0.58–0.84], P < 0.001), and total length of stents (0.95 [0.92–0.99], P = 0.016) were the potential predictors of in-stent restenosis in CAS (Supplemental Table 2). In multivariable analysis, age (0.96 [0.92–1.00], P = 0.042) was independently associated with the risk of in-stent restenosis in CAS.
Predictors of stented-territory infarction in CAS and VBS
Univariable cox proportional analysis showed that diabetes (3.17 [1.09–9.18], P = 0.034), HbA1c level (1.48 [0.96–2.28], P = 0.075), and the number of stents ≥2 (11.6 [1.42–94.0], P = 0.022) were potential predictors for long-term stented-territory infarction in VBS (Table 2). HbA1c levels were not included in the multivariable analysis, as there was multicollinearity between diabetes and HbA1c levels. Diabetes (3.82 [1.24–11.7], P = 0.019) and having ≥2 stents (22.4 [2.4–206.4], P = 0.006) were associated with long-term stented-territory infarction in VBS.
On the other hand, hypertension (0.30 [0.09–1.07], P = 0.064), maximum diameter (0.64 [0.48–0.86], P = 0.003) and total length of stents (0.93 [0.88–0.98], P = 0.009), and in-stent restenosis (24.3 [6.84–86.3], P < 0.001) were potentially associated with long-term stented-territory infarction in CAS (Table 3). Among them, in-stent restenosis (15.1 [3.17–72.2], P < 0.001) was the predictor of long-term stented-territory infarction in CAS in multivariable cox proportional analysis.
Discussion
Our study shows that stented-territory infarctions were significantly more frequent after VBS than after CAS, especially in the long-term. The predictors for in-stent restenosis and stented-territory infarction also differed; in-stent restenosis was a predictor for stented-territory infarction for CAS, but not for VBS. For those who received VBS, in-stent restenosis was associated with HbA1c level, clopidogrel resistance, and multiple stents; while stented-territory infarction was associated with diabetes and multiple stents.
The cumulative incidences of in-stent restenosis reported from separate studies on VBS and CAS, including a meta-analysis, were in line with our current results [13, 16,17,18,19]. Furthermore, previous meta-analysis showed the indifference of the occurrence of in-stent restenosis between intra- and extracranial VBS [9]. Although the results of previous reports were heterogenous, the periprocedural complication rate was low and the safety was acceptable for both intra-and extra-cranial VBS [9,10,11, 20, 21]. In the current study, periprocedural complication rate was similar between VBS and CAS. However, long-term stented-territory infarction was more frequently observed in VBS than in CAS. This may be explained by the difference in the location of stenting and stroke mechanism. In our patient cohort, half of the patients received stenting at the origin of the vertebral artery, and the other half received stenting at the distal vertebral or basilar artery. Those who received stenting at the distal vertebral or basilar artery might have had a stroke due to occlusion of the perforators. The occlusion of the perforators can be caused by in-stent atherosclerosis, even with stenosis less than 50% [14]. Therefore, though the incidence of in-stent restenosis was not significantly higher in those who had received VBS, still the risk of stroke may be higher in VBS. During the long-term follow-up period, a considerable portion of patients who had undergone VBS had stroke due to occlusion of the perforators (Supplemental Table 3). However, there was no significant difference in the proportion of long-term stented-territory ischemic event between the intra- and extra-cranial VBS (10/54 [18.5%] vs. 5/39 [12.8%], respectively, P = 0.461; data not shown). A study with larger number of patients comparing stented-territory infarction between intra- and extracranial VBS may be needed to clarify this issue.
Stented-territory infarction after VBS was not associated with in-stent restenosis. On the contrary, stented-territory infarction after CAS, which is mostly caused by artery-to-artery embolism, was significantly associated with in-stent restenosis [13, 22]. Stenosis degree more than 50% is critical for platelet aggregation and distal embolism. Younger age increased the risk of in-stent restenosis in CAS. Lower intimal cell proliferation and consequent lower intimal hyperplasia could help explaining this result [23]. In case of VBS, in-stent restenosis and stented-territory infarction was more associated with metabolic components, such as high HbA1c levels or the history of diabetes. Diabetes and metabolic syndrome are well-known risk factors for stroke in the posterior circulation [24]. Diabetes is also a major risk factor for branch atheromatous disease, which may be an important stroke mechanism in those who had received VBS [25]. Actively controlling diabetes, which may prevent development of atherosclerosis within the stent placed at the posterior circulation may be important after VBS.
Our study has some limitations. First, due to the retrospective nature of this study, patients with follow-up neuroimaging were limited, which might have caused a selection bias. Second, follow-up neuroimaging modality was heterogenous. This heterogenicity might have caused discrepancies in the incidence of in-stent restenosis, subsequently affecting the results. Third, we alternatively investigated the number, diameter, and length of stents, instead of the arterial diameter, the ratio of stenosis, and the maximum size of balloon. This difference might have affected the results of our study. Finally, this study was conducted at a single center; therefore, it is difficult to generalize the results. However, owing to this, the procedure was standardized, and it may not have affected the result.
Despite these limitations, we directly compared the prevalence and risk factors associated with VBS and CAS. The periprocedural risk was similar, however, VBS showed a higher risk of stented-territory infarction at long-term follow-up. In-stent restenosis was a risk factor for stented-territory infarction in CAS, whereas diabetes was associated with in-stent restenosis and stented-territory infarction in VBS.
Availability of data and materials
Data are available upon reasonable request to the corresponding author.
Abbreviations
- CAS:
-
Carotid artery stenting
- VBS:
-
Vertebrobasilar artery stenting
- DSA:
-
Digital subtraction angiography
- HbA1c:
-
Hemoglobin A1c
- LDL:
-
Low-density lipoprotein
- ARUs:
-
Aspirin reaction units
- PRUs:
-
P2Y12 reaction units
- %PI:
-
Percentage of platelet inhibition
- NASCET:
-
North American Symptomatic Carotid Endarterectomy Trial
- CTA:
-
Computed tomography angiography
- CDU:
-
Carotid duplex ultrasonography
- TIA:
-
Transient ischemic attack
References
Kim BJ, Kwon JY, Jung JM, Lee DH, Kang DW, Kim JS, et al. Association between silent embolic cerebral infarction and continuous increase of P2Y12 reaction units after neurovascular stenting. J Neurosurg. 2014;121:891–8.
Brott TG, Hobson RW 2nd, Howard G, Roubin GS, Clark WM, Brooks W, et al. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med. 2010;363:11–23.
Brott TG, Howard G, Roubin GS, Meschia JF, Mackey A, Brooks W, et al. Long-term results of stenting versus endarterectomy for carotid-artery stenosis. N Engl J Med. 2016;374:1021–31.
Markus HS, Harshfield EL, Compter A, Kuker W, Kappelle LJ, Clifton A, et al. Stenting for symptomatic vertebral artery stenosis: a preplanned pooled individual patient data analysis. Lancet Neurol. 2019;18:666–73.
Jiang WJ, Xu XT, Du B, Dong KH, Jin M, Wang QH, et al. Long-term outcome of elective stenting for symptomatic intracranial vertebrobasilar stenosis. Neurology. 2007;68:856–8.
Drazyk AM, Markus HS. Recent advances in the management of symptomatic vertebral artery stenosis. Curr Opin Neurol. 2018;31:1–7.
Compter A, van der Worp HB, Schonewille WJ, Vos JA, Boiten J, Nederkoorn PJ, et al. Stenting versus medical treatment in patients with symptomatic vertebral artery stenosis: a randomised open-label phase 2 trial. Lancet Neurol. 2015;14:606–14.
Fiorella D, Derdeyn CP, Lynn MJ, Barnwell SL, Hoh BL, Levy EI, et al. Detailed analysis of periprocedural strokes in patients undergoing intracranial stenting in stenting and aggressive medical Management for Preventing Recurrent Stroke in intracranial stenosis (SAMMPRIS). Stroke. 2012;43:2682–8.
Jiang Y, Xu X, Wen Z, Xu X, Yang L, Liu X. In-stent restenosis after vertebral artery stenting. Int J Cardiol. 2015;187:430–3.
Vajda Z, Schmid E, Güthe T, Klötzsch C, Lindner A, Niehaus L, et al. The modified Bose method for the endovascular treatment of intracranial atherosclerotic arterial stenoses using the Enterprise stent. Neurosurgery. 2012;70:91–101 discussion.
Song L, Li J, Gu Y, Yu H, Chen B, Guo L, et al. Drug-eluting vs. bare metal stents for symptomatic vertebral artery stenosis. J Endovasc Ther. 2012;19:231–8.
Jin M, Fu X, Wei Y, Du B, Xu XT, Jiang WJ. Higher risk of recurrent ischemic events in patients with intracranial in-stent restenosis. Stroke. 2013;44:2990–4.
Bonati LH, Gregson J, Dobson J, McCabe DJH, Nederkoorn PJ, van der Worp HB, et al. Restenosis and risk of stroke after stenting or endarterectomy for symptomatic carotid stenosis in the international carotid stenting study (ICSS): secondary analysis of a randomised trial. Lancet Neurol. 2018;17:587–96.
Kim JS, Nah HW, Park SM, Kim SK, Cho KH, Lee J, et al. Risk factors and stroke mechanisms in atherosclerotic stroke: intracranial compared with extracranial and anterior compared with posterior circulation disease. Stroke. 2012;43:3313–8.
Campo G, Fileti L, de Cesare N, Meliga E, Furgieri A, Russo F, et al. Long-term clinical outcome based on aspirin and clopidogrel responsiveness status after elective percutaneous coronary intervention: a 3T/2R (tailoring treatment with tirofiban in patients showing resistance to aspirin and/or resistance to clopidogrel) trial substudy. J Am Coll Cardiol. 2010;56:1447–55.
Cosottini M, Michelassi MC, Bencivelli W, Lazzarotti G, Picchietti S, Orlandi G, et al. In stent restenosis predictors after carotid artery stenting. Stroke Res Treat. 2010:864724.
Clavel P, Hebert S, Saleme S, Mounayer C, Rouchaud A, Marin B. Cumulative incidence of restenosis in the endovascular treatment of extracranial carotid artery stenosis: a meta-analysis. J Neurointerv Surg. 2019;11:916–23.
Li J, Hua Y, Needleman L, Forsberg F, Eisenbray JR, Li Z, et al. Arterial occlusions increase the risk of in-stent restenosis after vertebral artery ostium stenting. J Neurointerv Surg. 2019;11:574–8.
Chen W, Huang F, Li M, Jiang Y, He J, Li H, et al. Incidence and predictors of the in-stent restenosis after vertebral artery ostium stenting. J Stroke Cerebrovasc Dis. 2018;27:3030–5.
Markus HS, Larsson SC, Kuker W, Schulz UG, Ford I, Rothwell PM, et al. Stenting for symptomatic vertebral artery stenosis: the vertebral artery Ischaemia stenting trial. Neurology. 2017;89:1229–36.
Liu L, Zhao X, Mo D, Ma N, Gao F, Miao Z. Stenting for symptomatic intracranial vertebrobasilar artery stenosis: 30-day results in a high-volume stroke center. Clin Neurol Neurosurg. 2016;143:132–8.
Müller MD, Gregson J, McCabe DJH, Nederkoorn PJ, van der Worp HB, de Borst GJ, et al. Stent design, restenosis and recurrent stroke after carotid artery stenting in the international carotid stenting study. Stroke. 2019;50:3013–20.
Mousa AY, AbuRahma AF, Bozzay J, Broce M, Kali M, Yacoub M, et al. Long-term comparative outcomes of carotid artery stenting following previous carotid endarterectomy vs De novo lesions. J Endovasc Ther. 2015;22:449–56.
Kuroda J, Matsuo R, Yamaguchi Y, Sato N, Kamouchi M, Hata J, et al. Poor glycemic control and posterior circulation ischemic stroke. Neurol Clin Pract. 2019;9:129–39.
Sun LL, Li ZH, Tang WX, Liu L, Chang FY, Zhang XB, et al. High resolution magnetic resonance imaging in pathogenesis diagnosis of single lenticulostriate infarction with nonstenotic middle cerebral artery, a retrospective study. BMC Neurol. 2018;18:51.
Acknowledgements
None.
Funding
This research was supported by grants from the Brain Convergence Research Program of the National Research Foundation funded by the Korean government (MSIT No. 2020M3E5D2A01084576) and the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT No. 2020R1A2C2100077).
Author information
Authors and Affiliations
Contributions
JC Ryu contributed to the study concept and design, data collection and interpretation, and draft preparation and revision of the manuscript. JH Bae, SH Ha, BS Kwon, YS Song, DH Lee, JY Chang, DW Kang, SU Kwon, JS Kim contributed to data interpretation and revision of the manuscript. BJ Kim contributed to the study concept and design, data interpretation, and draft preparation and revision of the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations. This study was approved by the local ethics committee of Asan Medical Center (IRB No. 2022–0348). The Asan Medical Center waived the written informed consent because this study was retrospective.
Consent for publication
Not applicable. No information or images that could lead to identification of a study participant was mentioned in our study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplemental Table 1.
Hazard ratio for in-stent restenosis using a cox proportional analysis in VBS. Supplemental Table 2. Hazard ratio for in-stent restenosis using a cox proportional analysis in CAS. Supplemental Table 3. Stroke mechanism of stented-territory infarction in VBS. Supplemental Figure 1. A) Comparison of in-stent restenosis and stented-territory infarction between intra- and extracranial VBS. B) Comparison of in-stent restenosis and stented-territory infarction between intra- and extracranial CAS.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ryu, JC., Bae, JH., Ha, S.H. et al. In-stent restenosis and stented-territory infarction after carotid and vertebrobasilar artery stenting. BMC Neurol 23, 79 (2023). https://doi.org/10.1186/s12883-023-03110-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-023-03110-z