Abstract
Background
Wilson’s disease (WD) is an inherited disorder in which defective biliary excretion of copper leads to its accumulation, particularly in the liver and brain. Systemic lupus erythematosus (SLE) is a multi-system disorder that can manifest in any system. Cases with concomitant WD and SLE, unrelated to treatment with penicillamine, have been rarely reported.
Case presentation
We report a case of a young woman who had typical neuropsychiatric symptoms and laboratory tests results of WD. She also had concomitant massive hematuria and proteinuria, fever, multiple positive autoimmune antibodies, hypocomplementemia, abnormal lumbar puncture findings and evidence of Sjögren syndrome, which are all rare in WD. Hence, we considered the diagnosis of SLE. Tapering of steroid dosage also confirmed the diagnosis.
Conclusion
Wilson’s disease and SLE have varied clinical manifestations. Herein, we reported a rare case in which the two conditions concomitantly existed. In clinical practice, differential diagnosis of the two diseases is necessary for patients with hepatic, neurological, and psychiatric manifestations.
Similar content being viewed by others
Background
Wilson’s disease (WD) is an inherited disorder with defective biliary excretion of copper that leads to its accumulation, particularly in the liver and brain. Systemic lupus erythematosus (SLE) is a multi-system disorder that can manifest in any system. We report a case of a young woman who had typical neuropsychiatric symptoms of WD as well as other abnormalities unrelated to WD. The diagnosis of SLE gradually emerged, although cases with concomitant WD and SLE, unrelated to treatment with penicillamine, have been rarely reported.
Case presentation
An 18-year-old female was admitted to Peking Union Medical College Hospital in November 2016 with the chief complaints of abnormal limb movements and slurred speech for two years, which worsened 20 days ago. Initially, her movements were slower, her hands were clumsy, and she could not speak clearly. In the past 20 days, she gradually developed dysdipsia, unsteady gait, dyskinesia, significantly increased involuntary movements of limbs and fell > 4 times. Cranial magnetic resonance imaging (MRI) showed abnormal signals in bilateral basal ganglia and thalamus. Electroencephalography (EEG) demonstrated diffused 4–6 Hz theta waves. Slit-lamp examination showed Kayser–Fleischer (KF) ring in both eyes. Her serum ceruloplasmin concentration was 0.033 g/L (Normal range: 0.2–0.6). The symptoms progressively worsened, and she had a fever, with temperature between 37.5 and 38.0 °C, without chills, cough or diarrhea. The patient had difficulty in opening her mouth, could only speak one word at a time, and had occasional torsion spasm at the time of admission.
The patient had xerostomia, keratoconjunctivitis sicca, frequent oral ulcers, with no significant weight loss. There was no history of other diseases, but her mother recalled that she talked less, had behavioral changes, abnormal gait, involuntary smile and involuntary movements of all limbs since five years. The parents and older sister did not have similar symptoms. Physical examination revealed that the patient had normal comprehension, with low-grade fever, hepatomegaly, splenomegaly, dystonia, lack of coordination, slight tremor, dysarthria, dysphagia and right side Babinski sign positive.
After admission, routine tests revealed decreased white blood cell count of 2.87*109/L (Normal range: 4–10). Liver function test showed slightly elevated transaminase level and normal bilirubin level. Albumin level was decreased to 32 g/L (Normal range: > 35). Renal parameters were marginally elevated with proteinuria (1.12 g/24 h) and hematuria (++). Lumbar puncture showed elevated intracranial pressure, normal white blood cell count of 2/ul, elevated protein of 0.69 g/L and elevated immunoglobulin G (IgG) of 58.8 mg/L (Normal range: 0–40). Anti-AQP-4 (Anti-aquaporin 4) IgG and myelin basic protein were negative. MRI revealed symmetric abnormal signals with low signal in T1-weighted image, and high signals in T2-weighted and FLAIR images of bilateral basal ganglia thalamus, midbrain, and pons (Fig. 1). Computed tomography (CT) scans revealed diffused lesions in the liver, uneven density, and hepatosplenomegaly. The patient, her parents and her sister underwent genotype test for WD, which showed that the patient had a compound heterozygous mutation, while her family members did not.
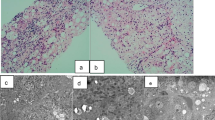
Other laboratory findings included elevated ESR, C-reactive protein, IgG, IgM and hypocomplementemia. The titers of antinuclear antibody (ANA) (S1:640), anti-SSA antibody (+++) and anti-rRNP antibody (+++) were remarkably increased, while anticardiolipin antibodies (ACL), Lupus anticoagulants (LA), and anti-β2-glycoprotein-1 (anti-β2GP1) antibodies were all positive. Stomatological and ophthalmological evaluations provided objective evidence of salivary gland (salivary flow rate and parotid sialography) and ocular (Schirmer’s test and ocular dye score) involvement. Salivary gland biopsy showed typical histopathology of Sjögren syndrome. Magnetic resonance angiography (MRA) showed normal arteries, and ultrasound examinations of arteries and veins of bilateral legs, bilateral subclavian, supra-mesenteric, inferior-mesenteric, bilateral renal found no thrombotic evidence.
Based on all the findings, the final diagnosis for this patient was WD, SLE, secondary Sjögren syndrome with anti-phospholipid (aPL) antibodies. Therefore, we started therapy with iv sodium dimercaptopropane sulfonate (DMPS), full dose zinc sulfate for WD, and methylprednisolone (80 mg iv for 7 days, then 40 mg po for 3 weeks), and hydroxychloroquine po for SLE, respectively. Since has three kinds of aPL antibodies were positive, the patient was also treated with anticoagulant therapy (low molecular weight heparin, and then aspirin po). One month later, her neurological symptoms and laboratory tests showed improvement. WBC count, liver function test including transaminase level, bilirubin level and serum albumin level, urine test, ESR, CRP, IgG and complement levels were all normal. Repeat lumbar puncture showed normal parameters. The titer of ANA had declined (S1:160), and aPL (ACL, LA, anti-β2GP1) antibodies were negative. The steroid dosage was gradually tapered and the patient was given oral dimercaptosuccinate (DMSA), zinc sulfate, hydroxychloroquine and aspirin for maintenance.
The patient was followed-up every three months at the outpatient clinic. Six months after discharge, her symptoms recurred, and she developed hyponatremia, hematuria and proteinuria, when the steroid was reduced to 2 mg/day. Hence, methylprednisolone dosage was increased to 16 mg/day, while the other treatment remained unchanged. Symptoms and abnormal laboratory findings were relieved in the next follow-up.
Discussion and conclusions
Wilson’s disease (WD) is an inherited disorder caused by mutations of the ATP7B gene on chromosome 13, which encodes a copper-transporting P-type ATPase (ATP7B) residing in the trans-Golgi network of hepatocytes. Our patient had a compound heterozygous mutation of ATP7B (Fig. 2), while her parents and sister did not. The clinical features of WD may include hepatic, neurological, and psychiatric manifestations. More than 90% of patients with neurological manifestations have a KF ring [1,2,3].
Our patient first showed symptoms of abnormal behavior several years before diagnosis. Literature review indicated that psychiatric problems can be the earliest manifestation in adult patients. In addition to the three main movement disorders including dystonia, lack of coordination, and tremor, our patient also presented some common neurological features of WD, such as dysarthria and dysphagia. MRI and CT scans showed typical findings of WD. However, lumbar puncture revealed increased pressure, increased protein level and immunoglobulin level, which were unrelated to WD. Moreover, our patient had massive hematuria and proteinuria, which are rare in WD. Because of fever, multiple autoimmune antibody positive, hypocomplementemia, renal involvement, abnormal lumbar puncture findings and evidence of Sjögren syndrome, we considered the diagnosis of SLE. Tapering of steroid dosage also confirmed the diagnosis.
WD can concurrently occur with autoimmune hepatitis and Coomb’s positive autoimmune hemolytic anemia [4, 5]. SLE has been reported to be associated with WD in patients treated with penicillamine in the form of drug-induced lupus (DILE). DILE has several different features from SLE [6]. But concomitant SLE and WD without penicillamine treatment is rare [7,8,9]. A possible pathogenetic mechanism of Fas-mediated apoptosis might play a role in autoimmune disease and WD [10]. In such patients, penicillamines should be avoided. According to the guidelines, we used iv DMPS and oral DMSA for this patient, followed by maintainance zinc monotherapy for WD, and 4 mg methylprednisolone and hydroxychloroquine for SLE. The patient has been following-up for 1.5 years, and her liver function and neurological condition continues to be stable [11].
Wilson’s disease and SLE have varied clinical manifestations. Herein, we reported a rare case in which the two conditions concomitantly existed. In clinical practice, differential diagnosis of the two diseases is necessary for patients with hepatic, neurological, and psychiatric manifestations.
Abbreviations
- ACL:
-
Anticardiolipin antibodies
- Anti-AQP4:
-
Anti-aquaporin 4
- Anti-β2GP1:
-
Anti-β2-glycoprotein-1 antibodies
- aPL:
-
Anti-phospholipid
- APS:
-
Anti-phospholipid antibody syndrome
- CT:
-
Computed tomography
- DILE:
-
Drug-induced lupus
- DMPS:
-
Sodium dimercaptopropane sulfonate
- DMSA:
-
Dimercaptosuccinate
- EEG:
-
Electroencephalograph
- IgG:
-
Immunoglobulin G
- KF ring:
-
Kayser–Fleischer ring
- LA:
-
Lupus anticoagulants
- MRA:
-
Magnetic resonance angiography
- MRI:
-
Magnetic resonance imaging
- SLE:
-
Systemic lupus erythematosus
- WD:
-
Wilson’s disease
References
Roberts EA, Schilsky ML. A practice guideline on Wilson disease. Hepatology. 2003;38(2):1475–92.
Gitlin JD. Wilson disease. Gastroenterology. 2003;125(6):1868–77.
Thomas GR, Forbes JR, Roberts EA, et al. The Wilson disease gene: spectrum of mutations and their consequences. Nat Genet. 1995;9(2):210–7.
Milkiewicz P, Saksena S, Hubscher SG, et al. Wilson’s disease with superimposed autoimmune features: report of two cases and review. J Gastroenterol Hepatol. 2000;15(5):570–4.
Guha SK, Modak D, Basu A, et al. Coomb’s positive autoimmune Haemolytic Anaemia in a case of Wilson disease: co-incidence or association? JIACM. 2009;10(1 & 2):78–80.
Walshe JM. Penicillamine and the SLE syndrome. J Rheumatol Suppl. 1981;7:155.
Dell'Era L, Boati E, Nebbia G, et al. Wilson’s disease treated with penicillamine and lupus erythematosus: related or distinct entities? Minerva Pediatr. 2012;64(1):55.
Kim TY, Lee SH, Kim TJ, et al. A case of fulminant hepatic failure in Wilson's disease combined with systemic lupus erythematosus. Taehan Kan Hakhoe Chi. 2002;8(1):100–4.
Santhakumar R, Gayathri K, Ramalingam PK, et al. Wilson’s disease with systemic lupus erythematosus. J Assoc Physicians India. 2016;64(4):81.
Stassi G, Di FV, Todaro M, et al. Involvement of Fas/FasL system in the pathogenesis of autoimmune diseases and Wilson’s disease. Arch Immunol Ther Exp. 1999;47(3):129.
Ranucci G, Dato FD, Tufano M, et al. Long term follow-up of Wilson disease patients diagnosed in childhood: reasons for treatment changes. Dig Liver Dis. 2013;45(5444):e273.
Acknowledgments
We thank all the physicians from the division of general internal medicine of PUMCH who contributed to the patient care.
Funding
This work was supported by the National Health and Family Planning Commission of People’s Republic of China (No. 201502024).
Availability of data and materials
All data generated or analyzed during this study are included in the published article.
Author information
Authors and Affiliations
Contributions
YZ drafted the main manuscript. DW collected the clinical data and redrafted the manuscript. WW participated in the care of the patient and paper review. XZ conceptualized and executed the case report. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This case report was approved by the Ethics Board of Peking Union Medical College Hospital.
Consent for publication
Written informed consent was obtained from the patient and her parents for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zhang, Y., Wang, D., Wei, W. et al. Wilson’s disease combined with systemic lupus erythematosus: a case report and literature review. BMC Neurol 18, 85 (2018). https://doi.org/10.1186/s12883-018-1085-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-018-1085-5