Abstract
Background
Congenital central hypoventilation syndrome (CCHS) is a rare disease characterized by severe central hypoventilation due to abnormal autonomic control of breathing. The PHOX2B gene, mutations of which define the disease, is expressed in a group of nuclei located in brainstem areas. Pathways controlling breathing and auditory pathways traverse very similar anatomic structures. In the present study, we measure brainstem auditory evoked potentials (BAEP) to assess auditory pathways in CCHS and investigate to which extent brainstem auditory pathways are also affected.
Methods
BAEPs were measured in 15 patients with PHOX2B mutations positive CCHS (8 boys and 7 girls. mean age 6.3 yrs ± 5) as part of their regular follow-up in the Centre of reference for central hypoventilation (Robert Debré University Hospital. Paris. France).
Results
BAEP responses were found normal in nine patients (60% of the study group) and abnormal in the other six (40%). Abnormal BAEPs which resulted from brainstem dysfunction were found in three patients (20%).
Conclusion
Dysfunction of brainstem auditory pathways can be observed in CCHS. However, auditory evoked responses can be normal in the disease, therefore suggesting much more complex yet-to-be determined interactions between pathways and functions of central control of breathing and of control of hearing.
Similar content being viewed by others
Background
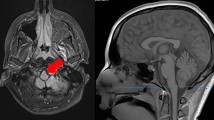
Congenital central hypoventilation syndrome (CCHS) is a rare disease characterized by abnormal autonomic control of breathing resulting in severe alveolar hypoventilation that is most marked during non-rapid eye movement sleep [1,2]. Incidence of CCHS is estimated to be around 1 for 200 0000 live births [3]. Mutations of the PHOX2B gene have been found in over 90% of the cases [4,5]. CCHS is frequently associated with a number of clinical conditions caused by abnormal development of the autonomic nervous system: Hirschsprung’s disease [5,6], neural crest tumors [3], reduced or absent central chemosensitivity and dyspnea sensations [7,8], heart rate and blood pressure dysregulation [9-11], esophageal dysmotility [12] and ocular disorders [13]. Widespread dysfunction of brainstem structures has been shown based upon functional magnetic resonance imaging (fMRI) studies of patients with CCHS [14-18].
Brainstem auditory evoked potentials (BAEP) are the changes in the ongoing electric activity generated in auditory pathways of the brain that is elicited by external auditory stimuli. Auditory pathways start from the auditory nerve (wave I) to the cochlear nuclei (wave II) in the medulla to the superior olivary complex (wave III) in the pons and end in the inferior colliculus (waves IV and V) in the midbrain. Prolonged latencies of the different waves and prolonged interpeaks latencies of BAEPs are considered as resulting from dysfunction of auditory pathways [19]. Recordings of BAEPs are used as a non-invasive neurophysiologic method to assess brainstem function, both in adults and in children, and may aid in the evaluation of various neurologic diseases.
Very limited BAEP data are available in CCHS. When studying 4 young toddlers with CCHS (age 6 weeks to 15 months), the authors found abnormal wave III and subsequently suggested a disruption in the auditory pathways at the level of mid to upper brainstem, an area close to that of central respiratory control [20]. Another patient with CCHS has been reported as having numerous alterations in the electronystagmograph and auditory potentials [21]. The genetic status of these patients was unknown, as these observations were reported long before identification of PHOX2B mutations as responsible of CCHS [4].
In the present study, we measured BAEPs in a large group of patients with PHOX2B mutations positive CCHS. We aimed to assess the integrity of auditory pathways in CCHS and investigate the extent in which brainstem auditory pathways were affected in the disease.
Methods
Patients
Fifteen children and adolescents with CCHS (8 boys and 7 girls. mean age 6.3 yrs ± 5) underwent BAEP recordings. The latter were part of a multidisciplinary assessment performed in the CCHS patients followed-up in the French Center of reference for central hypoventilation (Robert Debré University Hospital. Paris. France). Table 1 shows the main clinical characteristics of the study group. All patients had alveolar hypoventilation while spontaneously breathing during overnight polysomnography, absent respiratory response to exogenous CO2 and presence of mutations in the PHOX2B gene, all of these being +5 to +7 alanine expansions. Diagnosis was made in the first days of life for all, except for two of them (N°10 and 15). None was born prematurely. Hirschsprung’s disease was associated in three patients (N°3, 7 and 9). The study was approved by the Robert Debré Hospital Ethics Committee. Parents received full information before giving a written consent to undergo the procedure and publish individual clinical data. Parents were present throughout the procedure.
Methods
Without any previous sedation, each patient underwent BAEPs using a Nicolet Spirit system. BAEPs were recorded by surface electrodes attached by tape to the scalp at the Cz area and at the ipsilateral earlobe after 2000 monaural stimulations of 70 dB intensity and with a controlateral “masking” of 40 dB intensity. If no response is obtained with 70 dB stimulation intensity, a new stimulation is done with 90 dB intensity. The objective auditory level of the V wave is systematically studied by progressively decrease of the stimulation intensity. Latencies and amplitudes of the I, II, III, IV and V waves were measured and the interpeaks latencies (IPL) of waves III-I. V-I and V-III were analyzed. Data from patients were compared to those obtained in our laboratory from 30 healthy control matched subjects in different age groups (0-2 months. 3-5 months. 6-18 months. 1.5-5 years. 6-10 years and young adults). Table 2 displays the upper values considered for defining abnormalities, expressed as mean + 2.5 SD for each age group.
Statistical analysis
Comparison of right and left BAEP data was done with the paired two-tailed Student’s t-test (SPSS version 19, IBM SPSS inc). Difference was considered significant for P values of 0.05 or less.
Results
Table 3 shows BAEP responses for the study group. Normal BAEP responses were observed in nine children (60%) and abnormal responses in the other six (40%). For three patients (N°6, 11 and 14), abnormalities consisted in significantly delayed responses of the auditory nerve (wave I) with normal inter-latencies IPL V-I and V-III in patients 6 and 11 but asymmetric responses in patient 14. These results were considered as peripheral auditory transmission dysfunction. For two other patients (N°3 and 4), latencies of the three first waves (I, II, III) were normal but significantly delayed latencies or lost responses of the fourth and fifth waves responses were observed with increased or incalculable IPL V-I and V-III. These results were considered as brainstem dysfunction. Finally, one patient (N°2) showed asymmetric and drastically altered responses with an unidentified bilateral wave II suggesting major peripheral auditory dysfunction and loss or prolonged latencies of IV and V waves with loss or increased interpeaks V-I and V-III suggesting brainstem dysfunction.
For the whole group, mean values of wave latencies and interpeaks latencies did not differ between right and left ears of the patients. BAEPs data were not correlated with presence of associated clinical conditions or with genetic status.
Discussion
Our study indicates abnormalities of the BAEPs in 40% of the patients with CCHS examined. However, abnormalities related to brainstem dysfunction were observed in 20% of them only. Significant alterations in the brainstem autonomic structures in CCHS have been described using fMRI studies [14-18]. The alterations are thought to be caused by maldevelopment or neural demyelization as a consequence of gene mutations. This likely accounted for the delayed BAEPs observed in some of our patients.
Several authors have reported that BAEP responses in neonates and preterm infants are affected by the maturity of the auditory system. However, the effect of maturity is more evident in premature infants; thus, the response pattern in these children may differ from those in term neonates [22-24]. In our group, we had no premature infant. We also compared patients’ data to those obtained from healthy control matched subjects corrected for age to determine abnormal BAEP. Nevertheless, alterations in BAEPs found in our CCHS patients were not correlated with age, i.e. patient 1 of 1 month of age had normal data, whereas patient 14, aged 13 years showed altered responses.
One new finding of the present study was dysfunction of peripheral auditory transmission in some patients without any auditory infection such as otitis or rhinopharyngitis. One may hypothesize a cochlear dysfunction secondary to a possible cochlear malformation.
More interestingly, the normal conduction in BAEPs found in the majority of our patients showed the complexity of the roles of the anatomic structures in this disease. In fMRI studies conducted in patients with CCHS, abnormalities appeared in brainstem areas involving the ventral midbrain, pons, and dorsal and ventral medulla. These areas are principally traversed by fibers of significance for breathing and autonomic control, but not by fibers for auditory control that are situated more laterally. The auditory fibers enter the brainstem at the lateral side of the pons lateral to the restiform body and immediately split up to enter the dorsal and ventral cochlear nuclei. The auditory pathways to the cortex are complex. The further cell stations are the superior olive, the nucleus of the lateral lemniscus, the inferior colliculus on the roof of the midbrain and the medial geniculate body. Between cochlear nuclei and medial geniculate body, there are at least two neurons. Many but not all fibers decussate. Of these decussations, the most ventral one at the level of the superior olive is the strongest, known as the trapezoid body. The pathway between superior olive and inferior colliculus is a compact bundle of fibers known as the lateral lemniscus. The distribution of the different waves recorded through auditory evoked potentials indicate wave I as the volley of eight nerve action potentials generated by the click stimulus in the segment of the nerve close to the cochlea. Waves II and III are assigned to the cochlear nucleus and superior olivary complex, respectively. Waves IV and V are considered generated in inferior colliculus or lateral lemniscus [19]. Therefore, we could suggest that BAEP abnormalities may be observed in patients with CCHS when damage or underdevelopment is more diffuse in brainstem areas.
Conclusions
Using BAEP studies, we found arguments for dysfunction of brainstem auditory pathways in a few patients with CCHS. In the others, BAEPs were normal. This finding likely suggests much more complex yet-to-be determined interactions between pathways and processes of central control of breathing and of control of hearing.
Abbreviations
- BAEP:
-
Brainstem auditory evoked potentials
- CCHS:
-
Congenital central hypoventilation syndrome
- fMRI:
-
Functional magnetic resonance imaging
References
Mellins RB, Balfour HH, Turino GM, et al. Failure of automatic control of ventilation (Ondine’s curse). Medicine. 1970;49:487–504.
Weese-Mayer DE, Berry-Kravis EM, Ceccherini I, Keens TG, Loghmanee DA, Trang H. An official ATS clinical policy statement: congenital central hypoventilation syndrome: genetic basis. Diagnosis. And management. Am J Respir Crit Care Med. 2010;181(6):626–44.
Trang H, Dehan M, Beaufils F, Zaccaria I, Amiel J, Gaultier C, et al. French CCHS working group. The French congenital central hypoventilation syndrome registry: general data, phenotype and genotype. Chest. 2005;127(1):72–9.
Amiel J, Laudier B, Attié-Bitach T, Trang H, et al. Polyalanine expansion and frameshift mutations of the paired-like homeobox gene PHOX2B in congenital central hypoventilation syndrome. Nat Genet. 2003;33(4):459–61.
Matera I, Bachetti T, Puppo F, et al. PHOX2B mutations and polyalanine expansions correlate with the severity of the respiratory phenotype and associated symptoms in both congenital and late onset Central Hypoventilation syndrome. J Med Genet. 2004;41(5):373–80.
Haddad GG, Mazza NM, DeFendini R, Blanc WA, Driscolli JM, Epstein MAF, et al. Congenital failure of automatic control of ventilation. gastrointestinal motility and heart rate. Medicine. 1978;57:517–26.
Spengler CM, Banzett RB, Systrom DM, Shannon DC, Shea S. Respiratory sensations during heavy exercise in subjects without respiratory chemosensitivity. Respir Physiol. 1998;114:65–74.
Shea SA, Shea J. Symptoms of inadequate ventilation in congenital central hypoventilation syndrome. Am J Respir Crit Care Med. 1999;159:781.
Woo MS, Woo MA, Gozal D, Jansen MT, Keens TG, Harper RM. Heart rate variability in congenital central hypoventilation syndrome. Pediatr Res. 1992;31:291–6.
Trang H, Girard A, Laude D, Elghozi JL. Short-term blood pressure and heart rate variability in congenital central hypoventilation syndrome (Ondine’s curse). Clin Sci (Lond). 2005;108(3):225–30.
Macey PM, Valderama C, Kim AH, et al. Temporal trends of cardiac and respiratory responses to ventilatory challenges in congenital central hypoventilation syndrome. Pediatr Res. 2004;55(6):953–9.
Faure C, Viarme F, Cargill G, Navarro J, Gaultier C, Trang H. Abnormal esophageal motility in children with congenital central hypoventilation syndrome. Gastroenterology. 2002;122:1258–63.
Goldberg DS, Ludwig IH. Congenital central hypoventilation syndrome: ocular finds in 37 children. J Pediatr Ophtalmol Strabismus. 1996;33:176–81.
Macey PM, Woo MA, Macey KE, Keens TG, Saeed MM, Alger JR, et al. Hypoxia reveals posterior thalamic, cerebellar, midbrain, and limbic deficits in congenital central hypoventilation syndrome. J Appl Physiol. 2004;98:958–69.
Kumar R, Macey PM, Woo MA, Alger JR, Keens TG, Harper RM. Neuroanatomic deficits in congenital central hypoventilation syndrome. J Comp Neurol. 2005;487:361–71.
Macey PM, Richard CA, Kumar R, et al. Hippocampal volume reduction in congenital central hypoventilation syndrome. PLoS One. 2009;4(7):e6436.
Kumar R, Macey PM, Woo MA, Harper RM. Selectively diminished corpus callosum fibers in congenital central hypoventilation syndrome. Neuroscience. 2011;178:261–9.
Kumar R, Woo MS, Macey PM, Woo MA, Harper RM. Progressive gray matter changes in patients with congenital central hypoventilation syndrome. Pediatr Res. 2012;71(6):701–6.
Chiappa KH. Evoked potentials in clinical medicine. New York: Raven press; 1990.
Beckerman R, Meltzer J, Sola A, Dunn D, Wegmann M. Brain-stem auditory response in Ondine’s syndrome. Arch Neurol. 1986;43(7):698–701.
Gallina S, Restivo S, Cupido G, Speciale R, Giammanco AM, Cimico G. Otoneurological findings in a case of congenital central hypoventilation syndrome (Ondine’s curse). Acta Otorhinolaryngol Ital. 2000;20(2):121–4.
Sleifer P, Costa SS, Cóser PL, Goldani MZ, Dornelles C, Weiss K. Auditory brainstem response in premature and full-term children. Int J Pediatr Otorhinolaryngol. 2007;71(9):1449–56.
Gorga M, Kaminski J, Beauchaine K, Jesteadt W, Neely S. Auditory brainstem responses from children three months to three years of age: normal patterns of response II. J Speech Hear Res. 1989;32(2):281–8.
Starr A, Amlie RN, Martin WH, Sanders S. Development of auditory function in newborn infants revealed by auditory brainstem potentials. Pediatrics. 1977;60:831–9.
Acknowledgements
The authors deeply thank all the patients with CCHS and theirs families, and the Association Française du syndrome d’Ondine for their support.
Funded by the French Center of reference for central hypoventilation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
TMZ performed all BAEP measurements, analyzed and interpreted the data. FH analyzed and interpreted the data, and drafted the manuscript. HT designed and coordinated the study, interpreted the data, performed statistical analysis, and revised the manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Trang, H., Masri Zada, T. & Heraut, F. Abnormal auditory pathways in PHOX2B mutation positive congenital central hypoventilation syndrome. BMC Neurol 15, 41 (2015). https://doi.org/10.1186/s12883-015-0299-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-015-0299-z