Abstract
Purpose
This study aimed to identify the factors related to treatment adherence behaviors among old-age hemodialysis patients in Hamadan based on the Extended Theory of Planned Behavior (ETPB) during the covid-19 pandemic.
Methods
This cross-sectional study was conducted from January to March 2021 in Hamadan, Iran. 191 hemodialysis patients were recruited who were referred to hemodialysis centers via the census method. Data were collected by a questionnaire containing items on socio-demographic information, End-Stage Renal Disease Adherence (ESRD-Adherence) Questionnaire, and ETPB constructs scale. Data analysis was performed using descriptive statistics and structural equation modeling.
Results
The mean (SD) age of participants was 62.49 (10.66). Also, the mean (SD) hemodialysis vintage/Month of them was 36.56 (43.34). Moreover, Treatment Adherence Behaviors are associated with education level, sex, and marital status (p < 0.001). Besides, Perceive Behavior Control (β = 0.414, t-value = 3.810) associated with intention. Also, intention (β = 0.158, t-value = 1.976) was associated to adherence behaviors. No significant associations were observed between positive attitudes, subjective norms, a perceived threat with intention, and adherence behaviors. The model explained about 54% of the variance of adherence behaviors. Finally, the goodness of fit index of 0.78, indicating the model good fit.
Conclusion
The present study demonstrates that some of the ETPB constructs such as perceived behavior control and intention are useful to improve adherence among the oldest hemodialysis patients. Also. This framework is revealed alongside the theory of planned behavior (TPB) applicable in the treatment adherence of old-age hemodialysis patients.
Similar content being viewed by others
Introduction
Chronic kidney failure is one of the most common non-communicable diseases that occurs during the progressive process of decreased nephron function. The end stage of the disease (end-stage renal disease) leads to disability in the patient [1].
According to the World Health Organization, treatment adherence is the correspondence level of a person receiving medication, following a prescriptive diet, or implementing lifestyle changes due to healthcare providers’ recommendations [2]. Adherence to hemodialysis (HD) for patients with end-stage renal disease is essential and leads to lifestyle changes such as the need to regularly go to a dialysis center, consistently take prescribed medications, and extensively modify their diets [3]. Also, successful treatment of HD patients depends on maximum patient adherence to treatment. Evidence demonstrated that four behaviors could result in the decreased quality of life, increased morbidity, healthcare costs, and mortality in these patients [4]. However, management of renal replacement therapy includes behaviors such as HD attendance, medications, fluid restrictions, and diet prescription [4, 5]. The result of the study indicated that HD patients needed complex care to manage this chronic disease [6]. In contrast, a study matched with the Iranian context showed that it was essential to identify factors effective for treatment adherence in HD patients [7].
The treatment adherence concept
Treatment adherence plays a critical role in decreasing the economic burden of disease for families and society [8, 9]. Patient non-adherence in the literature can be considered a patient’s “incomplete implementation of instructions” issued by a provider [8, 10]. The results of studies proved average patient non-adherence rates of 24.8% across physician-recommended treatments types, with some non-adherence rates approaching 40% [8, 11, 12]. The type of treatment implemented significantly impacts treatment adherence and non-adherence, with treatment regimens such as lifestyle or behavior changes presenting rates of non-adherence of up to 70% [8, 13].
The conceptual framework
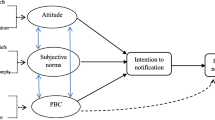
The model-based approach assists in promoting or changing behavior by understanding adherence to health behavior. This approach includes the Health Belief Model, Theory of Planned Behavior (TPB), Theory of Reasoned Action, and other theories or models [14]. TPB is a social-cognitive approach that provides a useful framework for predicting and understanding health-related behaviors [15, 16]. According to this theory, intention is the primary determinant of behavior. The individual’s intention is influenced by the three factors of attitude, subjective norms, and perceived behavioral control (PBC) [17, 18]. Evidence demonstrated several important factors that could predict and affect adherence behavior in patients, such as attitude, subjective norms, PBC, and intention [19, 20]. On the other hand, a perceived threat to treatment adherence can play a decisive role in adherence behaviors in HD patients [21].
Therefore, the Extended Theory of Planned Behavior (ETPB) was used in this study to identify factors affecting treatment adherence behaviors. In this framework, perceived threat includes perceived susceptibility, and perceived severity is added to TPB (Fig. 1).
Also, since December 2019, coronavirus (COVID-19) has become a global pandemic, and results of clinical studies showed that the risk of COVID-19 infection hospitalized was more than 10% in dialysis patients and 6.4% in in-hospital medical staff [22]. Additionally, concerns increased about non-adherence behaviors in HD patients, especially in the COVID-19 pandemic [23, 24]. Thus, the present study aimed to identify factors related to treatment adherence behaviors among older HD patients in Hamadan, Iran, based on ETPB.
Methods
Design and participants
This cross-sectional study was conducted from January to March 2021 in Hamadan, Iran. Hamadan Province, with an area of 19,493 square kilometers in extent, is located in western Iran. We used patients’ information from two hospitals with dialysis wards, including Besat and Shahid-Beheshti in Hamadan city. A total of 191 HD patients were recruited and referred to HD centers via the census method. Participants were selected based on the following inclusion criteria: being diagnosed with end-stage renal disease and treated with HD for at least three months; receiving HD for three to four hours per session, three times per week; ability to complete the survey and willingness to participate in the study; and ability to give informed consent. Patients on transient HD due to acute renal failure were excluded.
Data collection
All methods were performed following relevant guidelines and regulations. Verbal informed consent was obtained from all the patients; they were informed about the confidentiality of the information and the project’s purpose, and they were enrolled in the study if they liked. The Ethics Committee approved the study with the consent process at the Hamadan University of Medical Sciences.
Measurements
The data collection tool used in the study consisted of three parts completed by the participants through the self-reporting method. The first part included demographic information such as age, education level, economic status, marital status, number of families, and COVID-19 morbidity in the participants or their families.
The second section included the 46-item ESRD-Adherence Questionnaire (ESRD-AQ) designed by Kim et al. [4] that assesses four behaviors: HD attendance, medications, fluid restrictions, and diet prescription.
The ETPB constructs were assessed using the ETPB scale for treatment adherence behavior designed and regulated by the researcher through the study of books, papers, and literature [25, 26]. It was compiled of 43 items and nine subscales as follows: behavior beliefs (seven items, e.g., “Attending HD sessions makes me feel happy, relaxed and at peace”), outcome evaluation (seven items, e.g., “I need to take prescription drugs on time and correctly.”), normative beliefs (four items, e.g., “My children or my family thinks that I should take my medication on time and correctly.”), motivation to comply (four items, e.g., “For me, the opinion of my children and family that I should take my medication on time and correctly is important.”), control beliefs (six items, e.g., “I regularly attend recommended dialysis sessions, even if the HD session is long.”), perceive power (five items, e.g., “I do not attend an HD session because of travel problems.”), perceive susceptibility (three items, e.g.,“ Compared to other people my age, I am more likely to have coronavirus.”), perceive severity (six items, e.g., “If I get Covid-19, my life will be shortened..”), intention (three items, e.g., “I plan to attend regular HD sessions.”), and the treatment adherence behaviors (46 items, e.g., “During the last month, how many dialysis treatments did you miss completely?”). These items were assessed using a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree). The score of each subscale was obtained by the average computed as the sum of items of it [4]. It is essential to mention that based on a previous study [4], the patients were categorized in two levels, “adherence” and “non-adherence,” based on biological and biochemical markers of clinical outcomes such as degree of weight gain (increase in weight in kg after a weekend), serum potassium levels (average of last three measures) in meq/l, serum phosphate levels (average of last three measures) in mg/dl, and serum albumin (average of last three measures) in mg/dl [27,28,29].
The content validity ratio (CVR) and the content validity index (CVI) were used to determine content validity. The results showed high overall CVI and CVR of the ETPB scale. The means scores for CVI and CVR were 0.92 and 0.80, respectively. The CFA results confirmed goodness of fit the ETPB sub-constructs. The discriminant validity was verified using the Fornel-Larcker and Average Variance Extracted (AVE) methods. The composite reliability (CR) range and Cronbach’s alpha range [30]. The composite reliability ranged from 0.86 to 0.98, and Cronbach’s alpha ranged from 0.76 to 0.98.
Results
Sample characteristics
In this present study, with 191 participants, 47.8% were female (n = 93) and, with a mean age of participants was 62.49 ± 10.66. Also, the mean HD vintage (Month) of them was 36.56 ± 43.34.
According to the findings, Treatment Adherence Behaviors associated with education level, sex, and marital status as treatment adherence behaviors in a patient with secondary education level with OR = 0.17 (95% CI 0.04, 0.75) and, in female patients with OR = 0.29 (95% CI 0.09, 0.94) (p < 0.05), while, in married patients with OR = 7.70 (95% CI 1.89, 31.44) (p < 0.001) were calculated. Other demographic data were presented in Table 1.
The ETPB constructs about treatment adherence behaviors
Table 2 shows the means and standard deviations of the ETPB constructs. Participants rated perceived behavioral (PBC) (84%), perceived threat (84%), Intention (79%), positive attitude (75%), subjective norms (70%), which were the highest percentage of the mean from the maximum obtainable score. The mean of constructs showed that all constructs were considered desirable (Table 2).
Associations between the ETPB constructs
Although, based on results there was a positive direct positive association between intention with attitude (p = 0.05), PBC, perceived threat (p < 0.01). While there was a positive direct positive correlation between treatment adherence behaviors with attitude, PBC, intention (p < 0.01).
However, perceive a threat (r = 0.33) and perceive behavior control (r = 0.27) were more correlated with intention among other extended theories of planned behavior constructs.
Though, intention (r = 0.33) and PBC (r = 0.38) were more correlated with treatment adherence behaviors among other ETPB constructs (Table 2).
The structural modeling analysis
Table 3, Fig. 2 presented the results of analyzing, the model 54% of the variance of adherence behaviors as the dependent variable (R square = 0.536). The R square for intention is 0.286 that suggests 29% of the variance of intention can be explained by PBC.
The PBC (β = 0.414, t-value = 3.810) associated with intention. Also, intention (β = 0.158, t-value = 1.976) was associated to adherence behaviors. No significant associations were observed between positive attitudes, subjective norms, perceived threat with Intention, and adherence behaviors (Table 3).
The model’s predictive power was tested by calculating Q2 indexes of intension (Q2 = 0.672) and adherence behaviors (Q2 = 0.557), exceeding the recommended threshold value (Q2 > 0), demonstrating an adequate predictive value of the model. Finally, GoF = 0.78, indicating the model good fit (Table 4).
Discussion
The current study utilized the ETPB framework to identify factors affecting treatment adherence behaviors among HD patients. It was shown that TPB could predict and improve adherence behaviors of chronic kidney disease patients, which is in line with Chironda et al.’s results [14].
According to the findings, treatment adherence behaviors are associated with the education level. Recently, similar to our results, Kim has reported that with increasing the education level, treatment adherence behaviors are improved [31]. We can mention that patient noncompliance is attributed to personal qualities of patients, such as forgetfulness, lack of willpower or discipline, or low level of education [32]. Although, patients need to clearly and appropriately understand health information related to their specific illness or disease [33, 34]. This understanding may be essential to helping patients generate beliefs and attitudes and improve adherence behaviors [34]. Thus, when patients are adequately informed and understand clearly what they are asked to do, they are better able to share in decisions that affect their health and are thus more adherent to treatments [33, 35]. On the other hand, it seems that mastery experiences and social roles in high educational individuals caused to increase self-efficacy and PBC, which other results of several studies proved to have higher PBC lead to the formation of a behavioral intention, and performance of behavior [16, 18, 36, 37]. Therefore, it is recommended to design and plan educational interventions to improve PBC and intention for all HD patients, especially low-educated individuals.
Based on the present study, treatment adherence behaviors associated with sex were better in females than in males. Consequently, gender should also affect treatment adherence behaviors [38]. However, a relationship between gender and adherence has not been consistently shown in the literature. Several studies have found women to be more non-adherent than men [39,40,41]. Others have reported that women tend to follow their prescriptions better than men [42, 43]. Nevertheless another study mentioned no difference between male and female regarding drug adherence [44]. These conflicting results may be due to different conditions and treatments compared to the present study. Thus, it is recommended to plan educational intervention to improve treatment adherence behaviors for all HD patients.
Based on findings, treatment adherence behaviors are associated with marital status. In line with this result, Turan et al.’s study showed that social supports affected patients’ adherence to the treatment [45]. Generally, evidence was emphasized that family members or peer supports may promote better adherence in some patient groups [46]. So, it is recommended to plan educational intervention to improve treatment adherence behaviors for singles, widows or widowers, the divorced, or partners death HD patients.
Although all ETPB constructs were considered desirable. In line with this finding, Beerappa et al. reported a fair to good adherence level for fluid and dietary restrictions in patients [47].
Based on results, PBC is associated with intention and among the constructs of ETPB, PBC plays a significant role in explaining the variance of the intention of treatment adherence behaviors among HD patients, which is similar to Biddle’s study, showing that having higher PBC was a predictor of improved self‐care [39]. Based on TBP, PBC over behavior performance can explain great variance in intentions and actions [48].
This study found that intention was associated with adherence behaviors, as mentioned in previous studies (Husebø et al.) which [49] intention to engage in the health‐changing behavior and PBC demonstrated significant association with adherence behaviors. Moreover, Finchman et al. revealed possible decreased medical complications and mortality due to PBC and intention to improve adherence to the dietary and fluid restrictions among HD patients [50].
This study has several limitations. First, this was a cross-sectional study that enrolled a small number of patients. Thus, it is recommended to identify additional factors in future research. Second, future research should analyze data from a larger sample of participants. In contrast, the potential for recall and interviewer biases may be included, and a longitudinal study design could be useful for managing bias. The findings of this study might not be generalized to all populations of older people. Therefore, future research can investigate predictors of treatment adherence behaviors from a more ecological approach by examining TPB constructs complemented by wider levels of individual and social factors.
Conclusion
The present study demonstrated that some of the ETPB constructs, such as PBC and intention, were useful to improve adherence among older HD patients. Also. the framework revealed alongside TPB is applicable in the treatment adherence of older HD patients. Thus, future studies are suggested to pay more attention to increasing PBC and intention in designing and implementing educational programs. Interventions can also heighten perceived behavioral control to increase treatment adherence behaviors among HD patients.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ETPB:
-
The Extended Theory of Planned Behavior
- TPB:
-
The theory of planned behavior
- HD:
-
Hemodialysis
- CVR:
-
Content validity ratio
- CVI:
-
Content validity index
- PBC:
-
Perceived behavioral control
References
Centers for Disease Control and Prevention (CDC). Chronic Kidney Disease Basics: CDC. 2020. https://www.cdc.gov/kidneydisease/basics.html. Accessed 20 Apr 2021.
E. S. World Health Organization. Adherence to long-term therapies: evidence for action. 2003. http://apps.who.int/iris/bitstream/handle/10665/42682/9241545992.pdf;jsessionid=69DD547138169C24724B8622BF4276BD?sequence=1. Accessed 20 Apr 2021.
Dodd R, Palagyi A, Guild L, Jha V, Jan S. The impact of out-of-pocket costs on treatment commencement and adherence in chronic kidney disease: a systematic review. Health Policy Plan. 2018;33(9):1047–54.
Kim Y, Evangelista LS, Phillips LR, Pavlish C, Kopple JD. The End-Stage Renal Disease Adherence Questionnaire (ESRD-AQ): testing the psychometric properties in patients receiving in-center hemodialysis. Nephrol Nurs J. 2010;37(4):377.
Geldine CG, Bhengu B, Manwere A. Adherence of adult chronic kidney disease patients with regard to their dialysis, medication, dietary and fluid restriction. Res J Health Sci. 2017;5(1):3–17.
Graham J. Nursing theory and clinical practice: how three nursing models can be incorporated into the care of patients with end stage kidney disease. CANNT J. 2006;16(4):28–31 Journal ACITN.
Rahimi F, Gharib A, Beyramijam M, Naseri O. Effect of self-care education on self efficacy in patients undergoing hemodialysis. Life Sci J. 2014;11(1 SPEC):136–40.
Hock R, Kinsman A, Ortaglia A. Examining treatment adherence among parents of children with autism spectrum disorder. Disabil Health J. 2015;8(3):407–13.
DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42(3):200–9.
Blackwell B. Treatment adherence. Br J Psychiatry. 1976;129(6):513–31.
DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23(2):207.
DiMatteo MR, DiNicola DD. Achieving Patient Compliance: The Psychology of the Medical Practitioner’s Role. New York: Pergamon Press; 1982.
Chesney MA. Factors affecting adherence to antiretroviral therapy. Clin Infect Dis. 2000;30(Supplement_2):S171–6.
Chironda G, Bhengu B, Manwere A. Models and theories of care applicable to predicting and improving adherence behaviours among Chronic Kidney Disease (CKD) patients. Rwanda J Med Health Sci. 2019;2(1):48–58.
Sharma M, Romas JA. Theoretical foundations of health education and health promotion. Sudbury: Jones & Bartlett Publishers; 2008.
Khani Jeihooni A, Jormand H, Harsini PA. The effect of educational program based on beliefs, subjective norms and perceived behavior control on doing pap-smear test in sample of Iranian women. BMC Womens Health. 2021;21(1):1–10.
Ajzen I. The theory of planned behaviour: reactions and reflections. Taylor & Francis. 2011;26(9):1113–27.
Karimi M, Jormand H, Zangeneh M. Factors related with tobacco smoking among college students: the application of the extended theory of planned behavior. J Educ Community Health. 2020;7(2):81–7.
Dilekler İ, Doğulu C, Bozo Ö. A test of theory of planned behavior in type II diabetes adherence: the leading role of perceived behavioral control. Curr Psychol. 2021;40(7):3546–55.
Rich A, Brandes K, Mullan B, Hagger MS. Theory of planned behavior and adherence in chronic illness: a meta-analysis. J Behav Med. 2015;38(4):673–88.
Ramezani T, Sharifirad G, Rajati F, Rajati M, Mohebi S. Effect of educational intervention on promoting self-care in hemodialysis patients: applying the self-efficacy theory. J Educ Health Promot. 2019;8:65.
Li J, Xu G. Lessons from the experience in Wuhan to reduce risk of COVID-19 infection in patients undergoing long-term hemodialysis. Clin J Am Soc Nephrol. 2020;15(5):717–9.
Atighechian G, Tavakoli N, Rezaei F. The information needs of the Iranian people in the COVID-19 pandemic from the perspective of health professionals: a qualitative approach. J Educ Community Health. 2021;8(3):195–202.
Jormand H, Bashirian S, Barati M, Khazaei S, Jenabi E, Zareian S. A qualitative study on people’s experiences of Covid-19 media literacy. Med Lit Acad Res. 2021;4(1):38–52.
Dormanesh B, Daryabeigi R, Hadi S, Sepahvand V, Sarkhosh TA. Application of the theory of planned behavior in dietary and physical activity behaviors among hemodialysis patients visiting army hospitals. Pajouhan Sci J. 2018;16(2):19–27.
Pakpour AH, Zeidi IM, Chatzisarantis N, Molsted S, Harrison AP, Plotnikoff RC. Effects of action planning and coping planning within the theory of planned behaviour: a physical activity study of patients undergoing haemodialysis. Psychol Sport Exerc. 2011;12(6):609–14.
Hecking E, Bragg-Gresham JL, Rayner HC, Pisoni RL, Andreucci VE, Combe C, et al. Haemodialysis prescription, adherence and nutritional indicators in five European countries: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant. 2004;19(1):100–7.
Durose CL, Holdsworth M, Watson V, Przygrodzka F. Knowledge of dietary restrictions and the medical consequences of noncompliance by patients on hemodialysis are not predictive of dietary compliance. J Am Diet Assoc. 2004;104(1):35–41.
Kutner NG, Zhang R, McClellan WM, Cole SA. Psychosocial predictors of non-compliance in haemodialysis and peritoneal dialysis patients. Nephrol Dial Transplant. 2002;17(1):93–9.
Hair Jr JF, Sarstedt M, Ringle CM, Gudergan SP. Advanced issues in partial least squares structural equation modeling (3rd ed.). SAGE Publications Inc; 2017.
Kim B, Kim J. Influence of uncertainty, depression, and social support on self-care compliance in hemodialysis patients. Ther Clin Risk Manag. 2019;15:1243–51.
Delamater AM. Improving patient adherence. Clin Diabetes. 2006;24(2):71–7.
Miller TA. Health literacy and adherence to medical treatment in chronic and acute illness: a meta-analysis. Patient Educ Couns. 2016;99(7):1079–86.
Martin LR, Haskard-Zolnierek KB, DiMatteo MR. Health Behavior Change and Treatment Adherence: Evidence-Based Guidelines for Improving Healthcare. New York: Oxford University Press; 2010.
DiMatteo MR, Haskard-Zolnierek KB, Martin LR. Improving patient adherence: a three-factor model to guide practice. Health Psychol Rev. 2012;6(1):74–91.
Ajzen I. Constructing a TPB questionnaire: Conceptual and methodological considerations. 2002. http://www.people.umass.edu/aizen/pdf/tpb.measurement.pdf. Accessed 18 Apr 2021.
Khazaei S, Bashirian S, Jenabi E, Barati M, Karimi-Shahanjarini A, Moeini B, et al. COVID-19 preventive behaviors and its related beliefs among health workers: the role of threat and coping appraisals. J Educ Community Health. 2020;7(3):221–7.
Thunander Sundbom L, Bingefors K. Women and men report different behaviours in, and reasons for medication non-adherence: a nationwide Swedish survey. Pharm Pract (Granada). 2012;10(4):207–21.
Biddle MJ, Moser DK, Pelter MM, Robinson S, Dracup K. Predictors of adherence to self-care in rural patients with heart failure. J Rural Health. 2020;36(1):120–9.
Puskas CM, Forrest JI, Parashar S, Salters KA, Cescon AM, Kaida A, et al. Women and vulnerability to HAART non-adherence: a literature review of treatment adherence by gender from 2000 to 2011. Curr HIV/AIDS Rep. 2011;8(4):277–87.
Chan DC, Shrank WH, Cutler D, Jan S, Fischer MA, Liu J, et al. Patient, physician, and payment predictors of statin adherence. Med Care. 2010;48(3):196–202.
Hawthorne A, Rubin G, Ghosh S. Medication non-adherence in ulcerative colitis–strategies to improve adherence with mesalazine and other maintenance therapies. Aliment Pharmacol Ther. 2008;27(12):1157–66.
Barati M, Akbari-Heidari H, Samadi-Yaghin E, Jenabi E, Jormand H, Kamyari N. The factors associated with the quality of life among postmenopausal women. BMC Womens Health. 2021;21(1):1–8.
Goudarzi H, Barati M, Bashirian S, Moeini B. Determinants of medication adherence among hypertensive patients using the Pender’s health promotion model. J Educ Health Promot. 2020;9:89.
Turan GB, Aksoy M, Çiftçi B. Effect of social support on the treatment adherence of hypertension patients. J Vasc Nurs. 2019;37(1):46–51.
Shahin W, Kennedy GA, Stupans I. The association between social support and medication adherence in patients with hypertension: a systematic review. Pharm Pract (Granada). 2021;19(2):2300.
Beerappa H, Chandrababu R. Adherence to dietary and fluid restrictions among patients undergoing hemodialysis: an observational study. Clin Epidemiol Glob Health. 2019;7(1):127–30.
Ajzen I. Perceived behavioral control, self-efficacy, locus of control, and the theory of planned behavior 1. J Appl Soc Psychol. 2002;32(4):665–83.
Husebø AML, Dyrstad SM, Søreide JA, Bru E. Predicting exercise adherence in cancer patients and survivors: a systematic review and meta-analysis of motivational and behavioural factors. J Clin Nurs. 2013;22(1–2):4–21.
Fincham D, Kagee A, Moosa R. Dietary and fluid adherence among haemodialysis patients attending public sector hospitals in the Western Cape. South Afr J Clin Nutr. 2008;21(2):7–12.
Acknowledgements
The authors would like to acknowledge the staff of HD centers and hospitals of Hamadan city, and the patients with CKD were participating in this work.
Funding
The Research Ethics Committee approved this study of Hamadan University of Medical Sciences with a specific ID IR.UMSHA.REC.1399.565 & was funded by the Hamadan University of Medical Sciences (No, 997295318) that participated in financial support of this study. This funding source had no role in the analysis and interpretation of data; in the writing of the article; nor in the decision to submit it for publication.
Author information
Authors and Affiliations
Contributions
VSH conceived the study, obtained funding, and supervised data collection; VSH & HJ was responsible for data collection. HJ prepared questioner; MB, SKH undertook other data analyses; VH & HJ drafted the manuscript; all authors contributed to the manuscript review and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were performed in accordance with relevant guidelines and regulations. Verbal informed consent was obtained from all participants; all participants were informed about the confidentiality of the information and the project’s purpose, and only if they would like, they were enrolled in the study. The Ethics Committee approved this study with all consent process at Hamadan University of Medical Sciences (No: ID IR.UMSHA.REC.1399.565).
Consent for publication
Not applicable
Competing of interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sheikh, V., Barati, M., Khazaei, S. et al. Factors related to treatment adherence behaviors among old-age hemodialysis patients in Hamadan, Iran: the application of the extended theory of planned behavior during Covid-19 pandemic. BMC Nephrol 23, 58 (2022). https://doi.org/10.1186/s12882-022-02694-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-022-02694-x