Abstract
Background
Head and neck squamous cell carcinoma (HNSCC) represents the 6th leading cancer worldwide. In most cases, patients present a locally advanced disease at diagnosis and non-surgical curative treatment is considered the standard of care. Nowadays, [18F]FDG PET/CT is a validated tool in post-treatment evaluation, with a high level of evidence. However, to standardize imaging response, several visual scales have been proposed with none of them approved yet. The study’s aim is a head-to-head comparison between the diagnostic performance of the Hopkins criteria, the Deauville score, and the new proposed Cuneo score, to establish their prognostic role. Secondly, we investigate the possible value of semiquantitative analysis, evaluating SUVmax and ΔSUVmax of the lymph node with the highest uptake on the restaging PET scan. Moreover, we also considered morphological features using the product of diameters measured on the co-registered CT images to assess the added value of hybrid imaging.
Methods
We performed a retrospective analysis on histologically proven HNSCC patients who underwent baseline and response assessment [18F]FDG PET/CT. Post-treatment scans were reviewed according to Hopkins, Deauville, and Cuneo criteria, assigning a score to the primary tumor site and lymph nodes. A per-patient final score for each scale was chosen, corresponding to the highest score between the two sites. Diagnostic performance was then calculated for each score considering any evidence of locoregional progression in the first 3 months as the gold standard. Survival analysis was performed using the Kaplan–Meier method. SUVmax and its delta, as well as the product of diameters of the lymph node with the highest uptake at post-treatment scan, if present, were calculated.
Results
A total of 43 patients were finally included in the study. Sensitivity, specificity, PPV, NPV, and accuracy were 87%, 86%, 76%, 92%, and 86% for the Hopkins score, whereas 93%, 79%, 70%, 96%, and 84% for the Deauville score, respectively. Conversely, the Cuneo score reached the highest specificity and PPV (93% and 78%, respectively) but the lowest sensitivity (47%), NPV (76%), and accuracy (77%). Each scale significantly correlated with PFS and OS. The ROC analysis of the combination of SUVmax and the product of diameters of the highest lymph node on the restaging PET scan reached an AUC of 0.822. The multivariate analysis revealed the Cuneo criteria and the product of diameters as prognostic factors for PFS.
Conclusions
Each visual score statistically correlated with prognosis thus demonstrating the reliability of point-scale criteria in HNSCC. The novel Cuneo score showed the highest specificity, but the lowest sensibility compared to Hopkins and Deauville criteria. Furthermore, the combination of PET data with morphological features could support the evaluation of equivocal cases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Head and Neck Squamous Cell Carcinoma (HNSCC) represents the 6th leading cancer worldwide [1]. After the primary treatment, the recurrence rate within 2 years accounts for approximately 60% of patients, with 20–30% experiencing distant metastases, underlining the need for reliable post-treatment evaluation and proper follow-up [2].
In most cases, patients present a locally advanced disease at diagnosis (stage III or IV) with nodal involvement. In this setting, the combined chemo-radiotherapy (CRT) approach or, less frequently, radiotherapy alone (RT) with curative intent is considered the standard of care. After the end of therapy, a clinical assessment is needed to guide the following decision-making [3].
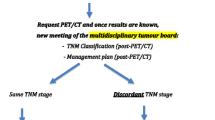
It is well known that treatment-related changes, particularly edema and fibrosis after high radiation dose, could often limit morphological imaging in post-treatment evaluation [4,5,6]. Nowadays, fluorine-18 fluorodeoxyglucose positron emission tomography/computed tomography ([18F]FDG PET/CT) is a validated tool in post-treatment HNSCC evaluation, with a high level of evidence. The most recent guidelines recommend the use of [18F]FDG PET/CT preferably 12 weeks after the end of treatment, pointing out a PET-guided approach. In case of a negative PET exam, the patient is followed-up with clinical observation; in doubtful cases, the patient can be subjected to clinical observation or can repeat the [18F]FDG PET/CT in 3–6 months. Finally, a clear PET positivity requests biopsy, primary surgery, or lymphadenectomy after CT or MRI confirmation [3].
In 2016, the PET-NECK, randomized, controlled trial data demonstrated that [18F]FDG PET/CT is an accurate and cost-effective technique for HNSCC response assessment, sparing unnecessary neck dissection in nearly 80% of patients [7]. Notably, the metabolic assessment showed a high negative predictive value (NPV) assessing its essential role in HNSCC surveillance [8, 9].
Over the last few years, the need to clarify the diagnostic value of [18F]FDG PET/CT even in doubtful and positive cases has promptly emerged. In order to better distinguish the disease from treatment-related changes, some authors have evaluated the prognostic role of several semiquantitative parameters, such as maximum standardized uptake value (SUVmax), but failed to find out a reliable method [4, 10, 11].
Therefore, there has been growing interest in optimizing the qualitative analysis by proposing different visual scales to standardize the metabolic imaging response. The first scoring system, named the Hopkins Criteria (HC), was introduced by Marcus and colleagues in a retrospective study considering a cohort of 214 patients. The 5-point scale achieved an NPV and overall diagnostic accuracy of 91.1% and 86.9%, respectively. These results were confirmed by the prospective multicenter ECLYPS study, where the use of HC resulted in a NPV of 92.1% [12, 13]. However, considering the studies’ bias as well as the low positive predictive value (PPV), other PET qualitative scores have recently been proposed: the well-known Deauville score (DS) and the novel Cuneo score (CS). In particular, CS, a 6-point visual scale, was introduced to minimize false-negative and false-positive results, resulting in a higher PPV to better discriminate persistent disease from treatment-related changes (e.g. inflammatory reactions after RT) [14]. In addition, each scale takes into account different visual reference regions (e.g. internal jugular vein (IJV); mediastinal blood pool (MBP); liver); only the CS introduces the absence/presence of the local background in PET images evaluation to highlight the possible interference of the post-treatment reaction of local tissue that impacts on visual score interpretation.
The first goal of this study was a head-to-head comparison between the diagnostic performance of the Hopkins criteria, Deauville score, and Cuneo score, together with the assessment of their prognostic role.
Secondly, we extracted SUVmax and ΔSUVmax of the lymph node with the highest uptake and we calculated the product of diameters measured on the co-registered CT images on the restaging PET/CT scan to investigate the possible added value of semiquantitative analysis and morphological data as a useful variable to consider in doubtful cases.
Methods
Patients’ selection
Data about patients with histologically proven non-metastatic locally advanced HNSCC, who were referred to our institution between February 2011 and January 2021, were retrospectively reviewed. All patients eligible for non-surgical curative-intent treatment (radiotherapy alone or chemoradiotherapy), who underwent both baseline and response assessment [18F]FDG PET/CT were included for analysis. Exclusion criteria included: previous resection of primary or nodal disease; prior radiotherapy to the head and neck district; other primary cancers. Response assessment PET/CT was performed at least 12 weeks after the end of treatment. All demographics, baseline characteristics, staging, treatment, and outcome details were recorded. Human papillomavirus (HPV) status was also collected, if available.
[18F]FDG PET/CT examination and analysis
All PET/CT scans included in the study were performed according to our institute’s clinical scanning protocols. Acquisitions were performed using a Discovery 710 PET/CT scanner (GE, General Electrics, Milwaukee, WI, USA). The field of view and pixel size of the PET images reconstructed for fusion was 70 cm and 2.73 mm respectively, with a matrix size of 256 × 256. The technical parameters used for CT imaging were: pitch 0.98, gantry rotation speed of 0.5 s/rot, 120 kVp, and modulated tube current of 140 mA. After 6 h of fasting, patients received an intravenous injection of 3 MBq/kg [18F]FDG. About 60 min after radiopharmaceutical administration, images were obtained from the skull base to the midthigh. Multimodal image analysis was carried out using a dedicated console (AW Server 4.7, General Electrics, Milwaukee, WI, USA).
Post-treatment scans were reviewed according to Hopkins, Deauville, and Cuneo criteria (Table 1) by two expert nuclear medicine physicians (C.F. and A.R.P.). Observers had access to pre-treatment disease stage and pre-treatment imaging but were blind to patient outcomes and the other reviewer's assignment. A visual score was assigned both to the primary tumor site and lymph nodes. Then, a per-patient final score for each scale was chosen, corresponding to the highest score between the two sites.
As usual, scores of 1–3 for Hopkins and Deauville scores and 1–4 for the Cuneo criteria were considered a metabolic response. Further analysis was performed considering the intermedium score 3 for Hopkins and Deauville and score 4 for Cuneo criteria as no response.
To assess the secondary study endpoint, SUVmax of the lymph node with the highest [18F]FDG uptake on restaging PET/CT scans of both indeterminate and positive cases were collected, if present, together with the corresponding product of the two largest diameters (mm2) measured on the co-registered CT images. Accordingly, the delta SUVmax (ΔSUVmax), calculated as the difference between the highest lymph node SUVmax at the baseline and the post-treatment PET/CT, was registered.
Statistical analysis
Post-treatment disease status was determined by any evidence of clinical, pathological, and/or radiological locoregional progression in the first 3 months from the final fraction of radiotherapy treatment. Progression-free survival (PFS) was defined as the time from the last day of treatment to the date of first recurrence (including primary tumor or regional lymph nodes recurrence as well as distant metastasis). Overall survival (OS) was defined as the time from the cancer diagnosis to death from any cause or last follow-up.
Sensitivity, specificity, PPV, NPV, and overall accuracy were calculated for each score. PFS and OS were estimated by the Kaplan–Meier method. In order to discriminate progression vs treatment-related changes, the optimal cutoff values of SUVmax, its delta, and the diameters product of the lymph node with the highest [18F]FDG uptake were evaluated using the ROC curve. In addition, to select potential prognostic factors a Cox proportional hazards regression analysis was performed by calculating the hazard ratios (HR) and corresponding 95% confidence intervals (CI 95%). The statistical significance level was set at p < 0.05. Statistical analysis was performed using SPSS for Windows software (Version 28.0; IBM Corp., Armonk, New York, USA).
Results
Patients’ characteristic
Among 812 [18F]FDG PET/CT scans performed in our Nuclear Medicine Department on 329 patients with histologically proven HNSCC, a total of 43 patients (median age 57 y; M:F = 32:11) met the inclusion criteria and were ultimately recruited for the analysis. The most frequent primary tumor site was the oropharynx (19/43, 44.2%), but HPV status was known only in 4 patients. Other primary tumor sites were the nasopharynx in 9/43 (21%) patients, larynx in 8/43 (18.6%), salivary glands in 4/43 (9.3%), and hypopharynx in 1/43 (2.3%), while 2/43 (4.6%) patients present an occult HNSCC.
Most patients experienced a stage IV (39/43, 90.7%), and a minority had a III stage (4/43, 9.3%) at diagnosis. Concurrent CRT was the primary treatment in most patients (93%), followed by RT alone in 3 patients (7%).
The median time between the end of treatment and the restaging [18F]FDG PET/CT was 5 months (range 2–11). The median time between diagnosis and the last follow-up was 48 months (range 7–153). In the first three months after the first restaging PET/CT exam, 15/43 (35%) patients showed disease progression in any site. During follow-up 19/43 (44%) patients experimented recurrence or metastatic disease; in particular, 5/19 (26%) experimented a primary tumor site recurrence, 4/19 (21%) had a locoregional lymph node involvement, 4/19 (21%) both primary tumor site and lymph node recurrence and 6/19 (32%) a metastatic disease (5 lung and 1 liver metastasis). Finally, 18/43 (42%) patients died during the follow-up.
Patients’ characteristics were resumed in Table 2.
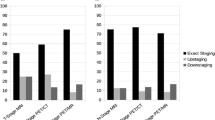
Visual score performance and survival correlation
The cumulative sensitivity, specificity, PPV, NPV, and accuracy were 87%, 86%, 76%, 92%, and 86% for the Hopkins score, whereas 93%, 79%, 70%, 96%, and 84% for the Deauville score, respectively. Conversely, the Cuneo score reached the highest specificity and PPV (93% and 78%, respectively) but the lowest sensitivity (47%), NPV (76%), and accuracy (77%). Diagnostic performance concerning the primary tumor site, lymph nodes, and overall score are summarized in Table 3.
Shifting patients with intermedium score for each criterion (score 3 for Hopkins and Deauville, and score 4 for Cuneo) into the no-responder group, the cumulative performance of the three criteria revealed a sensitivity, specificity, PPV, NPV, and accuracy of 93%, 71%, 64%, 95%, and 79% respectively for Hopkins score. Deauville and Cuneo score reached a 100% of sensitivity and NPV, indicating that treatment-related changes could often impact the intermedium score. Instead, specificity, PPV, and accuracy were respectively 64%, 60%, and 77% for the Deauville score and 75%, 68%, and 84% for the Cuneo criteria. The comparison between cumulative diagnostic performance considering different risk groups is shown in Table 4.
Considering the correlation of each visual score with the survival analysis, among the 19 patients who experienced disease recurrence or progression at any site, 16/19 (84%) showed a 4–5 HS, 18/19 (95%) a 4–5 DS, and 17/19 (89%) patients a 5–6 CS. Moreover, among 18 patients who died during follow-up, 12/18 (60%) patients had a 4–5 HS, 15/18 (68%) a 4–5 DS, and 8/18 (64%) a 5–6 CS. Each visual scale significantly correlated with PFS (p < 0.0001) and OS (Hopkins p = 0.05; Deauville p = 0.001; Cuneo p = 0.002). Kaplan–Meyer curves are displayed in Figs. 1 and 2.
Morphological and metabolic lymph node evaluation at restaging PET/CT
Focusing on the restaging [18F]FDG PET/CT scans, 19/43 (44.2%) patients showed a residual lymph node uptake. It was categorized as indeterminate in 11/19 using HS (others 8/19 scored 4 or 5), 9/19 with DS (others 10/19 scored 4 or 5), and 5/19 CS (others 14/19 scored 5 or 6).
The mean SUVmaxmax of residual lymph node uptake was 4.4 (SD ± 2.7), the mean ΔSUVmax was − 5.6 (SD ± 7.4) and the mean product of diameters of the lymph node with the highest uptake was 174.8 mm2 (SD ± 117.4).
Based on ROC curve analysis results (Fig. 3), a SUVmax cut-off of 2.75 extracted from post-treatment [18F]FDG PET/CT reached the best area under the curve (AUC) in discriminating progression from treatment-related changes (sensitivity 90%, specificity 56%; AUC = 0.806). The best cutoff for ΔSUVmax was − 6.6 (sensitivity 92%, specificity 54%; AUC = 0.667). The ROC curves for the product of diameters did not reach a significative AUC (0.567). The ROC analysis of the combination of the SUVmax and the product of diameters (Fig. 4) showed good discriminatory power with AUC of 0.822 (95% CI 0.624–1.0).
In the subgroup of indeterminate and positive cases, the multivariate analysis revealed the Cuneo criteria (HR 0.271, 95% CI 0.082–0.892, p = 0.032) and the product of diameters (HR 1.004, 95% CI 1.0–1.009, p = 0.051) as prognostic factors for PFS.
Discussion
Despite the consolidated role of [18F]FDG PET/CT in the treatment response evaluation of HNSCC, there is no clear consensus on the optimal interpretation criteria to use in this clinical scenario. Semi-quantitative PET parameters, such as the well-known SUVmax, have not proved to be reliable indicators probably due to the numerous technical and patient variables that could influence this value, especially in the investigated population (e.g. inflammation and post-treatment effects) [4, 15, 16].
Over the last years, considerable efforts have been made to standardize the reporting system in the surveillance of HNSCC and several qualitative assessment methods for predicting regional disease control have been proposed to find out the best [18F]FDG PET visual scale. However, none of them were approved and routinely used up to date. As known, one of the major limits remains the low sensitivity and PPV.
In our study, the head-to-head comparison between scales showed good sensitivity, specificity, and PPV (87%, 86%, and 76% respectively) and a high NPV (92%) of the first introduced Hopkins scale. Comparing our results with the reference one, published by Marcus and colleagues, we reported almost similar specificity and NPV (92.2% and 91.1%, respectively), but a higher sensitivity and PPV compared to 68.1% and 71.1% in the reference study [12].
Similarly, a 2017 study by Kendi et al. [17] on 69 HNSCC patients showed a sensitivity, specificity, PPV, and NPV of the overall therapy assessment of 66.7%, 87.3%, 33%, 96.5% respectively, underlining the higher sensitivity and PPV reached in our study. The diagnostic accuracy of PET/CT response assessment in our study might be affected by the time interval between treatment and follow-up imaging; the later median time point of imaging post-therapy (20 weeks) compared to other studies may explain slightly higher PPV[18].
More recently, other authors proposed to apply the Deauville score, the most famous 5-point standardized Likert scale used for Hodgkin’s and non-Hodgkin’s lymphoma, to post-treatment HNSCC PET assessment [19]. Benjamin et al. conducted a retrospective analysis on 43 HNSCC patients who underwent organ preservation radiotherapy and applied the DS to [18F]FDG PET/CT scan. Their study results showed a higher PPV than our (100% vs 70%), but only 4/43 patients experienced disease progression (4 or 5 DS) [4].
Another study by Zhong et al., in a larger cohort of 562 patients, compared the diagnostic performance of the Hopkins and Deauville score for the prediction of locoregional control and PFS. The study confirmed the high NPV of both visual criteria, also achieving a very high PPV compared to our as well as to the existing literature (51–78%). However, the authors attributed this higher value to the later median time point of imaging post-therapy (17 weeks) [20].
To deal with these conflicting results, in 2020 an Italian Multicentric study introduced a novel 6-point visual system called Cuneo score to find out a higher PPV [14]. The reference article compared the three different PET visual scores, reporting the best PPV for Cuneo score (with scores 3 and 4 clustered with 1 and 2, indicative of the absence of disease) for all categories: 42.9% for the primary tumor, 100% for the nodal involvement, and 50% for the cumulative score. In our cohort, primary tumor, lymph node involvement, and the cumulative Cuneo score reached higher PPV values (86%, 83%, and 78% respectively), at the expense of lower values of sensitivity and NPV, compared to Hopkins and Deauville scores. Our results support the hypothesis proposed by Bonomo et al. of considering 6-point visual criteria to minimize false positive PET findings in post-treatment evaluation of HNSCC, resulting in a better PPV. Further prospective studies with a larger sample are warranted to support the Cuneo criteria. However, since none of the mentioned criteria showed to be able to solve equivocal cases (e.g., Fig. 5) a further repeat PET/CT 3–6 months later is still necessary, as suggested by current guidelines [3].
♂, 53yo. with poorly differentiated squamous carcinoma of the posterior tongue histologically proven. Baseline PET/CT showed a pathological FDG-uptake in the primary tumor site as well as in the right cervical and supraclavicular lymph nodes. End-of-treatment (EOT) PET/CT, performed 14 weeks after radiotherapy, showed moderate residual uptake near the primary tumor site first considered as treatment-related and scores undetermined in 2 out of 3 visual scores. However, the follow-up PET/CT, performed about 10 months after EOT, showed a relapse of the disease in the primary tumor site as well as a contralateral lymph node spread
The survival analysis was consistent with the current literature [21]. All the studied scores again showed their high prognostic value in terms of both PFS and OS, underlining the reliability of a prognostic scoring system in HNSCC patients. Two clinical examples extracted from our sample are shown in Figs. 6 and 7, supporting the prognostic role of each visual score.
♀, 47yo. with a histological diagnosis of moderately differentiated squamous carcinoma of the oropharynx. Baseline [18F]FDG PET/CT showed a high uptake into the oropharynx extended to the nasopharynx with bilateral cervical lymph nodes involvement. Subsequently, the patient underwent concomitant chemo-radiotherapy. End-of-treatment (EOT) PET/CT, performed 17 weeks after radiotherapy, showed mild uptake in the primary site (SUVmax 4.1) and a persistent high FDG-uptake in the left cervical lymph node (SUVmax 5.8). All visual criteria scored pathologically. The follow-up PET/CT, performed about 9 months after EOT, demonstrated the persistence/recurrence of both locoregional and lymph node disease
♂, 69yo. with moderately differentiated squamous carcinoma of the oral cavity histologically proven. Baseline PET/CT showed a pathological FDG-uptake in the oral cavity. In addition, a moderate uptake was detected in the left retromandibular lymph node. Afterward, the patient underwent concomitant chemo-radiotherapy. End-of-treatment (EOT) PET/CT, performed 14 weeks after radiotherapy, showed no significant uptake both in the oral cavity and retromandibular lymph node, which appeared also calcific. Scores assigned are consistent with the metabolic response and confirmed at the follow-up PET/CT performed about 10 months later
Regarding the secondary endpoint of the study, both SUVmax extracted from restaging PET and ΔSUVmax were able to discriminate lymph node persistent disease from treatment-related changes, showing a good performance in predicting outcomes. However, their cutoff value found (2.75 for SUVmax, − 6.6 for ΔSUVmax) needs to be considered with caution, confirming the debated role of semiquantitative analysis in literature.
The added value of our study was the evidence that hybrid imaging, combining morphological and metabolic imaging, could improve [18F]FDG PET/CT interpretation in treatment response evaluation. Notably, the ROC analysis of the combination of the SUVmax and the product of diameters with the highest uptake on the restaging PET scan showed good discriminatory power with an AUC of 0.822. The multivariate analysis also demonstrated that the Cuneo criteria and the product of lymph node diameters could be considered prognostic factors for PFS. To the best of our knowledge, only one other study from 2016 study attempted to consider lymph node diameters (those with short axis) in the restaging PET scan but failed to assess its usefulness [21]. These results could help the visual interpretation of [18F]FDG PET/CT to clarify indeterminate cases and assign new risk classes. The use of contrast-enhanced CT on PET/CT exams could strengthen our hypothesis to better discriminate lymph node involvement [22].
The unknowledge of HPV-status in more than half of our sample limits our study. To note, HPV status is a well-known prognostic factor in HNSCC. HPV-related HNSCCs, which primarily arise in the oropharynx, have a markedly better prognosis compared to HPV-unrelated [15]. One study suggests that lymph node involvement may take longer to regress in patients with HPV-positive disease [23]. Accordingly, we can speculate that the slightly higher PPV obtained in our study than reported rates, could be related to the unknown HPV status as well as the time interval between the restaging PET/CT and the end of radiotherapy. As reported by some literature data, it is possible that HPV-positive patients with equivocal findings at 3-month [18F]FDG PET/CT assessment, could avoid a demolitive neck dissection if they undergo a further later PET/CT exam. For positive lymph node disease in HPV-associated patients achieving incomplete response on the 12-week restaging PET/CT, a repeat 16-week PET/CT showed to spare patients from unnecessary surgery [7, 24, 25]. Moreover, the retrospective nature of the study and the relatively small sample size should also be considered.
Conclusions
In conclusion, each PET-based qualitative therapy assessment was statistically related to prognosis, thus demonstrating the reliability of visual point-scale criteria in HNSCC after definitive non-surgical therapy. The new Cuneo score showed the highest specificity and PPV, but the lowest sensitivity and NPV compared to Hopkins and Deauville criteria. Furthermore, the combination of PET data with morphological features could support the evaluation of equivocal cases.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- HNSCC:
-
Head and neck squamous cell carcinoma
- [18F]FDG PET/CT:
-
Fluorine-18 fluorodeoxyglucose positron emission tomography/computed tomography
- SUV:
-
Standardized uptake value
- HC:
-
Hopkins criteria
- DS:
-
Deauville score
- CS:
-
Cuneo score
- PFS:
-
Progression-free survival
- OS:
-
Overall survival
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- HPV:
-
Human papillomavirus
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Denaro N, Merlano MC, Russi EG. Follow-up in head and neck cancer: do more does it mean do better? A systematic review and our proposal based on our experience. Clin Exp Otorhinolaryngol. 2016;9:287–97.
Treatment by Cancer Type. https://www.nccn.org/guidelines/category_1. Accessed 13 Apr 2022
Benjamin J, Hephzibah J, Shanthly N, Oommen R, Mathew D, Pavamani S, Rajnikanth J. F-18 FDG PET-CT for response evaluation in head and neck malignancy: experience from a tertiary level hospital in south India. Cance Rep. 2021. https://doi.org/10.1002/cnr2.1333.
Taghipour M, Mena E, Kruse MJ, Sheikhbahaei S, Subramaniam RM. Post-treatment FDG-PET/CT versus contrast-enhanced CT in patients with Oropharyngeal squamous cell carcinoma: comparative effectiveness study HHS public access. Nucl Med Commun. 2017;38:250–8.
Carbonara R, Bonomo P, di Rito A, Didonna V, Gregucci F, Ciliberti MP, Surgo A, Bonaparte I, Fiorentino A, Sardaro A. Investigation of radiation-induced toxicity in head and neck cancer patients through radiomics and machine learning: a systematic review. J Oncol. 2021. https://doi.org/10.1155/2021/5566508.
Mehanna H, Wong W-L, McConkey CC, et al. PET-CT surveillance versus neck dissection in advanced head and neck cancer. N Engl J Med. 2016;374:1444–54.
Gupta T, Master Z, Kannan S, Agarwal JP, Ghsoh-Laskar S, Rangarajan V, Murthy V, Budrukkar A. Diagnostic performance of post-treatment FDG PET or FDG PET/CT imaging in head and neck cancer: a systematic review and meta-analysis. Eur J Nucl Med Mol Imaging. 2011;38:2083–95.
McDermott M, Hughes M, Rath T, et al. Negative predictive value of surveillance PET/CT in head and neck squamous cell cancer. AJNR Am J Neuroradiol. 2013;34:1632–6.
Pak K, Cheon GJ, Nam HY, Kim SJ, Kang KW, Chung JK, Kim EE, Lee DS. Prognostic value of metabolic tumor volume and total lesion glycolysis in head and neck cancer: a systematic review and meta-analysis. J Nucl Med. 2014;55:884–90.
Paidpally V, Chirindel A, Chung CH, Richmon J, Koch W, Quon H, Subramaniam RM. FDG volumetric parameters and survival outcomes after definitive chemoradiotherapy in patients with recurrent head and neck squamous cell carcinoma. AJR Am J Roentgenol. 2014;203:W139.
Marcus C, Ciarallo A, Tahari AK, Mena E, Koch W, Wahl RL, Kiess AP, Kang H, Subramaniam RM. Head and neck PET/CT: therapy response interpretation criteria (Hopkins Criteria)-interreader reliability, accuracy, and survival outcomes. J Nucl Med. 2014;55:1411–6.
van den Wyngaert T, Helsen N, Carp L, et al. Fluorodeoxyglucose-positron emission tomography/computed tomography after concurrent chemoradiotherapy in locally advanced head-and-neck squamous cell cancer: the ECLYPS study. J Clin Oncol. 2017;35:3458–64.
Bonomo P, Merlotti A, Morbelli S, et al. Does a 6-point scale approach to post-treatment 18F-FDG PET-CT allow to improve response assessment in head and neck squamous cell carcinoma? A multicenter study. Eur J Hybrid Imaging. 2020. https://doi.org/10.1186/S41824-020-00077-9.
Kale H, Rath TJ (2017) Chapter 3. The role of PET/CT in squamous cell carcinoma of the head and neck. In: Seminars in ultrasound CT MR, vol. 38, pp. 479–94
Niccoli Asabella A, Nappi AG, Trani O, Sardaro A, Rubini G. Heterogeneous response to immunotherapy in a patient with tonsillar squamous cell carcinoma assessed by 18 F-FDG PET/CT. Diagnostics (Basel). 2021. https://doi.org/10.3390/DIAGNOSTICS11020348.
Kendi AT, Brandon D, Switchenko J, Wadsworth JT, El-Deiry MW, Saba NF, Schuster DM, Subramaniam RM. Head and neck PET/CT therapy response interpretation criteria (Hopkins criteria)—external validation study. Am J Nucl Med Mol Imaging. 2017;7:174.
Leung AS, Rath TJ, Hughes MA, Kim S, Branstetter BF. Optimal timing of first posttreatment FDG PET/CT in head and neck squamous cell carcinoma. Head Neck. 2016;38:E853–8.
Ferrari C, Asabella AN, Merenda N, Altini C, Fanelli M, Muggeo P, de Leonardis F, Perillo T, Santoro N, Rubini G. Pediatric Hodgkin lymphoma: predictive value of interim 18F-FDG PET/CT in therapy response assessment. Medicine. 2017. https://doi.org/10.1097/MD.0000000000005973.
Zhong J, Sundersingh M, Dyker K, Currie S, Vaidyanathan S, Prestwich R, Scarsbrook A. Post-treatment FDG PET-CT in head and neck carcinoma: comparative analysis of 4 qualitative interpretative criteria in a large patient cohort. Sci Rep. 2020. https://doi.org/10.1038/S41598-020-60739-3.
Wray R, Sheikhbahaei S, Marcus C, Zan E, Ferraro R, Rahmim A, Subramaniam RM. Therapy response assessment and patient outcomes in head and neck squamous cell carcinoma: FDG PET Hopkins criteria versus residual neck node size and morphologic features. Am J Roentgenol. 2016;207:641–7. https://doi.org/10.2214/AJR.15.15730.
Kendi AT, Corey A, Magliocca KR, et al. 18F-FDG-PET/CT parameters as imaging biomarkers in oral cavity squamous cell carcinoma, is visual analysis of PET and contrast enhanced CT better than the numbers? Eur J Radiol. 2015;84:1171–6.
Huang SH, O’Sullivan B, Xu W, et al. Temporal nodal regression and regional control after primary radiation therapy for N2–N3 head-and-neck cancer stratified by HPV status. Int J Radiat Oncol Biol Phys. 2013;87:1078–85.
Liu HY, Milne R, Lock G, Panizza BJ, Bernard A, Foote M, McGrath M, Brown E, Gandhi M, Porceddu SV. Utility of a repeat PET/CT scan in HPV-associated Oropharyngeal Cancer following incomplete nodal response from (chemo)radiotherapy. Oral Oncol. 2019;88:153–9.
Rulach R, Zhou S, Hendry F, et al. 12 week PET-CT has low positive predictive value for nodal residual disease in human papillomavirus-positive oropharyngeal cancers. Oral Oncol. 2019;97:76–81.
Acknowledgements
The abstract of this manuscript was presented at the 15th National Congress of the Italian Association of Nuclear Medicine and Molecular Imaging (AIMN). Clin Transl Imaging 10(Suppl 1), 1–111 (2022). https://doi.org/10.1007/s40336-022-00492-x
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
CF and GS conceptualized the study design and wrote the original draft. PM and DR were in charge of data collection and statistical analysis. AS1 and AS2 substantively revised the original draft. ARP and CF acquired, analyzed, and interpreted patient data. GR contributed to the study conception, critically reviewed the manuscript, and supervised the study. All authors contributed to the manuscript preparation, read, and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The institutional review board of Azienda Ospedaliero-Universitaria Consorziale Policlinico di Bari waived the ethical committee approval need for the retrospective analysis of clinically acquired data. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
All subjects provided written informed consent for publication of this study and accompanying images.
Competing interests
The authors declare that there is no competing interests regarding the publication of this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ferrari, C., Santo, G., Mammucci, P. et al. [18F]FDG PET/CT in head and neck squamous cell carcinoma: a head-to-head between visual point-scales and the added value of multi-modality imaging. BMC Med Imaging 23, 34 (2023). https://doi.org/10.1186/s12880-023-00989-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12880-023-00989-5