Abstract
Background
We aimed to evaluate the diagnostic performance of 99mTc-MIBI SPECT/CT and ultrasonography in patients with secondary hyperparathyroidism (SHPT), and explored the factors that affect the diagnostic performance.
Methods
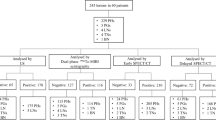
99mTc-MIBI SPECT/CT and ultrasonography were performed in 50 patients with SHPT within 1 month before they underwent surgery. Imaging results were confirmed by the pathology. Pearson correlation analysis was used to determine the correlation of PTH level with clinical data. The optimal cutoff value for predicting positive 99mTc-MIBI results was evaluated by ROC analysis in lesions diameter.
Results
Forty-nine patients had a positive 99mTc-MIBI imaging results and 39 patients had positive ultrasonography results. The sensitivities of 99mTc-MIBI and ultrasonography were 98.00% and 78.00%, respectively. A total of 199 lesions were resected in 50 patients. Among them, 183 lesions were proved to be parathyroid hyperplasia. On per-lesion basis analysis, the sensitivity and specificity of 99mTc-MIBI and ultrasonography were 59.34% and 75.00% vs 46.24% and 80.00%, respectively. The Pearson correlation analysis showed that the serum AKP and PTH level had a significant linear association (r = 0.699, P < 0.001). The lesion diameter was a statistically significant predictive factor in predicting positive 99mTc-MIBI SPECT/CT. The optimal cutoff value for predicting positive 99mTc-MIBI results evaluated by ROC analysis in lesions diameter was 8.05 mm.
Conclusion
Dual phase 99mTc-MIBI SPECT/CT imaging had a higher sensitivity in patients with SHPT than ultrasonography. Therefore, using 99mTc-MIBI positioning the lesion could be an effective method pre-surgical in patients with SHPT.
Similar content being viewed by others
Background
Secondary hyperparathyroidism (SHPT) occurs due to a progressive increase in the level of parathyroid hormone (PTH) in diseases that affect the metabolism of calcium or phosphorus and is a common complication in patients with chronic kidney disease [1, 2]. Patients with severe SHPT often develop high turnover bone disease, which can cause bone pain and skeletal fractures risk [3]. SHPT is also associated with an increased risk of cardiovascular calcification and mortality [4]. Traditional therapies such as administration of calcium salts and vitamin D are limited by hypercalcemia, hyperphosphatemia and lack of long-term efficacy [5].
Surgical parathyroidectomy remains the only option in 5% to 10% of patients with chronic renal failure who are treated with long-term dialysis and fail to respond to medical therapy [6, 7]. Successful surgical treatment can reduce the PTH levels and improve the clinical symptoms such bone pain. Different from primary hyperparathyroidism (PHPT) in which patients generally have only one lesion [8], patients with SHPT have multiple lesions [9]. The unguided bilateral neck exploration is effective in 90–95% patients [10]: surgical failure is due to ectopic glands and undetected multi-glandular disease. Surgical outcome is often unfavorable, resulting in persistent or recurrent hyperparathyroidism in 10–30% cases [11]; therefore, pre-surgical localization is necessary in patients with SHPT.
Parathyroid glands can be detected with multiple modalities, such as imaging, high-resolution (7.0–14.0 MHz) ultrasonography (USG), thin-section CT and MRI [12]. USG is an advantageous modality as a non- radiation emitting, and widely available technique in clinic. 99mTc-methoxyisobutyl isonitrile (99mTc-MIBI) is a common radiopharmaceutical used in parathyroid imaging. Dual-phase parathyroid imaging with 99mTc-MIBI currently represents the current diagnostic modality for parathyroid glands. The diagnostic performance of 99mTc-MIBI SPECT/CT in patients with SHPT showed a higher sensitivity and specificity compared with ultrasonography in detecting hyperplastic glands on a per-patient-based analysis [9, 13].
There were already some studies have reported the diagnostic performance of ultrasonography and 99mTc-MIBI dual phases imaging. But the results of sensitives had a vary difference. The sensitives of ultrasonography and 99mTc-MIBI dual phases imaging had a wide range of 35.9–91.5% and 36.6–66%, respectively [14,15,16]. Now we study the diagnostic performance of 99mTc-MIBI SPET/CT and ultrasonography in patients and lesions with SHPT were all studied, to explore the factors that affect the diagnostic performance of SPECT/CT, such as PTH level and diameter. The patients with secondary hyperparathyroidism that all had renal failure. Patients were undergoing both 99mTc-MIBI dual phases SPECT/CT imaging and ultrasonography before surgery.
Methods
Patients characteristic
We retrospectively studied the patients who underwent parathyroid 99mTc-MIBI imaging for elevated PTH level and ultrasonography for existing abnormal parathyroid between December 2012 and January 2017 in Ren Ji Hospital, School of Medicine, Shanghai Jiao Tong University. Medical record review included patient demographics (gender, age, dialysis vintage), clinical history, imaging, laboratory values (calcium, phosphorus, parathyroid hormone, alkaline phosphatase), and operative and pathological results and outcomes. Fifty pathologically confirmed secondary hyperparathyroidism patients were included in this study.
Imaging examinations
All patients with SHPT received an intravenous injection of 740 MBq of 99mTc-MIBI. Early parathyroid imaging was obtained 20 min post injection, and a delayed parathyroid imaging was obtained 2 h post the injection. SPECT/CT integrated imaging was performed at 2 h immediately after the delayed planar image. The imaging acquisition was using Philips precedence 16 (Philips, Medical Systems, Netherlands). A 256 × 256 matrix was used and 32 20-s projections were acquired over 360°. Imaging data were reconstructed using a three-dimensional iterative algorithm. Images were smoothed with a three-dimensional spatial Gaussian filter. CT acquisition parameters were as follows: tube current, 250 mA; and tube voltage, 120 kV. For CT data reconstruction, a 3-mm slice thickness with 2-mm slice increment was used. Both SPECT and CT 3-mm slices were generated using an Astonish bone application package (Philips) and were transferred to a picture archiving and communication system after generation of DICOM files. SPECT/CT images were fused using the Syntegra software (Philips). Ultrasonography (USG) was performed using the Technos DU8 scanner (Esaote SpA, Genoa Italy) with an 8 - 13MHZ LA523 linear-array transducer.
Image analysis
The imaging results were evaluated by visual analysis and the uptake value of lesions were judged by semi-quantitative visual analysis. SPECT/CT images were analyzed by two experienced nuclear medicine physicians who were blinded to the laboratory, surgical, and pathological results. Abnormal 99mTc-MIBI uptake was considered to be positive on visual analysis, and the different uptake value of each lesion was graded to three levels through the calculation of the tumor to background ratio (TBR) for the delayed phase. These areas were scored for activity on a three-point scale: 1 = slight uptake (1 < TRB ≤ 2), 2 = medium uptake (2 < TRB ≤ 3), 3 = high uptake (TRB > 3) [17] (Fig. 1). A positive parathyroid imaging result was increased uptake of 99mTc-MIBI on the delayed image compared to the early-stage image, with precise localization of the focus on the delayed planar image by SPECT/CT; negative parathyroid scan had no 99mTc-MIBI increased uptake on the delayed image compared to background.
The diameters of excised parathyroid adenoma, hyperplasia, or parathyroid carcinoma were measured by SPECT/CT. In positive 99mTc-MIBI cases, SPECT/CT located not only the lesion with 99mTc-MIBI on planar imaging but also measured the diameters of tumor.
Statistical analysis
Data are shown as mean ± standard deviation (SD). Semi-quantitative analysis of 99mTc-MIBI SPECT/CT was compared with the uptake value sum of a patient and the PTH level. Pearson’s correlation co-efficient was used for statistical analysis. Comparisons of continuous variables between two groups were performed using the t test. The Chi-square test was used for categorical variables. The optimal cutoff value of lesion diameter for predicting positive 99mTc-MIBI imaging was evaluated using receiver-operating characteristic (ROC) analysis. P value less than 0.05 was considered significant in this study. Statistical analysis was performed using the MedCalc version 15.6 statistical software (MedCalc Software bvba, Ostend, Belgium) and the IBM SPSS version 22.0 statistical software (IBM, Armonk, USA).
Results
The clinic pathological characters and 99mTc-MIBI data of the 50 patients with SHPT who underwent surgery are summarized in Table 1. For the patients included in the study, the primary diseases of all patients were chronic renal failure. And among them, there were 42 patients with peritoneal dialysis or hemodialysis. Among the 50 patients, 49 (98.00%) patients had a positive 99mTc-MIBI imaging, and only 1 patient had a negative 99mTc-MIBI imaging. 99mTc-MIBI imaging found an ectopic parathyroid in one patient (Fig. 2). For ultrasonography, there were 39 (78.00%) patients were found had at least one increased parathyroid. In patients with known serum calcium and phosphorus levels, 34.00% (17/50) and 76.00% (38/50) patients showed higher serum calcium and phosphorus levels, respectively.
A middle-aged patient was affected by SHPT. A dual-phase 99mTc-MIBI planar imaging was performed before surgery. Early and delayed phase imaging showed an ectopic parathyroid within the upper mediastinum (an arrow). 99mTc-MIBI SPECT integrated CT found the lesion located in front the aortic arch. The histology result confirmed the parathyroid hyperplasia
In 50 patients who underwent surgery, two patients had parathyroid subtotal resection, 48 patients had complete parathyroid resection and autologous transplantation. A total of 199 glands were resected in the surgery of the 50 patients. One hundred and eighty-three glands were proved to be parathyroid lesions. Four glands were confirmed to be normal parathyroid glands, twelve were lymph nodes. In 100 and 83 confirmed lesions, 179 were parathyroid hyperplasia, and 4 lesions in 3 patients were confirmed to be parathyroid adenoma (Fig. 3). Among the fifty patients, the pathological results revealed one lesion from one patient (2%), two lesions from 4 patients (4%), three lesions from 6 patients (12%), and four lesions from the rest 39 patients (78%). 99mTc-MIBI imaging showed 112 positive lesions in 50 patients, and 108 lesions confirmed to be true positive. For the 4 false positive lesions found in three patients, two lesions were confirmed to be thyroid tissue, two lesions were lymph nodes. Seventy-four lesions found in 39 patients showed negative 99mTc-MIBI uptake but were the pathological confirmed to be parathyroid hyperplasia or adenoma. On per-lesion basis analysis, the sensitivity and specificity of 99mTc-MIBI were 59.34% and 75.00%, respectively. Eighty-nine enlarged lesions in ultrasonography, 86 lesions were confirmed to be true positive. Ninety-seven normal size lesions were pathological confirmed to be parathyroid hyperplasia. Therefore, on per-lesion basis analysis, the sensitivity and specificity of ultrasonography were 46.24% and 80.00%, respectively. A representative ultrasonography imaging showed in the Fig. 4.
A old age patient was affected by SHPT. A dual-phase 99mTc-MIBI imaging was performed. Early and delayed phase imaging showed two enlarged parathyroid glands located superior the right thyroid glands (an arrow). 99mTc-MIBI SPECT/CT imaging depicting the biggest focus located superior the right thyroid gland. The histology confirmed the lesion was a parathyroid adenoma
The three-point scale the score of lesions were judged by semi-quantitative visual analysis
. The image a represent slight uptake (TBR = 1.61) scores one point, the image b show medium uptake (TBR = 2.26) scores two points, the image c show high uptake (TBR = 3.58) scores three points. The red arrow refers to the parathyroid glands with the MIBI uptake
Abnormal 99mTc-MIBI uptake was considered to be positive on visual analysis, and the different uptake strength of each lesion was graded to three levels. Each lesion was scored according to 99mTc-MIBI uptake level. And then the lesions number of each patient and lesion uptake value scores of one patient were grouped for the 50 patients included; the numbers of patients in each group were listed in Table 2. Furthermore, for these patients, the number of lesions for each patient was counted on the basis of the pathological results. The correlation between PTH level and laboratory test items such as calcium, phosphorus and alkaline phosphatase were analyzed. Pearson correlation results showed a significant linear association between the serum AKP level and PTH level (r = 0.699, P < 0.001). The lesions diameter and the number of lesions were confirmed by pathological results, and the lesion uptake value scores of each patient showed no significant linear association with PTH levels.
Following ROC analysis, the optimal cutoff values of the maximum tumor diameter for predicting positive 99mTc-MIBI was 8.05 mm (AUC 0.731, 95% CI 0.618–0.843; sensitivity = 82.20% and specificity = 52.90%) (Fig. 5). The cutoff values of 8.05 mm was used for lesion diameter in the 118 lesions as measured by SPECT/CT. Eighteen lesions (66.67%) of 27 lesions were negative in 99mTc-MIBI SPECT/CT in patients with a lesion diameter lower than the cutoff value (P < 0.0001) (Table 3).
Discussion
We studied rare cases in patients with secondary hyperparathyroidism that all had renal failure. All the patients were undergoing both 99mTc-MIBI dual phases SPECT/CT imaging and ultrasonography before surgery. 99mTc-MIBI parathyroid imaging is a valuable method based on the differential washout rate between the thyroid tissue and parathyroid hyperplasia [12]. Parathyroid hyperplasia has very high metabolic rate despite its small size, and it shows intense 99mTc-MIBI uptake. More recently, SPECT/CT systems combining state-of-the-art multi-detector CT and state-of-the-art gamma cameras are being produced, and guidelines for image acquisition, interpretation, and reporting for patients with SHPT have been published [13, 18]. SPECT/CT imaging also influences the surgical approach, enabling to choose different surgical approaches for lesions in different areas [19]. In our study, imaging detected an ectopic parathyroid in one patient. The major significance of 99mTc-MIBI imaging pre-surgery was the detection of ectopic parathyroid, which guided the surgery. In our study, the sensitivities of 99mTc-MIBI imaging on a per-patient basis and on a per-lesion basis were 98.00% and 59.34%, respectively. For USG the results were 78.00% and 46.24%, respectively.
In our study the sensitivity of 99mTc-MIBI imaging on a per-lesion basis was 59.34% that exactly matches to a meta-analysis publication on planar 99mTc-MIBI imaging the pooled sensitivity was 58% in SHPT [20]. There were many researches results showed that the sensitivity of SPECT/CT should be higher than planar 99mTc-MIBI imaging [21]. There was also study showed that single-phase SPECT/CT (early or delayed) had not significant in superior to dual-phase planar imaging for sensitivity. Dual-phase SPECT/CT had statistically significant in superior to single-phase SPECT/CT and superior to dual-phase planar imaging and dual-phase SPECT [22, 23]. Therefore, 99mTc-MIBI imaging show a limitation in the diagnosis of lesions in patients with SHPT. Usually we used the 99mTc-MIBI uptake value as the guide information to diagnose whether the parathyroid lesions were; and CT information only was used to confirm the diagnosis. However, it was very difficult to differentiate the lymph node and the tumors only by CT for the lesions without 99mTc-MIBI uptake in SPECT imaging. 99mTc-MIBI has a lower sensitivity in multiple gland disease [24]. But the mechanism is not clear at present. The pre-surgical localization determines the success rate of surgery and the risk of recurrence. Compared to patients with PHPT who mostly have only one lesion [8], most of the patients with SHPT have multiple lesions [9]. The surgical results in our research also proved that 78% of the patients had four lesions. If the surgeon determines the surgical resection according to the 99mTc-MIBI imaging results, many lesions would be missed. Intraoperative PTH assay is routinely used in clinical practice, and Ohe’s study showed that the decrease in the level of intraoperative PTH could predict the rate of successful parathyroidectomy [25].
In the per-lesion-based analysis, the specificity of 99mTc-MIBI imaging was 75.00%. The most common cause false-positive results were the presence of thyroid nodules. Because MIBI can be taken up by both hyper-functioning parathyroid and thyroid tissue, the differential diagnosis is based on its elimination from the hyper-functioning thyroid and parathyroid glands. Normal parathyroid tissue without uptake in either of the two phases. The possibility of clearances in similar times for both tissues, which could lead to false negatives, has also been described [11, 26]. Specificity of parathyroid imaging is highly dependent on the prevalence of thyroid nodular disorders in the evaluated patient population [23]. The factors may affect the diagnostic accuracy rate were the followings: the location of parathyroid glands, the size of the lesion, and the functional activity of the lesions, and the prevalence of mitochondria-rich oxyphil cells [27, 28]. Lesion size is important as it relates to the system resolution and to the amount of tracer taken up by the parathyroid tissue [29]. Our results showed that lesion diameter was a statistically significant predictive factor in predicting positive 99mTc-MIBI SPECT/CT. The larger the lesion diameter, the higher was the MIBI uptake value.
Serum PTH is a major regulator of mineral metabolism that plays a critical role in the maintenance of calcium and phosphate levels [30]. The major physiologic function of PTH is the circulation of ionized calcium. PTH has effects on the gut, kidney, and bone, serving to maintain serum calcium level within a tight range [31]. The pathogenesis of patients with PHPT is independent secretion of PTH by the parathyroid tissue. Unlike patients with PHPT, patients with SHPT have a compensatory PTH secretion for hypocalcaemia. Therefore, in patients with SHPT, the serum calcium level is uncertain; it may increase or remain normal. Pearson correlation analysis between PTH level and various factors showed that the serum AKP level and PTH level exhibit a significant linear association. PTH increased the bone metabolism conversion to elevate the serum AKP level. High level of AKP is the marker of increased bone conversion [32].
Conclusion
Our study demonstrated that the dual phase 99mTc-MIBI SPECT/CT imaging had a higher sensitivity in the diagnosis of patients with SHPT than ultrasonography on a per-patient-based analysis (98.00% vs. 78.00%). On a per-lesion-based analysis, the sensitivity and specificity of 99mTc-MIBI were 59.34% and 75.00%, respectively. The results of ultrasonography were 46.24% and 80.00%. Dual phase 99mTc-MIBI scan for positioning the lesion is an effective pre-surgical tool for patients with SHPT. The lesion diameter maybe a limitation for 99mTc-MIBI SPECT/CT imaging sensitivity, when the lesion diameter was above 8.05 mm, the higher positive result can be obtained. Serum AKP and PTH level exhibited a significant linear association. That means the higher PTH level, the higher AKP level.
Abbreviations
- 99mTc-MIBI:
-
Technetium-99 m-hexakis [2-methoxy-2-methylpropylisonitrile]
- PHPT:
-
Primary hyperparathyroidism
- PTH:
-
Parathyroid hormone
- ROC:
-
Receiver-operating characteristic
- SD:
-
Standard deviation
- SHPT:
-
Secondary hyperparathyroidism
- USG:
-
ultrasonography
References
Kumar R, Thompson JR. The regulation of parathyroid hormone secretion and synthesis. J Am Soc Nephrol. 2011;22(2):216–24.
Canalejo A, Canalejo R, Rodriguez ME, Martinez-Moreno JM, Felsenfeld AJ, Rodriguez M, Almaden Y. Development of parathyroid gland hyperplasia without uremia: role of dietary calcium and phosphate. Nephrol Dial Transplant. 2010;25(4):1087–97.
Jadoul M, Albert JM, Akiba T, Akizawa T, Arab L, Bragg-Gresham JL, Mason N, Prutz KG, Young EW, Pisoni RL. Incidence and risk factors for hip or other bone fractures among hemodialysis patients in the dialysis outcomes and practice patterns study. Kidney Int. 2006;70(7):1358–66.
Kimata N, Albert JM, Akiba T, Yamazaki S, Kawaguchi T, Fukuhara S, Akizawa T, Saito A, Asano Y, Kurokawa K, et al. Association of mineral metabolism factors with all-cause and cardiovascular mortality in hemodialysis patients: the Japan dialysis outcomes and practice patterns study. Hemodial Int. 2007;11(3):340–8.
Torres PU, Prie D, Beck L, Friedlander G. New therapies for uremic secondary hyperparathyroidism. J Ren Nutr. 2006;16(2):87–99.
Rajhbeharrysingh U, El Youssef J, Leon E, Lasarev MR, Klein R, Vanek C, Mattar S, Berber E, Siperstein A, Shindo M, et al. Expanding the net: the re-evaluation of the multidimensional nomogram calculating the upper limit of normal PTH (maxPTH) in the setting of secondary hyperparathyroidism and the development of the MultIdimensional predictive hyperparaTHyroid model (mi-PTH). Surgery. 2016;159(1):226–39.
Puccini M, Carpi A, Cupisti A, Caprioli R, Iacconi P, Barsotti M, Buccianti P, Mechanick J, Nicolini A, Miccoli P. Total parathyroidectomy without autotransplantation for the treatment of secondary hyperparathyroidism associated with chronic kidney disease: clinical and laboratory long-term follow-up. Biomed Pharmacother. 2010;64(5):359–62.
Khan AA, Bilezikian JP, Potts JT Jr. Guest editors for the third international workshop on asymptomatic primary H: the diagnosis and management of asymptomatic primary hyperparathyroidism revisited. J Clin Endocrinol Metab. 2009;94(2):333–4.
Michaud L, Balogova S, Burgess A, Ohnona J, Huchet V, Kerrou K, Lefevre M, Tassart M, Montravers F, Perie S, et al. A pilot comparison of 18F-fluorocholine PET/CT, Ultrasonography and 123I/99mTc-sestaMIBI dual-phase dual-isotope Scintigraphy in the preoperative localization of Hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism: influence of thyroid anomalies. Medicine (Baltimore). 2015;94(41):e1701.
Stracke S, Keller F, Steinbach G, Henne-Bruns D, Wuerl P. Long-term outcome after total parathyroidectomy for the management of secondary hyperparathyroidism. Nephron Clin Pract. 2009;111(2):c102–9.
Ardito G, Revelli L, Giustozzi E, Giordano A. Radioguided parathyroidectomy in forearm graft for recurrent hyperparathyroidism. Br J Radiol. 2012;85(1009):e1–3.
Delbeke D, Coleman RE, Guiberteau MJ, Brown ML, Royal HD, Siegel BA, Townsend DW, Berland LL, Parker JA, Zubal G, et al. Procedure guideline for SPECT/CT imaging 1.0. J Nucl Med. 2006;47(7):1227–34.
Kim YI, Jung YH, Hwang KT, Lee HY. Efficacy of (9)(9)mTc-sestamibi SPECT/CT for minimally invasive parathyroidectomy: comparative study with (9)(9)mTc-sestamibi scintigraphy, SPECT, US and CT. Ann Nucl Med. 2012;26(10):804–10.
Lee JB, Kim WY, Lee YM. The role of preoperative ultrasonography, computed tomography, and sestamibi scintigraphy localization in secondary hyperparathyroidism. Ann Surg Treat Res. 2015;89(6):300–5.
Lai EC, Ching AS, Leong HT. Secondary and tertiary hyperparathyroidism: role of preoperative localization. ANZ J Surg. 2007;77(10):880–2.
Perie S, Fessi H, Tassart M, Younsi N, Poli I, St Guily JL, Talbot JN. Usefulness of combination of high-resolution ultrasonography and dual-phase dual-isotope iodine 123/technetium Tc 99m sestamibi scintigraphy for the preoperative localization of hyperplastic parathyroid glands in renal hyperparathyroidism. Am J Kidney Dis. 2005;45(2):344–52.
Kaczirek K, Prager G, Kienast O, Dobrozemsky G, Dudczak R, Niederle B, Kurtaran A. Combined transmission and (99m)Tc-sestamibi emission tomography for localization of mediastinal parathyroid glands. Nuklearmedizin. 2003;42(5):220–3.
Henry JF, Sebag F, Cherenko M, Ippolito G, Taieb D, Vaillant J. Endoscopic parathyroidectomy: why and when? World J Surg. 2008;32(11):2509–15.
Ohe MN, Santos RO, Kunii IS, Carvalho AB, Abrahao M, Neves MC, Lazaretti-Castro M, Cervantes O, Vieira JG. Intraoperative PTH cutoff definition to predict successful parathyroidectomy in secondary and tertiary hyperparathyroidism. Braz J Otorhinolaryngol. 2013;79(4):494–9.
Caldarella C, Treglia G, Pontecorvi A, Giordano A. Diagnostic performance of planar scintigraphy using (9)(9)mTc-MIBI in patients with secondary hyperparathyroidism: a meta-analysis. Ann Nucl Med. 2012;26(10):794–803.
Oksuz MO, Dittmann H, Wicke C, Mussig K, Bares R, Pfannenberg C, Eschmann SM. Accuracy of parathyroid imaging: a comparison of planar scintigraphy, SPECT, SPECT-CT, and C-11 methionine PET for the detection of parathyroid adenomas and glandular hyperplasia. Diagn Interv Radiol. 2011;17(4):297–307.
Lavely WC, Goetze S, Friedman KP, Leal JP, Zhang Z, Garret-Mayer E, Dackiw AP, Tufano RP, Zeiger MA, Ziessman HA. Comparison of SPECT/CT, SPECT, and planar imaging with single- and dual-phase (99m)Tc-sestamibi parathyroid scintigraphy. J Nucl Med. 2007;48(7):1084–9.
Qiu ZL, Wu B, Shen CT, Zhu RS, Luo QY. Dual-phase (99m)Tc-MIBI scintigraphy with delayed neck and thorax SPECT/CT and bone scintigraphy in patients with primary hyperparathyroidism: correlation with clinical or pathological variables. Ann Nucl Med. 2014;28(8):725–35.
Pattou F, Huglo D, Proye C. Radionuclide scanning in parathyroid diseases. Br J Surg. 1998;85(12):1605–16.
Mullan BP. Nuclear medicine imaging of the parathyroid. Otolaryngol Clin N Am. 2004;37(4):909–39. xi-xii
Sun Y, Cai H, Bai J, Zhao H, Miao Y. Endoscopic total parathyroidectomy and partial parathyroid tissue autotransplantation for patients with secondary hyperparathyroidism: a new surgical approach. World J Surg. 2009;33(8):1674–9.
Torregrosa JV, Fernandez-Cruz L, Canalejo A, Vidal S, Astudillo E, Almaden Y, Pons F, Rodriguez M. (99m)Tc-sestamibi scintigraphy and cell cycle in parathyroid glands of secondary hyperparathyroidism. World J Surg. 2000;24(11):1386–90.
Vulpio C, Bossola M, De Gaetano A, Maresca G, Bruno I, Fadda G, Morassi F, Magalini SC, Giordano A, Castagneto M. Usefulness of the combination of ultrasonography and 99mTc-sestamibi scintigraphy in the preoperative evaluation of uremic secondary hyperparathyroidism. Head Neck. 2010;32(9):1226–35.
Hindie E, Zanotti-Fregonara P, Just PA, Sarfati E, Melliere D, Toubert ME, Moretti JL, Jeanguillaume C, Keller I, Urena-Torres P. Parathyroid scintigraphy findings in chronic kidney disease patients with recurrent hyperparathyroidism. Eur J Nucl Med Mol Imaging. 2010;37(3):623–34.
Hindie E, Ugur O, Fuster D, O'Doherty M, Grassetto G, Urena P, Kettle A, Gulec SA, Pons F, Rubello D, et al. 2009 EANM parathyroid guidelines. Eur J Nucl Med Mol Imaging. 2009;36(7):1201–16.
Salamone D, Muresan S, Muresan M, Neagoe R: Multilevel brown tumors of the spine in a patient with severe secondary hyperparathyroidism A case report and review of the literature. Ann Ital Chir 2016;87(ePub):1–5.
Powell WF Jr, Barry KJ, Tulum I, Kobayashi T, Harris SE, Bringhurst FR, Pajevic PD. Targeted ablation of the PTH/PTHrP receptor in osteocytes impairs bone structure and homeostatic calcemic responses. J Endocrinol. 2011;209(1):21–32.
Acknowledgments
There is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding
This work was funded by the National Natural Science Foundation of China (Grant No. 81471708), Shanghai Jiao Tong University Medical Engineering Cross research fund (No. YG2016MS55) and Shanghai Municipal Education Commission— Gaofeng Clinical Medicine Grant Support (No.20172010).
Availability of data and materials
The datasets analyzed during the current study are not publicly available due to them containing information that could compromise research participant privacy/consent. The data are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
Study concept: L PL, L QL, S XG, S SL; Study design: L PL, S XG, S SL; Data acquisition: L PL, L QF; Data analysis and interpretation: L PL, L QF, X L; Statistical analysis: T DQ, Z YY; Manuscript preparation: L PL; Manuscript editing: S XG, S SL; Manuscript review: S SL. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective study was approved by the Ethics Committee of Renji Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, which is to be carried out in compliance with the International guidelines for human research protection of the Declaration of Helsinki and International Conference on Harmonization in Good Clinical Practical (ICH-GCP). Written informed consent was obtained from all individual participants included in the study.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Li, P., Liu, Q., Tang, D. et al. Lesion based diagnostic performance of dual phase 99mTc-MIBI SPECT/CT imaging and ultrasonography in patients with secondary hyperparathyroidism. BMC Med Imaging 17, 60 (2017). https://doi.org/10.1186/s12880-017-0235-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12880-017-0235-3