Abstract
Background
To evaluate the reproducibility of signal intensity index (SII) measurements with MRI systems from different vendors and with different field strengths, and to test the effectiveness of flip angle.
Methods
Thirty-two healthy volunteers (mean age 35.3 ± 9.3 years) were enrolled in this ethics committee-approved study. Chemical shift MR imaging was performed on 1.5- and 3.0-T MR systems from three vendors. Two independent observers measured SII values in five lumbar segments. Inter- and intraobserver agreement was assessed using the interclass correlation coefficients (ICCs). Differences of mean SII values between different field strengths and MR vendors as well as flip angles were compared by using repeated-measures analysis of variance. Differences of mean SII values between different flip angles were also compared by using paired-sample t test.
Results
Inter- and intra-observer correlation coefficients showed good agreement (all ICC > 0.75) when measuring SII values at different MR systems (ICCs ranging from 0.896 to 0.983) and flip angles (ICCs ranging from 0.824 to 0.983). There were no significant differences in mean SII values measured by different MR vendors with different field strengths (all p > 0.05 ranging from 0.337 to 0.824). The differences in the mean SII between the four different flip angles were statistically significant (all p < 0.05 ranging from < 0.001 to 0.004) except the group of flip angle 50° versus 70° (p = 0.116).
Conclusion
The SII measurement using chemical shift MR imaging may be comparable between different MR systems. Also high flip angles showed better stability to quantitate lumbar fat content.
Similar content being viewed by others
Background
Chemical shift magnetic resonance (MR) imaging (also known as in-phase and out-of-phase imaging or opposed-phased imaging) is a simple technique that takes advantage of the fact that water and lipid hydrogen protons in a single voxel show slightly different precession frequencies [1]. Based on phase differences in images acquired via different TEs, lipid and water signals are additive on in-phase images and subtracted on opposed-phase images [2]. This technique has been proved to be extremely useful for characterization of lesions and organs with fatty components and has gained widespread acceptance [3–6]. In clinical practice, it is widely used to diagnose lipid-poor adrenal adenomas [3, 7]. On the same bias, chemical shift MR imaging has been used to evaluate vertebral bone marrow fat content in osteoporosis or in distinguishing benign and malignant causes of vertebral bone morrow infiltration [2, 4, 7–16]. Furthermore, some investigators measured the signal intensity index (SII) value to avoid the problem of signal intensity variability produced by the reference tissue, and found that it appeared to be the most reliable method for differentiating adenomas from non-adenomas [7, 17]. However, there exists a major difference if measurements are performed at the adrenal gland or the bone marrow as reproducibility errors always have to be considered in relation to the variance that is expected in a population.
In spite of great interest in and enthusiasm about chemical shift MR imaging, there is a clear need for standardization of both the acquisition and the interpretation of chemical shift MR images to resolve current difficulties in comparing SII values from different studies or from different sites to enable validation of this quantitative parameter as a qualified biomarker in the context of multicenter studies.
SII measurements can be influenced by many factors such as chemical shift effect, susceptibility effect (i.e. T2* decay) and T1 relaxation, etc. [8, 18, 19]. Chemical shift effect occurs due to the slightly different precession frequency of water and fat. Susceptibility effect results from field inhomogeneity which is obvious at 3.0 Tesla or from the composition of the lesion itself [19]. As for the T1 relaxation, it depends on imaging parameters such as repetition time (TR) and flip angle [20]. Overall, whether SII values measured by chemical shift MR imaging can be compared across MR systems from different vendors and across field strengths remains an open question.
Thus, the aims of this study were to evaluate the reproducibility of SII values in the lumbar segments measured with MRI systems from different vendors and at different field strengths, and to test the effect of flip angle on assessing bone marrow fat content with respect to measurement of the signal intensity index (SII).
Methods
This clinical study was approved by our Institutional Review Board (First Affiliated Hospital of Fujian Medical University) and written informed consent was obtained from all healthy volunteers enrolled in the study.
Study population
In this present study, 35 healthy volunteers were included for chemical shift MR imaging of the lumbar spine between March 2015 and May 2015. The inclusion criteria for this study were as follows: (1) no history of trauma or surgery in the lumbar spine; (2) no history of acute or chronic pain in lower back; (3) no history of diseases which could change the signal intensity of lumbar marrow. The exclusion criteria was performed after interviewing the volunteers and reviewing their medical records, which included: (a) a history of or findings related to marrow diseases such as osteoporotic/traumatic fracture, traumatic, myeloma, osteosarcoma, lymphoma, spondylitis, etc.; (b) contraindications to MR imaging; (c) failure to complete the chemical shift imaging procedure for any reason; and (d) poor image quality insufficient for image analysis.
MR imaging protocol
Data were acquired with 1.5 T MR systems (Vantage Altas, Toshiba Medical Systems, Otawara-shi, Japan) using phased-array spine coils with the following sequences: sagittal T1-weighted spin-echo sequence (500/10 [repetition time msec/echo time msec]), sagittal T2-weighted fast spin-echo sequence (4000/110 [repetition time msec/echo time msec]) and sagittal short inversion time inversion-recovery (STIR) fast spin-echo sequence (3500/65 [repetition time mse/echo time msec]). Chemical shift imaging data were acquired with 1.5 T MR systems from two vendors (Vantage Altas, Toshiba Medical Systems, Otawara-shi, Japan; Signa Twinspeed, GE Healthcare, Milwaukee, WI) and 3.0 T MR system from one vendor (Magneton Verio, Siemens Medical Solutions, Erlangen, Germany) using phased-array spine coils in one week. The sequence parameters on 1.5 T MR systems were as follows: sagittal out-of-phase (OP) (2.4/192 [repetition time mse/echo time msec]) fast spoiled gradient echo MR imaging was first scanned, followed by sagittal in-phase (IP) (4.8/192 [repetition time mse/echo time msec]) MR imaging. And the sequence parameters on 3.0 T MR system were as follows: sagittal in-phase (IP) (2.4/192 [repetition time mse/echo time msec]) MR imaging was first scanned, followed by out-of-phase (OP) (5.8/192 [repetition time mse/echo time msec]) fast spoiled gradient echo MR imaging. In addition, chemical shift MR imaging was performed on 3.0 T MR scanners with four flip angles (10, 30, 50, 70°), whereas only one flip angle at 70° was used in 1.5 T scanner. For all sagittal sequences, the field of view was 24 cm × 24 cm. The matrix was 256 × 256, and the section thickness was 4.0 mm, with a skip of 1.0 mm.
Image analysis
All chemical shift MR imaging data were transferred to an independent workstation for evaluation. Two readers (Z.X. and Y.Z., radiologists with 2 and 4 years of clinical experience in musculoskeletal MR imaging, respectively) independently drew rectangular regions of interest (ROIs) with a specific size in the center of three representative sections of each vertebral body, including midsagittal sections and adjacent two sections. The ROI size was initially defined by two authors in consensus (D.C. and J.L., radiologists with 28 and 23 years of clinical experience in musculoskeletal MR imaging, respectively) in a test set of images. The ROI was defined based on the largest possible rectangular size measuring 1.0 cm × 1.5 cm for the respective sections, and size for each region was kept constant during placement of ROIs by using the function of copy and paste in our workstation. Thus, a total of 54 ROIs were collected for each volunteer (three sections per vertebral body, five vertebral body, three vendors with two field strength plus other three flip angles in three sections of one vertebral body in 3.0 T scanner, 3 × 5 × 3 + 3 × 3 × 1 = 54). Care was taken to exclude areas with obvious artifacts from the ROIs.
The signal intensity index (SII) was measured independently by two radiologists blinded for patient data (C.L. and D.S. with 6 and 4 years of clinical experience in musculoskeletal MR imaging, respectively). SII was defined as the percentage of signal change on the OP sequence compared to the IP sequence according to previously described equation [21, 22]: SII = (SIIP-SIOP)/SIIP × 100%. SIIP refers to mean signal intensity of the bone marrow on IP sequences and SIOP refers to mean signal intensity of the bone marrow on OP sequences. For further analyses, the mean SII value of the two readers was calculated for each placed ROI.
Statistical analysis
SII values were expressed as mean ± standard deviation (SD) and were tested first with the Kolmogorov-Smirnov test for normality and then with the Levene test for variance homogeneity.
Intra- and inter-observer agreement of SII measurements were assessed using intra- and interclass correlation coefficients (ICCs). An ICC greater than 0.75 was indicative of good agreement [23]. The mean differences, SD, and 95% limits of agreement (LOA) were calculated using the Bland-Altman method [24, 25]. Measurement repeatability was assessed by the Bland-Altman analysis in order to define the agreement between replicate measurements. The repeatability coefficient, which represents the threshold value below which the absolute differences between two measurements on the same subject is expected to lie for 95% of the measurement pairs, was assessed using the formula 1.96 × SD of the mean difference (dSD), and expressed as percentage of the mean SII value.
Differences of mean SII values between different field strengths and MR vendors as well as flip angles were compared by using repeated-measures analysis of variance. Next, differences of mean SII values between different flip angles were also compared by using paired-sample t test. The Bonferroni method was used to adjust for multiple comparisons when necessary.
All statistical calculations were performed using the commercially available software package (PASW, Version 18.0, SPSS Inc., Chicago, IL, USA). Differences were considered significant when p values were less than 0.05.
Results
Population demographics
Thirty-five volunteers were enrolled in this study. Three of them did not complete the study because of poor image quality (n = 2) or incomplete acquisition of all sequences (n = 1). Thirty-two volunteers successfully completed the imaging examinations (22 men and 10 women; mean age 35.3 ± 9.3 years; age range 21–50 years), and all the MR data sets were eligible for evaluation.
Repeatability of SII measurements in different MR systems and flip angles
The SIIs measured in this study met the normal distribution (p = 0.193) and homogeneity of variance (p = 0.128). The intraobserver ICC calculated based on reader 1’s two measurements of SII values in 3.0 T Siemens system ranged from 0.896 to 0.972, with the 95% LOA ranging from (0.860, 0.923) to (0.962, 0.989) (Table 1). Interobserver agreement between reader 1’s first measurements and reader 2’s measurements was good for the three MR systems, with ICC (95% LOA) ranging from 0.916 (0.885, 0.938) to 0.983 (0.954, 0.975). The intra- and interobserver ICC results show good agreement between MR systems (all ICC > 0.75).
As shown in Table 2, the intra- and inter-observer ICC (95% LOA) ranged from 0.824 (0.668, 0.907) to 0.983 (0.954, 0.995), showing good agreement in measuring SIIs in different flip angles (all ICC > 0.75).
Mutual agreement of mean SII measurements with different MR systems
The goal of this study was to assess agreement of mean SII values with different vendors at the same field strength (1.5 T Toshiba Vantage–1.5 T GE Signa), different field strengths and vendors (1.5 T GE Signa–3.0 T Siemens Verio; 1.5 T Toshiba Vantage-3.0 T Siemens Verio).
Overall, the agreement of above three conditions was desirable as the mean differences were very small (the mean differences ranged from −1. 324 to 3.462) and most of the data points lied within 95% LOA (Figs. 1, 2). As shown in Table 3, the bias was not systematic, but depended on the specific lumbar segments and on the different MR systems. For instance, there existed significant bias on the measurements of SII values in L1 with three different MR systems; some segments (for example L3) showed negligible bias in comparison within the same field strength (Toshiba-GE), but a little bias when combining 1.5 T and 3.0 T data (1.5 T GE–3.0 T Siemens and 1.5 T Toshiba–3.0 T Siemens).
Mutual agreement of signal intensity index (SII) measured from different MR systems. The Bland-Altman plots show SII difference versus SII mean in different MR systems. For each lumbar segment, the mean SII difference (the red solid line) and the limits of agreements (lower limit: the green interrupted horizontal line; upper limit: the blue interrupted horizontal line) are shown. For reference, zero SII difference is shown as a black dotted line
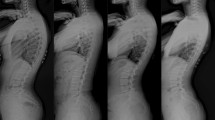
Representative images of chemical shift MR imaging in different MR systems. (a) in-phase image acquired at 3.0 T Siemens MR system; (b) out-of-phase image acquired at 3.0 T Siemens MR system; (c) in-phase image acquired at 1.5 T GE MR system; (d) out-of-phase image acquired at 1.5 T GE MR system; (e) in-phase image acquired at 1.5 T Toshiba MR system; (f) out-of-phase image acquired at 1.5 T Toshiba MR system
Comparison of mean SII values with three vendors in Two field strengths
The mean SII values of all lumbar vertebrae at 3.0 T Siemens, 1.5 T GE and 1.5 T Toshiba were 70.9 ± 5.4%, 71.3 ± 5.4%, and 71.5 ± 8.2%, respectively. Table 4 and Fig. 3 summarized the comparison of mean SII values with 3 MR systems in different lumbar segments. From the aspect of different field strength of MR systems, there were no significant differences in mean SII values (3.0 T Siemens vs 1.5 T GE, p = 0.337; 3.0 T Siemens vs 1.5 T Toshiba, p = 0.561). From the aspect of the same field strength of different vendors (1.5 T GE vs 1.5 T Toshiba), there were no significant differences in mean SIIs (p = 0.824). Moreover, the mean SII values in the same lumbar segment had no significant differences among the measurement in the three different MR vendors (all p > 0.05, range from 0.26 to 0.95), and the mean SIIs for each MR vendor at different lumbar segments had no significant differences either (all p > 0.05, ranging from 0.17 to 0.88).
Comparison of mean SII values between different MR systems. In each box, horizontal line is the median, boundaries are 25th and 75th percentiles, and whiskers are lowest and highest data points still within a 1.5 interquartile range of the lower and upper quartiles, respectively. The mean SII values in the same lumbar segment had no significant differences in three different MR vendors
Comparison of mean SII values in different flip angles
The mean SII of lumbar vertebra at 3.0 T Siemens with different flip angles (flip angle = 10, 30, 50, 70°) was 63.7 ± 7.4%, 67.7 ± 7.5%, 69.7 ± 6.0% and 71.0 ± 5.5%, respectively. The mean SII values showed a tendency of increasing with flip angles, and there were significant differences between different flip angles (p < 0.001) although there was no significant difference between the groups of flip angle 50° and 70° (p = 0.116) (Fig. 4, 5).
Graph shows SII values for each flip angle at 3.0 T Siemens MR scanner. In each box, horizontal line is the median, boundaries are 25th and 75th percentiles, straight line (bar) on each box is the range of data distribution and empty circles represent outliers (value > 1.5 box length from the 75th and 25th percentile). **: p < 0.01; ***: p < 0.001
Representative images of chemical shift MR imaging in different flip angles (FA, flip angle). (a) in-phase and opposed-phase images acquired when flip angle = 10°; (b) in-phase and opposed-phase images acquired when flip angle = 30°; (c) in-phase and opposed-phase images acquired when flip angle = 50°; (d) in-phase and opposed-phase images acquired when flip angle = 70°
Discussion
Chemical shift imaging is an useful technology in abdominal imaging by detecting lipid content [1, 3, 22, 26]. It was initially introduced for the assessment of bone marrow in 1985 by Wismer et al. [27], and also has been widely used in musculoskeletal imaging by measuring SII value for evaluation of bone marrow fat content or differentiation benign from malignant lesions [8, 9, 11–14]. But the lack of standardization in data analysis is a major challenge to the widespread and uniform use of chemical shift MR imaging in musculoskeletal imaging when comparing results of different studies. Furthermore, a reliable interpretation of the results contributed by different centers requires comparability of data acquired with MR systems at different institutions, which are often from different vendors and are operated at different field strengths. To the best of our knowledge, there are no previous reports describing the repeatability of SII measurements in different vendors, field strengths and flip angles.
In the present study, inter- and intraobserver correlation coefficients were good when measuring SII values with different MR systems (all ICC > 0.75), which indicates an excellent repeatability. Further study demonstrated that the mutual agreement of three MR systems was satisfying as the mean differences were very small and most of the data points lied within 95% LOA. Considering that imaging parameters are typically optimized for signal-to-noise ratio (SNR) and/or scan time, a given protocol may induce significant T1-weighting bias in the fat fraction estimate [18]. Our study has also shown that the bias was not systematic but depended on specific lumbar segments and on the different MR systems.
The mean SII values measured in our study for different lumbar segments lied within the previously reported range for all three vendors and for both field strength [15], but the mean SII values were slightly higher than the literature reported, which probably resulted from the effects of T1-weighting amplification induced by the high flip angle in our study. For the same field strength of different MR vendors, we did not find a significant difference in mean SII values in any of the evaluated lumbar segments. Furthermore, the agreement of mean SII values in the same field strength was better than different field strengths. All of these pointed to the conclusion that quantitative analysis for lumbar fat content with chemical shift imaging in different MR vendors of the same field strength is comparable.
With the improvements in MR technology, the theoretical advantage of an increased SNR provided by the higher field strength is paralleled by disadvantages and challenges [19, 22]. Moreover, there exists fundamental differences in the MR physics of 3.0- and 1.5-T MR systems. As a result, chemical shift MR imaging at 1.5 T cannot be applied to 3.0 T MR imaging [19]. Thus, the repeatability of different field strengths is necessary to be researched. In this context, we found no significant difference in mean SII values with 1.5- and 3.0-T MR systems, and the repeatability of mean SII values in different field strength were good. Although the literature had reported that there were two factors influencing SI loss on OP images: chemical shift effect and susceptibility effect (i.e. T2* decay), and susceptibility effect occurred due to field strength inhomogeneity which was stronger at 3.0 T than at lower field strength [18, 19, 28], the results in our study indicated that quantitative analysis for lumbar fat content with chemical shift imaging in different field strengths MR systems may be comparable. Sebastian et al. had investigated the SII at 3.0- and 1.5-T MR imaging for prospectively quantitative analysis in a phantom study, and the result was similar to what we obtained.
In theory, the SI loss on OP images should be sensitive to differences in T1 relaxation, except for chemical shift effect and susceptibility effect [19]. With a poor choice of TE, susceptibility artifact on an OP image acquired later than an IP images can occur and may lead to the misinterpretation of a malignant adrenal lesion as a benign adenoma [22]. As a result, there were several studies focusing on effect of echo time in chemical shift MR imaging, but little or none literatures discuss the effects of T1 relaxation, which introduces a dependence on imaging parameters such as flip angle. In our current study, we did find no significant difference between the group of flip angle 50° versus 70° while there were significant differences between other groups. Moreover, the mean SII values increased with the augment of flip angle. The reason may be that a low flip angle could decrease the SNR leading to a bias in measuring SII and smaller estimates, and/or that due to the shorter T1 of fat, a low flip angle would influence full T1 recovery and make the ratio TE/TR changed.
The result of our study indicated that chemical shit MR imaging might be applicable as a biomarker in the lumbar spine, even in multicenter studies combining different vendors and different field strengths. For instance, studies that focus on treatment-induced SII value differences can be performed with any combination of MR systems. Ongoing research could focus on providing correction factors for intervendor or interfiled strength comparisons or further optimizations of SNR to reduce overall test-retest variability.
Our study still have some limitations. Firstly, we included healthy volunteers instead of a phantom for measurements. But we aimed to simulate a clinical environment similar to clinical practice for our analysis. Secondly, we did not evaluate the reproducibility in subjects with pathology to make meaningful comparisons. A large number of patients with different diseases in various vertebrae or organs would be necessary. However, it may be difficult to acquire a large number of patients with the disease who would be willing to undergo three repeated measurements. Thirdly, subjected to the limited conditions, we did not strictly compare mean SII values between different filed strength at the same vendor. A next multicenter study will be performed to refine our research. Lastly, as SIIs measured in chemical shift MR imaging are not quantitative, quantitative MR measurement including T1 and T2 relaxation times, such as a proton density fat fraction (PDFF) should be intended in our further research.
Conclusion
In conclusion, the signal index (SII) using chemical shift MR imaging may be comparable between MR systems from different vendors and at different field strengths. In addition, high flip angles (50° or 70°) showed better stability for quantitative analysis of lumbar fat content, indicating that high flip angles should be chosen when other parameters are fixed.
Abbreviations
- FA:
-
Flip angle
- ICC:
-
Interclass correlation coefficients
- IP:
-
In phase
- LOA:
-
limits of agreement
- MRI:
-
Magnetic resonance imaging
- OP:
-
Out of phase
- PDFF:
-
Proton density fat fraction
- SII:
-
Signal intensity index
- SNR:
-
Signal-to-noise ratio
- STIR:
-
Short inversion time inversion-recovery
- TR:
-
Repetition time
References
Savci G, Yazici Z, Sahin N, Akgoz S, Tuncel E. Value of chemical shift subtraction MRI in characterization of adrenal masses. AJR Am J Roentgenol. 2006;186(1):130–5.
Chang JS, Taouli B, Salibi N, Hecht EM, Chin DG, Lee VS. Opposed-phase MRI for fat quantification in fat-water phantoms with 1H MR spectroscopy to resolve ambiguity of fat or water dominance. AJR Am J Roentgenol. 2006;187(1):W103–106.
Haider MA, Ghai S, Jhaveri K, Lockwood G. Chemical shift MR imaging of hyperattenuating (>10 HU) adrenal masses: does it still have a role? Radiology. 2004;231(3):711–6.
Kohl CA, Chivers FS, Lorans R, Roberts CC, Kransdorf MJ. Accuracy of chemical shift MR imaging in diagnosing indeterminate bone marrow lesions in the pelvis: review of a single institution's experience. Skeletal Radiol. 2014;43(8):1079–84.
Wang X, Hernando D, Reeder SB. Sensitivity of chemical shift-encoded fat quantification to calibration of fat MR spectrum. Magn Reson Med. 2016;75(2):845–51.
Priola AM, Priola SM, Ciccone G, Evangelista A, Cataldi A, Gned D, Paze F, Ducco L, Moretti F, Brundu M, et al. Differentiation of rebound and lymphoid thymic hyperplasia from anterior mediastinal tumors with dual-echo chemical-shift MR imaging in adulthood: reliability of the chemical-shift ratio and signal intensity index. Radiology. 2015;274(1):238–49.
Tsushima Y, Ishizaka H, Matsumoto M. Adrenal masses: differentiation with chemical shift, fast low-angle shot MR imaging. Radiology. 1993;186(3):705–9.
Del Grande F, Santini F, Herzka DA, Aro MR, Dean CW, Gold GE, Carrino JA. Fat-suppression techniques for 3-T MR imaging of the musculoskeletal system. Radiographics. 2014;34(1):217–33.
Gokalp G, Mutlu FS, Yazici Z, Yildirim N. Evaluation of vertebral bone marrow fat content by chemical-shift MRI in osteoporosis. Skeletal Radiol. 2011;40(5):577–85.
Gokalp G, Yildirim N, Yazici Z, Ercan I. Using chemical-shift MR imaging to quantify fatty degeneration within supraspinatus muscle due to supraspinatus tendon injuries. Skeletal Radiol. 2010;39(12):1211–7.
Kransdorf MJ, Bridges MD. Current developments and recent advances in musculoskeletal tumor imaging. Semin Musculoskelet Radiol. 2013;17(2):145–55.
Liney GP, Bernard CP, Manton DJ, Turnbull LW, Langton CM. Age, gender, and skeletal variation in bone marrow composition: a preliminary study at 3.0 Tesla. J Magn Reson Imaging. 2007;26(3):787–93.
Ragab Y, Emad Y, Gheita T, Mansour M, Abou-Zeid A, Ferrari S, Rasker JJ. Differentiation of osteoporotic and neoplastic vertebral fractures by chemical shift {in-phase and out-of phase} MR imaging. Eur J Radiol. 2009;72(1):125–33.
Regis-Arnaud A, Guiu B, Walker PM, Krause D, Ricolfi F, Ben Salem D. Bone marrow fat quantification of osteoporotic vertebral compression fractures: comparison of multi-voxel proton MR spectroscopy and chemical-shift gradient-echo MR imaging. Acta Radiol. 2011;52(9):1032–6.
Zajick Jr DC, Morrison WB, Schweitzer ME, Parellada JA, Carrino JA. Benign and malignant processes: normal values and differentiation with chemical shift MR imaging in vertebral marrow. Radiology. 2005;237(2):590–6.
Zampa V, Cosottini M, Michelassi C, Ortori S, Bruschini L, Bartolozzi C. Value of opposed-phase gradient-echo technique in distinguishing between benign and malignant vertebral lesions. Eur Radiol. 2002;12(7):1811–8.
Fujiyoshi F, Nakajo M, Fukukura Y, Tsuchimochi S. Characterization of adrenal tumors by chemical shift fast low-angle shot MR imaging: comparison of four methods of quantitative evaluation. AJR Am J Roentgenol. 2003;180(6):1649–57.
Bydder M, Yokoo T, Hamilton G, Middleton MS, Chavez AD, Schwimmer JB, Lavine JE, Sirlin CB. Relaxation effects in the quantification of fat using gradient echo imaging. Magn Reson Imaging. 2008;26(3):347–59.
Del Grande F, Subhawong T, Flammang A, Fayad LM. Chemical shift imaging at 3 Tesla: effect of echo time on assessing bone marrow abnormalities. Skeletal Radiol. 2014;43(8):1139–47.
Kuhn JP, Jahn C, Hernando D, Siegmund W, Hadlich S, Mayerle J, Pfannmoller J, Langner S, Reeder S. T1 bias in chemical shift-encoded liver fat-fraction: role of the flip angle. J Magn Reson Imaging. 2014;40(4):875–83.
Disler DG, McCauley TR, Ratner LM, Kesack CD, Cooper JA. In-phase and out-of-phase MR imaging of bone marrow: prediction of neoplasia based on the detection of coexistent fat and water. AJR Am J Roentgenol. 1997;169(5):1439–47.
Schindera ST, Soher BJ, Delong DM, Dale BM, Merkle EM. Effect of echo time pair selection on quantitative analysis for adrenal tumor characterization with in-phase and opposed-phase MR imaging: initial experience. Radiology. 2008;248(1):140–7.
Busing KA, Kilian AK, Schaible T, Debus A, Weiss C, Neff KW. Reliability and validity of MR image lung volume measurement in fetuses with congenital diaphragmatic hernia and in vitro lung models. Radiology. 2008;246(2):553–61.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet (London, England). 1986;1(8476):307–10.
Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8(2):135–60.
Fishbein MH, Gardner KG, Potter CJ, Schmalbrock P, Smith MA. Introduction of fast MR imaging in the assessment of hepatic steatosis. Magn Reson Imaging. 1997;15(3):287–93.
Wismer GL, Rosen BR, Buxton R, Stark DD, Brady TJ. Chemical shift imaging of bone marrow: preliminary experience. AJR Am J Roentgenol. 1985;145(5):1031–7.
Wu RH, Ducreux D, Crawley A, Lin R, Kong KM, Guo G, Luo XT, Lang ZJ, Terbrugge K, Mikulis DJ. Improving spatial signal homogeneity in MR 2D chemical shift imaging using outer volume saturation bands. Conf Proc IEEE Eng Med Biol Soc. 2004;2:1084–7.
Acknowledgements
None.
Funding
None.
Availability of data and materials
Due to statutory provisions regarding data- and privacy protection, the dataset supporting the conclusions of this article is available upon individual request directed to the corresponding author.
Authors’ contributions
ZX and JL participated in the design of the study, performed the experiments and the statistical analysis and drafted the manuscript. DC participated in the design of the study, performed the experiments and the statistical analysis. YZ participated in the design of the study and assisted with manuscript preparation. CL participated in the design of the study and assisted with manuscript preparation. DS assisted with manuscript preparation. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The protocols were reviewed and approved by the Ethics Committee of our University Hospital and was conducted in accordance with the Declaration of Helsinki. All patients gave written informed consent to participate in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Xiao, Z., Li, J., Li, C. et al. Chemical shift MR imaging in the lumbar vertebra: the effect of field strength, scanner vendors and flip angles in repeatability of signal intensity index measurement. BMC Med Imaging 16, 64 (2016). https://doi.org/10.1186/s12880-016-0167-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12880-016-0167-3