Abstract
Background
Healthcare workers (HCWs) are at a higher risk of contracting COVID-19 due to their close contact with infected patients. However, the true burden of COVID-19 among HCWs in Yemen is unknown due to the inadequate availability of healthcare and the subclinical nature of the disease. This study aims to estimate the seroprevalence of SARS-CoV-2 infection among HCWs in two Yemeni governorates and identify associated factors using a cross-sectional design.
Method
A total of 404 HCWs were surveyed from June 2022 to September 2022 in Lahj and AL-Dhalea hospitals. A self-administered questionnaire collected demographic data, COVID-19 infection history, and vaccination status. A total of 404 human sera were tested using a specific electrochemiluminescence immunoassay assay. Association analysis was conducted to identify associations between antibody prevalence and demographic and vaccine-related variables.
Result
The median age of the HCWs was 31 (Range 20–64) years, with 65.0% being male and 35.0% female. Of all HCWs, 94% were SARS-CoV-2 seropositive and 77.0% had no confirmed test of COVID-19-related symptoms. There was no significant association between seropositivity and demographic factors such as age, gender, occupation, or COVID-19 vaccination (P > 0.05).
Conclusion
The seroprevalence of SARS-CoV-2 was high among HCWs in Yemen, primarily due to natural infection rather than vaccination. Compliance with infection prevention and control measures did not significantly affect seropositivity. This study highlights the need for improved healthcare systems and resources to reduce the burden of COVID-19 and promote infection prevention and control (IPC) measures among HCWs in Yemen.
Similar content being viewed by others
Introduction
The coronavirus diseases-19 (COVID-19) pandemic has rapidly spread across the world, with devastating effects on public health, economies, and societies. With its five consecutive waves of infection, it resulted in over 693 million confirmed cases and 6.9 million deaths as of August 14, 2023 [1]. In response, countries implemented several measures, including lockdowns, social distancing, and travel restrictions, while awaiting the development of vaccines, which have now been administered to millions of people worldwide [2].
Based on the guidelines of the World Health Organization (WHO), several hospitals commenced their strict implementation of strategies to protect their HCWs. These included providing adequate personal protective equipment (PPE), implementing infection prevention and control (IPC) measures, and regular screening of staff [3, 4]. Despite measures to protect healthcare workers, the burden of COVID-19 infections among them remained high [5, 6]. Therefore, the protection of HCWs requires both the application of the hierarchy of controls for IPC in healthcare settings and public health measures aimed at reducing COVID-19 transmission [7, 8]. HCWs face increased patient volumes and longer shifts, leading to exhaustion, burnout, and physical and mental stress, which puts them at risk of non-compliance with recommended infection prevention and control measures. Serological assays for SARS-CoV-2 have shown variable seroprevalence among HCWs, reflecting differences in time and region [9]. The findings of this assay based on detecting antibodies from prior exposure to the virus whether due to asymptomatic infection or an overt COVID-19.
Over the first three years of the pandemic variable seroprevalence among HCWs have been reported worldwide with different epidemiological models related to person-place and time. In early studies of the pandemic mainly in the year 2020, a COVID-19 seroprevalence of 14.8% was reported among HCWs in Saudi Arabia [10], 19% in Turkey [11], 25.6% in Egypt [12], 27% in New York City [13], 42.7% in Poland [14], 45% in Nigeria, [15], and 48% in Ethiopian [16]. As of late 2021, higher seroprevalence was reported among HCWs as it reached 89.3% in Hong Kong [17], and 94.5% in Delhi India [18]. This progressive increase of seroprevalence with time suggests an expansion of seropositivity rates although the extent, effectiveness, and role of this seropositivity in immunity to infection remained to be resolved. However, the available evidence is that the vaccine induced immunity seems to have played a part in at least reducing the disease severity. Uncertainty and underestimation of the true number of cases in many countries may be due to insufficient testing of all suspected cases [19]. Given all this, the HCW working in the frontline of healthcare settings would be highly exposed to COVID-19 during the different waves of the pandemic.
Yemen reported its first COVID-19 case on April 28, 2020, with over 11,000 infections and 2,159 deaths reported to date [8, 20]. Despite the low global case fatality (1.0%), COVID-19 case fatality rate in Yemen reached as high as is 22.6% [20]. The high case fatality rate in Yemen suggests that the actual number of cases and deaths may be much higher than official figures, and underreporting remains a concern due to the multitude of challenges Yemen still facing, including the political instability, conflict, and humanitarian crisis an well as lack of developing reliable epidemiological surveillance and reporting system [20, 21].
In mid-2020 COVID-19 cases in Yemen were estimated to have reached 1 million and this figure was predicted to reach 11 million with 85,000 deaths at the end of the year 2020 if people do not make serious behavioural changes, and if authorities do not introduce more mitigation to control the infection [22, 23]. However, according to the WHO reports from April 2020 to 13 January 2023, there have been 11,945 confirmed cases of COVID-19 with 2,159 deaths [23]. These figures indicate underreporting and thus uncertainty about the actual epidemic status of COVID-19 in the country. The political conflict left Yemen with many challenges to develop reliable epidemiological reports on the actual COVID-19 status due to inadequacy of epidemiological surveillance, lack of laboratory capacity and absence of community cooperation with the epidemiological surveillance teams. However, a study conducted among HCWs in Yemen during the COVID-19 pandemic illustrated that healthcare system capability and general preparedness to face COVID-19 was rated as very poor or poor by the majority of HCWs who participated in the study [24]. This is consistent with international reports, which show that Yemen's healthcare system is fragile and has limited capacity to cope with public health emergencies [25].
The situation among frontline teams in Yemen has not been fully assessed as yet. Thus, this study aims to investigate the seroprevalence of SARS-CoV-2 infection among health care workers (HCWs) in hospitals of two Yemeni governorates and identify associated factors.
Methods
Study design and setting, and study population
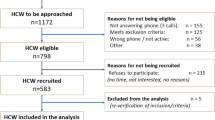
This is a cross-sectional study conducted in the hospitals located of Lahj and AL-Dhalea governorates in the southern part of Yemen in the period from June 2022 to September 2022 (Map of Yemen identifying the study areas). Lahj governorate, with a population of nearly 900,000 people, is located northwest of major southern city of Aden and is divided into 15 administrative districts with the city of Al-Hawtah as its capital. Al-Dhalea governorate, with a population of almost 500,000 people, is located in the southern-central part of Yemen with a population of nearly 500,000 people and encompasses nine administrative districts, with Al-Dhalea as its capital, [26] as seen in Fig. 1 [27].
The study population included a range of HCWs, such as doctors, nurses, x-ray physicians, dentists, laboratory personnel, pharmacists, respiratory therapists, and nutritionists, in addition to auxiliary HCWs such as clerks, housekeeping staff, laundry personnel, and social workers. Those who didn't agree to participate in the study and did not fill in the questionnaire were excluded with around 12 out of the total 416 (2.9%). However, participants were gathered into four categories according to the importance of the participants and the level of contact with patients complaining of COVID-19 infection such as physicians, nurses, allied health workers who involved in giving healthcare services distinct from medicine or nursing [28], and finally those categorized as support services, as people responsible for providing and maintaining a sanitary and therapeutic environment in which health care can be appropriately delivered to individuals [29]. Therefore, allied health workers included those working in the x-ray department, laboratory, and pharmacy accounting around 92 workers (22.8%). While those working in supporting services section such as cleaning and laundry personnel, maintenance, admission/reception clerks, patient transporters social workers, and housekeeping with a total of 58 participants (14.4%).
To recruit the participants, the research team obtained permission from the hospital administration in each governorate to conduct the study [30], as well as the work was approved by the Ethics Research Committee (ERC) of the Faculty of Medicine and Health Sciences, University of Aden (REC-#119–2022). An informed consent was given to the participants and the study team provided a brief overview of the study objectives to potential participants and requested their voluntary participation. Those who agreed to participate were asked to complete a self-administered questionnaire and provide a blood sample for serological testing. The questionnaire collected information on demographic characteristics, work-related factors, COVID-19-related symptoms, and exposure to COVID-19 patients or suspected cases.
Sampling and sampling technique
The prevalence of anti-SARS-CoV-2 antibodies among healthcare workers in Yemen is not well understood, so a large sample size was needed to estimate it accurately. Based on an assumed prevalence rate of 50%, a 95% confidence interval, and a 5% margin of error, a sample size of 384 was calculated using Daniel’s equation [31]. To account for possible missing data or participant dropouts, an additional 5% of the sample size was added, resulting in a final sample size of 404 HCWs.
To ensure a representative sample, we used the Probability Proportional to Size (PPS) sampling technique to enroll participants from both Lahj and Al-Dhalea governorates proportionally. Of the HCWs who presented in the hospitals during the sampling period, 267 (66%) from Lahj and 137 (34%) from Al-Dhalea were enrolled in the sample and a convenience sampling method was used to complete the required sample from each hospital and governorate.
Data collection
The study used a self-reported questionnaire based on the WHO protocol for COVID-19 infection among HCWs in a healthcare setting [4]. The HCWs completed the questionnaire in front of the investigator for any assistance needed by the participant and before the collection of the blood sample (8–12 min average). The questionnaire comprised of five domains, including demographic data, data related to exposure to COVID-19, COVID-19 symptoms and PCR confirmed or suspected infection, comorbidities, IPC measures, and COVID-19 vaccination. The first domain encompassed the demographic data including age, sex, healthcare setting, work experience, and occupation category. The second domain included data related to exposures to COVID-19 and these consisted of the frequency of exposure, time of occurrence, and the setting as a source of infection. The third domain comprised COVID-19 symptoms and PCR confirmed or suspected infection. The fourth domain consisted of data of comorbidities encompassing asthma, heart disease, hypertension, kidney disease, diabetes mellitus, and immune deficiency. The fifth domain encompassed data on IPC measures which included follow IPC standard precautions, following 5 recommended moments, use alcohol-based hand rub or soap, wear PPE with the COVID-19 patient, PPE available in sufficient quantity, and attended IPC training. In addition, this domain includes variables related to COVID-19 vaccination which included receiving of vaccine, acceptance, or hesitancy to receive the vaccine.
The questionnaire was originally in English and was translated into Arabic for ease of understanding and back to English to secure the consistency of the questions.
Pre-testing
Reliability test was undertaken among 30 HCWs in analogy to the site of the study to ensured that the questionnaire was easy to use and acceptable by the interviewees. Reliability also was considered by reaching a Cronbach alpha of not less than 0.73 of the completed questionnaires which indicates that the overall response values for each participant across a set of questions are consistent.
Laboratory investigation
A volume of five ml venepuncture blood sample was drawn from each participant via the venipuncture technique with universal precautions conducted by the concerned technician. Blood samples were collected in EDTA tubes and stored at 4 °C and transferred on the same day to the hospital laboratory for analysis. The samples were labelled with the department name, name of the participant, date, and identification number [4]. Sera were tested for anti-SARS-CoV-2 using Elecsys Anti-SARS-CoV-2 Qualitative assay for use on the Cobas, Roche Diagnostics GmbH, electrochemiluminescence immunoassay (ECLIA) according to the instructions of the manufacturer. The assay has a sensitivity of 99.81% (CI 95%: 99.6–99.9%) and a specificity of 99.5% (CI 95%: 98.63–99.85%) and is certified by WHO [32, 33]. The assay provides a qualitative detection of all antibody classes (including IgG) to SARS-CoV-2 in human serum and plasma and is intended for use as an aid in identifying individuals with an adaptive immune response to SARS-CoV-2, for recent or prior infection. It can detect the presence of anti-SARS-CoV-2 antibodies in serum within days to weeks following acute infection [34, 35]. Sera with a Cut off Index (COI; signal sample/cut-off, COI) ≥ 1.0 were considered positive, those with a COI < 1.0 were considered negative.
Data management and statistical analysis
The data was coded and entered into SPSS version 23 for analysis. Descriptive statistics, including mean and standard deviation, were used to summarize continuous variables, while absolute and relative frequencies were used for categorical variables. The Chi-square test was used to examine the association between the dependent and the independents variables. A P- of < 0.05 was considered statistically significant.
Results
Of 404 HCW, 264 (65.3%) were male whereas 140 (34.7%) were female, the median age was 31 years (Range 20–64) years. Nurses constituted the highest proportion (51.2%) while physicians comprised the lowest proportion (11.6%). The overall seroprevalence of SARS-CoV-2 was 94.3%; 95%CI = (92.1–96.5%). Seroprevalence was similarly high and did not significantly differ (P > 0.05) between; genders, age groups, work experience, different occupation categories (Table 1). No significant association (P > 0.05) between the seroprevalence and the reported risk factors such as smoking, comorbidities including, cardiovascular diseases, history of diabetes mellitus, or renal diseases with a reported history of COVID-19 (Fig. 2). Further, seroprevalence was similarly high and did not differ significantly (P > 0.05) between different governorates, districts, hospitals (Table 2), those who did or did not adhere to IPC measures recommended by the WHO and those who attended and who did not attend IPC training course (Table 3). There was a convergently high seroprevalence (≥ 90.0%) which did not differ significantly (P > 0.05) among HCW who reported or denied history of COVID-19, breathing difficulty, cough, anosmia or loss of taste or fever/ chills, (Table 4), positive or negative history of close contact with confirmed COVID- 19 cases or with overt COVID-19 (Table 5). Among those who reported previous history of COVID-19 (n = 112) only 22 i.e., 5.4% of total HCW reported that they were tested by PCR and were all positive. Among all HCWs, 12.0% received one vaccine dose, 11.5% received two doses’, 76.5% have not received any vaccine. Of all HCWs 95 (23.5%) were vaccinated, 66 (70%) with AstraZeneca vaccine and 29 (30%) with Jenson & Jenson/Osinovac. More than half of the HCWs (58.9%) reported lack of desire to receive COVID-19 vaccine, while 9.9% will think too carefully before they take it. Equally high seroprevalence (> 93.0%) was not significantly (P > 0.05) associated with vaccine uptake, vaccine type or number of vaccine doses (Table 5).
Discussion
Our study found a significantly high seroprevalence rate of SARS-CoV-2 (94.3%) among HCWs in Yemen between June 2022 and the end of September 2022, after the peak of the COVID-19 epidemic in the country [36]. This is a significant increase compared to a previous study conducted during the first peak of the pandemic in the southern city of Aden between November and December 2020, which reported a seroprevalence rate of 27.5% [21]. Earlier during the pandemic, another study among general population which was conducted between June 2020 through January 2021 in the capital Sana’a, Yemen, showed 51.4% seroprevalence among COVID-19 suspected patients [37]. The high seroprevalence among HCW in this study reflects the reality that HCWs are at a high-risk of acquiring SARS-CoV-2 infection given their direct role in patient care [38]. This is in line with reports from Saudi Arabia where seroprevalence among HCW in December 2020 was 10-folds higher (26.5%) than that among general population (2.36%) in May 2020 [39, 40]. Another study from South Africa (Gauteng Province), illustrated a period prevalence of SARS-CoV-2 infections ranged from 6.1% to 15.4% for the period 1 June—31 August 2020 [41].
Due to the political status in Yemen, epidemiological containment measures were inadequately implemented in the country. In fact, this study reported a lack of PPE in around 80.0% of HCWs despite reporting a high level of compliance with other IPC measures. The lack of PPE made compliance with other IPC measures ineffective, and this was translated into a seroprevalence that is as high as that among those reported non-compliance. This favours to some extent the inference of double exposure of HCW which occurred within and outside the health care setting in the community where poor containment measures were practiced. All these factors and others such as poor financial resources likely accelerated the spread of the virus among the HCWs and ultimately increased the pressure on the healthcare settings that lacked access to appropriate PPE and practiced limited compliance to IPC measures and ultimately intensely exposed HCWs to infection [24].
The scenario of exposure outside the health care setting is more likely to have occurred as the seroprevalence among auxiliary HCW such as clerks, housekeeping staff, laundry personnel, and social workers who literally has less contact with patients was as high as 96%.
The present study did not find a significant difference in seropositivity between HCWs who received the COVID-19 vaccine and those who did not. This is, realistically, due to the fact that the assay used in this study only detects anti-nucleocapsid antibodies [32, 33] while the existing COVID-19 vaccines only use the spike antigen. It is worth noting that the vaccination coverage with COVID-19 vaccine in Yemen is extremely low, as of 2 January 2023, a total of 1,242,982 vaccine doses have been administered in a country of 32 million population. The high seropositivity in our present study is likely due to natural infection rather than vaccination. It is reasonable to expect that the HCW could have produced anti-spike antibodies in even a higher proportion, as other studies reported that higher non-severe COVID-19 patients seroconverted to anti-spike antibodies than anti-nucleocapsid antibodies which declined more rapidly compared to anti-spike antibodies [38, 42].
Therefore, given the nature of the assay used in this study as it only detects anti-nucleocapsid antibodies [32, 33] this assay may have underestimated the actual seroprevalence and thus a higher proportion of the HCWs may have produced more durable anti-spik antibodies than anti-nucleocapsid. This suggests the existence of a higher SARS-CoV-2 seroprevalence among general population albite somewhat lower than that existing among HCWs although the immune role of the produced antibodies in term of durability and the efficacy remains to be elucidated.
The high proportion of HCW who reported either unacceptance or hesitancy to take the COVI-19 vaccine highlights a concerning misconception that is likely to be prevalent among the general population. This will be a major barrier towards development of efficient COVID-19 vaccination program.
Our study found no significant association (P > 0.05) between seroprevalence and gender, age, residence, professional work experience, occupation categories and workplace. This suggests that all HCWs were equally at the same level of risk. These results are consistent with previous studies conducted elsewhere [14, 18, 21]. The absence of significant association between seropositivity and chronic comorbidities and tobacco consumption is in agreement with a study among HCWs elsewhere [43]. The high rate (28.0%) of seropositive HCWs who had never been diagnosed with COVID-19 in the past or those who were asymptomatic (72.0%) infers that a considerable proportion HCWs had subclinical infections and had been carrying out their clinical practice while infected and thus spreading the infection among their patients and among other health personnels. Other findings reported elsewhere suggest a similar scenario [44] which further emphasize the necessity of promotion of IPC measures.
A small number of HCWs with a history of COVID-19 reported undergoing PCR testing to confirm their infection. This points to inadequate adherence to local and international policies regarding testing suspected COVID-19 cases particularly for HCWs, possibly due to fear of stigma, isolation, feel as it was unnecessary, and a shortage of tests supplies, as reported in any other studies [45, 46].
Seroprevalence did not significantly associate with COVID-19-related symptoms including, shortness of breathing, cough, anosmia or loss of taste, and fever/chills. Similar finding have been reported from Saudi Arabia where a sizable proportion of seropositive HCW had not been previously diagnosed with COVID-19 [47].
Strengths and limitations
The study has the merit of being the first to estimate the seroprevalence of SARS-CoV-2 among HCWs in a minor governorate in Yemen, two years after the start of the pandemic and at the fifth wave. This study showed a significant value as it provides insights into the epidemiological status of COVID-19 and its burden in Yemen.
However, the generalizability of the findings is limited as the study was conducted in only two governorates out of a total 22 in the country. Additionally, the used serological test was only qualitative rather than quantitative, so it does not determine the quantitative value or the rate of the increased levels of antibodies to SARS-CoV-2. Furthermore, there might be several potential sources of bias, including information recall bias on reporting of previous infection with SARS-CoV-2, the use of PPE, and attending IPC training as well as limitation related to the self-completeness of the questionnaire (ignorance of questions, or different interpretations of the question). Finally, the study did not assess antibodies from vaccination, particularly anti-spike, which is an important limitation.
Conclusions
The study findings highlight the urgent need for improving infection prevention and control measures among HCWs in Yemen, as well as increasing vaccination coverage. The high seroprevalence among HCWs may also suggest a high level of seroprevalence among the general population, emphasizing the importance of continued surveillance and monitoring of the epidemiological situation in Yemen.
SARS-CoV-2 seroprevalence and its impact on the clinical outcomes of infection in term of severity and duration in HCW need to be regularly monitored. Vaccination campaigns should be enhanced according to the WHO current recommendation and assessment of the vaccine. In summary, this study highlights the high burden of SARS-CoV-2 infection among HCWs in Yemen and underscores the need for urgent action to improve infection prevention and control measures and increase vaccination coverage to protect HCWs and prevent the further spread of the virus.
Availability of data and materials
The data that support the study findings of the current study are available from the corresponding author on reasonable request via this email: bawazir56@gmail.com.
References
WHO. Coronavirus (COVID-19) Dashboard: World Health Organization; 2023. Available from: https://covid19.who.int/.
Wilson N, Baker MG, Eichner M. Estimating the impact of control measures to prevent outbreaks of COVID-19 associated with air travel into a COVID-19-free country: a simulation modelling study. medRxiv. 2020. https://doi.org/10.1038/s41598-021-89807-y.
Al-Tawfiq JA, Garout MA, Gautret P. Preparing for emerging respiratory pathogens such as SARS-CoV, MERS-CoV, and SARS-CoV-2. Infez Med. 2020;28(suppl 1):64–70.
WHO. Protocol for assessment of potential risk factors for 2019-novel coronavirus (2019-nCoV) infection among health care workers in a health care setting. 2020.
Barranco R, Ventura F. Covid-19 and infection in health-care workers: an emerging problem. Medico-Legal J. 2020;88(2):65–6. https://doi.org/10.1177/0025817220923694.
Wei X-S, Wang X-R, Zhang J-C, Yang W-B, Ma W-L, Yang B-H, et al. A cluster of health care workers with COVID-19 pneumonia caused by SARS-CoV-2. J Microbiol Immunol Infect. 2021;54(1):54–60. https://doi.org/10.1016/j.jmii.2020.04.013.
Ontario PH. Interim IPAC Recommendations for Use of Personal Protective Equipment for Care of Individuals with Suspect or Confirmed COVID‑19. 2021. Available from: https://www.publichealthontario.ca/-/media/documents/ncov/updated-ipac-measures-covid-19.pdf?la=en .
WHO. Health workers exposure risk assessment and management in the context of COVID-19 virus: interim guidance, 4 March 2020. Geneva: World Health Organization; 2020. Contract No.: WHO/2019-nCov/HCW_risk_assessment/2020.1]. Available from: https://apps.who.int/iris/handle/10665/331340.
WHO. Infection prevention and control during health care when coronavirus disease (COVID-19) is suspected or confirmed: interim guidance, 12 July 2021. World Health Organization; 2021.]. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC-2021.1.
Alroqi F, Masuadi E, Alabdan L, Nogoud M, Aljedaie M, Abu-Jaffal AS, et al. Seroprevalence of SARS-CoV-2 among high-risk healthcare workers in a MERS-CoV endemic area. J Infect Public Health. 2021;14(9):1268–73. https://doi.org/10.1016/j.jiph.2021.08.029.
Sonmezer MC, Erul E, Sahin TK, Rudvan Al I, Cosgun Y, Korukluoglu G, et al. Seroprevalence of SARS-CoV-2 antibodies and associated factors in healthcare workers before the era of vaccination at a tertiary care hospital in Turkey. Vaccines. 2022;10(2):258. https://doi.org/10.1016/j.jhin.2020.11.008.
Musa S, Alem SA, Amer K, Elnagdy T, Hassan WA, Ali MA, et al. Prevalence of SARS-CoV-2 infection and dynamics of antibodies response among previously undiagnosed healthcare workers in a university hospital: a prospective cohort study. J Infect Public Health. 2021;14:1466–73. https://doi.org/10.1016/j.jiph.2021.06.001.
Venugopal U, Jilani N, Rabah S, Shariff MA, Jawed M, Batres AM, et al. SARS-CoV-2 seroprevalence among health care workers in a New York City hospital: A cross-sectional analysis during the COVID-19 pandemic. Int J Infect Dis. 2021;102:63–9. https://doi.org/10.1016/j.ijid.2020.10.036.
Żółtowska B, Barańska I, Jachowicz E, Sydor W, Maziarz B, Mydel K, et al. The Seroprevalence of SARS-CoV-2 Antibodies among HealthCare Workers in University Hospital in Krakow before the Era of Vaccination. Int J Environ Res Public Health. 2022;19(7):4044. https://doi.org/10.3390/ijerph19074044.
Olayanju O, Bamidele O, Edem F, Eseile B, Amoo A, Nwaokenye J, et al. SARS-CoV-2 seropositivity in asymptomatic frontline health workers in Ibadan, Nigeria. Am J Tropl Med Hyg. 2021;104(1):91. https://doi.org/10.4269/ajtmh.20-1235.
Gelanew T, Seyoum B, Mulu A, Mihret A, Abebe M, Wassie L, et al. High seroprevalence of anti-SARS-CoV-2 antibodies among Ethiopian healthcare workers. BMC Infect Dis. 2022;22(1):1–9. https://doi.org/10.1186/s12879-022-07247-z.
Poon RW-S, Chan BP-C, Chan W-M, Fong CH-Y, Zhang X, Lu L, et al. SARS-CoV-2 IgG seropositivity after the severe Omicron wave of COVID-19 in Hong Kong. Emerg Microbes Infect. 2022;11(1):2116–9. https://doi.org/10.1080/22221751.2022.2106899.
Sharma P, Gupta E, Basu S, Agarwal R, Mishra S, Kale P, et al. Neutralizing antibody responses to SARS-CoV-2: A population based seroepidemiological analysis. Indian J Med Microbiol. 2022. https://doi.org/10.1101/2021.12.28.21268472.
Gupta M, Wahl B, Adhikari B, Bar-Zeev N, Bhandari S, Coria A, et al. The need for COVID-19 research in low-and middle-income countries. Global Health Res Policy. 2020;5(1):1–4. https://doi.org/10.1186/s41256-020-00159-y.
WHO. coronavirus diseases (COVID-19) dashboard. Geneva: World Health Organization 2023. Available from: https://covid19.who.int/region/emro/country/ye.
Bin-Gouth AS, Al-Shoteri S, Mahmoud N, Musani A, Baoom NA, Al-Waleedi AA, et al. SARS-CoV-2 Seroprevalence in Aden, Yemen: a population-based study. Int J Infect Dis. 2022;115:239–44. https://doi.org/10.1016/j.ijid.2021.12.330.
Besson ESK, Norris A, Ghouth ASB, Freemantle T, Alhaffar M, Vazquez Y, et al. Excess mortality during the COVID-19 pandemic: a geospatial and statistical analysis in Aden governorate, Yemen. BMJ Glob Health. 2021;6(3):e004564. https://doi.org/10.1136/bmjgh-2020-004564.
WHO. WHO Health Emergency Dashboard 2022. Available from: https://covid19.who.int/region/emro/country/ye.
Zawiah M, Al-Ashwal FY, Saeed RM, Kubas M, Saeed S, Khan AH, et al. Assessment of healthcare system capabilities and preparedness in Yemen to Confront the novel coronavirus 2019 (COVID-19) outbreak: a perspective of healthcare workers. Front Public Health. 2020;8:419. https://doi.org/10.3389/fpubh.2020.00419.
Dureab F, Hussain T, Sheikh R, Al-Dheeb N, Al-Awlaqi S, Jahn A. Forms of health system fragmentation during conflict: the case of Yemen. Front Public Health. 2021;9:659980. https://doi.org/10.3389/fpubh.2021.659980.
Yemen BFaPDF. Local Governance in Yemen: Resource Hub 2022. Available from: https://yemenlg.org/governorates.
UNHCR. Yemen Administrative Map: United Nations High Commissioner for Refugees; 2020. Available from: https://data.unhcr.org/ar/documents/details/82130.
Turnbull C, Grimmer-Somers K, Kumar S, May E, Law D, Ashworth E. Allied, scientific and complementary health professionals: a new model for Australian allied health. Aust Health Rev. 2009;33(1):27–37. https://doi.org/10.1071/AH090027.
NHS. Support services: National Health Service; 2021. Available from: https://www.healthcareers.nhs.uk/explore-roles/wider-healthcare-team/roles-widerhealthcare-team/support-services.
MOH/Aden. Administrative Permission to assess the investigator to conduct the study Lahej and AlDhalee. Ministry of Health/Aden Branch; 2022.
Dasgupta S, Laplante B, Wang H, Wheeler D. Confronting the environmental Kuznets curve. J Econ Perspect. 2002;16(1):147–68. https://doi.org/10.1257/0895330027157.
WHO. SARS‐CoV‐2 Antibody Tests: progress of the active applications in the emergency use listing assessment pipeline. 2022. Available from: https://extranet.who.int/pqweb/sites/default/files/documents/220203_eul_sars_cov_2_ivds_update.pdf.
Diagnostics R. Elecsys Anti-SARS-CoV-2. 2022. Available from: https://diagnostics.roche.com/global/en/products/params/elecsys-anti-sars-cov-2.html .
CDC. Interim guidelines for COVID-19 antibody testing: Centers for Disease Control and Prevention; 2020. Available from: https://www.cdc.gov/coronavirus/2019-ncov/lab/resources/antibody-tests-guidelines.html.
Hall VJ, Foulkes S, Charlett A, Atti A, Monk EJ, Simmons R, et al. SARS-CoV-2 infection rates of antibody-positive compared with antibody-negative health-care workers in England: a large, multicentre, prospective cohort study (SIREN). Lancet. 2021;397(10283):1459–69. https://doi.org/10.1016/S0140-6736(21)00675-9.
WHO. Coronavirus (COVID‐19) Dashboard. WHO 2022. Available from: https://covid19.who.int/.
A Sallam T, Al-Youssefi M, A Bawazir A. Prevalence and Classes of SARS-CoV-2 Antibodies among COVID-19 Suspected Patients who Attended a Health Care Setting in Sana’a, Yemen. AJI. 2021. https://journalaji.com/index.php/AJI/article/view/63.
El-Raey F, Alboraie M, Youssef N, Yousef A, Abdelmoaty AA, Hassan E, et al. Predictors for severity of SARS-cov-2 infection among healthcare workers. J Multidiscip Healthc. 2021;14:2973.
Amer HA, Abdallah HA, Alkheledan HS, Alzarzour SH, Shrahily A, Tamim H, et al. SARS-CoV-2 antibody prevalence among healthcare workers: A cross-sectional study at a quaternary healthcare center in Saudi Arabia. J Infect Public Health. 2022;15(3):343–8. https://doi.org/10.1016/j.jiph.2022.01.018.
Alserehi HA, Alqunaibet AM, Al-Tawfiq JA, Alharbi NK, Alshukairi AN, Alanazi KH, et al. Seroprevalence of SARS-CoV-2 (COVID-19) among healthcare workers in Saudi Arabia: comparing case and control hospitals. Diagnostic Microbiol Infect Dis. 2021;99(3):115273. https://doi.org/10.1016/j.diagmicrobio.2020.115273.
Mdzinwa N, Voigt M, Van Rensburg CJ, Paruk F. SARS-CoV-2 infection prevalence in healthcare workers and administrative and support staff: The first-wave experience at three academic hospitals in the Tshwane district of Gauteng Province South Africa. S Afr Med J. 2021;111(11):1092–7. https://doi.org/10.7196/SAMJ.2021.v111i11.15938.
Van Elslande J, Oyaert M, Lorent N, Weygaerde YV, Van Pottelbergh G, Godderis L, et al. Lower persistence of anti-nucleocapsid compared to anti-spike antibodies up to one year after SARS-CoV-2 infection. Diagn Microbiol Infect Dis. 2022;103(1):115659. https://doi.org/10.1016/j.diagmicrobio.2022.115659.
von Huth S, Lillevang ST, Røge BT, Madsen JS, Mogensen CB, Coia JE, et al. SARS-CoV-2 seroprevalence among 7950 healthcare workers in the Region of Southern Denmark. Int J Infect Dis. 2021;112:96–102. https://doi.org/10.1016/j.ijid.2021.09.023.
Tian S, Hu N, Lou J, Chen K, Kang X, Xiang Z, et al. Characteristics of COVID-19 infection in Beijing. J Infect. 2020;80(4):401–6. https://doi.org/10.1016/j.jinf.2020.02.018.
Widawati M, Pradani FY, Fuadiyah MEA, Fuadzy H, Rohmansyah WN, editors. Factors associated with COVID-19 test willingness in Indonesia: tele-survey study after ‘new normal’policy in risk groups. E3S Web of Conferences; 2021: EDP Sciences.
McDermott JH, Newman WG. Refusal of viral testing during the SARS-CoV-2 pandemic. Clin Med. 2020;20(5):e163.
Alhabbab RY, Alsaieedi A, Algaissi A, Almahboub S, Al-Raddadi RM, Shabouni OI, et al. Seroprevalence of SARS-CoV-2 binding and neutralizing antibodies in healthcare workers during the epidemic peak in referral hospitals and quarantine sites: Saudi Arabia. Viruses. 2021;13(7):1413. https://doi.org/10.3390/v13071413.
Acknowledgements
Not applicable.
Risks and benefits for subjects
Donation of the blood sample was under strict quality control and under the best-practice to avoid any risk for the participants. This study poses minimal risk to participants involving the collection of a small amount of blood. The direct benefit to the participant was the potential detection of COVID-19 infection, which would then allow for appropriate monitoring and treatment. The primary benefit of the study is indirect in that the data collected will help to improve and guide efforts to understand the transmission of COVID-19 and to prevent its further spread.
Funding
This study received no funding.
Author information
Authors and Affiliations
Contributions
Conceptualization: WTh and AB. Facilitate data collection: WTh. Formal analysis: AB and WTh. Consultancy and editing TS, and KhS. Writing original draft: WTh, AB, and TS. Writing–review & editing: WTh, AB, TS, and KhS.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research process was performed in accordance with guidelines and regulations of the Declaration of Helsinki laws for the protection of human participants in health research.
The study was approved by the Ethics Research Committee (ERC) of the Faculty of Medicine and Health Sciences, University of Aden (REC-#119–2022) and according to the national regulations and institutional policies on ethics.
Written informed consent was obtained from all study participants who agreed to participate in the study before data or blood collection. Explanation of the objectives, importance of the study, and benefits of the research and that the participation is voluntary, and they have the right to not complete this survey without giving any reason. They were assured that all the collected data will be handled with full confidentiality and used only for the research purpose.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Taher, W.T., Bawazir, A.A., Sallam, T.A. et al. Seroprevalence and factors associated with SARS-CoV-2 infection among healthcare workers: cross-sectional study. BMC Infect Dis 23, 761 (2023). https://doi.org/10.1186/s12879-023-08760-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08760-5