Abstract
Background
The aim of the study was to identify the pathogens, in addition to bordetella pertussis (B. pertussis), which cause pertussis-like syndrome in children and to compare clinical presentation between those with B. pertussis and pertussis-like syndrome.
Methods
A cross-sectional analysis was conducted from March 2016 to September 2018. In total, 281 children with suspected pertussis infections were enrolled in this study. Multi-pathogen detection was performed.
Results
In total, 281 children were enrolled including 139 males and 142 females. Among them, 149 (53.0%) were B. pertussis positive, and 72 (15.6%) children tested positive for other pathogens. Mycoplasma pneumoniae (MP, 27 cases) was the most common causative pathogen in pertussis-like syndrome, followed by human rhinovirus (HRV, 23 cases), Streptococcus pneumoniae (SP, 13 cases), Haemophilus influenzae (HI, 12 cases) and parainfluenza virus 3 (Pinf-3, 9 cases). Children in the B. pertussis group had a higher rate of vaccination and longer hospital stay (P < 0.05). B. pertussis was more likely to be detected in winter than other pathogens, but this difference was not significant (P = 0.074). The number of white blood cells, neutrophils and blood platelets was significantly higher in children in the B. pertussis than in the pertussis-like group (P < 0.05). In addition, the percentage of CD3-CD19+ cells was significantly higher in the B. pertussis group (P = 0.018).
Conclusion
About half of the children with pertussis-like syndrome were B. pertussis positive. MP was the second most common causative pathogen followed by HRV, SP, HI and Pinf-3. Children infected with B. pertussis had longer hospital stay and higher numbers of white blood cells, neutrophil and blood platelets compared with other pathogens.
Similar content being viewed by others
Background
Pertussis is one of the top ten fatal infections in children, causing serious and potentially fatal complications, especially in very young infants [1, 2]. It is a respiratory disease caused by infection with Bordetella pertussis (B. pertussis). The well-known symptoms of pertussis include repeated paroxysmal cough, inspiratory whoop, and post-cough vomiting [3]. However, these clinical symptoms are not limited to patients with B. pertussis infection. Other pathogens such as adenovirus (ADV), influenza virus (IV), and Mycoplasma pneumoniae (MP) also can cause similar clinical symptoms [4], collectively known as pertussis-like syndrome.
Pertussis-like syndrome can occur at all ages but is more common in children. It can be very unpleasant for patients, especially young infants and their parents, as symptoms frequently interfere with daily activities and cause significant sleep disturbance. Especially in the paroxysmal stage characterized by spasmodic cough followed by post-tussive whooping and vomiting, the effect of available medications is poor leading to anxiety in parents. It is difficult to distinguish the symptoms of infection with B. pertussis from infection with viruses. In addition, there is a lack of information around the etiology of pertussis-like syndrome worldwide. As such, a greater understanding of the pathogens that cause pertussis-like syndrome is important to inform treatment decision making.
In this study, we aimed to identify the causative pathogens associated with pertussis-like syndrome and to compare clinical presentation between those with B. pertussis and pertussis-like syndrome in children admitted to the Children’s hospital of Soochow university.
Methods
Study design and population
This was a cross-sectional study designed to identify the causative pathogens associated with pertussis-like syndrome. Children with suspected pertussis who were admitted to the Children’s Hospital of Soochow University from March 2016 to September 2018 were enrolled in this study. The clinical criteria for suspected pertussis are cough lasting for > 2 weeks with one or more of the following symptoms: whoop and staccato cough, apneic paroxysm or post-tussive vomiting. The exclusion criteria were historical diagnosis of chronic lung disease, congenital heart disease, immunodeficiency or preterm birth at ≤34 weeks’ gestation. In addition, 91 children admitted to the childcare unit for health examination were enrolled in the control group, including 75 boys and 16 girls. The average age was (0.67 ± 0.58) years old. Routine blood tests and cellular immunity results were collected.
Sample collection
Nasopharyngeal aspirates were obtained from each patient within 18 h after admission using a sterile plastic catheter, which was briefly inserted into the lower pharynx via the nasal cavity. These samples were used for detection of common microorganisms, such as respiratory syncytial virus (RSV), ADV, influenza viruses A and B (IV-A and B), parainfluenza viruses 1, 2, and 3 (Pinf-1, 2, 3), human metapneumovirus (hMPV), human bocavirus (HBoV), human rhinovirus (HRV), MP, and bacteria.
Blood samples were collected immediately after admission for routine tests (Sysmex XS-500i, Hua Sin Science Co., Ltd., Guangzhou, China), liver and kidney function (ADVIA 2400, Siemens Healthineers, America), and cellular immunity.
B. Pertussis detection
B. pertussis DNA was detected in nasopharyngeal aspirates by real-time polymerase chain reaction (PCR). Pathogen detection was achieved using a TaqMan genomic assay and fluorescent real-time PCR (BIO-RAD iCycler, USA). B. pertussis DNA was determined using two PCR assays, each specific for an independent region of the B. pertussis genome: (i) the insertion sequence IS481 and (ii) the pertussis toxin S1 (ptxA) promoter region. IS481 is a very sensitive target for screening B. pertussis because it is the most common insertion sequence, with multiple copies per genome [5, 6]. PtxA is highly specific but less sensitive because it usually exists as a single or occasionally double copy [7, 8]. Oligonucleotide primers targeting the ptxA promoter of B. pertussis (PTp1 and PTp2, Table 1) were used to amplify a 191-bp product, while primers targeting the insertion sequence IS481 of B. pertussis (BP-1 and BP-2MOD, Table 1) were used to amplify a 145-bp product. All primers and probes were purchased from Sangon Biotech (Shanghai) Co., Ltd. (Shanghai, China). Positive, negative and water blank controls were set for each PCR amplification. The judgement of positive results is generally < 34 cycles. Higher than this number, but with an amplification curve, and the curve is smooth, we would repeat the experiment. If the results of the two experiments were the same, a positive result was recorded, otherwise negative. B. pertussis infection was defined as IS481 PCR positive, whether ptxA PCR is positive or not.
Other microbiological analyses
Ten viruses and bacteria (including MP) were also tested in nasopharyngeal aspirates. Bacteria were tested by inoculating nasopharyngeal aspirates on blood plates that were read after incubating for 18–20 h. Bacterial growth was > 103 colony forming units/ml was considered significant. Viruses including RSV, ADV, IV-A and B and Pinf-1, 2, 3 were investigated by immunofluorescence tests using D3 Ultra™ Respiratory Virus Screening and LD Kit (Diagnostic Hybrids, Ohio, USA). A positive result was defined as over five inclusion bodies analyzed under a fluorescence microscope. MP and the various viruses were examined by PCR (Nucleic acid amplification fluorescent reagent kit, Ann Gene Co., Guangdong, China) according to the manufacturer’s instructions.
Cellular immunity
Venous blood was anticoagulated by heparin and antibodies were added to whole blood (anti-CD3+ and anti-CD19+ labeled with cyanobacteria-5 antibody, anti-CD4+, anti-CD23+ and anti-CD25+ labeled with fluorescein isothiocyanate, and anti-CD8+ antibody labeled with algal red protein). After mixing, the cells were incubated in a dark chamber and lysed with hemolysin, followed by further incubation in a dark chamber. Flow cytometry was performed using a BECKMAN COULTER flow cytometer and a specific kit (Immunotech, France).
Clinical data collection
Detailed demographic and clinical data such as age, gender, pertussis vaccination status, previous antibiotic consumption, family history of pertussis, and clinical symptoms were obtained from questionnaires that were answered by patients’ parents and from medical records.
Statistical analysis
Enumeration data are expressed as mean ± standard deviation (SD). Measurement data are expressed as a percentage (%). Statistical analysis was performed using SPSS 18.0 software (SPSS Inc., Chicago, IL); the rank sum test was used for comparison among groups and one-way analysis of variance was used for comparison. P < 0.05 was considered statistically significant.
Results
Study population
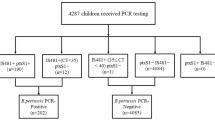
During the study period, a total of 281 children presenting with pertussis-like syndrome were included in the study. Among them, 139 were male and 142 were female. The male to female ratio was approximate 1:1.02. Age ranged from 1 month to 12 years old with a median age of 5 months (interquartile rane: 3–8.5 months). From the 281 nasopharyngeal aspirates, 149 (53.0%) were B. pertussis positive (140 cases for both IS481 and PtxA positive and 9 cases for only IS481 positive), referred to as the B. pertussis group. Another 132 children who were infected with pathogens other than B. pertussis or who tested negative overall were classified as the pertussis-like group.
Comparison between pertussis and pertussis-like syndrome
Clinical manifestation
Children in the pertussis-like group were younger than those in the B. pertussis group, but there was no significant difference between them (P = 0.291). The pertussis-like group seemed to include more girls while the B. pertussis group included more boys, but with no significant difference (P = 0.056). Children in the B. pertussis group had a higher rate of vaccination compared with the pertussis-like group (43.2% vs 60.4%, P = 0.004) (this does not include children under 3 months old who do not need to be vaccinated). Children who were not vaccinated against pertussis or who were not fully vaccinated according to age were judged to not have received a scheduled vaccination. There was no significant difference in the scheduled vaccination rate between the two groups (66.3% vs 78.4%, P = 0.072). Children in the B. pertussis group had longer hospital stay compared with the pertussis-like group (9.91 ± 3.74 days vs 11.37 ± 4.90, P = 0.006). B. pertussis was more likely to be detected in winter than other pathogens, but there was no significant difference in seasonality between the two groups (P = 0.074). There were no significant difference in clinical manifestation between the two groups with regards to symptoms such as paroxysmal cough, post-cough vomiting, inspiratory whoop and so on. Pertussis encephalopathy and pulmonary hypertension were not identified in any children. Data are presented in Table 2.
Laboratory examination
The number of white blood cells and neutrophils was significantly higher in children in the B. pertussis group and the pertussis-like group than the control group (P < 0.001). This phenomenon was more obvious in the B. pertussis group than the pertussis-like group (15.94 ± 9.40 vs 19.06 ± 9.99, P = 0.008; 9.34 ± 6.46 vs 11.52 ± 7.73, P = 0.011). Children infected with B. pertussis had a significantly higher number of blood platelets than patients in the pertussis-like group (455.05 ± 122.68 vs 487.01 ± 133.38, P = 0.038). Both groups had a significantly higher number of blood platelets than patients in the control group (P < 0.001). There were no significant differences in the number of lymphocytes or liver function as measured by serum creatine kinase of MB type (CKMB) or C-reactive protein (CRP). For cellular immunity, the percentage of CD3+ cells was significantly lower in the B. pertussis group than the control group (63.40 ± 9.34 vs 66.89 ± 6.58, P = 0.001) but no significant difference was identified compared with the pertussis-like group (P = 0.157). The percentage of CD3-CD19+ cells was significantly higher in the B. pertussis group than the other two groups (P = 0.018 and P < 0.001). Both the pertussis-like group and the B. pertussis group had a significantly lower percentage of CD3 + CD8+ cells than the control group (P < 0.001). The percentage of CD3-(CD16 + CD56) + cells was slightly lower than in the B. pertussis group, but with no significant difference (P = 0.152). Data are presented in Table 3.
Chest radiograph and pulmonary auscultation
The most common abnormal chest radiological findings in both groups were bilateral diffuse interstitial infiltrations and patchy shadows with no significant differences between the two groups. Moist rales and wheezing were most common in children with B. pertussis infection. Data were presented in Table 4.
Pathogens in children with pertussis-like syndrome
Among 132 children who had pertussis-like syndrome, 72 children tested positive for the pathogen (54.4%). Among them, 46 (63.9%) patients had simple infections and 26 (36.1%) patients had co-infections. MP was the most common pathogen in patients with pertussis-like syndrome. The most common virus was HRV, followed by Pinf-3, RSV, hBoV. The most common causative bacteria was Streptococcus pneumoniae (SP), followed by Haemophilus influenzae (HI). The distribution of all pathogens is shown in Table 5.
Comparison between pathogen-positive and negative pertussis-like syndrome
There were no significant differences in clinical manifestations or laboratory results between patients with pathogen-positive and negative pertussis-like syndrome. There were also no significant differences with regards to age, sex ratio, vaccination history or hospital stay between the two groups. Data are presented in Table 6.
Discussion
Pertussis is a series of respiratory symptoms caused by infection with B. pertussis, including paroxysmal fits of coughing, vomiting after coughing and deep inspirium. The intermittent symptoms of coughing can last for more than 28 days and up to 3 months [9]. However, in clinical practice, we found that other pathogens can also cause pertussis-like cough as part of pertussis-like syndrome. Stephanie Saiki-Macedo found that in Peru, there was a high prevalence of ADV, B. pertussis, MP and IV-B infection in patients with a probable diagnosis of pertussis [10]. In our study, detailed etiological examination was performed in 281 children who had typical pertussis-like syndrome. About half of the children were B. pertussis positive, and about a quarter of the children had infections with other pathogens. No pathogens were detected in around a quarter of the children tested. Our study found that, in addition to B. pertussis, the most common causative pathogen in children with pertussis-like syndrome children was MP, which was detected in more than one third of children. In addition, the rate of HRV, SP, HI and Pinf-3 infections was also high in pertussis-like syndrome.
Amal Al Maani compared pertussis and pertussis-like illness in Oman and found there was no significant difference in clinical criteria between them [11]. In our study, no children had pertussis encephalopathy or pulmonary arterial hypertension and there was no significant difference in other clinical manifestations between the pertussis-like group and the B. pertussis group. Spastic cough was more common in spring and summer and nearly half of these children had B. pertussis. However, more than 75% of children had B. pertussis infection in the winter. Therefore, the occurrence of whooping cough in winter should raise suspicion of B. pertussis infection.
Previous studies showed that leukocytosis, especially lymphocytosis was associated with mortalities and morbidities in patients with pertussis infection [12, 13]. In our study, the absolute lymphocyte count in the B. pertussis group was higher than the pertussis-like group, but with no significant difference. However, the absolute neutrophil count and blood platelet count in the B. pertussis group was significantly higher than in the pertussis-like group and control group. This may be associated with the time of onset. Joshua C. Eby studied the relationship between pertussis bacillus and neutrophils and found that the recruitment of neutrophils is suppressed by the pertussis toxin early in the course of the disease, but after the first week, the combined activities of pertussis toxin, lipooligosaccharide and adenylate cyclase toxin result in production of cytokines that generate an IL-17 response, promoting neutrophil recruitment [14]. In our study, most children with pertussis had been ill for more than a week before being hospitalized. This could explain the significant increase of neutrophils in the children with B. pertussis infection in our study. As for the relationship between pertussis and platelets, the study results are controversial. Pertussis toxin shows distinct early signalling events in platelet-activating factors leading to thrombocytosis and platelet activation through interaction with platelet glycoprotein Ib [15, 16]. However, other studies showed that platelet aggregation is suppressed by the B. pertussis adenylate cyclase toxin through increased intracellular cyclic adenosine monophosphate (cAMP), and this dysfunction resulted in hemorrhage [17]. In our study, children infected with B. pertussis had a significantly higher number of blood platelets, which may be related to the overactive immune inflammatory response following B. pertussis infection.
MP is one of the most common causes of community-acquired pneumonia in children. In older children, MP infection can cause lobular pneumonia with clinical manifestations including high fever and cough. However, in young children, chest radiographs often showed interstitial inflammation which mainly manifested as cough and wheezing. Many studies showed that MP can cause persistent cough [18, 19]. Wang K found that MP is an important infection in children with persistent cough but the course is shorter than pertussis [20], which is similar to our results. As both B. pertussis and MP are mainly treated with macrolide drugs like erythromycin or azithromycin, children with persistent cough or spasmodic cough can be treated empirically with these drugs in clinical practice.
The current study has some limitations. First, the sample size is still small. In the next stage, we will continue to enroll more children with pertussis-like syndrome and follow up them to explore the long-term prognosis of these children. Second, there are still limitations in pathogen detection. Our test did not include all the pathogen that can cause pertussis-like syndrome, like Bordetella parapertussis, which accounts for 10–14.9% of Bordetella [21]. We will detect more kinds of pathogens including Bordetella parapertussis later.
Conclusion
This was a cross-sectional study designed to identify the etiologic agents of pertussis-like syndrome. About half of the children were B. pertussis positive. MP was the second most common among other identified pathogens, followed by HRV, SP, HI and Pinf-3. Children infected with B. pertussis had a longer hospital stay and higher numbers of white blood cell, neutrophils and blood platelets.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- ADV:
-
Adenovirus
- HI:
-
Haemophilus influenzae
- hMPV:
-
human metapneumovirus
- HRV:
-
Human rhinovirus
- IV:
-
Influenza virus
- MP :
-
Mycoplsma pneumonia
- Pinf-3:
-
Parainfluenza Virus 3
- RSV:
-
Respiratory syncytial virus
- SD:
-
Standard deviation
- SP:
-
Streptococcus pneumoniae
References
Haghighi F, Shahcheraghi F, Abbasi E, Eshraghi SS, Zeraati H, Mousavi SA, et al. Genetic profile variation in vaccine strains and clinical isolates of Bordetella pertussis recovered from Iranian patients. Avicenna J Med Biotechnol. 2014;6:178.
Nguyen VTN, Simon L. Pertussis: the whooping cough. Prim Care. 2018;45(3):423–31.
Shojaei J, Saffar MJ, Hashemi A, Ghorbani GR, Rezai MS, Shahmohammadi S. Clinical and laboratory features of pertussis in hospitalized infants with confirmed versus probable pertussis cases. Ann Med Health Sci Res. 2014;4:910–4.
Pavic-Espinoza I, Bendezú-Medina S, Herrera-Alzamora A, Weilg P, Pons MJ, Aguilar-Luis MA, et al. High prevalence of Bordetella pertussis in children under 5 years old hospitalized with acute respiratory infections in Lima. Peru BMC Infect Dis. 2015;15:554.
Tizolova A, Guiso N, Guillot S. Insertion sequences shared by Bordetella species and implications for the biological diagnosis of pertussis syndrome. Eur J Clin Microbiol Infect Dis. 2013;32:89–96.
Papenburg J, Fontela P. What is the significance of a high cycle threshold positive IS481 PCR for Bordetella pertussis? Pediatr Infect Dis J. 2009;28:1143 author reply −4.
Gao F, Mahoney JC, Daly ER, Lamothe W, Tullo D, Bean C. Evaluation of a multitarget real-time PCR assay for detection of Bordetella species during a pertussis outbreak in New Hampshire in 2011. J Clin Microbiol. 2014;52:302–6.
Tatti KM, Sparks KN, Boney KO, Tondella ML. Novel multitarget real-time PCR assay for rapid detection of Bordetella species in clinical specimens. J Clin Microbiol. 2011;49:4059–66.
Sarbay H, Polat A, Mete E, Balci YI, Akin M. Pertussis-like syndrome associated with adenovirus presenting with hyperleukocytosis: Case report. North Clin Istanbul. 2016;3:140–2.
Saiki-Macedo V-E, Cornejo-Tapia CME, Petrozzi-Helasvuo V, Aguilar-Luis MA, et al. Identfication of viral and bacterial etiologic agents of the pertussis-like syndrome in children under 5 years old hospitalized. BMC Infect Dis. 2019;19:75.
Al Maani A, Al Qayoudhi A, Nazir HF, Omar H, Al Jardani A, Al Muharrmi Z, et al. Pertussis and pertussis like illness: pediatric experience in Oman. Oman Med J. 2017;32:396–402.
Guinto-Ocampo H, Bennett JE, Attia MW. Predicting pertussis in infants. Pediatr Emerg Care. 2008;24:16–20.
Pierce C, Klein N, Peters M. Is leukocytosis a predictor of mortality in severe pertussis infection? Intensive Care Med. 2000;26:1512–4.
Eby JC, Hoffman CL, Gonyar LA, Hewlett EL. Review of the neutrophil response to Bordetella pertussis infection. Pathog Dis. 2015;73:ftv081.
Sindt KA, Hewlett EL, Redpath GT, Rappuoli R, Gray LS, Vandenberg SR. Pertussis toxin activates platelets through an interaction with platelet glycoprotein Ib. Infect Immun. 1994;62:3108–14.
Teixeira MM, Giembycz MA, Lindsay MA, Hellewell PG. Pertussis toxin shows distinct early signalling events in platelet-activating factor-, leukotriene B4-, and C5a-induced eosinophil homotypic aggregation in vitro and recruitment in vivo. Blood. 1997;89:4566–73.
Iwaki M, Kamachi K, Heveker N, Konda T. Suppression of platelet aggregation by Bordetella pertussis adenylate cyclase toxin. Infect Immun. 1999;67:2763–8.
Sobieszczańska BM, Kasprzykowska U, Duda-Madej A, Secewicz A, Marciniak J, Gościniak G. Relevance of serology for mycoplasma pneumoniae infection among children with persistent cough. Adv Clin Exp Med. 2014;23:185–90.
Yuan X, Liu Y, Bai C, Luo Y, Wang R, Wang R, et al. Mycoplasma pneumoniae infection is associated with subacute cough. Eur Respir J. 2014;43:1178–81.
Wang K, Chalker V, Bermingham A, Harrison T, Mant D, Harnden A. Mycoplasma pneumoniae and respiratory virus infections in children with persistent cough in England: a retrospective analysis. Pediatr Infect Dis J. 2011;30:1047–51.
Koepke R, Bartholomew ML, Eickhoff JC, Ayele RA, Rodd D, Kuennen J, et al. Widespread Bordetella parapertussis infections-Wisconsin, 2011-2012: clinical and epidemiologic features and antibiotic use for treatment and prevention. Clin Infect Dis. 2015;61(9):1421–31.
Acknowledgments
Not Applicable.
Funding
This work was supported by National Natural Science Foundation of China (Approval no. 81573167), Science and Technology Support Program of Jiangsu Province (Approval no. BE2017657) and People’s livehood Science and Technology Projects of Suzhou (Approval no. SYS201646 and SYSD2017092).
Author information
Authors and Affiliations
Contributions
YW designed the study. KW, SC, MW performed the experiments. YH and YL provided the statistical analysis. XS and JX were responsible genomic analysis. XZ and WG drafted the initial manuscript. YW and CH revised the manuscript, and all authors approved the final content of this manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All the participants’ parents or guardians gave their written informed consent for participation in the study. The study was approved by the ethics committee of Soochow University.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gu, W., Wang, K., Zhang, X. et al. Pathogen analysis of pertussis-like syndrome in children. BMC Infect Dis 20, 353 (2020). https://doi.org/10.1186/s12879-020-05074-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-020-05074-8