Abstract
Background
In recent years, tuberculosis outbreaks in schools have occurred more frequently in China than in other parts of the world, and have posed a public health threat to students and their families. This systematic review aimed to understand the epidemiological characteristics of tuberculosis (TB) outbreaks and analyze the factors associated with TB outbreaks in schools in China.
Methods
We conducted this systematic review following the standard procedures of the Cochrane Collaboration and the Preferred Reporting Items for Systematic Review and Meta-Analysis statement. The meta-analysis was performed with STATA using a random effects model.
Results
We included 107 studies involving 1795 student patients with TB in mainland China. The results of the systematic analysis indicated that TB outbreaks were more frequently reported in senior middle schools and in Eastern China. The outbreaks mainly occurred during the winter and spring, and the median outbreak duration was 4 months. The meta-analysis showed that the total attack rate and the class attack rate of tuberculosis outbreaks among students were 4.60% (95% CI 3.80 to 5.70%) and 22.70% (95% CI 19.20 to 27.00%), respectively. Subgroup analysis showed that outbreaks that occurred at universities or colleges had a relatively higher attack rate than those occurred in senior middle schools. The prevalence of latent tuberculosis infection (LTBI) among close contacts was 23.70% (95% CI 19.50 to 28.90%). The median case-finding interval was 2 months, and 47.40% of the index cases had a case-finding delay.
Conclusion
The results of our review indicated that school TB outbreaks were reported most frequently in senior middle schools in China. The attack rates of outbreaks at universities or colleges were higher than those in senior middle schools. The TB outbreaks in schools usually occurred over prolonged periods. The case-finding delay in the index cases must be reduced to prevent transmission in classes and schools. Effective surveillance and screening of presumptive TB cases in schools should be strengthened to reduce outbreaks in schools.
Similar content being viewed by others
Background
Tuberculosis (TB) is one of the top 10 causes of death worldwide [1, 2]. In 2017, 10.1 million people fell ill with TB, and 1.6 million of them died from the disease (including 0.3 million people with HIV). About 87% TB cases was from 30 countries with the heaviest burden of tuberculosis [3]. China is one of 30 countries with the heaviest burden of tuberculosis patients, and it has the third highest number of cases [3, 4]. According to the fifth national tuberculosis epidemiological survey conducted in 2010, the prevalence of active pulmonary TB and smear-positive pulmonary TB was 459/100,000 and 66/100,000, respectively, in the population aged over 15 years [5]. In 2012, the reported incidence of PTB was 16.63 per 100,000 students [6]. According to the China Information System for Disease Control and Prevention, student TB patients accounted for 4.02% of total TB patients in 2014 [6]. The top five provinces had the highest TB incidence rates among school students, including Tibet(79.95/100,000), Qinghai(59.09/100,000), Guizhou(36.54/100,000), Chongqing(33.06/100,000) and Xinjiang(26.08/100,000) [7, 8], which are mainly western regions of china. As a respiratory infectious disease, PTB is more likely to spread within clusters and subsequently progress to outbreaks. According to previous studies, school TB outbreaks, refer to 3 or more cases with an epidemiological link at the same school within 2 years [9, 10]. The epidemiological link refers to the clustering of cases with a mutual contact history as detected by a field investigation in one place during the outbreak period [11]. Pulmonary TB outbreaks in schools usually cause an enormous social impact. According to a study investigating an outbreak in a training school in Shanxi Province, the prevalence of TB was 15.70%, which was a serious clustered outbreak that lead to an irreversible impact on students [12]. The recent outbreak of school tuberculosis in Taojiang County, Hunan Province was another typical example. According to related news reports, 81 confirmed tuberculosis cases and 7 presumptive tuberculosis cases were reported in this incident [13]. The outbreak caused a substantial social impact, especially on students and their families. Therefore, once tuberculosis spreads widely among students, it causes great panic among classes and schools and even affects social stability.
China has a relatively comprehensive mechanism for reporting school TB outbreaks. The outbreaks are reported to different institutions according to the number of cases. Outbreaks with more than 3 but fewer than 10 cases are reported to the local government, while outbreaks with more than 10 cases are reported to the government over province level as an emergency public health event. Once the Centers for Disease Control and Prevention (CDC) detects 3 or more cases based on the surveillance system, the Health and Education Department should investigate and address the epidemic, mainly through close contact screening, tracing the sources of infection, etc. An outbreak investigation report is then written by the Health Department and submitted to the government.
To the best of our knowledge, most research articles are case reports of single-school TB outbreaks in China. However, it is difficult to systematically obtain information about the epidemiological features of school TB outbreaks from single outbreak case reports. No studies have systematically reviewed TB outbreaks among Chinese schools. It is important to synthesize the characteristics of TB outbreaks among schools to help develop public health strategies for school TB outbreaks.
We conducted this systematic review and meta-analysis to identify all the available published case studies in the Chinese and English languages that reported TB outbreaks among schools in mainland China. The objectives of this review are the following: i) to obtain the attack rate of TB and prevalence of LTBI among students during TB school outbreaks in China; ii) to understand the main characteristics of school TB outbreaks, including the age and sex distribution of cases, outbreak duration, characteristics of the index case, and intervention measures; and iii) to analyze the factors associated with TB outbreaks in schools in China.
Methods
Search strategies
We searched the following six English and Chinese electronic databases for primary studies: China Knowledge Resource Integrated Database (http://www.cnki.net/); Wanfang Med Online (http://med.wanfangdata.com.cn/); Chinese Biomedical Literature Database(CBM) (http://www.sinomed.ac.cn/); VIP database (http://lib.cqvip.com/), PubMed (https://www.pubmed.gov); ScienceDirect, which is Elsevier’s leading platform for peer-reviewed scholarly literature (http://www.sciencedirect.com/search?qs=); and Web of Science (http://isiknowledge.com). Our search strategy included terms such as “tuberculosis”, “outbreak”, “school”, “university”, and “college” (details of the complete search strategy are provided in Additional file 1). All the results were retrieved in June, 2019. This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [14].
Inclusion and exclusion criteria
The inclusion criteria were 1) outbreaks that occurred at schools (junior middle schools, senior middle schools and universities, ≥3 reported cases with an epidemiological link; 2) sufficient basic information (school type, school location and epidemiological investigation information regarding the outbreak); 3) clear diagnosis of tuberculosis; and 4) epidemiological investigation processing of the outbreak (tracing of the index case, a clear contact investigation process, epidemiological analysis of cases and intervention measures). The exclusion criteria were 1) the research article was a review or described a nonoutbreak; 2) the reports and studies lacked key information on the epidemiological investigation process; and 3) the TB outbreaks occurred before 2000.
Data extraction
Two reviewers independently screened the citations (titles and abstracts) identified from all sources. The data extracted from the studies included the following items: author, publication year, journal, title, outbreak duration, outbreak area, school type, the living accommodation space of one person, attack rate, prevalence of LTBI, screening criteria, number of different TB types, interventions, and information on the index cases (age, sex, grade, time of TB onset, case-finding interval, secondary case onset time, and clinical information such as TB type and the results of sputum smears and chest X-rays). The terms used in this study are defined below.
School: included three types: i) junior middle school and primary school (aged 6–15 years), China’s 9-year compulsory education for all citizens [15]; ii) senior middle school (aged 15–17 years), the continuation of junior middle school education considered to be a critical preparation for college education [16]; and iii) university or college (age above 17 years), defined as an institution of higher education offering education in mainly nonvocational subjects and typically having the power to confer degrees [17]. University or college education usually lasts 4 years in China.
Outbreak: ≥3 epidemiological linked cases within 2 years, based on the CDC guidelines for contact investigations [9, 10].
Outbreak duration: the time period between index case confirmation and final case confirmation.
Attack rate: an incidence within a limited area during a short period [18]. In this study, we defined two attack rates, namely, the total attack rate and the class attack rate. The former rate was based on the screened populations and, was calculated as the number of new cases divided by the number of the screened populations. The number of the screened population was determined by the number of close contacts of the index case during an outbreak; these close contacts might have been from one class, several classes or the entire school. The class attack rate was based on the classes where the index cases occurred, calculated as the number of new cases in each class divided by the number of students in that class.
Prevalence of LTBI (latent tuberculosis infection) and screening criteria: LTBI refers to individuals who are infected with Mycobacterium tuberculosis, but do not develop active tuberculosis. Students who had a strong positive PPD (purified protein derivatives tuberculin) result were identified as LTBI. A strong positive result mainly refers to the judgment criteria used in different studies, namely, induration size more than 15 mm or 20 mm [19, 20], depending on the study. Articles used chest radiography as a screening method in our calculation of the prevalence of LTBI were excluded. In addition, we defined two prevalence of LTBI, namely, the total prevalence of LTBI and the prevalence of LTBI among close contact. The former was calculated as the number of students with LTBI divided by the number in the screened population, which may not be the close contacts of the index cases (all of school students may be screened in some outbreaks). The prevalence of LTBI among close contact was calculated as the number of students with LTBI divided by the number of close contacts who were strictly confirmed.
Season when the index case was detected: the season was divided according to the Meteorological Department of China. Spring occurred from March to May, summer occurred from June to August, autumn occurred from September to November, and winter occurred from December to February.
Case-finding interval: the time interval between the onset of TB symptoms and the first diagnosis of TB.
Case-finding delay: a case-finding interval longer than 2 months [19].
Index case: the first case with TB symptoms detected by field epidemiological investigation in one outbreak.
Data analysis
The meta-analysis was performed using STATA version 14.0 for Windows (STATA Corporation, College Station, Texas, United States). A random effects model was used for the analysis. The results are presented in tables (rate, number of studies, 95% CI, heterogeneity) and forest plots. Publication bias was assessed by a funnel plot. The systematic review was performed using Statistical Package for Social Sciences (SPSS) version 18.0 (SPSS Inc., Chicago, Illinois, USA). We used meta-regression to explore the associations among variables.
Results
Identified studies
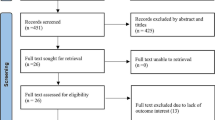
Among the 7027 articles we searched in the databases, 107 articles met our inclusion criteria (Fig. 1) [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127]. A total of 79 (73.80%) studies reported the attack rate of TB, and 81 (75.70%) studies determined the prevalence of LTBI. Additionally, 80 articles reported the interventions for the outbreaks.
Publication bias was tested with Begg’s test. The results showed that the P value was 0.34, which indicated that there was no significant publication bias (Fig. 2) [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127].
Main results
Outbreak and patient summaries
The 107 outbreaks included in our review involved 1795 student TB patients (median 16.8 cases/outbreak, range 4–66 cases) [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127]. Among these outbreaks, 66 (61.70%) outbreaks occurred at senior middle schools and involved 1100 patients; universities or colleges followed, with 29 (29.00%) outbreaks involving 587 patients. Only 10 outbreaks occurred at junior middle schools or primary schools and involved 108 patients. There were 22 (20.60%) outbreaks that lasted less than 1 month, and 34 outbreaks lasted more than 4 months. In terms of geographical distribution, there were 78 (72.90%) outbreaks involving 1207 patients reported in the eastern provinces of China while 13 (12.10%) outbreaks occurred in central provinces. As for the time season of index case detection, most outbreaks occurred in winter, accounting for 41.10% (Table 1).
Except for 484 patients whose sex was not documented, 799 (60.95%) cases were males, and 512 (39.05%) cases were females. Among the 1795 patients, 1572 (90.40%) patients had pulmonary TB, including 263 (16.73%) with smear-positive TB and 1309 (83.27%) with smear-negative TB. Another 167 (9.60%) patients had had extrapulmonary tuberculosis. There were 393 cases that reported a tuberculous cavity, of which 37 (9.41%) patients had cavernous pulmonary tuberculosis. Additionally, among LTBI cases in the studied outbreaks, 2398 students had received prophylaxis, while only 1645 (68.59%) finished 6 months of prophylaxis (Table 2).
Characteristics of the index cases
Table 3 presents the characteristics of the index cases of the outbreaks. According to 72 studies reporting the gender of the index cases, 54 (75.00%) cases were males, and 18 (25.00%) were females. A total of 17 outbreak studies reported the family history of the index case, among which 7 cases had a family history. A total of 90 outbreak studies provided information on sputum smear results, among which 75 (83.30%) cases were positive, and 15 (16.70%) cases were negative. There were 20 outbreak studies that reported the degree of smear positivity. The median case-finding interval was 2 months. A total of 48 (53.93%) cases had a case-finding interval less than or equal to 2 months, while 45 (47.40%) cases had a case-finding interval longer than 2 months, which was defined as a case-finding delay. The median interval from the confirmation of the first case to the report of the second case was 4 months among 37 outbreaks.
Attack rate of TB among students in mainland China, 2000–2017
As shown in the Tables 4, 79 (73.80%) studies determined the attack rate [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92, 122,123,124,125,126,127]. The results showed that the pooled total attack rate of TB was 4.60% (95% CI 3.80 to 5.70%). Subgroup analysis suggested that the pooled total attack rate of junior middle schools was 5.80% (95% CI 2.80 to 12.80%), followed by universities or colleges with a pooled attack rate of 5.00% (95% CI 3.50 to 7.10%). The pooled attack rate of outbreaks at senior middle schools was 4.30% (95% CI 3.30 to 5.80%). The results showed that the pooled total attack rate among outbreaks with 10 or more cases was 6.10% (95% CI 4.70 to 7.20%), and the total attack rate in outbreaks with fewer than 10 cases was 3.00% (95% CI 2.10 to 4.30%). In terms of regions, the pooled attack rate of outbreaks in the eastern, central and western regions of China were 4.70% (95% CI 3.70 to 6.00%), 8.70% (95% CI 5.80 to 13.20%), and 2.80% (95% CI 1.70 to 4.90%), respectively(see details in Additional file 2).
Table 5 shows that the pooled class attack rate of 61 outbreaks was 22.70% (95% CI 19.20 to 27.00%) [21,22,23,24,25, 28, 29, 32, 36, 39, 44, 47, 50, 53, 55, 57, 59, 61, 63, 68, 70, 72, 74, 77, 81, 83, 86, 91, 93, 95, 99, 102, 104, 106, 108, 114, 115, 117, 122, 124,125,126,27,128]. Subgroup analysis showed that the pooled class attack rate for the 40 senior middle school outbreaks was 21.80% (95% CI 17.40 to 27.40%), and that of the 16 university or college outbreaks was 25.00% (95% CI 18.30 to 34.10%). In terms of geographic distribution, the pooled class attack rates for the eastern and central regions, almost the same, were 21.80% (95% CI 18.00 to 26.30%) and 22.00% (95% CI 11.70 to 41.30%), respectively. The western region showed a relatively high attack rate of 30.70% (95% CI 18.10 to 52.30%). The pooled class attack rate of outbreaks with an index case case-finding interval of 2 months or less was 22.00% (95% CI 17.30 to 28.00%), and the rate for outbreaks with an index case case-finding interval of more than 2 months was 22.50% (95% CI 17.30 to 29.30%). The data were further divided into subgroups based on the number of cases in the outbreak. The class attack rate of outbreaks with 10 or more cases was 30.50% (95% CI 25.30 to 36.70%), and that of outbreaks with fewer than 10 cases was 13.40% (95% CI 11.10 to 16.20%) (see details in Additional file 3).
Prevalence of LTBI among students in mainland in China, 2000–2017
The pooled total prevalence of LTBI in 81 outbreaks was 20.50% (95% CI 16.90 to 24.80%). Subgroup analysis showed that the pooled total prevalence of LTBI in the group (induration≥15 mm) was 22.80% (95% CI 17.00 to 30.60%), and that of the group (induration≥20 mm) was 18.60% (95% CI 14.40 to 24.00%). Additionally, the pooled total prevalence of LTBI in outbreaks with 10 or more cases was 17.40% (95% CI 12.00 to 25.20%), and the total prevalence of LTBI in outbreaks with fewer than 10 cases was 22.20% (95% CI 17.70 to 27.90%).
The pooled prevalence of LTBI among close contacts in 73 outbreaks was 23.70% (95% CI 19.50 to 28.90%). Subgroup analysis showed that the pooled prevalence of LTBI among close contacts of the group (induration≥15 mm) was 27.60% (95% CI 20.40 to 37.30%), and that of the group (induration≥20 mm) was 21.70% (95% CI 16.10 to 29.40%). Furthermore, the pooled prevalence of LTBI among close contacts in outbreaks with 10 or more cases was 27.50% (95% CI 21.80 to 34.80%), and the prevalence in outbreaks with fewer than 10 cases was 18.80% (95% CI 13.50 to 26.20%).
Factors associated with TB outbreaks, 2000–2017
Meta regression showed that the type of outbreak school, the region where the outbreak school was located, and the outbreak duration were correlated with the total attack rate of outbreaks (B1 = 0.37, p1 < 0.05; B2 = -0.31, p2 < 0.05, B3 = 0.22, p2 < 0.05); the type of outbreak school and the outbreak duration were correlated with the prevalence of LTBI (B4 = -0.34, p4 < 0.05; B5 = 0.16, p5 < 0.05); and only the outbreak duration was correlated with the class attack rate (r6 = 0.24, p6 < 0.01).
Interventions for TB outbreaks, 2000–2017
We identified five main interventions for TB outbreaks. Eighty 80 (74.80%) outbreaks were addressed with an intervention that used standardized management and treatment of confirmed cases and implemented a school strict rehabilitation system. A total of 75 (70.10%) outbreaks conducted PPD testing and X-ray examinations of close contact students and provided prophylaxis for strongly positive students. Ventilating the classroom and dormitory more frequently and timely disinfecting were reported in 73 (68.20%) outbreaks. A total of 70 (65.40%) outbreaks carried out health education for teachers and students through health education courses, publicity panels, blackboard newspapers, leaflets and other methods. Moreover, 33 (30.80%) outbreaks took measures that involved monitoring and reporting the TB epidemic, strictly implementing morning inspections, tracking absenteeism due to the disease, and reporting cases in a timely manner.
Discussion
This study was the first review to systematically analyze the epidemiological characteristics of school TB outbreaks in China. The pooled total attack rate of Chinese school TB outbreaks in the most recent 17 years was 4.60%, with 16.8 cases per outbreak. The pooled total prevalence of LTBI was 20.50% among the screened population. The pooled class attack rate was higher, at 22.70%. The median duration of outbreaks was 3 months, with a range of 1 month to 18 months. Additionally, the median case-finding interval for index cases was 2 months, which was higher compared with other studies [121, 129, 130].
In our meta-analysis, the attack rate was approximately much higher than the prevalence of active PTB according to the Fifth National Tuberculosis Epidemiology Survey and the average level of prevalence of student PTB in China [5, 8]. According to the 2018 TB report, the total TB incidence among general population in China was 88.9/100,000, which are also lower than the pooled attack rate reported in our review [3]. The high attack rate was probably due to the exposure to source of the infection in a closed environment. In addition to schools, there were also many other places with reported TB outbreaks, such as prisons and factories. According to research conducted in China and abroad, the prevalence of tuberculosis in prison is lower than that in outbreak schools included in our review [131,132,133,134] but higher than that among the general population [5]. All the results indicated that there was a high risk of TB in the closed places and clustering groups. More measures should be taken to reduce the risk of TB infection in such settings. The pooled prevalence of LTBI among close contacts (27.60%, TST ≥ 15 mm) was higher than the prevalence of LTBI among the general population worldwide (23%) [135] and in rural areas (19%, TST ≥ 15 mm) [136]. The prevalence of LTBI among school TB outbreaks was still higher than the study conducted by WL Meng, who reported a prevalence of 25.8% (TST ≥ 15 mm) over 5 outbreaks [137]. Furthermore, the prevalence of LTBI among students in our review was also higher than that reported in other countries [138,139,140,141]. For example, E. G. Teixeira et al demonstrated that the prevalence of LTBI among undergraduate students in Italy was 6.9% (TST ≥ 10 mm) [141]—far lower than our results. The basic TB burden in China was much heavier than Italy may partially explain the inconsistency [142, 143]. The meta-analysis also presented that the pooled total attack rate appeared to be higher than the attack rate in the eastern provinces or cities of China such as Beijing and Dalian [137, 144].
According to previous studies, the prevalence of active pulmonary tuberculosis in western provinces of China was higher than that in eastern provinces of China [5, 145]. Therefore, the higher attack rate of school TB outbreaks in the western region might result in a higher total attack rate among general population. However, we also found that far more outbreaks reported in eastern China than that in western China. This difference could be explained by the fact that researchers in the eastern provinces of China published articles more frequently than researchers in the western provinces. Notably, our estimate of the attack rate at universities was higher than that at senior middle schools, while the number of patients was highest at senior middle schools.. The outbreaks at senior middle schools mainly involved students in grade 12, who have the intensive burden of studying to prepare for college entrance tests [146, 147]. Hence, target actions should be taken for outbreaks at senior middle schools and universities. Our review also found that winter and spring seemed to be the two seasons for more frequent student TB outbreaks. The spring and winter peaks of student tuberculosis outbreaks could be the result of long-term contact in poorly ventilated rooms [148, 149].
Tracking and investigating index cases is a significant part of an epidemiological investigation of an outbreak. The results showed that the M:F ratio of all index cases was 3:1, which was much higher than that reported by the WHO and other studies [3, 150]. However, the M:F ratio among all student TB patients in our review was approximately 1.59:1, far lower than that of the index cases. This finding suggest that male students are more likely to be a potential source of infection because men have poorer health-seeking behaviors than women [151]. However, when males and females are exposed to the same source of an infection within the same closed space, the gender difference in TB susceptibility was not so obvious.
The case-finding interval of the index case is a significant factor in attack rate [152]. Through a subgroup analysis of the class attack rate based on the case-finding interval, we discovered that patients with a case-finding delay showed a relatively high class attack rate compared to those without a case-finding delay. A longer interval leads to greater opportunity of TB infection in the same space. Moreover, patients who were delayed in detection were more likely to develop severe pulmonary tuberculosis and increase the susceptibility among close contacts [121, 130]. The median time interval from the report of the first case to the emergence of the secondary case was 4 months, which indicated that this period could be recognized as a time window for timely interventions to prevent the occurrence of secondary cases.
According to the patient summary in our review, we found that only 16.70% of cases were reported to be sputum smear positive, while 83.30% of index cases were sputum smear positive. This finding suggests that the index cases were more contagious than subsequent cases. Therefore, it is necessary to isolate the source of the infection in a timely manner [153, 154]. Complete prophylaxis could greatly reduce the possibility of the subsequent activation and spread of tuberculosis [155, 156]. In our review, a total of the 2398 close contacts with strongly positive PPD test results had received prophylaxis, only 68.59% finished the six-month prophylaxis. The results also showed that there remains a shortage of knowledge concerning TB prevention and treatment among students. Therefore, health education regarding prophylaxis should be strengthen in more effective ways to ensure they exactly completed the six-month course of therapy.
We found a positive correlation between the outbreak duration and the TB attack rate, the prevalence of LTBI and class attack rate, which indicates that longer-lasting epidemics result in a more infectedstudents in the outbreak. Furthermore, we found that in areas from east to west, the prevalence of LTBI decreased while as previous studies have reported, the burden of tuberculosis is heavier in Western China than in Eastern China [157, 158]. A possible explanation for this result is that the sample size was too small when assessing the prevalence of LTBI in Western China.
We synthesized the interventions for school TB outbreaks that were reported in the included studies. Our review showed that few outbreaks (33/107) involved interventions that monitored the TB epidemic and implemented strict morning inspections, which suggests that schools should strengthen their epidemic monitoring and disease absence tracking abilities.
Limitations
Our review had some limitation. Firstly, due to the geographical limitation of the search area on the mainland of China, the results may not be extrapolated to other regions and continents. Secondly, apart from the studies that our review included or excluded, there are still many outbreaks not published, especially in the western parts of China. This lack of coverage may have partially affected our conclusions. Moreover, some of the included studies had incomplete information concerning outbreaks led to information loss. Thirdly, most of the articles we included in our review were case reports from different settings and the infection source from some open universities might be multiple which may cause heterogeneity. Finally, due to the equipment inadequacy and technical deficiency of low level TB laboratories over the last decade in China, there were different diagnostic methods used among the included studies. Although we conducted subgroup-analysis, meta-regression to explain and reduce heterogeneity, it’s still hard to avoid.
Conclusion
In conclusion, school TB outbreaks were more frequently reported at senior middle schools in China. The attack rates of outbreaks at universities or colleges were higher than those at senior middle schools, and the attack rate of class contacts was higher in the western provinces of China than that in the eastern provinces of China. Longer duration of case-finding was correlated with the severity of the outbreak. There was an urgent need to reduce case-finding delays in index cases to reduce the spread in classes and schools. Relevant departments and institutions should strengthen active case-finding measures such as monitoring and screening for presumptive TB cases in schools in order to prevent school outbreaks in early stage.
Availability of data and materials
The key information generated and/or analyzed during this study are included as the additional files in this publication.
Abbreviations
- CDC:
-
Centers for Disease Control
- CI:
-
Confidence interval
- LTBI:
-
Latent tuberculosis infection
- M:F:
-
Male:female
- PPD:
-
Purified protein derivatives tuberculin
- PTB:
-
Pulmonary tuberculosis
- TB:
-
Tuberculosis
- TST:
-
Tuberculin skin test
References
Listed N. Tuberculosis global facts 2010/2011. Cent Eur J Public Health. 2010;18(4):197.
Sheet F, Ten THE, Causes L, Death OF, Broad BY, Group I: The Top Ten Causes of Death. 2007.
WHO: Global tuberculosis report 2018. http://www.who.int/tb/publications/global_report/en/. Accessed sept 2018.
Zhen YC, Geng H, Zhou CC, Liu ZM, Xu LZ, Li CJ, Sun L. Use of tuberculosis control institution service among tuberculsis patients in floating population and its influencing factors. Chin J Public Health. 2010;26(2):157–8 (In Chinese).
Wang LX, Cheng SM, Chen MT, Zhao YL, Zhang H, Jiang SW, He GX, Lv Q, Du X, Chen W. The fifth national tuberculosis epidemiological survey in 2010. Chin J Antituberc. 2012;34(8):485–508 (In Chinese).
Zhang S, Li X, Zhang T, Fan Y, Li Y. The experiences of high school students with pulmonary tuberculosis in China: a qualitative study. BMC Infect Dis. 2016;16(1):758.
National Bureau of Statistics of the People’s Republic of China: China statistical yearbook 2017. http://www.stats.gov.cn/tjsj/ndsj/2017/indexeh.htm. Accessed Oct 2018.
Chen W, Chen QL, Xia YY, Cheng SM. Analysis of the characteristics of national TB epidemic situation in schools from 2008 to 2012. Chin J Antituberc. 2013;35(12):949–54 (In Chinese).
Association NTC. Guidelines for the investigation of contacts of persons with infectious tuberculosis. Recommendations from the National Tuberculosis Controllers Association and CDC. MMWR Recomm Rep. 2005;54(RR-15):1.
Mitruka K, Oeltmann JE, Ijaz K, Haddad MB. Tuberculosis outbreak investigations in the United States, 2002-2008. Emerg Infect Dis. 2011;17(3):425–31.
National Health Commission of the People’s Republic of China: Regulation for school tuberculosis prevention and control (2017 version). http://www.nhfpc.gov.cn/jkj/s7914/201707/4d2f57086b65450c8f674bf07323b9ad.shtml. Accessed June 2017.
Chen W, Xia Y, Li X, Zhou L, Li C, Wan K, Cheng S. A tuberculosis outbreak among senior middle school students in China in 2011. J Int Med Res. 2012;40(5):1830–9.
Outbreak of tuberculosis in Taojiang, Hunan Province: 90 suspected cases of suspected cases of 10 cases. http://new.qq.com/cmsn/20171125/20171125011661.html. Accessed 25 Nov 2017. (In Chinese).
Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred reporting items for systematic reviews and Meta-analyses: the PRISMA statement. Revista Española De Nutrición Humana Y Dietética. 2009;18(3):889–96.
Middle school. https://en.wikipedia.org/wiki/Middle_school.html. Accessed 5 June 2018.
Education in China. https://en.wikipedia.org/wiki/Education_in_China#Senior_secondary.html. Accessed 5 June 2018.
University. https://en.wikipedia.org/wiki/University#Around_the_world.html. Accessed 5 June 2018.
Zhan SY. Epidemiology. The seventh edition. Beijing: People’s Medical Publishing House; 2012.
Zhou JQ. Pulmonary tuberculosis diagnostic criteria. Tuber Health Educ. 2008;1:7–9.
Health and Family Planning Commission of the People's Republic of China. WS 288—2017 Pulmonary tuberculosis diagnosis(instead of WS 288—2008), 2017. (In Chinese).
Qi Y, Lu HY, Yang LJ, Yang YT, Zhou Y, Lu XW. The retrospective analysis of a tuberculosis outbreak in a middle school. J Tuberc Lung Health. 2014;3(3):161–5 (In Chinese).
Chen MS, Jin CQ, Shao JP. Epidemiological investigation of an outbreak of tuberculosis in a school. China Prev Med. 2009;10(07):675–6 (In Chinese).
Ding JM, Han WC, Zhang J, Pang HB. A survey and disposal of an outbreak of pulmonary tuberculosis among students. Occup Health. 2002;18(11):71–2 (In Chinese).
Yang ML, Zhang SS. Epidemiological analysis of an outbreak of tuberculosis among college students. J Med Pest Control. 2012;28(10):1168–71 (In Chinese).
Xue CH, Sun BB. An investigation and analysis of tuberculosis outbreak in middle school students. Chin J Sch Doct. 2012;26(05):370–1 (In Chinese).
Mao GH, Yu M, Lin X. Epidemiological investigation of a tuberculosis outbreak in a middle school in Ningbo City. Mod Pract Med. 2013;25(05):566–7 (In Chinese).
Xia XJ, Jiang H, Luo WH, Dai B. Analysis of an outbreak of tuberculosis in a university in Jiangsu. Mod Prev Med. 2013;40(21):4082–4 (In Chinese).
Tian YT, Li Z, Xiong XH. The investigation and disposal of tuberculosis outbreak in a senior high school student in Yubei District. Pract Prev Med. 2011;18(10):1886–7 (In Chinese).
Yu DH, Du CN, Li Y. Investigation of an outbreak of tuberculosis in a middle school in Weihai City. Lit Inf Prev Med. 2003;9(05):554 (In Chinese).
Hu G, Zhang JX, Jiang DM. An investigation on collective infection of tuberculosis in a university. Occup Health. 2004;20(07):80 (In Chinese).
Li DH, Liu T. Investigation and analysis of an outbreak of pulmonary tuberculosis in a rural middle school. Chin Prim Health Care. 2005;19(12):57 (In Chinese).
Jiang XD. An investigation of tuberculosis outbreak among senior middle school students in Zhejiang Province. Chin J Sch Health. 2006;27(05):453 (In Chinese).
Luo KY, Liao SJ, Wang XF, Li HH, Jiang LN, Gui B, Zhang HY, Li J, Cheng DJ. Analysis of an outbreak of tuberculosis in schools. Pract Prev Med. 2006;13(04):939–40 (In Chinese).
Wu LM, Luo J, Lu M, Wang L, Hu ZQ, Wang M. Analysis of an outbreak of TB in an university in Hangzhou. J Med Res. 2006;35(06):61–3 (In Chinese).
Hao J, Tan HM, Xie YZ, Zhang M. Investigation on the prevalence of tuberculosis among students in a secondary school in Pingyin County in 2006. Prev Med Tribune. 2007;13(05):476 (In Chinese).
Lin BC, Huang SH. An investigation of tuberculosis outbreaks among high school students. Occup Health. 2007;23(14):1231–2 (In Chinese).
Lv QQ, Ju YX, Li YY. Investigation of an outbreak of tuberculosis among college students. Chin J Sch Health. 2007;28(12):1147 (In Chinese).
Zhong CQ. An on-campus tuberculosis outbreak investigation and disposal. Chin J Pest Control. 2008;24(08):604–5 (In Chinese).
Wang YH. Analysis of an outbreak of tuberculosis in a certain university. Chin J Sch Doct. 2009;23(05):540–1 (In Chinese).
Yin W, Xue H, Zhang CG. Analysis of an outbreak of tuberculosis in a certain university. Jiangsu J Prev Med. 2009;20(02):45–6 (In Chinese).
Cheng ZX, Hu LJ, Fang YR, Li YX, Wang R. Epidemiologic survey on tuberculosis outbreak which happened at a high school in Wuhu. World J Infect. 2010;10(4):195–8 (In Chinese).
Cui QR, Ge JH, Pang MW, Chen YL, Xie WF. Survey of a school cluster of pulmonary tuberculosis. Dis Surveil. 2010;25(04):335–7 (In Chinese).
Fu GX, Shao YX, Chen H. Epidemiological investigation of an outbreak of tuberculosis among college students. Chin J Sch Health. 2010;31(02):244–5 (In Chinese).
Weng YF, Zhang JY. Survey of a tuberculosis epidemic in a university in Zhoushan city, Zhejiang province. Dis Surveil. 2010;25(10):842–3 (In Chinese).
Yang XP, Yang SJ. Analysis of an outbreak of tuberculosis in a school. Chin J Sch Health. 2010;31(09):1144 (In Chinese).
Zheng LX, Long HP, Zheng SJ, Xiao ML, Li B. Epidemiological investigation after tuberculosis outbreak in a middle school. Pract Prev Med. 2010;17(04):672–3 (In Chinese).
Guo XY, Shang XS, Fan J. Investigation and analysis of a tuberculosis outbreak. J Public Health Prev Med. 2011;22(05):98–9 (In Chinese).
Hu DB, Wang B. Epidemiological investigation of outbreaks of tuberculosis in schools. Shanghai J Prev Med. 2011;23(02):54–5 (In Chinese).
Hu YQ, Shen SQ, Jiang W. A school tuberculosis cluster epidemic survey. Zhejiang J Prev Med. 2011;23(05):43–4 (In Chinese).
Zhao XP, Zhang TH. Investigation and disposal for clustered tuberculosis cases in a professional technology college. Occup Health. 2011;27(24):2912–3 (In Chinese).
Chen QP, Chen TM, Zhao HW. Assessment on investigation and control measures of tuberculosis outbreaks in college. Chin J Sch Health. 2012;33(02):172–173,176 (In Chinese).
Fu YY, Zhang GQ, Wei WL, Zhang YH, Shang J, Zhong D. Epidemiological analysis of tuberculosis outbreak among internship students in a vocational and technical college. Chin J Sch Health. 2012;33(05):621–2 (In Chinese).
Hu HW, Liu ML. Investigation report on pulmonary tuberculosis aggregation on campus. Anhui J Prev Med. 2012;18(04):299–300 (In Chinese).
Peng LR, Zhang L, Peng R. Tuberculosis outbreak in Kangding middle school. China Pract Med. 2012;7(26):250–1 (In Chinese).
Shen TY, Li JY, Fu LJ. Investigation and analysis of a clustered pulmonary tuberculosis case in a school in Shaoxing county. Chin Rural Health Serv Adm. 2012;32(09):937–9 (In Chinese).
Wang LG, Zhu JW. Investigation of a tuberculosis outbreak in a school. Zhejiang J Prev Med. 2012;24(05):46–7 (In Chinese).
Zhu XC, Ying XJ, Wang Y, Weng LX, Qiu L. Investigation of pulmonary tuberculosis outbreak in a school. Chin J Sch Health. 2012;33(04):453–4 (In Chinese).
Chen JY, Shi SJ, Fang XH, Pan Y. Report on the investigation and disposal of a tuberculosis outbreak in a middle school in Jing County. Anhui J Prev Med. 2013;19(01):35–6 67. (In Chinese).
Huang G, Zhou XT, Zhang CM. Field epidemiological investigation on TB outbreak in a middle school of Shaoxing City. Occup Health. 2013;29(02):124–257 (In Chinese).
Ji W. Investigation of tuberculosis outbreaks in Tibetan classes in a child care school. Jiangsu Health Care. 2013;15(04):7–8 (In Chinese).
Wu HZ, Hu YQ. An investigation of tuberculosis cluster infection in high school students. Zhejiang J Prev Med. 2013;25(04):46–7 50. (In Chinese).
Zhao SJ, Zhang YQ, Guo JH. Investigation and analysis of an outbreak of tuberculosis in a school. Shanxi Med J. 2013;42(12):1368–9 (In Chinese).
Zhu J, Fan FN, Xu JY. Investigation on the outbreak of tuberculosis aggregation in senior three students. Chin J Sch Health. 2013;34(06):748–9 (In Chinese).
Chen QF, Gao HQ. Investigation on tuberculosis aggregation in a middle school. Zhejiang J Prev Med. 2014;26(08):824–6 (In Chinese).
Ding SN, Sun ZP, Li C, Nie JQ, Liu R, Liu X, Ji W. Epidemiologic survey on an outbreak of tuberculosis in a school in Jiangsu. Mod Prev Med. 2014;41(07):1164–6 1169. (In Chinese).
Ding SN, Sun ZP, Li C, Nie JQ, Liu R, Liu X, Zang TY. Epidemiologic survey of an outbreak tuberculosis in a university in Nanjing City. Chin J Sch Doct. 2014;28(02):124–126,128 (In Chinese).
Huang XQ, WY WU, Huang LM. Tuberculosis aggregation report in middle schools in a mountainous area. Zhejiang J Prev Mede. 2014;26(11):1143–4 (In Chinese).
Jiang WY, Shao JP, Lin BC. Investigation on tuberculosis aggregation in high school student in Wenling City. Chin J Sch Health. 2014;35(07):1097–9 (In Chinese).
Kong W, Ding XY, Lu W, Liu Q. Investigation on pulmonary tuberculosis in a middle school in Jiangsu Province. Jiangsu J Prev Mede. 2014;25(04):54–5 (In Chinese).
Wang B, Wang ZG, Gu MX, Zheng JJ, Yu YJ. Epidemiological investigation of tuberculosis aggregation in a school. Chin J Sch Health. 2014;35(08):1253–4 (In Chinese).
Wang Y, Yang SQ, Luan H, Liu XY. Investigation and analysis of pulmonary tuberculosis epidemics among college students. Chin J Health Lab Technol. 2014;24(03):432–4 (In Chinese).
He YJ, Huang MP, Cao Y, Liang ZQ. Analysis of a pulmonary tuberculosis outbreak and follow-up of 3 years in a school. J Med Theory Pract. 2015;28(13):1810–1 (In Chinese).
Ren C, Gao L, Huang SY, Deng YR, Ying LP. Investigation and analysis of tuberculosis aggregation in a school. Mod Pract Med. 2015;27(08):1025–6 (In Chinese).
Shi YF, Miao C, Shen XL. Investigation report on tuberculosis aggregation in a vocational middle school. Zhejiang J Prev Med. 2015;27(02):164–6 (In Chinese).
Wang DM, Wang JX, Wang XL. Analysis of tuberculosis aggregation in a university. Chin J Coal Ind Med. 2015;18(12):2086–9 (In Chinese).
Wang W, Zhou W, Lou MJ, Chen HJ. Investigation on tuberculosis aggregation in a university in Ningbo city. Shanghai J Prev Med. 2015;27(11):702–703,708 (In Chinese).
Zhu J, Gu YX, Zhang YG. An investigation report on an outbreak of tuberculosis in schools. Med Forum. 2015;19(07):995–7 (In Chinese).
Cui LC, Mu PH. Investigation and analysis of tuberculosis aggregation in colleges and universities. Chin J Antituberc. 2016;38(1):74–6 (In Chinese).
Song JS, Liu YJ. A school TB epidemiological investigation and disposal. World Latest Med Inf. 2016;16(60):183,188 (In Chinese).
Tang WJ, Yang WQ, He FH, Feng DZ. Investigation on tuberculosis aggregation in a middle school in Jinhu County. Jiangsu J Prev Med. 2016;27(03):317–8 (In Chinese).
Wang YB, Zhao X. An epidemiological investigation of tuberculosis aggregation in a school in Xinle City. J Med Pest Control. 2016;32(12):1413–4 (In Chinese).
Xu H, Sun B. Report on a pulmonary tuberculosis cluster epidemic occurred in a senior high school, Donghai County. Mod Prev Med. 2016;43(17):3217–20 (In Chinese).
Yang NZ, Chen Y, Yang WY, Wang SS, Ni Z. An analysis of tuberculosis clustered outbreaks in schools. Prev Med. 2016;28(11):1146–9 (In Chinese).
Yang XT, Xiang LH, Liu XF, Wang N, Ma Y, Hu WH, Cao M. An epidemiological investigation of a tuberculosis outbreak in a university in Shanghai. Chin J Sch Health. 2016;37(12):1902–4 (In Chinese).
Zheng J. Investigation and interventions on an outbreak of tuberculosis. China Trop Med. 2016;16(02):184–5 189. (In Chinese).
Hong YD, Xue FH, Chen Q. Investigation on the pulmonary tuberculosis epidemics in a vocational school. Chin Rural Health Serv Adm. 2017;37(02):169–71 (In Chinese).
Fang Y, Zhang L, Tu C, Ye D, Fontaine R, Ma H, Hao J, Fu L, Ying X, Chen Q, et al. Outbreak of pulmonary tuberculosis in a Chinese high school, 2009-2010. J Epidemiol. 2013;23(4):307–12.
Ji M, Chen J, Zhu W, Zhou Y. Investigation and analysis of a tuberculosis epidemic in middle school. Chin J Antituberc. 2013;35(11):941–3 (In Chinese).
Pang XW, Zhang D, Fu YY. Analysis of screening results of close contacts after tuberculosis outbreak in a school. Chin J Sch Health. 2015;36(8):1265–7 (In Chinese).
Zhu XC, Ying XJ, Wang Y, Weng LX, Qiu L. Investigation and disposal of pulmonary tuberculosis aggregation in a school, vol. 5. Shaoxing: The 19th Zhejiang Rural Health Reform and Development Conference; 2011. (In Chinese)
Qin TX, Yin N, Zhao RX. Analysis of tuberculosis aggregation in a school. Chi J Sch Doct. 2015;29(03):193–4 (In Chinese).
He XX, Luo P, Li B, Gao ZD. Surveillance and disposal of tuberculosis in a certain university in Beijing. Chin J Antituberc. 2014;36(12):1101–4 (In Chinese).
Wang ZF. Investigation of tuberculosis outbreak in a middle school in Rongcheng City. Lit Inf of Prev Med. 2002;8(01):26 (In Chinese).
Wang L, Wu LM, Lu M, Hu ZQ, Zhang YZ. An investigation of outbreak of tuberculosis among students and countermeasures. Chin J Sch Health. 2003;24(05):539–40 (In Chinese).
Fan C, Hu DY, Zhou KX, Su Q. Analysis of 24 cases of tuberculosis in a third grade in a middle school in Chongqing. Chongqing Med. 2007;36(19):2004–5 (In Chinese).
Guo SY, Liang MH, Qiao HY, Zheng FF. A clustered tuberculosis epidemic investigation report. Henan J Prev Med. 2014;25(04):302–3 316. (In Chinese).
He BS, Dai XP, Xiang QH, Li SC, Chen H, Wang J, Hu XQ, Guo YX, Yu HH. Report on the investigation and disposal of tuberculosis outbreak in the first middle school in Xiaogan City. Chin J Antituberc. 2009;31(11):668–71 (In Chinese).
Xie QG, Li ZX. Epidemiological survey of tuberculosis among middle school students. Med Innov China. 2012;9(10):102–3 (In Chinese).
Jin SF. An analysis of tuberculosis epidemic in colleges and universities. Dandong Med. 2005;3:37 (In Chinese).
Li AH. An investigation report of a tuberculosis outbreak. Occup Health. 2004;20(06):88 (In Chinese).
Li JC. Analysis of tuberculosis outbreak in schools. Chin Community Doct. 2012;14(16):399–400 (In Chinese).
Li PP, Zhang HL, Wan CG. Investigation and handling of the epidemic situation of tuberculosis in a middle school in Yandu District of Yancheng City. Occup Health. 2008;24(07):672–3 (In Chinese).
Li RY, Wang SP, Yu JP. Epidemiological survey of tuberculosis clusters in a school in Weihai City. Prev Med Tribune. 2011;17(12):1121–3 (In Chinese).
Liu YJ, Liu CS, Wang GY, Li HB, Pan P, Nie JS, Yang YL. Epidemic investigation and disposal of tuberculosis outbreak in a high school in Chaoyang City, Liaoning Province. J Trop Dis Parasitol. 2007;5(1):49–51 (In Chinese).
Piao YN, Jin H. Disposal and analysis of tuberculosis outbreak in a high school in Hunchun. J Chin Antituberc Assoc. 2008;30(02):149–50 (In Chinese).
Qin LL. Investigation and analysis of tuberculosis outbreak in a high school. Chin J Sch Doct. 2011;25(7):526,528 (In Chinese).
Wang QZ, Fang XH. Site investigation and analysis of a tuberculosis outbreak in a high school. J Anhui Health Vocational Tech Coll. 2012;11(04):101–2 108. (In Chinese).
Wang HZ, Chang JH, Li PJ. An epidemiological investigation of tuberculosis outbreaks in schools. Chin J Sch Health. 2015;36(04):618–9 (In Chinese).
Wang ML, Li XP, Zhao W, Wang FY. School tuberculosis epidemiological investigation and interventions. J Qiannan Med Coll Nationalities. 2006;19(1):37–8 (In Chinese).
Wang WB. Investigation of tuberculosis outbreak in a high school student in Gansu Province. Chin J Sch Health. 2005;26(11):74 (In Chinese).
Xu K, Zheng LL. Epidemiological analysis of an outbreak of tuberculosis in a high school. China Mod Doct. 2015;53(05):118–20 (In Chinese).
Yang SB, Li Q, Miao ZP. An outbreak of tuberculosis among school students. Chin J Sch Health. 2004;25(06):750 (In Chinese).
Yang YC. Survey on tuberculosis outbreak at a boarding school in Hongyuan County. J Prev Med. 2008;24(09):742–3 (In Chinese).
Yu DX, Liu JW. Epidemiological survey on a tuberculosis outbreak in a military academy. Mod Prev Med. 2016;43(06):1124–6 1141. (In Chinese).
Yu GP. An investigation and disposal of an outbreak of tuberculosis in schools. Strait J Prev Med. 2009;15(02):40–1 (In Chinese).
Zhang XM, Zeng LC, Du XL, Wang XL, Han YL, Wang CJ. An epidemiological survey of tuberculosis outbreaks in secondary schools. Occup Health. 2007;23(01):33–5 (In Chinese).
Zhang JH, Yang HT, Zhang YM, Yu AF, Chen YH, Wang F, Chen LY. Investigation and disposal of a tuberculosis epidemic in a school. Zhejiang J Prev Med. 2007;19(12):28 31. (In Chinese).
Zhao DY, Wang MQ, Wang XL, Zhou LP, Luo JM, Yang CF, Wang XJ, Liu X, Pi Q. Epidemiological investigation of a tuberculosis outbreak among senior high school students. J Public Health Prev Med. 2013;24(5):90–2 (In Chinese).
Zhao RX. Investigation and analysis of an outbreak of pulmonary tuberculosis in a university. Med Inf. 2013;26(10):383 (In Chinese).
Zhou S, Chen M. Epidemiological survey of the breakout of pulmonary tuberculosis on a campus of a university in Chongqing. Health Med Res Pract Higher Inst. 2005;2(02):7–10 (In Chinese).
Ying QD. An epidemiological survey of tuberculosis outbreaks in middle schools in Yiwu city. Chin Rural Health Serv Adm. 2018;38(7):923–4 (In Chinese).
Yin CL, Zhang H, Cheng Y. Investigation on a cluster outbreak of tuberculosis among students in a middle school in Dazhou. J Prev Med Inf. 2018;34(9):1177–80 (In Chinese).
Xu XD. Investigation and analysis of a tuberculosis epidemic in a university in Yixing. Chin Community Doct. 2018;34(34):178–9 181. (In Chinese).
Wang ZP. Investigation and treatment of tuberculosis epidemic in a middle school in Feng County. Chin J Sch Doct. 2017;31(5):358–9 (In Chinese).
Tang J. Monitoring and management for clustering epidemics of tuberculosis colleges of Liuzhou. Master dissertation: Guangxi Med Univ. 2017:1–47. (In Chinese)
Li J, Zhu XM, Shan ZL, Zhang SL, Mao LQ, Niu YY. Investigation and analysis of a cluster of tuberculosis epidemics in a school. Chin Rural Health Serv Adm. 2017;37(8):1–1 (In Chinese).
Gao CM, Li HY, Ma YX, Jing ZJ, Wang LG, Qin FJ, Liu YD, Tong LB. Epidemiological survey of a clustering infection with pulmonary tuberculosis in a University in Jinan. J Prev Med Chin People’s Liberation Army. 2018;36(10):1231–4 (In Chinese).
Verhagen LM, Kapinga R, van Rosmalen-Nooijens KA. Factors underlying diagnostic delay in tuberculosis patients in a rural area in Tanzania: a qualitative approach. Infection. 2010;38(6):433–46.
Osei E, Akweongo P, Binka F. Factors associated with DELAY in diagnosis among tuberculosis patients in Hohoe Municipality, Ghana. BMC Public Health. 2015;15:721.
Sreeramareddy CT, Panduru KV, Menten J, Van den Ende J. Time delays in diagnosis of pulmonary tuberculosis: a systematic review of literature. BMC Infect Dis. 2009;9:91.
Schwitters A, Kaggwa M, Omiel P, Nagadya G, Kisa N, Dalal S. Tuberculosis incidence and treatment completion among Ugandan prison inmates. Int J Tuberc Lung Dis. 2014;18(7):781–6.
Winetsky DE, Almukhamedov O, Pulatov D, Vezhnina N, Dooronbekova A, Zhussupov B. Prevalence, risk factors and social context of active pulmonary tuberculosis among prison inmates in Tajikistan. PLoS One. 2014;9(1):e86046.
Ali S, Haileamlak A, Wieser A, Pritsch M, Heinrich N, Loscher T, Hoelscher M, Rachow A. Prevalence of pulmonary tuberculosis among prison inmates in Ethiopia, a cross-sectional study. PLoS One. 2015;10(12):e0144040.
Xiong CF, Zhou LP, Wang MQ, Li AG, Sha S, Liu X, Wang XJ, Ding X, Liu XJ. Cross-sectional survey on pulmonary tuberculosis in two prisons of Huhei. Chin J Antituberc. 2012;34(05):289–92 (In Chinese).
Campos-Outcalt D. Screening for tuberculosis: updated recommendations. J Family Pract. 2017;66(12):755–7.
Gao L, Lu W, Bai L, Wang X, Xu J, Catanzaro A, Cardenas V, Li X, Yang Y, Du J, et al. Latent tuberculosis infection in rural China: baseline results of a population-based, multicentre, prospective cohort study. Lancet Infect Dis. 2015;15(3):310–9.
Meng WL, Wang FH, Wang CM, Hu JK. The prevalence of contacts of 5 tuberculosis epidemic in Beijing Xicheng city. Chin J Sch Health. 2017;38(8):1264–6 (In Chinese).
Mumpe-Mwanja D, Verver S, Yeka A, Etwom A, Waako J, Ssengooba W, Matovu JK, Wanyenze RK, Musoke P, Mayanja-Kizza H. Prevalence and risk factors of latent tuberculosis among adolescents in rural eastern Uganda. Afr Health Sci. 2015;15(3):851–60.
Durando P, Alicino C. Latent tuberculosis infection among a large cohort of medical students at a teaching hospital in Italy. 2015;2015:746895.
Kato S, Kuwabara K. Lessons learned from tuberculosis outbreak cases. Biomed Res Int. 2014;89(2):77–88.
Teixeira EG, Menzies D, Comstock GW, Cunha AJ, Kritski AL, Soares LC, Bethlem E, Zanetti G, Ruffino-Netto A, Belo MT, et al. Latent tuberculosis infection among undergraduate medical students in Rio de Janeiro state, Brazil. Int J Tuberc Lung Dis. 2005;9(8):841–7.
Schiroli C, Carugati M, Zanini F, Bandera A, Di Nardo SS, Monge E, Morosi M, Gori A, Matteelli A, Codecasa L, et al. Exogenous reinfection of tuberculosis in a low-burden area. Infection. 2015;43(6):647–53.
Mammina C, Bonura C, Barchitta M, Quattrocchi A, Palermo M, Agodi A. Tuberculosis surveillance in Sicily, Italy. Epidemiol Prev. 2014;38(6 Suppl 2):83–7.
Wang T. Analysis of the characteristics of TB epidemic situation in school in a city in 2011–2016. Master dissertation. Liaoning: Dalian Medical University; 2017. (In Chinese)
Xia YY, Du X, Chen W, Zhang H, Liu XQ, Li X, Jiang SW, Wang LX, Cheng SM. Pulmonary tuberculosis prevalence among different regions in China in 2010. Chin J Antituberc. 2012;34(12):803–7 (In Chinese).
Gao HQ, Lu QL, Niu WK. Epidemiological analysis of tuberculosis among students in Shaoxing from 2010 to 2014. Chin J Sch Health. 2016;37(5):788–91 (In Chinese).
Shen SQ, Hu YQ. Epidemiological analysis of pulmonary tuberculosis among primary and secondary school students in Jinhua City from 2010 to 2014. Chin Rural Health Serv Adm. 2015;35(8):1013–5.
Luo T, Sumi A, Zhou D, Kobayashi N, Mise K, Yu B, Kong D, Wang J, Duan Q. Seasonality of reported tuberculosis cases from 2006 to 2010 in Wuhan, China. Epidemiol Infect. 2014;142(10):2036–48.
Dogba JB, Cadmus SI, Olugasa BO. Mapping of Mycobacterium tuberculosis cases in post-conflict Liberia, 2008-2012: A descriptive and categorical analysis of age, gender sonal pattern. Afr J Med Med Sci. 2014;43(Suppl):117–24.
Horton KC, MacPherson P, Houben RM, White RG. Sex Differences in Tuberculosis Burden and Notifications in Low- and Middle-Income Countries: A Systematic Review and Meta-analysis. Plos Med. 2016;13(9):e1002119.
Yuceege M, Sanisoglu B, Baran R. Gender difference in clinical presentation of Turkish patients with pulmonary tuberculosis. Acta Med Iran. 2014;52(1):52–5.
Said K, Hella J, Mhalu G, Chiryankubi M, Masika E, Maroa T, Mhimbira F, Kapalata N, Fenner L. Diagnostic delay and associated factors among patients with pulmonary tuberculosis in Dar Es Salaam, Tanzania. Infect Dis Poverty. 2017;6(1):64.
Kaynak S, Bauer C, Richter V, Richter E, Niemann S. Tuberculosis outbreak in 13 people in Saxony-Anhalt: indications of an infection chain by spoligotyping. Gesundheitswesen. 2012;74(6):351–7.
Rubinstein U, Schachter J, Sharon N, Talnir R, Amir J. Tuberculosis in a pair of twins--the use of molecular biology methods for the detection of the source of infection. Harefuah. 2007;146(3):170–2 248.
Tuberculosis. A message from preventive medicine and your physician. Prev Med. 2001;32(2):101–2.
Pitman R, Jarman B, Coker R. Tuberculosis transmission and the impact of intervention on the incidence of infection. Int J Tuberc Lung Dis. 2002;6(6):485–91.
Shi QN, Zhao ZX, Ma JQ. Big data analysis of tuberculosis dynamic surveillance in China. Chin J Health Inf Manag. 2017;14(05):643–8 (In Chinese).
Yu GQ, Lei MZ, Wei Y, Long BS, Chen SY, Tang WY, Zhang ZY, Tan J. Characteristic of spatial-temporal distribution of pulmonary tuberculosis in mainland China from 2004 to 2015. Mod Prev Med. 2017;44(20):3649–54 (In Chinese).
Acknowledgments
Not applicable.
Funding
This study was supported by the National Natural Science Foundation of China (71640019), Zhejiang Provincial Science and Technology Project (GF19H260004), Zhejiang Provincial Medical Research project (2016RCA007 and 2015KYA052) and Zhejiang Provincial Philosophy and Social Science Project (19NDJC243YB).The funding body had no role in the study design, collection, analysis, interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
JMJ, BC conceived, designed the study. BC, KL and HDB led the protocol design, study design, the literature review and data extraction. HDB and ZKW conducted the statistical analysis and wrote the draft. TNH, WW, WF, CLC, XMW and YP help to modify and proofread the article. All the authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Table S1.
The search strategy of our review.
Additional file 2: Figure S1.
Forest plot of total attack rates of different schools, Figure S2. Forest plot of total attack rates of different regions where the outbreaks schools located and Figure S3. Forest plot of total attack rates of different case number.
Additional file 3: Figure S4.
Forest plot of class attack rates of different schools, Figure S5. Forest plot of class attack rates of different regions where the outbreaks schools located, Figure S6. Forest plot of class attack rates of different case number, Figure S7. Forest plot of class attack rates of different diagnose interval of index cases.
Additional file 4:
Table S2. The outcomes of each outbreak for the meta-analysis.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Bao, H., Liu, K., Wu, Z. et al. Tuberculosis outbreaks among students in mainland China: a systematic review and meta-analysis. BMC Infect Dis 19, 972 (2019). https://doi.org/10.1186/s12879-019-4573-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-019-4573-3