Abstract
Background
Making a definite diagnosis of infectious uveitis is a challenging task because many other infectious, and non-infectious uveitis, may have similar non-specific symptoms and overlapping clinical appearances. Co-infections in immunocompetent patients are not frequently proved with traditional serologic-diagnostic tools.
Methods
Descriptive transversal study, in a Uveitis Service of an Ophthalmology Reference Center, in Bogotá, Colombia, from July 2014 to February 2016. Aqueous humor (AH) and/or vitreous fluid, blood and serum samples were collected from consecutive patients suspected of having infectious uveitis. The diagnosis of ocular toxoplasmosis (OT) was confirmed by the Goldmann–Witmer coefficient (GWC) and by polymerase chain reaction (PCR). Differential diagnosis by PCR in AH was done for viral origin such as Cytomegalovirus (CMV), Herpes simplex virus type 1 (HSV1), Herpes simplex virus type 2 (HSV2), Varicella zoster virus (VZV), Epstein-Barr virus (EBV) and Mycobacterium tuberculosis.
Results
In 66 Colombian patients with uveitis of presumed infectious origin: 22 (33.3%) were confirmed as OT, 16 (24.2%) as undetermined OT, five (7.5%) as co-infections and 23 (34.8%) as other uveitis. Toxoplasma coinfection with M. tuberculosis was identified in one case by PCR and in four cases with HSV by GWC. The initial clinical diagnosis changed, after laboratory examination, in 21 cases (31.8%).
Conclusions
Clinical diagnosis can be changed by laboratory examination in a significant proportion of cases of uveitis. Diagnosis of OT should combine the use of PCR and GWC to reach the maximum of confirmation of cases. The use of multiple laboratory methods is necessary to identify co-infections and viral infections that can mimic OT in immunocompetent patients.
Similar content being viewed by others
Background
Toxoplasma gondii is one of the most common human zoonosis, affecting about a third of the world’s population [1]. Around 10% of people that acquire this infection postnatally [2, 3], and up to 80% of children congenitally infected [4, 5], develop ocular toxoplasmosis (OT). This clinical form of toxoplasmosis is the most common etiology of posterior uveitis worldwide [1, 6].
Although in clinical practice a majority of cases of OT are diagnosed by a combination of consistent clinical features and supportive serological results [7], in cases of atypical presentations it is of utmost importance to differentiate OT from other causes of posterior uveitis that share similar clinical characteristics [8,9,10,11,12,13,14].
A definitive diagnosis is only obtained after direct evidence of the presence of the parasite in aqueous humor (AH) by polymerase chain reaction (PCR) that amplifies specific Toxoplasma DNA or by determining the eye’s own antibody production through Goldmann-Witmer coefficient (GWC) [15, 16]. These methods cannot only confirm the OT diagnosis but can also rule out other similar infectious diseases [17].
It has been described that the analysis of AH by PCR changed the diagnosis and treatment in more than a third of patients, and it should be considered for uveitis of an atypical clinical form, recurrent severe uveitis of unclear etiology, and therapy refractory cases [18]. As the relative importance of different etiologies changes from one geographical site to another, we aim to evaluate the differential diagnosis of this parasitic infection in immunocompetent patients seen in an Ocular Immunology and Uveitis Service, in Bogotá, Colombia. No previous description of this diagnostic approach has been presented in Latin America.
Methods
Purpose
To estimate the number of co-infections and infections by Toxoplasma gondii, Mycobacterium tuberculosis and Herpesvirus in Colombian immunocompetent patients with uveitis of presumed infectious origin.
Population sample
A descriptive transversal study was carried out involving 66 patients of a Uveitis Service of an Ophthalmology Reference Center, Clínica Barraquer, in Bogotá, Colombia, from July 2014 to April 2016.
Inclusion criteria and clinical data collection
The inclusion criteria were patients of all ages, presenting with uveitis of presumed infectious origin. A complete clinical history was taken and an ophthalmological examination was performed for all patients. Data collected included demographic features, age and sex, ophthalmic findings, which comprised affected eye, best corrected visual acuity (BCVA) using the Snellen Charts, intraocular pressure, slit-lamp examination findings, the grade of inflammation in the anterior chamber and in the vitreous according to the Standardization of Uveitis Nomenclature (SUN) guidelines, fundus examination findings with a description of retinochoroidal lesions, size, number and localization if present, and evaluation of ocular complications.
Ethics approval and consent to participate
This study was conducted according to the tenets of the Declaration of Helsinki, strictly following the Guide for Good Laboratory Procedures. The protocol was approved by the Institutional Ethical Committees (Reference numbers: 5–14-1 from Universidad Tecnológica de Pereira and 030314 from Escuela Superior de Oftalmología - Instituto Barraquer de América) and all participants provided written informed consent.
Laboratory analysis
AH and/or vitreous fluid, blood and serum samples were collected from consecutive patients suspected of having uveitis of infectious origin at presentation. The diagnosis of OT was confirmed by serum titers, quantification of antibodies with the GWC and by detection of Toxoplasma gondii genomes with PCR. Differential diagnosis by PCR in AH was done for viral origin and Mycobacterium tuberculosis. AH samples (0.1 to 0.2 ml) were obtained at the Ophthalmologic Center, Clínica Barraquer, in a surgery room, under sterile conditions after topical anesthesia, and were sent to a laboratory for analyses. For real-time PCR (qPCR) assays, DNA extraction was performed using the QIAamp DNA Mini Kit (Qiagen, Hilden, Germany) and procedures were performed as recommended by the manufacturer. DNA from a pellet of AH was obtained by incubating samples for 10 min at 56 °C with the cell lysis solution. After centrifuging at 6000 g for 1 min at 37 °C, flow through was discarded and the spin column was recovered. A two wash step was performed with washing solution and the cellular proteins were then eluted from the spin column. To detect Toxoplasma DNA in AH (0.1 to 0.2 ml), a qPCR TaqMan-based assay was used for this study, as described previously [19]. Briefly, this test amplifies a 100-bp of a 529-bp repetitive fragment (RE) that is reported to be repeated 300 times in the genome of T. gondii (Genebank accession number AF146527). The TaqMan probe TACAGACGCGATGCCGCTCC, and RE primers F- GCCACAGAAGGGACAGAAGT and R- ACCCTCGCCTTCATCTACAG, were redesigned using web-based software (found at https://www.genscript.com/ssl-bin/app/primer). The Taqman probe was labeled at the 5’with 6-carboxyfluorescein (FAM) and at the 3′ with non-fluorescent quencher. qPCR was performed using a Platinum® Quantitative PCR SuperMix-UDG (Invitrogen, Carlsbad, California, United States). The amplification protocol consisted of two initial stages of 50 °C for 2 min, held for UDG incubation, and 95 °C for 2 min, held for UDG inactivation, followed by 40 cycles of 95 °C for 15 s of denaturation, followed by 60 °C for 30 s of annealing and extension. The positive control was DNA from the RH strain and the negative control was distilled water in the presence of primers. Control for contamination during DNA extraction was also included and consisted of a tube without a template but containing all reagents for DNA extraction and filled with the same pipette. An additional control was a blood sample from a patient that tested negative for Immunoglobulin G (IgG) and Immunoglobulin M (IgM) Toxoplasma antibodies.
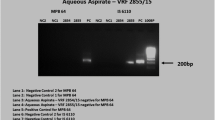
The presence of human herpes virus 3 (VZV) IE62 gene, HVS2 UL36 region, human herpes virus 5 (CMV) glycoprotein B gene, glycoprotein B gene and the EBV (human herpes virus 4) non-glycosylated membrane protein (BNRF1) gen and M. tuberculosis MPB64/IS6110 repeated genomic sequence, were tested with the Genesig Advanced Kit (Primerdesign Ltd., York House, School Lane, Chandler’s Ford, United Kingdom) by following the instructions of the manufacturer. These tests have previously shown good sensitivity and specificity for diagnosis of herpes virus infections in humans [20]. Results of the qPCR were expressed as cycle thresholds or Ct values. All amplifications were performed using an Applied Biosystems Step One plus qPCR system.
All serum samples were analyzed for anti-Toxoplasma IgG and IgM antibody titers by using ELISA commercial assays and following the manufacturer’s (Human, Gesellschaft für Biochemica und Diagnostica mbH Max-Planck-Ring 21, 65,205 Wiesbaden, Germany) recommendation. Those with positive Toxoplasma IgG results underwent local ocular antibody production testing to calculate the GWC. This index was calculated by measuring the levels of intraocular anti-Toxoplasma antibodies, as described previously [16]: anti-Toxoplasma IgG in AH/total IgG in AH/anti-Toxoplasma IgG in serum/total IgG in serum [16].
Patients were also submitted to measurement of IgG and IgM in serum for HSV1, HSV2, VZV, CMV and EBV. Those with positive IgM results were considered to have active viral infection and were given specific treatment.
Diagnostic flowchart, classification of diagnosis and clinical follow-up
We used a diagnostic algorithm that was previously used in French patients to unequivocally confirm OT in up to 80% of cases [16]. This consisted in the analysis of AH samples for diagnosis of Toxoplasma or other infections (Fig. 1). If local IgG production was detected (GWC < 2), or if PCR analysis in AH detected parasitic DNA, then the clinical diagnosis was considered to confirm OT. If no local specific IgG production or PCR was negative or an aqueous humor sample was not available, but the lesions were characteristic of toxoplasmosis and anti-Toxoplasma IgG antibodies were positive in serum, the diagnosis was considered as undetermined ocular toxoplasmosis (UOT). If anti-Toxoplasma IgG antibodies were negative in serum or an AH sample was not available and PCR was positive in AH for other etiologies, the diagnosis was considered as other uveitis (OU). If two or more PCR were positive for different pathogens in the same sample then it was considered a case of co-infection (COINF). The primary outcome measure was the frequency of OT, UOT, OU and COINF. Secondary outcomes were change in treatment based on the laboratory results and if improvement was observed after change of treatment or without change of treatment, during follow-up. Improvement after therapy was defined as recovering one or more lanes in visual acuity (using any measure) at the end of follow-up and reduction in retinochoroidal lesion size after 6 weeks of treatment. Patients were followed up closely to determine treatment response in terms of reduction of anterior chamber cellularity, vitreous cells and haze, reduction in lesion size, if applicable, and improvement in visual acuity.
Statistical analysis
A data collection instrument was created for this study and entered into the database in Excel (Additional file 1) for subsequent statistical analysis using SPSS v14.0 (IBM, Armonk, New York,USA). Results were expressed as the median [min-max] for continuous variables and N (%) for categorical variables. Differences in proportions were analyzed using the chi-square test or Fisher’s exact test, when appropriate. Differences in means were compared by ANOVA or a non-parametric test if not normally distributed. Values below p < 0.05 were considered statistically significant.
Results
Five hundred forty-seven patients presented with the diagnosis of uveitis from July 2014 to April 2016, 174 with active uveitis, from which 67 patients were suspected to have uveitis of infectious origin; and 66 patients, who accepted to provide written informed consent, were included in the study period.
Sixty-six consecutive patients – 32 females (47.8%), and 34 males (51.5%), aged between 13 and 79, with a median age of 37 years – who presented with uveitis that was clinically consistent with OT were first studied by Toxoplasma serological tests. According to the results of serum tests, specific Toxoplasma PCR and GWC analyses were performed in AH samples obtained by diagnostic anterior chamber paracentesis (Fig. 1). There were 22 cases of confirmed OT, eight of confirmed OU and five COINF. In total, 35 patients (53%) had etiological diagnosis confirmed by PCR or GWC (Fig. 1). OT was conclusively diagnosed for 27 patients through examination of aqueous humor samples (five of them with COINF): 9 tested positive on both tests (PCR and GWC) in aqueous humor; in 15 patients diagnosis was made by the high load of specific antibodies in aqueous humor alone and in three by the PCR alone. In confirmed OT, 12 out of 27 patients with PCR analysis were tested positive by PCR (44.4%) and 24 out of 27 with GWC analysis (88.8%) were found to be positive.
No significant differences in demographic and clinical characteristics were found between the group of patients according to their diagnoses, except for frequency of anterior uveitis that was only observed in OU or in unconfirmed toxoplasmosis (Table 1). In 21 patients (31.8%), there was a change of treatment after diagnosis. As expected, the change of treatment after diagnosis was significantly greater for the group of patients with OU and with COINF (Table 1). For the group of patients with OU, when treatment was changed from topical anti-inflammatory therapy to systemic anti-viral therapy, anti-TB therapy or to immunomodulatory therapy, according to the final diagnosis, improvement was observed in 12 out of 13 patients (92,3%). All of the patients with diagnosis of viral uveitis improved after anti-viral treatment. In contrast, improvement was observed in six out of eight patients without change in therapy after diagnosis (75%): however, this difference was not statistically significant (Fisher test p = 0,53). Coinfected patients were closely followed up, treated with the specific therapy for each case. Acyclovir was added in patients with VZV (n = 3) and anti-TB therapy was added in the case of Toxo+TB coinfection (n = 1) with improvement and resolution of the uveitis. In the case of triple coinfection, Toxo+VZV + CMV (n = 1) valacyclovir was prescribed in addition to the anti-Toxoplasma treatment, with improvement but not resolution of the inflammation, due to the unavailability of valganciclovir therapy. This patient persists with low grade of inflammation.
Patients with UOT (n = 11) because of insufficient AH sample (n = 2) or because they did not undergo AH sampling (n = 3), might have been diagnosed with viral uveítis and/or ocular toxoplasmosis if AH could have been tested.
Considering the clinical signs, panuveitis was more common in patients with COINF, than in patients with UOT (80% vs 6.3%). While posterior uveitis was more common in patients with UOT (87% vs 20%), the presence of anterior uveitis was more frequent in patients with OU including viral origin than in patients with UOT or patients with COINF (21.7%, vs 6.3% vs 0% respectively). The specific clinical signs are shown in Table 1.
Of interest, IgM serological tests for the herpesvirus family (HSV1, HSV2, HSV3 and EBV) were positive without relation to the presence of the virus as detected by qPCR in aqueous humor (Table 1). In total, 9 patients were positive for these IgM assays (7 for EBV and 2 HSV1). One patient was positive simultaneously for IgM anti- HSV1 and EBV. Patients with IgM for several viruses might have had recent infection with one of them, inducing cross-IgM detection. Nevertheless, in our study none of them presented positive anti-Toxoplasma IgM. Also, none of these patients had positive serum tests for syphilis, thus we did not include aqueous humor PCR for Treponema pallidum in the patients. The five COINF patients were further investigated by IgM for CMV, and none of them had positive results.
OT was conclusively diagnosed in 27 patients through examination of AH samples (five of them in COINF): 18 tested positive on both tests (PCR and GWC) in AH; six diagnoses were made by the high load of specific antibodies in AH alone and three by the PCR alone. In confirmed OT, 12 out of 25 patients with PCR analysis were tested positive by PCR (48%) and 24 out of 26 with GWC analysis (92.3%) were found to be positive. Concerning the positivity of GWC and PCR according to the days of symptoms at the time of sampling and degree of inflammation, there were no statistically significant differences between positivity of AH PCR or of the GWC (Tables 2 and 3). A Toxoplasma IgG avidity test was performed in 44 patients with positive IgG titers. All the results of avidity were higher than 30%, indicating chronic infection acquired more than 4 months ago, including the four patients with a positive anti-Toxoplasma IgM test.
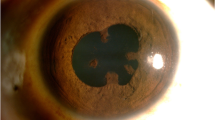
Intraocular pressure was very high in eight patients (12%). One of these patients with COINF was initially diagnosed as typical recurrent OT, with a bad response to conventional treatment; this patient presented OT + VZV COINF. Another patient with triple COINF (TO+VZV + CMV), had bilateral compromise and did not have any history or clinical or laboratory evidence of immunodeficiency.
Discussion
Diagnostic doubts are a factor in the management of uveitis [15, 21,22,23,24]. There are several differential diagnoses that must be considered when dealing with patients with suspected infectious uveitis [15, 21,22,23,24]. Several studies have demonstrated that by combining PCR and GWC the diagnostic certainty for toxoplasmic retinochoroiditis is increased, reaching 80–93% sensitivity and specificity of ~ 93% [23]. In our study, we made an accurate diagnosis of uveitis causes using GWC and PCR in 53% of our patients. The frequency of PCR positivity was similar to that reported in previous studies [16, 25, 26]. To the best of our knowledge, there are no previous studies about the presence of COINF in immunocompetent Colombian patients with OT. In the present work, combined laboratory techniques, in serum and AH, were of significant diagnostic value for patients diagnosed as having other intraocular infections (VZV, EBV, tuberculosis).
GWC is based on the comparison of levels of specific antibodies in ocular fluid and serum samples [26]. It has been reported in a study in French patients that the time interval from symptoms onset to anterior chamber tap is highly correlated with the GWC positivity. In our cases, there were no differences in days of symptoms in patients with positive or negative PCR; a similar result has previously been reported [26]. This could be explained because Toxoplasma infection is caused by different strains in Colombia and Europe. The load of parasites is higher in Colombian patients compared with European patients and this can induce a rapid increase in antibodies [27]. Colombian strains are usually known as more virulent, triggering a higher intraocular inflammatory response [28]. This might influence the delay or intensity of DNA detection or antibody detection in AH. The different strains explain why test results and clinical decisions vary according to the geographical origin of the ocular infection [29]. Our group in Colombia has consistently demonstrated that South American strains producing ocular toxoplasmosis are different and induce a different humoral response with different cytokine mediators [30]. This can help to understand why diagnostic performances of serological and molecular tests differ [31]. It also has been proven that the performance of RE target for PCR amplification is different when used in South American patients [29, 32, 33].
Patients with UOT (n = 16) were treated with anti-Toxoplasma therapy. All of them had a good clinical response. This is consistent with the traditional practice around the world (treating patients with suspected clinical picture of OT with positive serological anti-Toxoplasma tests). If the outcome was favorable under anti-Toxoplasma therapy, then patients could be definitely considered as OT even with aqueous humor negative. PCR is used only in patients with atypical clinical presentations or in patients with bad response to anti-Toxoplasma treatment [34, 35]. However, in our study we carried out these diagnostic techniques in patients with typical and atypical presentation. We have to take into account that a negative PCR result for Toxoplasma gondii does not rule out the diagnosis and that, in these cases, the clinical response to therapy is crucial to confirm the diagnoses [35]. Although there were no typical granulomas in the posterior pole suggesting ocular infection by Toxocara canis in our patients, toxocariasis was ruled out serologically when patients presented posterior uveitis or panuveitis and none of the patients screened had positive antibodies. Although Lyme disease is also an infectious cause of uveitis, it was not screened for, because there are not cases of Lyme disease reported as a cause of uveitis in Colombia and patients did not have any traveling history to the northern hemisphere. Thus, differential diagnosis by PCR in AH was not done for toxocariasis or Lyme disease [36] . As it cannot be excluded that OT was not diagnosed due to lack of sensitivity of the PCR or GWC, we merge the 3 patients with positive serological assay for Toxoplasma with the 20 patients with “other uveitis”. Considering that Mycobacterium tuberculosis and Leptospira [37] can also cause uveitis, we prefer to keep the term as “Other Uveitis (OU)” instead to consider cases of other uveitis only as of viral origin. This population was clinically homogenous regarding the characteristics of uveitis, leading as to think in infectious origin. It is necessary to improve the sensitivity of diagnostic techniques in AH in order to get definitive and conclusive diagnosis in these patients.
Multiple infectious diseases can be associated in immune-deficient patients with human immunodeficiency virus infection and acquired immune deficiency syndrome (HIV/AIDS), presented as simultaneous or separate infections leading to severe intraocular compromise [38, 39]. In our study, all patients were immunocompetent, including those with co-infection. It has been reported that EBV-DNA was found in HIV negative immunocompromised patients with uveitis. However, authors hypothesized that EBV is not a direct cause of uveitis, but it may play a role as a secondary factor in the pathogenesis of uveitis, producing a homologue of IL-10. This interleukin is known as an immunosuppressant that influences the course of intra-ocular inflammation caused by other pathogens as Toxoplasma, HSV, VZV and CMV [40].
CMV has been associated with anterior, chronic, hypertensive, unilateral and recurrent uveitis in immunocompetent patients [41]. In our work, we did not find CMV infection as a single cause of uveitis in this group of patients. We found CMV infection in coexistence with OT + VZV in one immunocompetent patient. To the best of our knowledge, there are no previous reports about triple intraocular co-infection in the literature in immunocompetent patients. Intraocular COINF of OT associated with viral infection was biologically proven in our patients. COINF presented in immune-competent patients deserves careful consideration. For instance, in a recent study, three immunocompetent patients were AH PCR double positive, for VZV + EBV, Toxoplasma + EBV, and Toxoplasma + HSV [18]. In these double positive cases, therapy was decided according to the clinical criteria, with close follow-up. Double positive PCR has previously been reported in immunosuppressed patients: it is probably due to secondary reactivation of latent parasitic or viral infections triggered by acute infectious uveitis. In the positive cases for EBV, we have to consider that the EBV genome could be present in a latent phase in B lymphocytes, leading to cross reactivity, which can produce false PCR positive results [42]. In immunosuppressed patients, PCR testing for multiple pathogens in ocular fluids can be useful for selecting treatment, since clinical characteristics could be atypical in these cases [43].
PCR in AH samples, GWC and a differential diagnosis assisted with therapeutic trials have been studied by other authors in anterior uveitis [44]. CMV was identified by PCR in aqueous and vitreous samples as the most frequently recognized infectious organism in posterior and panuveitis of HIV-1-negative Thai patients [45]. In our study, none of our COINF patients presented any associated systemic diseases or alterations in ancillary tests. Thus, we excluded primary or secondary immunodeficiencies.
It has been reported that intraocular immune response in OT differs depending on the infecting Toxoplasma gondii strain [46]. Virulent parasites, such as South American strains, may cause more severe OT due to an inhibition of the protective effect of interferon gamma (IFN-γ) [46]. IFN-γ is crucial in the immune response to viral diseases, providing antiviral protection from CMV infection [47]. There is also an important antiviral role for virus-specific CD4(+) T cells in protecting from pathogenic CMV infection [47]. In Colombian patients with OT, the immune response after antigenic stimulation has been found to have a preferential Th2-skewed response, regardless of the nature of antigen stimulus [48] and more severe clinical characteristics in patients infected by type I/III strains [30]; strain-dependent Th2 skewed response should be investigated to identify if it plays a role in favoring this type of co-infections. The Th2-skewed response in patients infected by virulent Toxoplasma gondii strains might have a detrimental role in the defense against viruses, aiding parasites and viral co-infection. T-helper response induction may be confounded by co-infection of a single host by multiple intracellular pathogens. Due to normally adaptive feedback loops that tend to polarize T-helper responses, it can become very difficult for the immune system to mount effective, conflicting responses [48].
Conclusions
Ocular fluids PCR is useful in the diagnosis of uveitis with unusual clinical appearance, severe recurrent intraocular inflammation of unclear origin, and therapy-resistant patients. Additional studies are necessary to analyze how the co-infection affect the therapeutic response and prognosis in this group of patients, and to investigate the need to include additional tests. In future studies, additional molecular analysis for multiple pathogens in aqueous humor would be needed in order to determine if some etiologies were dismissed.
Possible bias
The use of GWC instead of WB might reduce the sensitivity of the diagnosis of infection uveitis. GWC was used because we do not have Western-blotting currently commercially available in Colombia, it should be of interest to test this technique in the future to examine if this can increase the diagnostic performance in these cases.
Five patients lack data from AH tests; 2 because there was insufficient AH volume sample and 3 with only one functional eye who did not undergo AH sampling.
Abbreviations
- AH:
-
Aqueous humor
- BCVA:
-
Best corrected visual acuity
- CMV:
-
Cytomegalovirus
- COINF:
-
Case of co-infection
- EBV:
-
Epstein-Barr virus
- GWC:
-
Goldmann–Witmer coefficient
- HIV/AIDS:
-
Human immunodeficiency virus infection and acquired immune deficiency syndrome
- HSV1:
-
Herpes simplex virus type 1
- HSV2:
-
Herpes simplex virus type 2
- IFN-γ:
-
Interferon gamma
- IgG:
-
Immunoglobulin G
- IgM:
-
Immunoglobulin M
- OT:
-
Ocular toxoplasmosis
- OU:
-
Other uveitis
- PCR:
-
Polymerase chain reaction
- qPCR:
-
Real-time polymerase chain reaction
- SUN:
-
Standardization of uveitis nomenclature
- TB:
-
Tuberculosis
- UOT:
-
Undetermined ocular toxoplasmosis
- VZV:
-
Varicella zoster virus
References
Saadatnia G, Golkar M. A review on human toxoplasmosis. Scand J Infect Dis. 2012;44:805–14.
Arantes TEF, Silveira C, Holland GN, Muccioli C, Yu F, Jones JL, et al. Ocular involvement following postnatally acquired Toxoplasma gondii infection in southern Brazil: a 28-year experience. Am J Ophthalmol. 2015;159:1002–12.
Petersen E, Kijlstra A, Stanford M. Epidemiology of ocular toxoplasmosis. Ocul Immunol Inflamm. 2012;20:68–75.
Gilbert RE, Freeman K, Lago EG, Bahia-Oliveira LMG, Tan HK, Wallon M, et al. Ocular sequelae of congenital toxoplasmosis in Brazil compared with Europe. PLoS Negl Trop Dis. 2008;2:277.
Vasconcelos-Santos DV, Machado Azevedo DO, Campos WR, Oréfice F, Queiroz-Andrade GM, Carellos EVM, et al. Congenital toxoplasmosis in southeastern Brazil: results of early ophthalmologic examination of a large cohort of neonates. Ophthalmology. 2009;116:2199–205.
de-la-Torre A, González G, Díaz-Ramirez J, Gómez-Marín JE. Screening by ophthalmoscopy for Toxoplasma retinochoroiditis in Colombia. Am J Ophthalmol. 2007;143:354–6.
Papadia M, Aldigeri R, Herbort CP. The role of serology in active ocular toxoplasmosis. Int Ophthalmol. 2011;31:461–5.
Vasconcelos-Santos DV, Dodds EM, Oréfice F. Review for disease of the year: differential diagnosis of ocular toxoplasmosis. Ocul Immunol Inflamm. 2011;19:171–9.
Ahn SJ, Ryoo N-K, Woo SJ. Ocular toxocariasis: clinical features, diagnosis, treatment, and prevention. Asia Pac Allergy. 2014;4:134–41.
Barisani-Asenbauer T. Sitting at the window to the world--ocular parasites. Wien Med Wochenschr. 2014;164:392–9.
Burkholder BM, Leung TG, Ostheimer TA, Butler NJ, Thorne JE, Dunn JP. Spectral domain optical coherence tomography findings in acute syphilitic posterior placoid chorioretinitis. J Ophthalmic Inflamm Infect. 2014;4:2.
Gorovoy IR, Desai S. Syphilitic posterior placoid chorioretinitis. Sex Transm Dis. 2013;40:852–3.
Miserocchi E, Fogliato G, Bianchi I, Bandello F, Modorati G. Clinical features of ocular herpetic infection in an italian referral center. Cornea. 2014;33:565–70.
Moradi A, Salek S, Daniel E, Gangaputra S, Ostheimer TA, Burkholder BM, et al. Clinical features and incidence rates of ocular complications in patients with ocular syphilis. Am J Ophthalmol. 2015;159:334–43.
Ozgonul C, Besirli CG. Recent developments in the diagnosis and treatment of ocular toxoplasmosis. Ophthalmic Res. 2017;57:1–12.
Villard O, Filisetti D, Roch-Deries F, Garweg J, Flament J, Candolfi E. Comparison of enzyme-linked immunosorbent assay, immunoblotting, and PCR for diagnosis of toxoplasmic chorioretinitis. J Clin Microbiol. 2003;41:3537–41.
Fardeau C, Romand S, Rao NA, Cassoux N, Bettembourg O, Thulliez P, et al. Diagnosis of toxoplasmic retinochoroiditis with atypical clinical features. Am J Ophthalmol. 2002;134:196–203.
Chronopoulos A, Roquelaure D, Souteyrand G, Seebach JD, Schutz JS, Thumann G. Aqueous humor polymerase chain reaction in uveitis - utility and safety. BMC Ophthalmol. 2016;16:189.
Cardona N, Basto N, Parra B, Zea AF, Pardo CA, Bonelo A, et al. Detection of Toxoplasma DNA in the peripheral blood of HIV-positive patients with neuro-opportunistic infections by a real-time PCR assay. J Neuro-Oncol. 2011;2:1–6.
Aliabadi N, Jamalidoust M, Asaei S, Namayandeh M, Ziyaeyan M. Diagnosing of herpes simplex virus infections in suspected patients using real-time PCR. Jundishapur J Microbiol. 2015;8:16727.
Errera M-H, Goldschmidt P, Batellier L, Degorge S, Héron E, Laroche L, et al. Real-time polymerase chain reaction and intraocular antibody production for the diagnosis of viral versus toxoplasmic infectious posterior uveitis. Graefes Arch Clin Exp Ophthalmol. 2011;249:1837–46.
Harper TW, Miller D, Schiffman JC, Davis JL. Polymerase chain reaction analysis of aqueous and vitreous specimens in the diagnosis of posterior segment infectious uveitis. Am J Ophthalmol. 2009;147:140–7.
Taravati P, Lam D, Van Gelder RN. Role of molecular diagnostics in ocular microbiology. Curr Ophthalmol Rep. 2013;1:181–9.
Torres-Morales E, Gómez-Marín JE. Evaluación de una prueba ELISA IgG De Avidez para toxoplasma para el diagnóstico en el embarazo y correlación con IgM e IgA en el laboratorio del Centro de Investigaciones Biomédicas de la Universidad del Quindío, 2008. Rev Col Obstet Ginecol. 2008;59:199–205.
Sugita S, Ogawa M, Inoue S, Shimizu N, Mochizuki M. Diagnosis of ocular toxoplasmosis by two polymerase chain reaction (PCR) examinations: qualitative multiplex and quantitative real-time. Jpn J Ophthalmol. 2011;55:495–501.
Talabani H, Asseraf M, Yera H, Delair E, Ancelle T, Thulliez P, et al. Contributions of immunoblotting, real-time PCR, and the Goldmann-Witmer coefficient to diagnosis of atypical toxoplasmic retinochoroiditis. J Clin Microbiol. 2009;47:2131–5.
de-la-Torre A, Sauer A, Pfaff AW, Bourcier T, Brunet J, Speeg-Schatz C, et al. Severe South American Ocular Toxoplasmosis Is Associated with Decreased Ifn-γ/Il-17a and Increased Il-6/Il-13 Intraocular levels. PLoS Negl Trop Dis. 2013;7:e2541.
Sánchez V, De-la-Torre A, Gómez-Marín JE. Characterization of ROP18 alleles in human toxoplasmosis. Parasitol Int. 2014;63:463–9. https://doi.org/10.1016/j.parint.2013.10.012.
Gómez Marín JE, Zuluaga JD, Pechené Campo EJ, Triviño J, De-la-Torre A. Polymerase chain reaction (PCR) in ocular and ganglionar toxoplasmosis and the effect of therapeutics for prevention of ocular involvement in South American setting. Acta Trop. 2018;184:83–7. https://doi.org/10.1016/j.actatropica.2018.01.013.
de-la-Torre A, Pfaff AW, Grigg ME, Villard O, Candolfi E, Gomez-Marin JE. Ocular cytokinome is linked to clinical characteristics in ocular toxoplasmosis. Cytokine. 2014;68:23–31. https://doi.org/10.1016/j.cyto.2014.03.005.
Garweg JG, Sobottka Ventura AC, Halberstadt M, Silveira C, Muccioli C, Belfort Jr. R, et al. Specific antibody levels in the aqueous humor and serum of two distinct populations of patients with ocular toxoplasmosis. Int J Med Microbiol. 2005;295.
Torres E, Rivera R, Cardona N, Sanchez V, Lora F, Gómez-Marín JE. Evaluation of IgG anti-toxoplasma avidity and polymerase chain reaction in the postnatal diagnosis of congenital toxoplasmosis. Pediatr Infect Dis J. 2013;32:693–5. https://doi.org/10.1097/INF.0b013e31828807a4.
Kompalic-Cristo A, Frotta C, Suárez-Mutis M, Fernandes O, Britto C. Evaluation of a real-time PCR assay based on the repetitive B1 gene for the detection of Toxoplasma gondii in human peripheral blood. Parasitol Res. 2007;101:619–25.
Montoya JG, Parmley S, Liesenfeld O, Jaffe GJ, Remington JS. Use of the polymerase chain reaction for diagnosis of ocular toxoplasmosis. Ophthalmology. 1999;106:1554–63. https://doi.org/10.1016/S0161-6420(99)90453-0.
Garweg JG, de Groot-Mijnes JDF, Montoya JG. Diagnostic approach to ocular toxoplasmosis. Ocul Immunol Inflamm. 2011;19:255–61.
de-la-Torre A, López-Castillo CA, Rueda JC, Mantilla RD, Gómez-Marín JE, Anaya J-M. Clinical patterns of uveitis in two ophthalmology centres in Bogota, Colombia. Clin Experiment Ophthalmol. 2009;37:458–66. https://doi.org/10.1111/j.1442-9071.2009.02082.x.
Verma A, Rathinam SR, Priya CG, Muthukkaruppan VR, Stevenson B, Timoney JF. LruA and LruB antibodies in sera of humans with leptospiral uveitis. Clin Vaccine Immunol. 2008;15:1019–23.
Tan DHS, Asztalos E, Douglas D, Read S, Bitnun A. Congenital transmission of human immunodeficiency virus, cytomegalovirus, and toxoplasmosis in a premature infant. Pediatr Infect Dis J. 2009;28:1129–31.
Zhang R, Qian J, Guo J, Yuan Y, Xue K, Yue H, et al. Clinical Manifestations and Treatment Outcomes of Syphilitic Uveitis in a Chinese Population. J Ophthalmol. 2016;2016.
Ongkosuwito J V, Van der Lelij A, Bruinenberg M, Wienesen-van Doorn M, Feron EJ, Hoyng CB, et al. Increased presence of Epstein-Barr virus DNA in ocular fluid samples from HIV negative immunocompromised patients with uveitis. Br J Ophthalmol. 1998;82:245–51.
van Boxtel LAA, van der Lelij A, van der Meer J, Los LI. Cytomegalovirus as a cause of anterior uveitis in immunocompetent patients. Ophthalmology. 2007;114:1358–62.
Lang D, Vornhagen R, Rothe M, Hinderer W, Sonneborn HH, Plachter B. Cross-reactivity of Epstein-Barr virus-specific immunoglobulin M antibodies with cytomegalovirus antigens containing glycine homopolymers. Clin Diagn Lab Immunol. 2001;8:747–56.
Yang S, Rothman RE. PCR-based diagnostics for infectious diseases: Uses, limitations, and future applications in acute-care settings. Lancet Infectious Diseases. 2004;4:337–48.
Chee S-P, Bacsal K, Jap A, Se-Thoe S-Y, Cheng CL, Tan BH. Clinical features of cytomegalovirus anterior uveitis in immunocompetent patients. Am J Ophthalmol. 2008;145:834–840. e1.
Kongyai N, Pathanapitoon K, Sirirungsi W, Kunavisarut P, de Groot-Mijnes JDF, Rothova A. Infectious causes of posterior uveitis and panuveitis in Thailand. Jpn J Ophthalmol. 2012;56:390–5.
Pfaff AW, De-la-Torre A, Rochet E, Brunet J, Sabou M, Sauer A, et al. New clinical and experimental insights into Old World and neotropical ocular toxoplasmosis. Int J Parasitol. 2014;44:99–107. https://doi.org/10.1016/j.ijpara.2013.09.007.
Jeitziner SM, Walton SM, Torti N, Oxenius A. Adoptive transfer of cytomegalovirus‐specific effector CD4 T cells provides antiviral protection from murine CMV infection. Eur J Immunol. 2013;43:2886–95.
Torres-Morales E, Taborda L, Cardona N, De-la-Torre A, Sepulveda-Arias JC, Patarroyo MA, et al. Th1 and Th2 immune response to P30 and ROP18 peptides in human toxoplasmosis. Med Microbiol Immunol. 2014;203:315–22.
Acknowledgements
We would like to Andrea C.de la Torre and Robin Trenbath (University of Oxford) for helping us with editing the manuscript. This study was supported by COLCIENCIAS Universidad Tecnológica de Pereira, Universidad del Quindío, Escuela Superior de Oftalmología, Instituto Barraquer de América and Clínica Barraquer.
Funding
This study was financed by COLCIENCIAS (the Colombian Innovation, Technology and Science Department, Project 111056934589, Contract 469–2013) who provided the necessary resources for the collection of serum samples and PCR studies. Universidad Tecnológica de Pereira (Project 5–14-1) and Universidad del Quindío who provided the necessary human resources for the application of diagnostic tests and the analysis of results. And Escuela Superior de Oftalmología - Instituto Barraquer de América and Clínica Barraquer who provided the database of patients and professional staff suitable for the assessment of individuals and statistical analysis of data.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
ADLT, JGM were involved in the design, analysis, interpretation and write-up of this study. CLDM, ACP and JCS were involved in the analysis and interpretation. JVC, FD and LMRP were involved in data collection and write-up. AUN and JDZ: data collection, analysis and interpretation. ETM, JT, MM: laboratory analysis. All authors have read and approved the final version of this manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted according to the tenets of the Declaration of Helsinki, strictly following the Guide for Good Laboratory Procedures. The protocol was approved by the institutional ethical committee (Universidad Tecnológica de Pereira, Act 06 of May 14, 2012) and the institutional ethical committee (Escuela Superior de Oftalmología, Instituto Barraquer de América Act 03 of March, 2014). All participants provided written informed consent. It was clearly explained to each participant the objectives of the study, informed of their rights to deny participation and assured for the confidentiality. Laboratory results were returned to patients.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Availability of Dataset. (XLSX 50 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
de-la-Torre, A., Valdés-Camacho, J., de Mesa, C.L. et al. Coinfections and differential diagnosis in immunocompetent patients with uveitis of infectious origin. BMC Infect Dis 19, 91 (2019). https://doi.org/10.1186/s12879-018-3613-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-018-3613-8