Abstract
Background
Over 80% of morbidity due to soil-transmitted helminthiasis (STH) occurs in low-income countries. Children under 5 account for 20–30% of the burden in endemic areas. This study assessed the prevalence, intensity and factors associated with STH infections among preschool-age children (PSAC) in Hoima district, Uganda. The PSAC are particularly vulnerable because the chronicity of this condition usually affects their physical and mental growth and development.
Methods
A cross-sectional study was carried out among 562 PSAC (1–5 years old) in 6 counties of Hoima district using Expanded Program on Immunization (EPI) method. Stool samples from children were examined using the formol ether concentration technique for STH egg detection. Egg counts were represented as egg per gram (EPG). A structured questionnaire was used to collect information on factors associated with STH infection. Generalized linear models were used to analyze relationships between STH infection and associated factors.
Results
Overall STH prevalence was 26.5%. Hookworm infection was the most prevalent (18.5%), followed by A.lumbricoides (9.8%) and T.trichiura (0.5%). Prevalence of STH infection was significantly higher in children aged 5 years (Pearson chi-square test, p = 0.009) than in children aged 1 year. The general geometric mean (GM) counts for Hookworm infection was (696.1 EPG; range (530.3–913.8)) with girls having a higher GM (789.8 EPG; range (120–13,200)) than boys. Eating uncooked or unwashed vegetables (adj. Prevalence Ratio (PR) = 1.9, 95% CI: 1.3–2.7) and fruits (adj.PR = 1.8, 95% CI: 1.1–2.8), indiscriminate disposal of young children’s faeces (adj.PR = 1.5, 95% CI: 1.1–2.0); not washing hands after defecation (adj.PR = 2.6, 95% CI: 1.9–3.6); and not deworming children regularly (adj.PR = 1.4, 95% CI: 1.1–1.8) were significantly associated with STH infection.
Conclusion
The prevalence of Soil transmitted helminths infection among preschool-age children in Hoima district significantly increased with age. Poor hygiene, inadequate sanitation and irregular deworming were associated with STH infections among PSAC in the study area. Intense health education on the importance of hygienic practices, improved sanitation and regular deworming of PSAC should be integrated into prevention and control programs.
Similar content being viewed by others
Background
Soil transmitted helminthes (STH), such as Ascaris lumbricoides (Round worm), Trichuris trichiura (Whipworm) and Ancylostoma spp (hookworms) are nematodes that infect more than a billion people worldwide, with low-income countries accounting for over 80% of the disease burden [1,2,3]. In areas with inadequate water, sanitation and hygiene conditions, children are particularly at higher risk for infections due to STH [4,5,6,7]. The affected children are usually malnourished and anemic because of the resultant nutritional deficiency [8, 9]. Long term effects associated with the condition include diminished physical fitness, growth retardation and delayed intellectual development and cognition [10, 11].
Some studies have associated STH infections with poverty, poor nutrition, nutritional insecurity, poor sanitation, lack of clean drinking water and low deworming uptake [9, 12,13,14,15,16,17,18]. Many of these studies however, focused on the school children on the basis of easy reach [15]. These studies also did not examine the influence of education, access to health services and household socio-economic status on the burden of STH in children [15].
Uganda started implementing the national child day plus in 2004 [8, 19]. The strategy targets children aged 1–14 years old and it was adopted to treat Schistosomiasis and STH with praziquantel and Albendazole. The aim is to reduce prevalence and intensity of STH and the risk of long term effect of STH infections in children. However, this approach misses out many preschool-age children whose caretakers fail to attend child day plus due to poor health seeking behaviours [1, 9, 20, 21]. Even where data has been available, it shows low deworming coverage in the country [22].
In Hoima district, deworming treatment coverage for STH was estimated at 60% in 2015, which was well below the national target of 80% and the prevalence of STH in the district was estimated at 22% [23, 24]. Preschool-age children accounted for 9% of the overall 22% STH prevalence in the district, despite the existence of the child day plus which has been ongoing since 2004 [24]. The most affected sub-counties in the district include: Kyangwali, Kabwoga, Buseruka, and Kigorobya and areas around the shores of Lake Albert where sanitation and hygiene conditions are poor [6, 24]. There is inadequate information on the prevalence, intensity and factors associated with STH infection among preschool-age children (PSAC) in Hoima district. This study therefore aimed at determining the prevalence, intensity and the factors associated with STH infections among PSAC in Hoima district so as to provide basis for appropriate strategies against STH infections.
Methods
Study setting and design
This was a cross-sectional study in which a structured questionnaire was used to collect data from caretakers of the preschool-age children aged 1–5 years old in 51 villages in Hoima district from March to April 2016. Hoima district is located in the western region, about 220 km from the capital city Kampala, Uganda. The district is made up of 13 sub-counties, 54 Parishes and a total of 643 villages with an estimated total population of 572,986 people. Over 90% of the population lives in rural areas and over 70% are peasant farmers who depend on subsistent agriculture for their livelihood needs. In Hoima, STH is more prevalent in lowland areas and areas along the shores of Lake Albert. Our study was conducted in March 2016 prior to the planned national deworming exercise.
Study population
The study participants comprised of 562 preschool-age children 1–5 years old selected from villages of 12 Parishes in Hoima district.
Sample size determination and sampling procedure
The sample size for this survey was estimated using Bennett’s cluster survey sampling formula estimating prevalence of 22% and assuming a precision of 0.03 type 1 error of 5%, design effect of 1.9, intra-cluster variability of 0.1 and number of respondents per cluster as 10 [25, 26], a sample size of 510 was obtained. Assuming 10% non-response rate, we sampled 561 participants to cater for non response. We actually collected data from 562 participants, after additionally identifying two preschool-age children from adjacent homes with diarrheal conditions.
The 2015 annual district Water Sanitation and Hygiene (WASH) report revealed that 11 Parishes in 4 lowland sub-counties of Kyangwali, Buseruka, Kabwoya and Buhimba and 9 Parishes in 2 upland sub-counties of Bugambe and Kiziranfumbi had poor sanitation and hygiene conditions. Therefore, on the basis of this background information, we selected a total of 12 Parishes (6 Parishes each from lowland and upland areas) using simple random selection method (balloting) without replacement. A total of 51 villages were selected from the 12 selected Parishes with probably proportionate to size of village in each Parish. We recruited 562 participants, one per household in the selected villages. To achieve this, the total number of households in each village was obtained from the Local Chairperson (LC-1) and a sampling interval K was calculated by dividing the total number of households per village by the number of household targeted for inclusion in the study in order to get the required number of target respondents per village. The research team located the center of the chosen village with the help of the LC-1 or representative and randomly selected a direction by using a compass to determine the starting direction. The team then moved in the northern direction as indicated on the compass to locate the starting household from which an eligible child aged 1–5 years old was selected to participate in the survey. In a household with more than one child aged 1–5 years old, one was recruited in the survey using simple random selection method without replacement. A household that did not have a child who met the inclusion criteria was substituted with the next household. The data collectors then moved every Kth household in clockwise concentric circles looking for eligible child till the required sample for that village was obtained. Respondents were caretakers of children aged between 1 and 5 years of age and have lived in Hoima for at least one year. Preschool-age children who were sick, who failed to defecate, who received deworming in the last 2–3 months or whose caretakers were absent at the time of the survey were excluded. Respondents of the PSAC were asked to tell the ages of their children in completed years and where possible, trained research assistants verified ages with immunization cards and/or birth certificates.
Data collection and laboratory procedure
Caretakers of the participating children were oriented on specimen collection procedures prior to specimen collection. Plastic Stool containers with applicator sticks were then marked with identification numbers and distributed to the caretakers of each selected child to submit about 5 g (a size of a thumb) of fresh stool samples, which were collected in the morning and examined in the afternoon of the same day. The stool samples and data collected using structured questionnaire for each child was assigned similar codes. The team made follow-up visit to collect samples from eligible children who failed to defecate on the date of the survey.
On the same day of stool collection, a structured questionnaire was administered to children’s caretakers so as to obtain information on Socio-demographic, economic, behavioural and community factors, as well as knowledge and practices about STH infections. The questionnaire was adopted from standard tools provided by the joint monitoring programme (JMP) of World Health Organization (WHO) and United Nations International Children Education Funds (UNICEF) [27]. The questionnaire was pre-tested and suitably modified through a pilot study in Kigorobya village that was not included in the sample.
Stool samples were stored in properly sealed boxes and transported to Hoima Regional Referral Hospital for analysis in the afternoon of the same day. The Formol- ether-sedimentation technique was used to separate the parasite from fecal debris, and unmask for visibility [28, 29]. The fecal samples were examined for appearance, colour, blood, and mucus.
In summary, an aliquot (matchstick head amount) of stool for each child was picked using applicator stick and mixed with formol water contained in screwed tube and mixed by shaking for at least 30 s. The floating liquid on top of the sediment was filtered through a sieve into a second centrifuge tube. After adding 3–4 ml (ml) of ethyl acetate, the sentiment in the second tube was centrifuged at minimum speed (2500 revolution per minute (rpm)) for 5 min [30]. The final sediment was then used for slide preparation. Thick smears were examined microscopically in the same way as that of the direct saline method [30]. The number of helminths eggs were counted and recorded for each species separately. To increase chances of diagnosing STH infection, 2 slides of the same stool sample were prepared and examined by two experienced laboratory technicians and for any discrepancies in diagnosis, the technicians re-examined stools inter-changeably to determine correct STH infection.
Data was collected on, socio-demographic, economic, behavioural and community factors, as well as knowledge and practices about STH infections. The primary outcome variable was STH infection, defined as any child aged 1–5 years in whose stool sample at least one type of soil helminthes parasite has been identified according to laboratory results. STH infection was measured as either ‘yes’ (infection present) or ‘no’ (no infection). Where the parasite was present, secondary outcome variable (the intensity of infection) was also measured as the number of soil helminthes eggs per gram of faeces [31]. Different thresholds of parasites according to this criterion included: A. lumbricoides (Round worms) (1–4999 egg per gram (EPG) = light intensity), (5000–49999EPG = moderate intensity) and (> = 50,000 = heavy intensity); Ancylostoma spp (Hookworms) (1–1999 EPG = light intensity, 2000–3999 EPG = moderate intensity, > = 4000 EPG = heavy intensity); T. trichiura (Whipworm) (1–999 EPG = light intensity, 1000–9999 EPG = moderate intensity, > = 10,000 heavy intensity).The number of eggs per gram of faeces was calculated by adding the egg counts in all fields together then multiply the total by 24 to give the EPG of faeces. (Example: 15 eggs are seen in total, then 15 * 24 = 600 EPG (WHO, 1987, 1993).
Data on socio-demographic characteristics was collected based on age, gender, residence, education, occupation, religion, and birth order. To classify socio-economic status (SES), wealth index was computed using, principal component analysis (PCA) based on ownership of 14 household assets including: 1) television; 2) radio; 3) mobile phone; 4) bicycle; 5) motorcycle; 6) moto vehicle; 7) piece of land; 8) large farm animals like cattle, goats and sheep; 9) small farm animals like poultry; 10) Machine made wooden/metallic bed; and 11) house wall made of brick; 12) house wall made of mud; 13) house floor made of cement and 14) house floor made of bare-earth floor as earlier described [32, 33]. Each household item was then assigned a weight or factor score generated through principal components analysis. The resulting asset scores were then standardized and the component on which factor loading appeared the most was used to generate total score for each respondent. The respondents’ scores was then grouped into quintile of wealth index (Lowest, second, middle, Fourth and Highest) using the PCA [34]. 20% of the population with lowest total asset scores became individuals in the lowest wealth quintile, the next 20% were members of the second quintile, up to the highest quintile [34]. The same approach was used by other studies and Demographic Surveillance Surveys in Africa [32, 33].
Knowledge about STH infection was measured in four domains including: mode of transmission/causes; prevention; choice of treatment option as well as; schedules for the annual mass deworming program. Participants were scored with a 1 for each knowledge items they knew, and with a 0 for those they did not know. The total score for the 17 questions used in the assessment of knowledge were used to grade participants into four knowledge levels: very low (0–4), low (5–9), moderate (10–14) and good (15–17). Participants in the ‘moderate’ and ‘good’ categories were regarded as having adequate knowledge about STH infections [35]. Behavioural factors: sandal/shoe wearing (not at all, sometimes, always), child eating habits (communal, self services, fed by someone else), frequency with which a child eats away from home (Not at all, Sometimes, often times), meal preparation (person aged < 15 years, Person aged 15–19 years, person aged 20+ years), child eating vegetables without washing /cooking (not at all, Sometimes, often times/always) and child eating fruits without washing them (not at all, Sometimes, often times/always) and community factors: household latrine facilities (open defecation, pit latrine, water closet). Sources of drinking water (safe, unsafe), disposal of young child’s feces (sanitary, unsanitary), disposal of domestic waste (sanitary, unsanitary), child received de-worming treatment in April 2015 (Yes, No), and child received de-worming treatment in October 2015 (Yes, No) were measured using nominal and dichotomous scales. In this study, sanitary disposal of human and animal faeces was defined as putting the faeces in the latrine or burring it into the soil [36].
Statistical analysis
Data was double entered into Epi-info version 3.5.1, cleaned and exported to STATA12 (StataCorp.; College Station, TX, United States of America) for analysis. Data exploration and reduction was undertaken and independent variables were selected and analyzed to determine their associations with the outcome variables. For continuous variables, summary statistics was obtained including means (±Standard Deviation (SD)). For categorical variables, proportions and frequencies were computed. Prevalence of STH infections and STH infection intensity disaggregated by sex, age group and residence were cross-tabulated and p-values computed using Persons chi-square test as well as t test for mean age of the PSAC. Homogeneity of variance among groups such as sex, residence and age group were also tested using Bartlett’s test.
Prevalence ratios (PRs) were used as measure of association between the outcome variables and the independent factors. They were computed using a generalized linear model (GLM) analysis with Poisson family and a log link with robust standard errors. All independent factors with p-value < 0.15 [37] and biologically plausible variables were included in the multivariable model. Logical model building technique was used to ascertain the best fitting model with a log likelihood tending towards zero. For all tests, a p-value ≤0.05 at 95% confidence intervals (95% CIs) were considered statistically significant. Unadjusted (PRs), adjusted prevalence ratios (adj.PR), and their respective 95% CI were reported.
Results
Demographic characteristics of preschool-age children
A total of 562 preschool-age children participated in the study and all their caretakers were interviewed, giving a 100% response rate. The response rate was 99.1% (557/562). The reasons for not obtaining 100% response rate included: 1) absence of caretakers at the time of stool sample collection, 2) some children failed to defecate in the morning, and 3) some caretakers misplaced stool containers. The mean age of the participating children was 3.2 years (SD = ±1.3). Majority 78.5% (441/562) of the children were aged 3–4 years. There were more girls 53.9% (303/562), p = 0.0157 than boys. Slightly more than half 51.1% (287/562) of the children lived in upland areas. There were no significant sex and age differences between residence [Bartlett’s test for equal variances: chi-square = 0.003, d.f (1, 560), p = 0.960 and chi-square = 0.0043, d.f (2, 559), p = 0.798) respectively. The rest of the results are shown in Table 1 below.
Socio-demographic and economic characteristics of the caretakers
Among the caretakers who provided information on behalf of their children; more than half 54.3% (305/562) were aged 30–39 years. Majority 62.5% (351/562) of the caretakers were married and 63.7% (221/562) were Christians. About 45.0% (246/562) of the caretakers attained primary education, whereas 7.3% (41/562) had tertiary education. The difference in education of caretakers across residence was not statistically significant (Bartlett’s test for equal variances: chi-square = 0.0930, d.f (3, 558), p = 0.993). Almost three-quarters 74.0% (416/562) of the participants were peasants (Table 2).
Prevalence of soil transmitted helminths infections among preschool-age children
Out of 562 children whose stool samples were examined, 26.5% (149/562) were positive of STH infection, while 73.5% (413/562) did not show any evidence of infection. Parasite specific infection prevalences were 18.5% (104/562) for Hookworm, 9.8% (55/562) for A. lumbricoides and 0.5% (03/562) for T. trichiura. Hookworm and A. lumbricoides infections were reported in all the age groups. The prevalence of STH infections was significantly higher in boys than in girl. This difference was statistically significant (Pearson chi-square test, p = 0.002). Children living in lowland residential areas presented with higher prevalence of Hookworm and A. lumbricoides infections compared to children living in upland residential areas (p = 0.009, and p = 0.002) (Additional file 1).
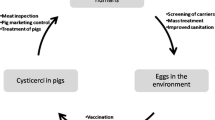
Prevalence of Hookworm infection was significantly higher in children aged 5 years (Pearson chi-square test, p = 0.045) than in children aged 1 year. There was significant sex difference in the prevalence of Hookworm infection (Pearson chi-square test: p = 0.004), but insignificant sex difference was observed in the prevalence of A. lumbricoides and T. trichiura infections (Pearson chi-square test: p = 0.298 and p = 0.657). The prevalence of Hookworm and A. lumbricoides coinfections was 2.8% (16/562). The 4 year old children exhibited the highest 4.5% (6/133) infection prevalence of (Hookworm + A. lumbricoides) co-infection, compared to other age groups (Additional file 1). However, these differences were not statistically significant (Pearson chi-square test, p = 0.693). Children aged 3–4 years had no T. trichiura infection. None of the children were diagnosed with multiple STH (Fig. 1, Additional file 2). Hookworm and A.lumbricoides infections were more prevalent 22.9% (95%CI: 0.18–0.28) among children living in homes where household members defecated in the open (Pearson chi-square test: p < 0.001) (Fig. 2, Additional file 3).
Intensity of soil transmitted helminths among preschool-age children
The geometric mean faecal egg count of Hookworm among infected children was 696.1 EPG (range: 48–13,200). For A. lumbricoides, it was 569.7 EPG (range: 120–7200) and for T. trichiura the count was 440.0 EPG (range: 168–1920). The geometric mean faecal egg count of Hookworm among children aged 5 years was 936.9 EPG, (95% CI: 562.3–1560.9) significantly higher compared to 482.9 EPG (95% CI: 281.6–828.3) and 689.3 EPG (95% CI: 456.4–1041.0) among children aged 1–2 and 3–4 years, respectively (F = 4.36, p = 0.012). Children infected with A. lumbricoides had the highest 663.6 EPG (95% CI: 436.5–1009.0) compared to the other age groups. However, this difference was statistically insignificant (F = 0.4, p = 0.668). Similarly there was insignificant age difference in the T. trichiura infection among PSAC (F = 1.37, p = 0,254). Females had the highest geometric mean faecal egg counts of hookworm 789.8 EPG (95% CI: 511.6–1219.3), compared to the mean faecal egg counts of 539.0 EPG (95% CI: 446.9–913.6) for males (t = − 3.21, p = 0.007). The rest of the details are shown in Table 3 below.
Of the children whose stool samples were positive for Hookworm infection, 12.6% (71/562) had light (1–1999 EPG) intensity, 3.4% (19/562) had moderate (2000–3999 EPG) and 2.0% (11/562) had heavy (> = 4000 EPG) infections intensity. As for A. lumbricoides infections, 14.4% (81/562) had light (1–4999epg) infection intensity, 0.5% (3/562) had moderate (5000–49,999 EPG) infection intensity. The proportions of children with light (1–999 EPG) and moderate (1000–9999 EPG) T. trichiura infection were 0.4% (2/562) and 0.2% (1/562), respectively. All the participating children had no heavy A. lumbricoides and T. trichiura infections, according to WHO classification [38]. The rest of the details are shown in Fig. 3 below.
Factors associated with STH infections among preschool-age children
Additional file 4 shows the distribution of background and socio-behavioural factors associated with STH infections among PSAC. Age had significant association with STH infection (p = 0.002) that PSAC aged 5 years were 1.2 times more likely (adj.PR = 1.2, 95% CI: 1.2–2.6) to be infected than those aged 1–2 years. After adjusting for gender, handwashing before eating and after defecation, sandal wearing, meal preparation, eating raw/uncooked vegetable, eating unwashed fruits, place of residence, toilet facility, human/domestic wastes disposal, SES, caretaker’s education, knowledge about STH infection and child de-worming. The odds of infection were 2.6 times higher (adj.PR = 2.6, 95% CI: 1.9–3.6) for children who rarely wash hands after defecation compared to those who often wash hands after defecation. Children who were reported to have eaten raw or uncooked vegetables were 1.9 time more affected (adj. PR = 1.9, 95% CI: 1.3–2.7) than those who eat cooked vegetables. The odds of infection were 1.8 times higher (adj. PR = 1.8, 95% CI: 1.1–2.8) for children eating fruits without washing or peeling them off as compared to children who wash or peel off before eating fruits. Children who did not swallow deworming drugs for STH were 1.4 times at higher risk (adj. PR = 1.4, 95% CI: 1.0–1.8) of being infected with STH as compared to those who swallow the drugs As expected, children from families that practiced unsanitary disposal of faeces were 1.5 times more likely (adj.PR = 1.5, 95% CI: 1.1–2.0) to be infected with STH than those from families that practice sanitary disposal,after adjusting for the effects of other significant factors in the model. The other considered socio-demographic and economic factors didn’t show significant level of association with STH infection (Additional file 4).
After adjusting for the effects of other significant factors in the model and potentially confounding and/or modifying variables, we found that older age, not handwashing with soap after defecation, eating vegetables and fruits without washing them, improper disposal of youngest child faeces, having caretakers with tertiary education and not deworming PSAC regularly were statistically and independently associated high risk for infections with STH. On the other hand, wearing sandal most of time while outside the home, having children’s food prepared by a person aged 20 years above, living in upland area, using pit latrine for defecation, moderate knowledge about STH infection and belonging to a family of highest socio-economic status were statistically and independently associated with lower risk of STH infection among PSAC.
Discussion
The overall prevalence of STH infection in PSAC was 26.5%, which is higher than the estimated prevalence of 9% among the PSAC in Hoima district. This is not surprising and it shows that community survey may be more effective in identifying PSAC with STH infections than facility-based secondary data [6, 23, 24]. The overall prevalence of the current study was also higher than the prevalences of 19.7, 23.3 and 24.3% reported in studies conducted in Dschang (Cameroon), Butajiri (Ethiopia) and Wonji Shoa sugar estate (Ethiopia) [15, 39, 40]. However, it is lower than the results of studies conducted in Sheska Kekele (Ethiopia) and Osun State (Nigeria) [41, 42]. The differences in the prevalence and distribution of STH among different communities might be due to differences in environmental conditions and poor knowledge and awareness about STH [15, 43]. For instance, areas with poor drainage system may experience frequent flooding and surface run-off during rainy seasons. This may lead to contamination of vegetables and fruits gardens and water sources especially in areas with poor human and domestic waste disposal system. Such conditions expose the children to contaminated soil, thus increasing their susceptibility to STH infection [36, 44].
In the present study, Hookworm was the most common species of STH recovered from the children. This is consistent with the findings of similar studies conducted in other settings [43, 45]. In rural settings where children walk bare foot, Hookworm infection may be more prevalent than A. lumbricoides and T.trichiura [30]. Other studies have reported T.trichiura as the predominant STH among PSAC [41, 46, 47]. These areas have cold climatic conditions, more favourable for the survival of T.trichiuris [44]. Many endemic countries have designed and implemented short deworming treatment intervals (3-monthly) with Albendazole and praziquantel combined with health education on personal and environmental hygiene so as to reduce the prevalence of intestinal helminths among children. Currently, Uganda is implementing four-monthly antihelminthic treatments with albendazole deworming program under the child health day plus strategy, which started in 2004. However, the effectiveness of the control efforts remain difficult to measure because of lack of routine monitoring, surveillance and periodic program evaluation [1, 20].
Although our study focused on the preschool-age children, the 26.5% prevalence reported is higher than the 17.2% prevalence that Standley and colleagues reported in their study of intenstinal schistosomiasis and STH infections among school going children in Lake victoria Region of Uganda [48]. This clearly demonstrates that STH infection is still a public health problem not only among school-age children but also among PSAC. Previous studies have revealed that moderate to heavy SHT infection could result in chronic dysentery, iron deficiency anaemia, intestinal obstruction, reduced physical growth and cognitive development [15, 49, 50]. These studies reported light and moderate STH infections among PSAC, which is similar to the results of our finding. This therefore suggest that PSAC continue to suffer from heavy infection intensity, which eventually leads to long term physical and mental growth retardations.
In this study, females had higher mean egg intensity of Hookworm infection than males. Other studies have congruously demonstrated that females have indeed heavy worm burdens, compared to their male counterpart [42, 51]. However, the cause of this in PSAC is yet unknown [42, 52] and could be attributed to behavioural differences between males and females [42, 52]. A study conducted in South Africa found a strong association between soil eating and Ascaris infection among school-age females. There is need to conduct further studies to explore factors that may explain observed gender differences in worm specific infection intensity among PSAC in these study areas.
The results of our findings showed that the likelihood of being infected with STH is significantly higher in children aged 5 years than in children aged 1–2 year. This is in conformity with the findings from other studies [15, 53, 54]. This is not surprising because in rural settings, hygiene and sanitation conditions are normally poor, yet it is allowed for older PSAC to interact with other children in the neighborhood. Their playful behaviours expose them to contaminated soil, food and/or water, hence increasing the risk of re-infection [4, 39, 55].
Studies conducted in Lake Victoria Region of Uganda and Western Côte d’Ivoire revealed that lack of funding for logistics and community mobilization in hard to reach areas hampers efforts to increase uptake of deworming treatment [7, 48, 56]. The results from our study showed that PSAC living in lowland residential areas were associated with higher likelihood of being infected with STH than those in upland areas. This suggests that apart from unhygienic conditions they face, many children in lowland and hard to reach areas may increasingly be exposed to infections mainly because some of them miss out deworming treatment scheduled for April and October of every year. In the rural context, caretakers may be busy preparing their gardens for cultivation as well as harvesting crops during the months of April and October respectively. This may contribute to forgetting deworming program schedule unless they are regularly reminded using Information, Education and Communication (IEC) materials. Another reason for missing out deworming treatment could be attributed to health workers’ failure to reach children with the deworming services because of logistical challenges.
Although the likelihood of acquiring STH infection was higher among children of caretakers with tertiary education than those whose caretakers had no formal education, the number is small (tertiary education 41) compared to other groups. Strikingly, the actual prevalence is lower in the tertiary group compared to the no formal education group (24.4 to 38.9%). This is surprising and it suggests that while the number of highly educated caretakers in the rural communities is relatively small, most of them may spend more time in outdoor activities as they fend for their families than they have time with their children. In their absence, teenagers who may maintain poor personal and food hygiene are forced to take care of the young ones, hence increasing PSAC’s susceptibility to infection. This argument is supported by the results of our finding that in homes where meals (breakfast and lunch) for young children are normally prepared by persons aged < 15 years, the risk of STH infection is higher than in homes where meals are normally prepared by persons aged ≥20 years. Further research is needed to explore the reasons: “Why children from families of caretakers with tertiary education tend to be at higher risk for STH infections than children of caretakers with no formal education?”
The results of this study revealed that personal hygiene such as clean hands and sandals wearing play important role in transmission of STH infections among the PSAC. This is similar to the findings of other studies [31, 43, 53]. In poor rural communities, there is high tendency for children to walk barefoot and to interact with contaminated soil, water and objects, thus increasingly exposing them to different forms of infections including STH [57, 58]. Sandal wearing and hand washing with soap after defecation and before eating food are some of the preventive measures against STH. However, unless caretakers of children understand that the larvae/eggs of parasitic worms can be transmitted through soil, skin and ingestion of dirty food and water, efforts to reduce the prevalence and burden of STH infection may be frustrated. There is need to increase people’s awareness on the importance of proper personal and environmental hygiene particularly in communities with poor water, sanitation and hygiene. This study also affirms that eating unwashed fruits and uncooked vegetable were positively associated STH infection, which is similar to what was reported in other studies [49, 53]. This could imply lack of knowledge about transmission and prevention of STH [39, 58].
In this study, open defecation, unsanitary disposal of faeces of young children and inadequate knowledge about transmission and prevention of STH were factors associated with STH infections among PSAC. This is similar to what other studies have reported [16, 39, 45, 59]. This implies that in situations where human and animal wastes are improperly disposed, the level of transmission of the infective eggs of parasitic worm is high [45]. It could also imply poor living standard and low level of education of caretakers, which may lead to poor access to safe water supply and improper human, animal and domestic wastes disposal system. Using self reports to factors associated with STH infections are also noted in the current study. However, we controlled it by using validated tools. There were some limitations in this study; firstly, anticipated higher prevalence of A. lumbricoides and T.trichiuris infections than what was reported in the current study if we had conducted a study during the rainy season of the year (June–August 2016). During this period children may increasingly be exposed to contaminations as they eat a lot of fruits and vegetables. Secondly, the reasons as to why girls presented with higher Hookworm intensity than boys and why some children did not receive de-worming treatment, could have been established through qualitative survey in the study area, thirdly, the average time taken to deliver stool samples for examinations was 4 h. Therefore, adding formol-ether with a delay of more than 4 h could have reduced our ability to detect more Hookworm infection and fourthly, we expected that more children would be diagnosed with STH infection if we had collected more than one stool sample per child on consecutive days. However, we increased chance of diagnosing STH by increasing the number of slide per sample during stool examinations. We also used experienced laboratory technicians to independently validate results by re-examining sample slides. There is need to conduct further studies to explore the reasons and draw strong conclusion about gender differences in worm specific infection intensity among PSAC in the study areas.
Conclusion
The prevalence of Soil transmitted helminths infection among preschool-age children in Hoima district was 26.5%. Hookworm infection intensity was the highest followed by A. lumbricoides and the mean egg intensity was higher among older children than younger ones. Not washing hands with soap after defecation, eating vegetables and fruits without proper cooking and or washing them, improper disposal of faeces of young children and irregular deworming of preschool-age PSAC are some of the factors associated with STH infection. There is need to create awareness about latrine construction and utilization as well as the importance of keeping personal and environmental hygiene particularly in communities with poor Water Sanitation and Hygiene (WASH). Deworming programs should focus on reaching communities in lowland areas, in addition to exploring the feasibility and cost effectiveness of shortening deworming treatment intervals from 6-monthly to 4-monthly, in order to reduce the risk of STH infections among PSAC.
Abbreviations
- CI:
-
Confidence interval
- EPG:
-
Eggs per gram of stool
- EPI:
-
Expanded program on immunization
- GM:
-
Geometric mean
- IEC:
-
Information, education and communication
- JMP:
-
Joint monitoring programme
- PCA:
-
Principal component analysis
- PR:
-
Prevalence ratio
- PSAC:
-
Preschool-age children
- SD:
-
Standard deviation
- SES:
-
Socio-economic status
- STH:
-
Soil-transmitted helminthiasis
- UNICEF:
-
United Nations International Children Education Funds
- WASH:
-
Water sanitation and hygiene
- WHO:
-
World Health Organization
References
WHO. Soil transmitted helminthiasis: estimates of the number of children needing preventive chemotherapy and number treated, 2009. Wkly Epidemiol Rec. 2011;25(86):257–68.
Brooker S. Estimating the global distribution and disease burden of intestinal nematode infections: adding up the numbers–a review. Int J Parasitol. 2010;40(10):1137–44.
Pullan RL, Smith JL, Jasrasaria R, Brooker SJ. Global numbers of infection and disease burden of soil transmitted helminth infections in 2010. Parasit Vectors. 2014;7(1):37.
Knopp S, Stothard JR, Rollinson D, Mohammed KA, Khamis IS, Marti H, Utzinger J. From morbidity control to transmission control: time to change tactics against helminths on Unguja Island, Zanzibar. Acta Trop. 2013;128(2):412–22.
Nalugwa A, Olsen A, Tukahebwa M, Nuwaha F. Intestinal schistosomiasis among preschool children along the shores of Lake Victoria in Uganda. Acta Trop. 2015;142:115–21.
Ssentamu J, Alinaitwe E, Nyangoma J, Nsita G: Hoima water sanitation and hygiene Anual Report-2015. 2015.
Brooker S, Kabatereine NB, Smith JL, Mupfasoni D, Mwanje MT, Ndayishimiye O, Lwambo NJ, Mbotha D, Karanja P, Mwandawiro C. International Journal of Health Geographics. Int J Health Geogr. 2009;8:42.
Freeman M, Chard A, Nikolay B, Garn J, Okoyo C, Kihara J, Njenga S, Pullan R, Brooker S, Mwandawiro C. Associations between school-and household-level water, sanitation and hygiene conditions and soil-transmitted helminth infection among Kenyan school children. Parasit Vectors. 2015;8(1):412.
Lwanga F, Kirunda BE, Orach CG. Intestinal helminth infections and nutritional status of children attending primary schools in Wakiso District, Central Uganda. Int J Environ Res Public Health. 2012;9(8):2910–21.
Hotez PJ, Brindley PJ, Bethony JM, King CH, Pearce EJ, Jacobson J. Helminth infections: the great neglected tropical diseases. J Clin Investig. 2008;118(4):1311–21.
Bethony J, Brooker S, Albonico M, Geiger SM, Loukas A, Diemert D, Hotez PJ. Soil-transmitted helminth infections: ascariasis, trichuriasis, and hookworm. Lancet. 2006;367(9521):1521–32.
Dalal S, Beunza JJ, Volmink J, Adebamowo C, Bajunirwe F, Njelekela M, Mozaffarian D, Fawzi W, Willett W, Adami H-O. Non-communicable diseases in sub-Saharan Africa: what we know now. Int J Epidemiol. 2011;40(4):885–901.
Aikins A-G, Unwin N, Agyemang C, Allotey P, Campbell C, Arhinful D. tackling Africa's chronic disease burden: from the local to the global. Glob Health. 2010;6(1):5.
Muhumuza S, Olsen A, Katahoire A, Nuwaha F. Uptake of preventive treatment for intestinal schistosomiasis among school children in Jinja district, Uganda: a cross sectional study. PLoS One. 2013;8(5):e63438.
Shivairo R, Muleke C, Mukabane D, Kumba J. Soil transmitted helminthes prevalence among pre-school age children in Elburgon municipality, Kenya. J Bio, Agri Health. 2014;4(21):36–41.
Ojurongbe O, Oyesiji K, Ojo J, Odewale G, Adefioye O, Olowe A, Opaleye O, Bolaji O, Ojurongbe T. Soil transmitted helminth infections among primary school children in Ile-Ife southwest, Nigeria: a cross-sectional study. Int Res J Med Med Sci. 2014;2(1):6–10.
Saboyá MI, Catalá L, Nicholls RS, Ault SK. Update on the mapping of prevalence and intensity of infection for soil-transmitted helminth infections in Latin America and the Caribbean: a call for action. PLoS Negl Trop Dis. 2013;7(9):e2419.
Abera B, Alem G, Yimer M, Herrador Z. Epidemiology of soil-transmitted helminths, Schistosoma mansoni, and haematocrit values among schoolchildren in Ethiopia. The Journal of Infection in Developing Countries. 2013;7(03):253–60.
WHO: Prevention and control of Schistosomiasis and Soil-Transmitted Helminths. 2003.
Parker M, Allen T. Does mass drug administration for the integrated treatment of neglected tropical diseases really work? Assessing evidence for the control of schistosomiasis and soil-transmitted helminths in Uganda. Health research policy and systems. 2011;9(1):3.
Kabatereine NB, Brooker S, Koukounari A, Kazibwe F, Tukahebwa EM, Fleming FM, Zhang Y, Webster JP, Stothard JR, Fenwick A. Impact of a national helminth control programme on infection and morbidity in Ugandan schoolchildren. Bull World Health Organ. 2007;85(2):91–9.
MOH: Uganda Ministry of Health Annual Report. 2015.
Kabagambe D, Byenume F, Ruyonga J: Hoima District health Indicator Report-2015. 2015.
Ruyonga J, Byanguma F, Kabagmbe D, Kugonza F: The district health information system (DHIS) for FY 2014/2015. 2015.
Bennett S, Woods T, Liyanage WM, Smith DL. A simplified general method for cluster-sample surveys of health in developing countries. World Health Stat Q. 1991;44(3):98–106.
Turner AG. Sampling strategies. United Nations Statistics Division: Handbook on designing of household sample surveys Geneva; 2003.
Arold F, Bostoen K, Croft T, David P, Frazier C, Henderson M, Hueb J, Kleinau E, Kolsky P, Luyendijk R, Mugai R, Wardlaw T. Core questions on drinking-water and sanitation for household surveys. Geneva, Switzerland: World Health Organization, United Nations Children’s Fund; 2006, 24. WHO, UNICEF: 2006.
Foreyt WJ. Diagnostic parasitology. Vet Clin N Am Small Anim Pract. 1989;19(5):979–1000.
Suwansaksri J, Nithiuthai S, Wiwanitkit V, Soogarun S, Palatho P. The formol-ether concentration technique for intestinal parasites: comparing 0.1 N sodium hydroxide with normal saline preparations. Southeast Asian J Trop Med Public Health. 2003;33:97–8.
Alemu G, Mama M. Intestinal helminth co-infection and associated factors among tuberculosis patients in Arba Minch, Ethiopia. BMC Infect Dis. 2017;17(1):68.
Alelign T, Degarege A, Erko B. Soil-transmitted helminth infections and associated risk factors among schoolchildren in Durbete town. Northwestern Ethiopia. Journal of parasitology research. 2015;2015
Mayega RW, Guwatudde D, Makumbi F, Nakwagala FN, Peterson S, Tomson G, Ostenson C-G. Diabetes and pre-diabetes among persons aged 35 to 60 years in eastern Uganda: prevalence and associated factors. PLoS One. 2013;8(8):e72554.
UBOS: Uganda Bureau of Statistics, Macro International Inc. (2007) Uganda Demographic and Health Survey 2006. In:, Calverton M, USA: UBOS and Macro. UBOS and Macro International Inc.. pp. 19–20. 2006.
Filmer D, Pritchett LH. Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in states of India. Demography. 2001;38(1):115–32.
Mayega RW, Makumbi F, Rutebemberwa E, Peterson S, Östenson C-G, Tomson G, Guwatudde D. Modifiable socio-behavioural factors associated with overweight and hypertension among persons aged 35 to 60 years in eastern Uganda. PLoS One. 2012;7(10):e47632.
Campbell SJ, Savage GB, Gray DJ, Atkinson J-AM, Magalhaes RJS, Nery SV, McCarthy JS, Velleman Y, Wicken JH, Traub RJ. Water, sanitation, and hygiene (WASH): a critical component for sustainable soil-transmitted helminth and schistosomiasis control. PLoS Negl Trop Dis. 2014;8(4):e2651.
Charles B, Babirye J, Atuyambe L: The level and determinants of male partner involvement in routine child immunization Care in Hoima District Uganda: a cross-sectional study. 2014.
Montresor A, Crompton D, Hall A, Bundy D, Savioli L. Guidelines for the evaluation of soil-transmitted helminthiasis and schistosomiasis at community level. Geneva: World Health Organization; 1998. p. 1–49.
Fusi-Ngwa C, Besong E, Pone JW, Mbida M. A cross-sectional study of intestinal parasitic infections in children in Ghettoed, diverse and affluent communities in Dschang, west region, Cameroon. Open Access Library J. 2014;1(09):1.
Degarege A, Erko B. Prevalence of intestinal parasitic infections among children under five years of age with emphasis on Schistosoma mansoni in Wonji Shoa sugar estate, Ethiopia. PloS one. 2014;9(10):e109793.
Nyantekyi LA, Legesse M, Belay M, Tadesse K, Manaye K, Macias C, Erko B. Intestinal parasitic infections among under-five children and maternal awareness about the infections in Shesha Kekele, Wondo Genet, Southern Ethiopia. Ethiop J Health Dev. 2010;24(3):185–90
Kirwan P, Asaolu SO, Molloy SF, Abiona TC, Jackson AL, Holland CV. Patterns of soil-transmitted helminth infection and impact of four-monthly albendazole treatments in preschool children from semi-urban communities in Nigeria: a double-blind placebo-controlled randomised trial. BMC Infect Dis. 2009;9(1):1.
Kabatereine NB, Standley CJ, Sousa-Figueiredo JC, Fleming FM, Stothard JR, Talisuna A, Fenwick A. Integrated prevalence mapping of schistosomiasis, soil-transmitted helminthiasis and malaria in lakeside and island communities in Lake Victoria, Uganda. Parasit Vectors. 2011;4:232.
Gungoren B, Latipov R, Regallet G, Musabaev E. Effect of hygiene promotion on the risk of reinfection rate of intestinal parasites in children in rural Uzbekistan. Trans R Soc Trop Med Hyg. 2007;101(6):564–9.
Echazú A, Bonanno D, Juarez M, Cajal SP, Heredia V, Caropresi S, Cimino RO, Caro N, Vargas PA, Paredes G. Effect of poor access to water and sanitation as risk factors for soil-transmitted helminth infection: selectiveness by the infective route. PLoS Negl Trop Dis. 2015;9(9):e0004111.
Nasr NA, Al-Mekhlafi HM, Ahmed A, Roslan MA, Bulgiba A: Towards an effective control programme of soil-transmitted helminth infections among Orang Asli in rural Malaysia. Part 2: Knowledge, attitude, and practices. Parasit Vectors 2013, 6:28.
Ngui R, Lim YAL, Kin LC, Chuen CS, Jaffar S. Association between anaemia, iron deficiency anaemia, neglected parasitic infections and socioeconomic factors in rural children of West Malaysia. PLoS Negl Trop Dis. 2012;6(3):e1550.
Standley CJ, Adriko M, Alinaitwe M, Kazibwe F, Kabatereine NB, Stothard JR. Intestinal schistosomiasis and soil-transmitted helminthiasis in Ugandan schoolchildren: a rapid mapping assessment. Geospat Health. 2009;4(1):39–53.
Wang X, Zhang L, Luo R, Wang G, Chen Y, Medina A, Eggleston K, Rozelle S, Smith DS. Soil-transmitted helminth infections and correlated risk factors in preschool and school-aged children in rural Southwest China. PLoS One. 2012;7(9):e45939.
Albonico M, Allen H, Chitsulo L, Engels D, Gabrielli A-F, Savioli L. Controlling soil-transmitted helminthiasis in pre-school-age children through preventive chemotherapy. PLoS Negl Trop Dis. 2008;2(3):e126.
Holland C, Asaolu S, Crompton D, Whitehead R, Coombs I. Targeted anthelminthic treatment of school children: effect of frequency of application on the intensity of Ascaris lumbricoides infection in children from rural Nigerian villages. Parasitology. 1996;113(01):87–95.
Saathoff E, Olsen A, Kvalsvig JD, Geissler PW. Geophagy and its association with geohelminth infection in rural schoolchildren from northern KwaZulu-Natal, South Africa. Trans R Soc Trop Med Hyg. 2002;96(5):485–90.
Menzies SK, Rodriguez A, Chico M, Sandoval C, Broncano N, Guadalupe I, Cooper PJ. Risk factors for soil-transmitted helminth infections during the first 3 years of life in the tropics; findings from a birth cohort. PLoS Negl Trop Dis. 2014;8(2):e2718.
Verhagen LM, Incani RN, Franco CR, Ugarte A, Cadenas Y, Ruiz CIS, Hermans PW, Hoek D, Ponce MC, de Waard JH. High malnutrition rate in Venezuelan Yanomami compared to Warao Amerindians and creoles: significant associations with intestinal parasites and anemia. PLoS One. 2013;8(10):e77581.
Abu-Madi MA, Behnke JM, Doiphode SH. Changing trends in intestinal parasitic infections among long-term-residents and settled immigrants in Qatar. Parasit Vectors. 2010;3(1):1–13.
Raso G, Matthys B, N'goran E, Tanner M, Vounatsou P, Utzinger J. Spatial risk prediction and mapping of Schistosoma mansoni infections among schoolchildren living in western Côte d'Ivoire. Parasitology. 2005;131(01):97–108.
Ziegelbauer K, Speich B, Mäusezahl D, Bos R, Keiser J, Utzinger J. Effect of sanitation on soil-transmitted helminth infection: systematic review and meta-analysis. PLoS Med. 2012;9(1):e1001162.
Freeman MC, Ogden S, Jacobson J, Abbott D, Addiss DG, Amnie AG, Beckwith C, Cairncross S, Callejas R, Colford JM Jr. Integration of water, sanitation, and hygiene for the prevention and control of neglected tropical diseases: a rationale for inter-sectoral collaboration. PLoS Negl Trop Dis. 2013;7(9):e2439.
Truscott J, Turner H, Anderson R. What impact will the achievement of the current World Health Organisation targets for anthelmintic treatment coverage in children have on the intensity of soil transmitted helminth infections? Parasit Vectors. 2015;8(1):1–12.
Acknowledgements
The authors are so grateful to the caretakers of the study participants for making the study possible. The authors are also thankful to the research assistants: James Christmas, Morris Baguma, Fred Wabuzi and Mary Steward who took part in data collection and Alex Mawa, Grace M. Joyce and Stephen Birungi who conducted laboratory analysis of the stool. Special acknowledgement also goes to Hoima District Health Officer Dr. Joseph Ruyonga and the District Health Inspector Mr. Fredrick Byenume for approving and supporting in data collection processes.
Funding
Funding for Manuscript writing was obtained from the African Field Epidemiology Network (AFENET). No fund was obtained for designing and data analysis.
Author information
Authors and Affiliations
Contributions
Conceptualized the study and designed the study proposal: SO, ME, DT, AH, SK, and JNM. Conducted field survey, data collection and analysis: SO. Wrote the paper: SO. Contributed in interpretation of data for substantial intellectual content: SK, RKM, and JNM. Drafted and revised the manuscript: SO, SK, RKM, DT, ANK, ME, AH and JNM. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by Makerere University School of Public Higher Degree Research and Ethics Committee (HDREC), Reference Number: IRB00005876. Permission was obtained from the district health officer before commencement of the study. Informed assent was obtained from caretakers of the preschool-age children prior to the study. Assent form were distributed to the caretakers of the preschool-age children after indicating to them that the information collected was for planning health interventions and that their participation was completely voluntary and that they were freed to withdraw participation at any time. Those who assented signed and return forms to the research assistants. Caretakers were also informed on the procedure for collecting stool sample, aims, objectives and benefits of the study. Individuals with A. lumbricoides, Ancylostoma spp (Hookworm), T. trichiura or other types of intestinal helminths infections were referred to the nearest health facility for treatment. All caretakers with inadequate knowledge about STH transmission, prevention and de-worming program, were given a health education message by the research assistants at the end of the interview.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Prevalence of soil transmitted helminths infections among the 562 preschool-age children that participated in the study in Hoima. (XLSX 18 kb)
Additional file 3:
Contains data used to draw conclusions. (XLSX 67 kb)
Additional file 4:
Factors associated with Soil-transmitted helminths infections among the 562 preschool-age children that participated in the study in Hoima District. (XLSX 13 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ojja, S., Kisaka, S., Ediau, M. et al. Prevalence, intensity and factors associated with soil-transmitted helminths infections among preschool-age children in Hoima district, rural western Uganda. BMC Infect Dis 18, 408 (2018). https://doi.org/10.1186/s12879-018-3289-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-018-3289-0