Abstract
Background
Klebsiella pneumoniae bloodstream infections (BSIs) occur with significant prevalence and high mortality worldwide. Antimicrobial resistance and virulence are two main factors participating in the pathogenicity of K. pneumoniae. Here we investigated the prevalence of blaKPC and virulence factors in K. pneumoniae isolated from patients with BSIs and their association with clinical outcome.
Methods
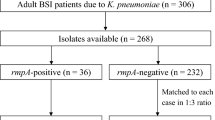
The clinical data of 285 K. pneumoniae BSI cases diagnosed from January 2013 to December 2015 in a Chinese university hospital were retrospectively evaluated. The “string test” was performed to identify hypermucoviscous K. pneumoniae (HMKP). blaKPC, rmpA, magA and serotype-specific genes were detected by PCR amplification. Finally, a Cox proportional hazards model was employed to determine the predictors of 14-day mortality.
Results
Of these isolates, the prevalence of blaKPC and rmpA were 33.3% (95/285) and 31.6% (90/285) respectively. 69 isolates (24.2%, 69/285) were HMKP. rmpA was strongly associated with HM phenotype. The KPC-producing KP and HMKP were almost non-overlapping and only three HMKP isolates harbored blaKPC. K1 (28, 40.6%) and K2 (22, 31.9%) were the most common serotypes in HMKP. 44.9% of HMKP BSIs had origin of biliary tract infection or liver abscess. The 14-day mortality was 100% in blaKPC+/HM+ subgroup (3/3), followed by blaKPC+/HM− (39/92, 42.4%), blaKPC−/HM+ (5/66, 7.6%) and blaKPC−/HM− (7/124, 5.6%). The 14-day cumulative survival was significantly different between blaKPC+ and blaKPC− subgroup (Log-rank p < 0.001) but almost equal between blaKPC−/HM+ and blaKPC−/HM− subgroup (Log-rank p = 0.578) under the condition of comparable illness severity between blaKPC−/HM+ and blaKPC−/HM− subgroup. Independent risk factors for 14-day mortality were Pitt bacteremia score (HR 1.24, CI 95% 1.13–1.36, p < 0.001), Charlson comorbidity index (HR 1.24, CI 95% 1.09–1.41, p = 0.001), septic shock (HR 2.61, CI 95% 1.28–5.35, p = 0.009) and blaKPC (HR 2.20, CI 95% 1.06–4.54, p = 0.034).
Conclusions
Most of HMKP were antibiotic-susceptible and people infected received appropriate antimicrobial therapy, which may explain the favorable outcome of HMKP BSIs. The KPC-producing HMKP BSIs were scarce but life-threatening. blaKPC was valuable in predicting 14-day mortality.
Similar content being viewed by others
Background
Klebsiella pneumoniae is the second most common pathogen in Enterobacteriaceae bloodstream infections (BSIs). The reported mortality rate of K. pneumoniae BSIs varies from 15 to 79% [1,2,3,4], which was lower than that of Acinetobacter baumannii BSIs (30 to 84%) [5, 6] but higher than Escherichia coli (5 to 22%) [7,8,9]. Antimicrobial resistance and virulence are generally considered as significant factors in the pathogenicity of K. pneumoniae. During the past years, as the increasing of antimicrobial resistance, especially the emerging of carbapenem-resistant K. pneumoniae, a serious dilemma has been posed to clinical therapy [10]. K. pneumoniae carbapenemase (KPC) is the most important genetic mechanism of carbapenem resistance [11]. Several studies that focus on KPC-producing K. pneumoniae (KPC-KP) BSI have found a high mortality rate [2,3,4]. However, similar large research in our geographical area is still missing.
Hypervirulent K. pneumoniae (hvKP), traditionally characterized as hypermucoviscous (HM) phenotype, has emerged as a significant pathogen since first described in 1986 [12]. The HM phenotype has been proved to be strongly associated with rmpA (regulator of the mucoid phenotype gene A) [13]. The other virulence-associated factors in hvKP include magA (mucoviscosity-associated gene A) and capsular polysaccharide, especially K1 and K2 serotypes. These factors confer K. pneumoniae the ability to colonize mucous surface and evade the phagocytosis of immune cells [14]. hvKP is usually associated with severe infectious diseases, such as pyogenic liver abscess, endophthalmitis, meningitis, and necrotizing fasciitis [15, 16], but only limited information is available about hvKP BSIs [1, 17, 18]. Studies in animal model have shown that both the HM phenotype and the capsular serotypes (K1 and K2) are strongly associated with death [19], but only small amounts of clinical studies with small sample size have evaluated the impact of these virulence factors in the outcome of K. pneumoniae BSIs hitherto, and the results are still controversial [1, 18, 20].
Generally, most HMKP are only resistant to ampicillin. There is largely non-overlapping between antimicrobial-resistant and HM phenotype, but recent study shows the antimicrobial resistant rate of HMKP is increasing [20]. Some cases of KPC-producing HMKP infections have been already reported in China [21, 22]. More surveillance is needed to illustrate the prevalence of KPC-producing HMKP strains. Therefore, we conducted this three-year period study of K. pneumoniae BSIs in a Chinese university hospital for two main objects: investigate microbial characteristics including the prevalence of blaKPC responsible for carbapenem resistance, and several virulence-associated factors; and analyze their impact on clinical outcomes.
Methods
Setting and design
This retrospective cohort study was conducted in The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, China, a 2500-bed tertiary hospital having approximately 131,000 admissions each year, and three intensive care units (ICU): a 29-bed medical ICU, a 29-bed surgical ICU and a 15-bed emergency ICU. There is infectious diseases service at this hospital.
The patients aged over 18 years and developed K. pneumoniae BSIs during hospitalization were identified between January 2013 and December 2015. Only the first episode for each patient was included in our analysis. Patients with polymicrobial bacteremia were excluded. The relevant clinical and microbiological data we needed were extracted from the electronic or paper medical records and microbiologic database. In present study, the data was de-identified and hence informed consent was waived. Ethical approval was granted from the Ethics Committees and review board of the First Affiliated Hospital, College of Medicine, Zhejiang University.
Variables and definitions
A K. pneumoniae BSIs were defined as an infection confirmed by blood culture positive for K. pneumoniae and clinical signs of the systemic inflammatory response syndrome [23].
The following data were collected: demographics (sex, age), date and unit of hospitalization; infections acquisition categorized as either nosocomial or community-acquired [20]; baseline severity of illness estimated by the Acute Physiology and Chronic Health Evaluation (APACHE) II score; comorbidities and severity of underlying diseases assessed by the Charlson comorbidity index [24]; severity of bacteremia calculated using Pitt bacteremia score [25]; and source of bacteremia. Immunosuppressive state (chemotherapy, radiotherapy and/or immunosuppressive drugs), septic shock and multiple organ dysfunction syndrome (MODS) at the onset of BSI were also documented. Empirical antibiotics therapy was defined as therapy given within 24 h of the culture being taken, while definitive antimicrobial therapy was considered the administration of antibiotics for at least 48 h. Antibiotics therapy was considered appropriate if it include at least on antimicrobial agent to which the causative pathogen displayed in vitro susceptibility [26].
Assessment of the resistance profile and bla KPC
The isolate identification and antimicrobial susceptibility testing were conducted by Vitek 2 automated system (bioMérieux, France). Minimum inhibitory concentrations (MICs) were categories according to the breakpoints defined by Clinical and Laboratory Standards Institute (CLSI, 2016). For tigecycline, disk diffusion method was used and the results were interpreted according to the U. S. Food and Drug Administration criteria (susceptible ≥19 mm, resistant < 14 mm).
The presence of the blaKPC was investigated by PCR and sequencing [27].
Detection of the HM phenotype, capsular serotype and virulence genes
The “string test” was used to identify HM phenotype. A positive string test was defined as the generation of a viscous string of > 5 mm in length, when using a bacteriology loop to stretch bacterial colony cultured on an agar plate overnight at 37 °C. [14].
The virulence genes magA, rmpA, and serotype-specific genes for the K1, K2, K5, K20, K54 and K57 capsular serotype were amplified by PCR as described previously [20].
Multilocus sequence typing (MLST)
In order to identify prevalent high-risk clones, MLST of the isolates from the non-survivors subgroup was performed. It was done with seven housekeeping genes (gapA, infB, mdh, phoE, pgi, rpoB and tonB) according to the protocol on the MLST website [28]. Sequence types (STs) that had not been described previously were submitted to the database.
Statistical analysis
Continuous variables were expressed as mean and standard deviation (SD) for normally distributed data, or as median and interquartile rang (IQR) for non-normal data. Categorical variables were presented as absolute numbers and their relative frequencies. The two-tailed t test or Mann-Whitney test was used for continuous variables, and the chi-square test or Fisher exact test was used for categorical variables, when appropriate. A Cox regression model by including the variables emerging from univariate analysis with P value < 0.1 as well as clinically important were applied to analysis the effect of different variables on 14-day mortality. In order to estimate the risk of death, survival curves were constructed with the Kaplan-Meier method and log-rank test. All the statistical analyses were two-tailed, and P value ≤0.05 was considered significant. The SPSS software (version 20.0) was used for data analysis in the present study.
Results
Microbiological characteristics
During the study period, a total of 285 K. pneumoniae BSI cases that met the inclusion criteria were identified. The characteristics of antimicrobial resistance and virulence-associated factors according to blaKPC and HM phenotype are shown in Table 1.
34.7% isolates (99/285) displayed non-susceptibility to carbapenem, most of which (92.9%, 92/99) carried blaKPC. There were another three blaKPC positive isolates were carbapenem susceptible. Amikacin and tigecycline had the lowest non-susceptible rates among the studied drugs. The detailed antimicrobial non-susceptibility profiles of the 15 drugs are listed in Additional file 1: Table S1.
The HM phenotype was found in 69 (24.2%) isolates. K1 (28 isolates) and K2 (22 isolates) were the most common serotypes. PCR detected virulence gene rmpA in 90 isolates (31.6%) and magA in 24 isolates (8.4%). The detection rates of K1, K2, rmpA and magA were significantly higher in HM+ group than HM− group. Multivariate analysis showed rmpA and K2 to be the independent factor truly associated with HM phenotype (Additional file 2: Table S2).
Compared with non-KPC-KP, KPC-KP showed much more antimicrobial resistance, but less HM phenotype, capsular serotype, magA and rmpA.
The HMKP and KPC-producing KP were almost non-overlapping. Three HMKP were proved to carry blaKPC, in which two isolates also harbored capsular serotype genes and rmpA.
Clinical characteristics according to bla KPC and HM phenotype
According to blaKPC and HM phenotype, the 285 KP BSI cases were divided into four subgroups, blaKPC+/HM+, blaKPC+/HM−, blaKPC−/HM+, and blaKPC−/HM−. The baseline demographic and clinical characteristics are shown in Table 2.
Due to the limited number, blaKPC+/HM+ subgroup was not included in statistical analysis.
To compare with blaKPC−/HM+ and blaKPC+/HM− subgroups, blaKPC+/HM− subgroup showed apparently distinct characterization by statistical analysis. Patients in the latter subgroup were more likely to be nosocomial acquired infection (96.7%) and have ICU hospitalization (40.2%). Respiratory tract source of BSIs was more frequent in blaKPC+/HM− subgroup, but fewer biliary tract or liver abscess origin. This group also had much severer illness process (higher APACHE II score and Pitt bacteremia score; more incidence of MODS and septic shock), less opportunity to receive appropriate antibiotic therapy and much higher 14-day mortality.
There were no significant differences in demographic data, underlying diseases, Charlson comorbidity index, severity of illness evaluation (APACHE II score, Pitt bacteremia score, MODS and septic shock) and 14-day mortality between the blaKPC−/HM+ and blaKPC−/HM− subgroups. However, community acquired infection, liver abscess source of BSIs and immunocompetent state were more frequent in blaKPC−/HM+ subgroup.
Outcomes and mortality predictors
Most fatalities occurred within 14 days after K. pneumoniae BSIs onset (18.9%, 54/285) and the in-hospital mortality rate was 32.6% (93/285). The 14-day mortality of three blaKPC+/HM+ KP-BSI cases was 100%, followed by blaKPC+/HM− (42.4%), blaKPC−/HM+ (7.6%) and blaKPC−/HM− subgroup (5.6%).
Kaplan-Meier curves were used to evaluate the impact of blaKPC and HM phenotype on 14-day survival. As shown in Fig. 1a, the 14-day cumulative survival was significantly different between blaKPC+ and blaKPC− group (55.8% versus 93.7%, P < 0.001). Although the 14-day cumulative survival of HM− group (78.7%) was lower than that of HM+ group (88.4%), the difference was not statistically significant (P = 0.08, Fig. 1b). The prevalence of blaKPC was significantly higher in HM− group than in HM+ group (42.6% versus 4.3%, P < 0.001. Table 1), which may contribute to the relatively low survival in HM− group. In order to exclude the influence of blaKPC, comparison of the 14-day cumulative survival was performed between blaKPC−/HM+ and blaKPC−/HM− subgroups. It also showed minor impact of HM phenotype on outcome (cumulative survival, 92.4% for blaKPC−/HM+ versus 94.4% for blaKPC−/HM−; Log-rank P = 0.578) under the condition of comparable illness severity between blaKPC−/HM+ and blaKPC−/HM− subgroups.
In the univariate analysis, several clinical and microbial factors were significantly associated with mortality (Table 3). Patients in nonsurvivor group were more likely to have ICU hospitalization, nosocomial acquired infection, chronic kidney disease, heart disease, and immunosuppression state. This group also had severer illness evaluation and higher prevalence of blaKPC. However, biliary tract or liver abscess sourced BSI, appropriate empiric or definitive antibiotic therapy, rmpA positive and HM phenotype were associated with survival.
Cox regression analysis identified Charlson comorbidity index (HR 1.24, CI 95% 1.09–1.41, P = 0.001), septic shock (HR 2.61, CI 95% 1.28–5.35, P = 0.009), Pitt bacteremia score (HR 1.24, CI 95% 1.13–1.36, P < 0.001), and blaKPC (HR 2.20, CI 95% 1.06–4.54, P = 0.034) as independent predictors of 14-day crude mortality (Table 3).
Molecular genotyping
MLST of the 54 isolates from the 14-day nonsurvival subgroup identified 19 sequence types (STs), as shown in Additional file 3: Figure S1. ST11 was the most prevalent (n = 36, 66.7%). The other STs had only one isolate each. All of the ST11 isolates were blaKPC positive except one isolate. Two cases caused by ST11 were defined as community-acquired infection. However, both of the patients had been hospitalized during previous 2 months. The remaining 34 ST11 cases were unambiguous nosocomial infection. Looking at the detailed clinical epidemiological information of all the 36 ST11 cases, there was no sudden increase in incidence of the infection during this period and the patients who had a close sampling time had non-overlapping stays in the same unit, suggesting just endemicity of ST11 clone in our hospital and nil outbreak happened. Eight HMKP isolates had unique STs. Three blaKPC+/HM+ isolates were ST11, ST893 and ST15, and had apparent diversity in genetic background.
Discussion
The retrospective study involved 285 K. pneumoniae BSI cases occurred from January 2013 to December 2015 in a Chinese hospital. The prevalence of blaKPC and several virulence-associated factors were investigated, as well as the impact of these factors on mortality. It represented one of the largest investigations of K. pneumoniae BSIs in Chinese hospital that focused on microbial and clinical characterization simultaneously.
In this study, the carbapenem resistant rate of K. pneumoniae isolated from BSIs was 34.7%, which was much higher than the result of a national investigation reported by Xu et al. in China (5.5%) [29]. The disparity can be attributed to the variant distribution of blaKPC among regions. As the most important carbapenemase gene of K. pneumoniae, blaKPC was detected in 33.3% of 285 isolates. Although there was no information concerning the detection frequency of blaKPC in K. pneumoniae isolated from BSIs in China hereto, this data was higher than that reported by Yedidah et al. (25.0%) in Israel [3]. MLST showed 66.7% of isolates from the 14-day nonsurvival group was ST11, which belonged to CC258, a well-known international high-risk MDR clone of K. pneumoniae [30]. Almost all of the ST11 isolates were blaKPC positive and caused nosocomial infection in this study. It is believed that the nosocomial clonal dissemination of KPC-producing ST11 K. pneumoniae played a significant role in the high detection rate of blaKPC. In addition, the positive rate of blaKPC was 44.2% in isolates from nosocomial-acquired infection, but only 5.1% in isolates from community-acquired infection. Therefore, including of more nosocomial infection cases (72.3%) and relatively less community infection cases (27.7%) may also lead to the increased overall carbapenem resistant rate.
The study showed 24.2% (69/285) of K. pneumoniae BSI cases were caused by HMKP. This percentage was much higher than that recently reported by Cubero et al. in Spain (5.4%) [17], but lower than that described in other regions of China (31.4% [1] and 28% [20]). In accordance with a number of previous studies, K1 and K2 were the most common serotypes [1, 17, 20, 31]. However, the prevalence of these two serotypes in this study was lower than those reported by other Chinese researchers [1, 20]. Besides the geographic variation, the discrepancy in sample size might account for these differences.
As expected, most HMKP displayed susceptibility to carbapenem (94.2%, 65/69), which was consistent to the traditional view that HMKP is rarely resistant to antibiotics except its intrinsic resistance to ampicillin [21]. However, recent studies have indicated that the degree of antimicrobial resistance of HMKP strains increased over time [20]. Even KPC-producing HMKP isolates have been reported in China [22, 32]. In our study, 4.3% (3 isolates) isolates were identified as KPC-producing HMKP strains and they belonged to three distinctive STs (ST11, ST15 and ST893) without molecular epidemiological relationship, suggesting they were sporadic cases. The isolates of ST11 and ST15 were K-nontypable and rmpA and magA negative. Other factors may be responsible for the HM phenotype. In addition, as far as our best knowledge, it is the first report of KPC-producing HMKP ST893 co-harboring K20 serotype and rmpA.
When classified according to HM and blaKPC phenotype, clinical characteristics were significantly different between subgroups. Besides community acquisition infections (P = 0.001), liver abscess (P = 0.004) and immune status (P = 0.002) were most significantly associated with HMKP (blaKPC−/HM+ versus blaKPC−/HM−). This feature is consistent with previous reports that HMKP usually infects immunocompetent subjects and causes liver abscess [14]. On the contrary, KPC-KP were more likely to be nosocomial acquisition, happen in patients with serious underlying diseases (solid organ transplantation, central nervous diseases and chronic kidney disease) and have respiratory tract or intraabdominal source. These differences indicate that HMKP and KPC-KP each has unique potential reservoir and pathogenicity.
Several studies have reported the mortality of HMKP BSIs was lower than that of cKP BSIs [1, 31]. Although without significant difference, the trend was also observed in this study (14-day mortality, HMKP 11.6% versus cKP 21.3%, Log-rank P = 0.08). Because of low resistant rates, the empirical and definitive anti-infective therapy against HMKP BSIs could be reasonable and effective, which may explain the relatively favorable prognosis. We also performed 14-day survival analysis between blaKPC−/HM+ and blaKPC−/HM− subgroups to exclude the interference of resistance. The result also showed HM phenotype alone had minor impact on the poor prognosis of BSIs (14-day mortality, 7.6% versus 5.6%, P = 0.578). However, new evidence has suggested that a HM phenotype only is not sufficient to indicate a hypervirulent state [33]. Other important virulence-associated factors such as siderophores were not performed in this study may lead to bias on identification of real hypervirulent K. pneumoniae.
Previous studies on KPC-KP BSIs reported mortality rates up to 79% [2]. In this study, the 14-day mortality of KPC-KP BSIs was 44.2%. Compared with patients of non-KPC-KP BSIs, patients of KPC-KP BSIs were more critical (higher APACHE II score and Pitt bacteremia score at the onset of BSIs). It might be that KPC carriage is collinear with severity of illness, and thus mortality might not be necessarily associated with KPC but rather with severity. Cox analysis subsequently showed blaKPC was an independent predictor of 14-day mortality, as well as Charlson comorbidity index, Pitt bacteremia score, and septic shock. Thus, KPC-KP BSIs are associated with a poor outcome. The mortality outside the ICUs in present study was 15.3% (33/216), which although significantly lower than that of patients stayed in ICUs (15.3% vs 38.9%, p = 0.005) but still relative high. Among the 27 patients stayed in hepato-biliary unit suffering from liver transplantation, 9 patients had fatal outcome at day 14. So, the high mortality of these patients (33.3%) might attribute to the overall high mortality of patients outside the ICUs. Additionally, the K. pneumoniae strains isolated from these 9 patients were all positive for blaKPC, which further confirmed that the KPC-KP BSIs were associated with a poor outcome.
The 14-day mortality of the three cases caused by KPC-producing HMKP was 100% in our study. Zhang et al. reported three cases of KPC-producing HMKP infections, in which two were survived and one unknown [32]. However, there was only one BSIs case. In another study, Zhang et al. reported five cases of KPC-producing HMKP BSIs with 100% mortality [22]. Although limited information available, it seemed KPC-producing HMKP BSIs had disastrous outcome.
Conclusions
Our study showed the resistance characteristics and clinical manifestation were significantly different between HMKP BSIs and KPC-KP BSIs. HMKP were usually antibiotic susceptible and associated with favorable outcome of BSIs. blaKPC was an independent predictor of poor outcome. The emergence of KPC-producing HMKP is a potential threat of public health and must be critically monitored.
Abbreviations
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- BSIs:
-
Bloodstream infections
- CI:
-
confidence interval
- cKP:
-
classic K. pneumoniae
- CLSI:
-
Clinical Laboratory Standards Institute
- CNS:
-
central nervous system
- HM:
-
hypermucoviscous
- HMKP:
-
hypermucoviscous K. pneumoniae
- HR:
-
hazard ratio
- hvKP:
-
hypervirulent K. pneumoniae
- ICU:
-
intensive care units
- IQR:
-
interquartile range
- KPC:
-
K. pneumoniae carbapenemase
- KPC-KP:
-
KPC-producing K. pneumoniae
- MICs:
-
minimum inhibitory concentrations
- MLST:
-
multilocus sequence typing
- MODS:
-
multiple organ dysfunction syndrome
- SD:
-
standard deviation
References
Liu YM, Li BB, Zhang YY, Zhang W, Shen H, Li H, et al. Clinical and molecular characteristics of emerging hypervirulent Klebsiella pneumoniae bloodstream infections in mainland China. Antimicrob Agents Chemother. 2014;58:5379–85.
da Silva KE, Maciel WG, Sacchi FP, Carvalhaes CG, Rodrigues-Costa F, da Silva AC, et al. Risk factors for KPC-producing Klebsiella pneumoniae: watch out for surgery. J Med Microbiol. 2016;65:547–53.
Fraenkel-Wandel Y, Raveh-Brawer D, Wiener-Well Y, Yinnon AM, Assous MV. Mortality due to bla KPC Klebsiella pneumoniae bacteraemia. J Antimicrob Chemother. 2016;71:1083–7.
Falcone M, Russo A, Iacovelli A, Restuccia G, Ceccarelli G, Giordano A, et al. Predictors of outcome in ICU patients with septic shock caused by Klebsiella pneumoniae carbapenemase-producing K. pneumoniae. Clin Microbiol Infect. 2016;22:444–50.
Liu Q, Li W, Du X, Li W, Zhong T, Tang Y, et al. Risk and prognostic factors for multidrug-resistant Acinetobacter Baumannii complex bacteremia: a retrospective study in a tertiary Hospital of West China. PLoS One. 2015;10:e0130701.
Freire MP, de Oliveira GD, Garcia CP, Campagnari Bueno MF, Camargo CH, Kono Magri ASG, et al. Bloodstream infection caused by extensively drug-resistant Acinetobacter baumannii in cancer patients: high mortality associated with delayed treatment rather than with the degree of neutropenia. Clin Microbiol Infect. 2016;22:352–8.
Giannella M, Pascale R, Toschi A, Ferraro G, Graziano E, Furii F, et al. Treatment duration for Escherichia coli bloodstream infection and outcomes: retrospective single-Centre study. Clin Microbiol Infect. 2018; https://doi.org/10.1016/j.cmi.2018.01.013.
Abernethy JK, Johnson AP, Guy R, Hinton N, Sheridan EA, Hope RJ. Thirty day all-cause mortality in patients with Escherichia coli bacteraemia in England. Clin Microbiol Infect. 2015;21:251 e1–8.
Schwab F, Geffers C, Behnke M, Gastmeier P. ICU mortality following ICU-acquired primary bloodstream infections according to the type of pathogen: a prospective cohort study in 937 Germany ICUs (2006-2015). PLoS One. 2018;13:e0194210.
Nordmann P, Cuzon G, Naas T. The real threat of Klebsiella pneumoniae carbapenemase-producing bacteria. Lancet Infect Dis. 2009;9:228–36.
Munoz-Price LS, Poirel L, Bonomo RA, Schwaber MJ, Daikos GL, Cormican M, et al. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect Dis. 2013;13:785–96.
Liu YC, Cheng DL, Lin CL. Klebsiella pneumoniae liver abscess associated with septic endophthalmitis. Arch Intern Med. 1986;146:1913–6.
Yu WL, Ko WC, Cheng KC, Lee HC, Ke DS, Lee CC, et al. Association between rmpA and magA genes and clinical syndromes caused by Klebsiella pneumoniae in Taiwan. Clin Infect Dis. 2006;42:1351–8.
Shon AS, Bajwa RP, Russo TA. Hypervirulent (hypermucoviscous) Klebsiella pneumoniae: a new and dangerous breed. Virulence. 2013;4:107–18.
Fang CT, Lai SY, Yi WC, Hsueh PR, Liu KL, Chang SC. Klebsiella pneumoniae genotype K1: an emerging pathogen that causes septic ocular or central nervous system complications from pyogenic liver abscess. Clin Infect Dis. 2007;45:284–93.
Cheng NC, Yu YC, Tai HC, Hsueh PR, Chang SC, Lai SY, et al. Recent trend of necrotizing fasciitis in Taiwan: focus on monomicrobial Klebsiella pneumoniae necrotizing fasciitis. Clin Infect Dis. 2012;55:930–9.
Cubero M, Grau I, Tubau F, Pallares R, Dominguez MA, Linares J, et al. Hypervirulent Klebsiella pneumoniae clones causing bacteraemia in adults in a teaching hospital in Barcelona, Spain (2007-2013). Clin Microbiol Infect. 2016;22:154–60.
Togawa A, Toh H, Onozawa K, Yoshimura M, Tokushige C, Shimono N, et al. Influence of the bacterial phenotypes on the clinical manifestations in Klebsiella pneumoniae bacteremia patients: a retrospective cohort study. J Infect Chemother. 2015;21:531–7.
Yu VL, Hansen DS, Ko WC, Sagnimeni A, Klugman KP, von Gottberg A, et al. Virulence characteristics of Klebsiella and clinical manifestations of K. pneumoniae bloodstream infections. Emerg Infect Dis. 2007;13:986–93.
Li W, Sun G, Yu Y, Li N, Chen M, Jin R, et al. Increasing occurrence of antimicrobial-resistant hypervirulent (hypermucoviscous) Klebsiella pneumoniae isolates in China. Clin Infect Dis. 2014;58:225–32.
Yao B, Xiao X, Wang F, Zhou L, Zhang X, Zhang J. Clinical and molecular characteristics of multi-clone carbapenem-resistant hypervirulent (hypermucoviscous) Klebsiella pneumoniae isolates in a tertiary hospital in Beijing, China. Int J Infect Dis. 2015;37:107–12.
Zhang R, Lin D, Chan EW, Gu D, Chen GX, Chen S. Emergence of Carbapenem-resistant serotype K1 Hypervirulent Klebsiella pneumoniae strains in China. Antimicrob Agents Chemother. 2016;60:709–11.
Kang CI, Kim SH, Park WB, Lee KD, Kim HB, Kim EC, et al. Bloodstream infections caused by antibiotic-resistant gram-negative bacilli: risk factors for mortality and impact of inappropriate initial antimicrobial therapy on outcome. Antimicrob Agents Chemother. 2005;49:760–6.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Paterson DL, Ko WC, Von Gottberg A, Mohapatra S, Casellas JM, Goossens H, et al. International prospective study of Klebsiella pneumoniae bacteremia: implications of extended-spectrum beta-lactamase production in nosocomial infections. Ann Intern Med. 2004;140:26–32.
Zarkotou O, Pournaras S, Tselioti P, Dragoumanos V, Pitiriga V, Ranellou K, et al. Predictors of mortality in patients with bloodstream infections caused by KPC-producing Klebsiella pneumoniae and impact of appropriate antimicrobial treatment. Clin Microbiol Infect. 2011;17:1798–803.
Qi Y, Wei Z, Ji S, Du X, Shen P, Yu Y. ST11, the dominant clone of KPC-producing Klebsiella pneumoniae in China. J Antimicrob Chemother. 2011;66:307–12.
MLST databases. Pasteur Institute, Paris. 2017. http://bigsdb.pasteur.fr/perl/bigsdb/bigsdb.pl?db=pubmlst_klebsiella_isolates_public. Accessed 13 May 2017.
Xu A, Zheng B, Xu YC, Huang ZG, Zhong NS, Zhuo C. National epidemiology of carbapenem-resistant and extensively drug-resistant gram-negative bacteria isolated from blood samples in China in 2013. Clin Microbiol Infect. 2016;22(Suppl 1):S1–8.
Mathers AJ, Peirano G, Pitout JD. The role of epidemic resistance plasmids and international high-risk clones in the spread of multidrug-resistant Enterobacteriaceae. Clin Microbiol Rev. 2015;28:565–91.
Zhang Y, Zhao C, Wang Q, Wang X, Chen H, Li H, et al. High prevalence of hypervirulent Klebsiella pneumoniae infection in China: geographic distribution, clinical characteristics and antimicrobial resistance. Antimicrob Agents Chemother. 2016;60:6115–20.
Zhang Y, Zeng J, Liu W, Zhao F, Hu Z, Zhao C, et al. Emergence of a hypervirulent carbapenem-resistant Klebsiella pneumoniae isolate from clinical infections in China. J Inf Secur. 2015;71:553–60.
Catalan-Najera JC, Garza-Ramos U, Barrios-Camacho H. Hypervirulence and hypermucoviscosity: two different but complementary Klebsiella spp. phenotypes? Virulence. 2017;8:1111–23.
Acknowledgements
We thank the entire staff at the Department of Microbiology, The First Affiliated Hospital, College of Medicine, Zhejiang University for their daily contributions to this study. We also thank the team of curators from the Institut Pasteur MLST system (Paris, France) for importing novel alleles and profiles at http://bigsdb.pasteur.fr/klebsiella/klebsiella.html.
Funding
This work was supported by the Natural Science Foundation of Zhejiang Province (no. LQ13H190001), Medical Science and Technology Project of Zhejiang Province (no. 2014KYB096) and National Natural Science Foundation (no. 81301459).
Availability of data and materials
The data that support the findings of this study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
MX and LL designed the study. MX and YF performed data analysis and drafted the manuscript. HK and YF participated in the collection of strains and clinical information. QY and XC performed the phenotypic and genotypic analysis of the clinical isolates. YC and LL reviewed the paper and provided recommendations. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was granted from the Ethics Committees and review board of the First Affiliated Hospital, College of Medicine, Zhejiang University. As this study used secondary data, informed consent was not obtained from patients.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Table S1. Non-susceptible rates of 15 antimicrobial agents for 285 K. pneumoniae isolates from bloodstream infections according to blaKPC and HM phenotype. (DOC 46 kb)
Additional file 2:
Table S2. Factors associated with hypermucoviscosity phenotype in K. pneumoniae isolated from BSIs. (DOCX 16 kb)
Additional file 3:
Figure S1. Characteristics of 54 K. pneumoniae isolates from the non-survival subgroup. (PDF 1596 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Xu, M., Fu, Y., Kong, H. et al. Bloodstream infections caused by Klebsiella pneumoniae: prevalence of blaKPC, virulence factors and their impacts on clinical outcome. BMC Infect Dis 18, 358 (2018). https://doi.org/10.1186/s12879-018-3263-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-018-3263-x