Abstract
Background
The principal goal of HAART is sustained viral load (VL) suppression resulting in immune reconstitution and improved HIV outcomes. We studied the factors associated with 10 years of continuous VL suppression on HAART in the US Military HIV Natural History Study.
Methods
Participants with continuous VL suppression (CS, n = 149) were compared to those who did not have continuous viral load suppression (NCS, n = 127) for ≥10 years on HAART. Factors associated with >10 years of VL suppression were evaluated by multivariate logistic regression. Additionally, association between CS and CD4 reconstitution was analyzed with a mixed effects model.
Results
Compared to NCS participants, a lower proportion of CS participants started HAART in the early HAART era (66 vs 90 %, for years 1996–1999; p < 0.001) and had less antiretroviral use prior to HAART (37 vs 83 %; p < 0.001). At initial HAART, the median CD4 cell count was higher and VL was lower for CS compared to NCS participants (375 cells/uL [256, 499] vs 261 cells/uL [146, 400]; p < 0.001 and 4.4 log10 copies/mL [3.5, 4.9] vs 4.5 log10 copies/mL [3.8, 5.0]; p = 0.048, respectively). New AIDS events were lower during HAART (5 vs 13 %; p = 0.032) and post-HAART CD4 trajectories were greater for the CS compared to NCS group. Factors negatively associated with ≥10 years of VL suppression included log10 VL at first HAART (OR 0.61, 95 % CI 0.4, 0.92; p = 0.020) and antiretroviral use prior to HAART (OR 0.16, 95 % CI 0.06, 0.38; p < .001).
Conclusions
Sustained VL suppression is a key to long-term health in HIV-infected patients, as demonstrated by the lower proportion of AIDS events observed 10 years after HAART initiation. The current use of more potent and well-tolerated regimens may mitigate the negative factors of pre-HAART VL and prior ARV use encountered by treatment initiated in the early HAART era.
Similar content being viewed by others
Background
The primary goal of highly active antiretroviral therapy (HAART) in HIV-infected individuals is sustained viral load (VL) suppression which, in turn, leads to several benefits. Immune recovery is evidenced by CD4 cell gains, a reduction in activated CD8 cells, decreased immune activation, and enhanced responsiveness to vaccines [1–3]. Effective HAART can also mitigate opportunistic infections and the development of acquired immunodeficiency syndrome (AIDS) events [4]. Successful HIV treatment is also associated with a reduction in HIV-associated non-AIDS diseases, including cancer and cardiovascular, renal, and liver disease [5, 6]. Recent studies have demonstrated life expectancy approaching that of HIV-uninfected persons for those with low rates of virologic failure and relatively preserved CD4 counts [7]. In addition, sustained VL suppression enhances the durability of the treatment regimen and prevents the development of antiretroviral resistance [8].
Unfortunately, not all patients are able to maintain VL suppression on HAART. In the US, approximately 40 % of HIV-infected persons have a suppressed VL [9]. Recent cohort studies report VL suppression rates ranging between 65 and 80 % on a variety of HAART regimens, whereas newer HAART regimens have suppression rates approaching 90 % in clinical trials [10–13]. There are many patient-related and treatment-related factors associated with virologic failure early in the course of HAART. Unlike many other chronic conditions, adherence is of major importance as the probability of VL suppression is diminished in patients with <95 % adherence [14]. In addition, suboptimal adherence can lead to increased drug resistance and reduced quality of life and survival [15, 16].
Sustained VL suppression is essential to achieve the best possible treatment outcomes. Because a significant proportion of patients do not achieve this goal, we examined factors associated with ≥10 years of VL suppression in the US Military HIV Natural History Study (NHS). We hypothesize that both patient and treatment-related factors will be associated with long-term VL suppression, and analyses included medication adherence and characteristics of the early HAART era such as prior therapy with single or dual agents. Longitudinal treatment outcomes spanning the entire HAART era were also analyzed to evaluate CD4 trajectories and development of new AIDS events during long-term HAART.
Methods
Study participants
The NHS is a large prospective multicenter cohort of HIV-infected individuals. The study population is comprised of active duty military, retired military, and their beneficiaries from the Army, Navy/Marines, and Air Force. Participants are evaluated approximately every 6–12 months at military treatment facilities throughout the United States. Data between study visits are systematically collected, including demographic characteristics, laboratory data, information on medication use, and reports of clinical events with medical record confirmation. The NHS has been enrolling since 1986 and consists of more than 5800 participants. Self-reported adherence (SRA) data has been systematically collected since 2006. All participants provided informed written consent and this study protocol was approved by the Uniformed Services University of the Health Sciences central IRB.
Inclusion criteria
NHS participants initiating HAART on or after January 1, 1996 with ≥10 years of continuous treatment were included. Participants were required to have ≥1 VL and CD4 count determinations per year during follow-up, with data collected through December 31, 2013. Treatment interruptions <6 months in duration were permitted. HAART was defined as two or more nucleoside reverse transcriptase inhibitors (NRTIs) in combination with at least one protease inhibitor (PI), one nonnucleoside reverse transcriptase inhibitor (NNRTI), or one integrase strand transfer inhibitor (INSTI). Regimens comprised of one NRTI with at least one PI and one NNRTI or an abacavir or tenofovir containing regimen of 3 or more NRTIs in the absence of both PIs and NNRTIs were also considered HAART. Non-HAART antiretroviral (ARV) use was defined as treatment not meeting HAART criteria above and typically consisted of mono- or dual-therapy prior to the availability of HAART. The total number of HAART regimens, defined as changes to any or all ARV components, were also captured during the study period.
VL suppression was defined as achieving a VL ≤400 copies/mL within the first year of HAART. Virologic failure was defined as not achieving suppression or two consecutive VL determinations ≥400 copies/mL after initial suppression. The threshold of 400 copies/mL was chosen in order to compare outcomes during the entire HAART era given the differences in VL assay detection limits over time. Participants were divided into two separate groups for analysis. The continuous VL suppression (CS) group was defined as those with all VL values ≤400 copies/mL for ≥10 years. The non-continuous VL suppression (NCS) group was defined as having 1 or more episodes of virologic failure during the study period. Since more sensitive VL assays with limits of detection <50 copies/mL became clinically available during the later HAART era, we also analyzed the proportion with VL suppression <50 copies/mL in both groups. CD4 count trajectories and development of AIDS events after HAART initiation were also analyzed. SRA data was obtained via voluntary participant questionnaire with adherence defined by the overall percentage of HAART doses taken in the prior 6 months.
Statistical analysis
Cohort demographics and other characteristics associated with HIV were described separately for participants in the CS and NCS groups. For continuous variables, t-tests were used for normally distributed variables or by Wilcoxon tests when appropriate. For categorical variables, chi-squared tests or Fisher’s exact tests were used. From the clinically relevant baseline characteristics, logistic regression was used to analyze the impact of factors on continuous VL suppression during 10 years of HAART. SRA data was calculated as the average and minimum percent adherence and evaluated by t-tests. Adherence was also evaluated as a categorical variable (report of 100 % adherence yes/no) and analyzed by chi-squared test.
Mixed effects models were used to analyze the factors associated with longitudinal CD4 cell reconstitution. The square root of the CD4 count was used to normalize the data. An interaction term between the years from HAART initiation to VL suppression was used to quantify the difference in the rate of CD4 cell increase between groups. From this data subset, a locally-weighted scatter plot smoothing (LOWESS) was created to visualize trends in CD4 cell reconstitution over 10 years on HAART.
Results
A total of 276 participants met the inclusion criteria (Table 1). Participants were predominately male with similar proportions of Caucasians and African Americans in each group. The median age at HIV diagnosis was 32 and 30 years in the CS and NCS groups, respectively (p = 0.065). A greater proportion of NCS participants (90 %) were treated in the early HAART era (1996–1999) compared with the CS group (66 %; p < 0.001). The median CD4 count at first HAART was higher in the CS compared with the NCS group (375 vs 261 cells/uL; p < 0.001) and the median VL at first HAART was 4.4 log10 copies/mL and 4.5 log10 copies/mL, respectively (p = 0.048). First HAART regimens differed among the groups (p < 0.001), with NCS having a higher proportion of unboosted PI use compared with CS participants (76 % vs 51 %). AIDS outcomes prior to first HAART were similar for CS (8 %) and NCS participants (12 %; p = 0.399). During longitudinal follow-up, groups had a median of 1 treatment interruption [0,1], with a higher proportion of any treatment interruption observed in NCS (57 %) compared to CS (17 %) participants (p < 0.001). NCS participants also had a greater median number of HAART regimens (7 [4, 9] vs 3 [2, 5]; p < .001) and a higher proportion of new AIDS events by 10 years of HAART (13 vs 5 %; p = 0.032) compared with CS participants. In a subgroup analysis of participants with VL data using assays with a limit of detection <50 copies/mL during HAART, the proportion with a suppressed VL <50 copies/mL was higher in the CS group (2399 of 2550 VL values, 94 %) compared to the NCS group (1545 of 2221, 70 %; p < 0.001).
Self-reported adherence
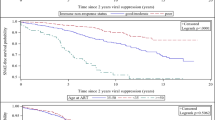
SRA was high in both groups (Fig. 1), with an average SRA of 99 % in the CS group and 98 % in the NCS group (p = 0.341). A similar proportion of participants reported always having 100 % adherence in the CS (26 %) and NCS (24 %; p = 0.727) groups.
Factors associated with VL suppression
Analysis of demographic factors showed no association between age at first HAART and VL suppression for ≥10 years (Odds ratio [OR] 1.0 per 10 years, 95 % confidence interval [CI] 0.68, 1.47; p = 0.984, Table 2). The use of non-HAART ARVs prior to first HAART (OR 0.16, 95 % CI 0.06, 0.38; p < 0.001) and log10 VL at first HAART (OR 0.61, 95 % CI 0.4, 0.92; p = 0.020) were both negatively associated with ≥10 years of VL suppression. A negative trend for long-term VL suppression was observed for African Americans compared with Caucasians, but this association was marginal (OR 0.53, 95 % CI 0.25, 1.07; p = 0.079). No association was observed for the time from HIV diagnosis to first HAART, CD4 count at first HAART, or type of first HAART regimen. For factors after initiation of first HAART, the total number of HAART regimens used during the study period was negatively associated with long-term VL suppression (OR 0.71, 95 % CI 0.6, 0.81; p < 0.001) due to virologic failures, while no association was observed for SRA (OR 0.82, 95 % CI 0.39, 1.73 for those always reporting 100 % adherence; p = 0.607).
CD4 cell reconstitution on HAART
Longitudinal CD4 cell trends during the first 10 years of HAART showed that the CS group had a greater upward trajectory of CD4 cell gains compared with the NCS group (Fig. 2). Analysis of factors associated with the change in CD4 count from first HAART initiation to 10 years after beginning HAART showed a negative adjusted difference in square root of CD4 (√CD4) for ARV use prior to first HAART (−1.73, 95 % CI−3.44,−0.02; p = 0.047), longer time from HIV diagnosis to first HAART (−0.02, 95 % CI−0.03, 0; p = 0.025), and higher log10 VL at first HAART (−1.7, 95 % CI−2.36,−1.03; p < 0.001; Table 3). Continuous VL suppression was associated with greater adjusted difference in √CD4 at baseline (2.3, 95 % CI 0.8, 3.81; p = 0.003) and marginal rate of increase in √CD4 during follow-up (0.13 95 % CI 0, 0.26; p = 0.049), whereas no association was observed for demographic factors and SRA.
Discussion
Over the past 20 years, the availability of HAART has effectively transformed HIV from a uniformly fatal condition to that of a chronic disease. Contemporary treatment is associated with improved life expectancy, with one study finding no elevated mortality risk in patients with CD4 counts above 500 cells/uL who maintained VL suppression [17]. Since long-term VL suppression is required for optimal HIV disease outcomes, we aimed to determine the factors associated with sustained virologic control on HAART in a large military cohort.
The inability of many patients to maintain VL suppression can be explained in part by the era in which participants began HAART. A previous study in our cohort reported VL suppression during the early HAART era (1996–2000) compared to the late HAART era (2000–2007), with 58 and 85 % VL suppression at 5 years for those treated in the early versus late HAART era, respectively [10]. Similarly, the Antiretroviral Therapy (ART) Cohort Collaboration analyzed treatment naïve participants who began HAART from 1995 to 2003 and observed an increase in VL suppression in later years, with 58 and 83 % for those initiating HAART between 1995–1996 and 2002–2003, respectively [18]. Our current study with a longer duration of follow-up after HAART initiation (≥10 years) affirms that treatment during the early HAART era is a risk for non-continuous VL suppression.
The use of ARVs prior to HAART, typically mono- or dual-therapy, is an important characteristic of the early HAART era. We observed that ARV use prior to HAART negatively impacted both the ability to achieve long-term VL suppression and the magnitude of CD4 cell gains during HAART. Although non-HAART ARV use was likely a major reason for suboptimal treatment outcomes, other features of the early HAART era other factors likely contributed to the lower rate of treatment success during that period. For example, the early HAART era is also characterized by less potent, unboosted PI regimens, which were more commonly used for first HAART in the NCS group, and other HAART regimens associated with greater adverse effects and reduced tolerability compared to more contemporary regimens [19, 20]. In contrast to the beginnings of HAART, continuous VL suppression is more attainable with newer HAART regimens. For example, recent studies of integrase inhibitor-based regimens have demonstrated VL suppression in approximately 87 % of treatment naïve patients [21, 22]. However, longer follow-up time is necessary to determine the long-term durability of newer regimens.
Advanced HIV disease, as evidenced by low CD4 cell count and AIDS events, is associated with lower rates of VL suppression on HAART [19, 23, 24]. In our current study, we observed that new AIDS events occurring during HAART were more common in those with non-continuous VL suppression despite long-term treatment. We previously found that high cumulative VL on HAART was associated with a greater than 2-fold increase in AIDS events and impacted overall CD4 gains [11]. In our current study, the trajectory of CD4 cells gains over a 10-year period was much higher in those with continuous VL suppression. This is consistent with other studies showing maximal CD4 reconstitution occurs with sustained VL suppression [25, 26]. Thus, the long-term maintenance of VL suppression is of key importance for achieving optimal immune recovery and for the reduction of AIDS events.
Suboptimal treatment outcomes involve both clinical and non-clinical factors. For example, access and engagement in care have been identified as key areas along the HIV care continuum [9]. Some of these barriers are minimized or removed in the NHS cohort as military members and beneficiaries have free access to care and prescription medications. These benefits were demonstrated in a previous NHS study demonstrating a high proportion of VL suppression (81 %) at 1 year [10]. Recent studies in other healthcare settings report slightly lower VL suppression ranging from 70 to 78 %, which may be contributed by access to care or patient characteristics such as injection drug use or socioeconomic factors not typically present in the military population [27–29].
Discordant HIV treatment outcomes have been observed in different racial/ethnic groups. A study of non-white participants found a VL suppression rate of 31 % compared to 54 % in white participants at 7–14 months in an urban setting [23]. Non-white ethnicity was also linked to higher number of missed appointments, injection drug use, and lower CD4 count at HAART initiation [23]. A previous study in our cohort showed that African Americans had lower odds of VL suppression at 6 and 12 months post-compared to participants of European ancestry, although time to virologic failure was no different once suppression was achieved [30]. Similarly, a negative trend for ≥10 years of VL suppression was also observed in African Americans in our current study, however only a small subset of the NHS cohort was included and additional studies are needed to evaluate potential differences according to race/ethnicity.
Adherence is a cornerstone of successful HIV treatment. We found no difference in those reporting 100 % SRA in CS and NCS participants and the overall adherence was 98 % or greater in both groups. This high degree of SRA may be somewhat explained by free access to care and medications, or possibly by other characteristics of our population such as level of education, socioeconomic status, or very low rate of injection drug use [31]. Other explanations may include potential disadvantages of SRA compared with other methods to assess adherence. For example, SRA is subject to recall and social desirability bias and patients tend to report a 10–20 % over estimation on adherence when directly compared to data obtained from electronic drug monitoring [32]. Methods such as medication event monitoring system (MEMS) track caps can be more accurate as they report exact date and times of all bottles opening. One study found that high MEMS adherence rates, but not high SRA, was associated with VL suppression [33]. However, MEMS has potential drawbacks of cost and tracking does not always directly correlate with pill ingestion [34].
The strengths of this study include long-term follow-up spanning the entire HAART era in a diverse cohort of patients with free access to care and medications. Limitations included the inability to assess adherence in the early HAART era since SRA data was not systematically captured until 2006. The high level of SRA in our study likely limited the ability to detect an association between adherence and VL suppression, since >95 % adherence is associated with optimal and sustained VL suppression [14]. However, equally high SRA in both groups allowed for the evaluation of other factors associated with ≥10 years of VL suppression in our cohort. Other potential study limitations include the retrospective study design and non-randomized treatment decisions. Differing limits of detection of VL assays used during the 18-year study period, particularly in the early HAART era, may have limited the interpretation of factors associated with continuous viral load suppression. Our results may not be generalizable to women, given the high proportion of males in our cohort, or to populations with other characteristics such as injection drug use.
Conclusion
Sustained VL suppression is essential to reduce long-term morbidity in HIV-infected patients, as demonstrated by the lower proportion of AIDS events and improved CD4 cell reconstitution after ≥10 years of continuous VL suppression. We identified factors negatively associated with ≥10 years of VL suppression, including high VL at first HAART, prior ARV use, HIV diagnosis in the pre-HAART era, and number of HAART regimens used. It is likely that treatment in the current era, characterized by regimens that are more potent, more convenient, and less toxic, may promote higher success rates and more durable VL suppression in the future.
Abbreviations
AIDS, acquired immune deficiency syndrome; ARV, antiretroviral therapy; CS, continuous viral load suppression; HAART, highly active antiretroviral therapy; HIV, human immunodeficiency virus; INSTI, integrase strand transfer inhibitor; LOWESS, locally-weighted scatter plot smoothing; NCS, non-continuous viral load suppression; NHS, natural history study; NNRTI, non-nucleoside reverse transcriptase inhibitor; NRTI, nucleoside reverse transcriptase inhibitors; PI, protease inhibitor; SRA, self-reported adherence; VL, viral load
References
Al-Harthia L, Siegela J, Spritzlerb J, Pottagec J, Agnolic M, Landaya A. Maximum suppression of HIV replication leads to the restoration of HIV-specific responses in early HIV disease. AIDS. 2000;14:761–70.
Hunt PW, Brenchley J, Sinclair E, McCune JM, Roland M, Page-Shafer K, et al. Relationship between T cell activation and CD4+ T cell count in HIV-seropositive individuals with undetectable plasma HIV RNA levels in the absence of therapy. J Infect Dis. 2008;197:126–33.
Landrum ML, Huppler Hullsiek K, Ganesan A, Weintrob AC, Crum-Cianflone NF, Barthel RV, et al. Hepatitis B vaccine responses in a large U.S. Military cohort of HIV-infected individuals: another benefit of HAART in those with preserved CD4 count. Vaccine. 2009;27:4731–8.
Kaplan JE, Hanson D, Dworkin MS, Frederick T, Bertolli J, Lindegren ML, et al. Epidemiology of human immunodeficiency virus-associated opportunistic infections in the united states in the era of highly active antiretroviral therapy. Clin Infect Dis. 2000;30:S5–S14.
Freiberg MS, Chang CH, Kuller LH, Skanderson M, Lowy E, Kraemer KL, et al. HIV infection and the risk of acute myocardial infarction. JAMA Intern Med. 2013;173:614–22.
The Strategies for Management of Antiretroviral Therapy (SMART) Study Group. CD4+ count-guided interruption of antiretroviral treatment. N Engl J Med. 2006;355:2283–96.
Nakagawa F, Lodwick RK, Smith CJ, Smith R, Cambiano V, Lundgren JD, et al. Projected life expectancy of people with HIV according to timing of diagnosis. AIDS. 2012;26:335–43.
Richman DD, Morton SC, Wrin T, Hellmann N, Berry S, Shapiro MF, et al. The prevalence of antiretroviral drug resistance in the united states. AIDS. 2004;18:1393–401.
Gray KM, Cohen SM, Hu X, Li J, Mermin J, Hall HI. Jurisdiction level differences in HIV diagnosis, retention in care, and viral suppression in the united states. JAIDS. 2014;65:129–32.
Marconi VC, Grandits GA, Weintrob AC, Chun H, Landrum ML, Ganesan A, et al. Outcomes of highly active antiretroviral therapy in the context of universal access to healthcare: the US military HIV natural history study. AIDS Res Ther. 2010;7:14.
Marconi VC, Grandits G, Okulicz JF, Wortmann G, Ganesan A, Crum-Cianflone N, et al. Cummulative viral load and virologic decay patterns after antiretroviral therapy in HIV-infected subjects influence CD4 recovery and AIDS. PLoS One. 2011;6, e17956.
Guest JL, Weintrob AC, Rimland D, Rentsch C, Bradley WP, Agan BK, et al. A comparison of HAART outcomes between the US military HIV natural history study (NHS) and HIV Atlanta veterans affairs cohort study (HAVACS). PLoS One. 2013;8, e62273.
Molina JM, Cahn P, Grinstzejn B, Lazzarin A, Mills A, Saag M, et al. Rilpivirine versus egavirenz with tenofovir and emtricitabine in treatment-naïve adults infected with HIV-1 (ECHO): a phase 3 randomised double-blind active-controlled trial. Lancet. 2011;378:238–46.
Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133:21–30.
Chesney MA. The elusive gold standard. Future perspectives for HIV adherence assessment and intervention. J Acquir Immune Defic Syndr. 2006;43:S149–55.
Mannheimer SB, Morse E, Matts JP, Andrews L, Child C, Schmetter B, et al. Sustained benefit from a long-term antiretroviral adherence intervention. Results of a large randomized clinical trial. J Acquir Immune Defic Syndr. 2006;43:S41–7.
Rodger AJ, Lodwick R, Schechter M, Deeks S, Amin J, Gilson R, et al. Mortality in well controlled HIV in the continous antiretroviral therapy arms of SMART and ESPIRIT trials compared with the general population. AIDS. 2013;27:973–9.
The Antiretroviral Therapy (ART) Cohort Collaboration. HIV treatment response and prognosis in Europe and north America in the first decade of highly active antiretroviral therapy: a collaborative analysis. Lancet. 2006;368:451–8.
D’Arminio Monforte A, Testa L, Adorni F, Chiesa E, Bini T, Moscatelli GC, et al. Clinical outcome and predictors factors of failure of highly active antiretroviral therapy in antiretroviral experienced patients in advanced stages of HIV-1 infection. AIDS. 1998;12:1631–7.
Mocroft A, Youle M, Moore A, Sabin CA, Madge S, Lepri AC, et al. Reasons for modification and discontinuation of antiretrovirals: results from a single treatment centre. AIDS. 2001;15:185–94.
Van Lunzen J, Maggiolo F, Arribas JR, Rakhmanova A, Yeni P, Young B, et al. Once daily dolutegravir (S/GSK1349572) in combination therapy in antiretroviral-naive adults with HIV: planned interim 48 week results from SPRING-1, a dose-ranging, randomised, phase 2b trial. Lancet Infect Dis. 2012;12:111–8.
Sax PE, Dejesus E, Mills A, Zolopa A, Cohen C, Wohl D, et al. Co-formulated elvitegravir, cobicistat, emtricitabine, and tenofovir versus co-formulated efavirenz, emtricitabine, and tenofovir for initial treatment of HIV-1 infection: a randomised, double-blind, phase 3 trial, analysis of results after 48 weeks. Lancet. 2012;379:2439–48.
Lucas GM, Chaisson RE, Moore RD. Highly active antiretroviral therapy in a large urban clinic: risk factors for virologic failure and adverse drug reactions. Ann Intern Med. 1999;131:81–7.
Grabar S, Pradier C, Le Corfec E, Lancar R, Allavena C, Bentata M, et al. Factors associated with clinical and virological failure in patients receiving a triple therapy including a protease inhibitor. AIDS. 2000;14:141–9.
Kaufmann GR, Bloch M, Zaunders JJ, Smith D, Cooper DA. Long-term immunlogical response in HIV-1 infected subjects receiving potent antiretroviral therapy. AIDS. 2000;14:959–69.
Wood E, Yip B, Hogg RS, Sherlock CH, Jahnke N, Harrigan NP, et al. Full supression of viral loads is needed to achieve an optimal CD4 cell count among patients on triple drug antiretroviral therapy. AIDS. 2000;14:1955–60.
Althoff KN, Rebeiro P, Brooks JT, Buchacz K, Gebo K, Martin J, et al. Disparities in the quality of HIV care when using US Department of Health and Human Service Indicators. Clin Infect Dis. 2014; doi:10.1093/cid/ciu044.
Willis S, Castel AD, Ahmed T, Olejemeh C, Frison L, Kharfen M. Linkage, engagement, and viral suppression rates among HIV-infected persons receiving care at medical care at medical case management in Washington, DC. JAIDS. 2013;64:S33–41.
Eberhart MG, Yehia BR, Hillier A, Voytek CD, Blank MB, Frank I, et al. Behind the cascade: analyzing spatial patterns along HIV care continuum. JAIDS. 2013;64:S42–51.
Weintrob AC, Grandits GA, Agan BK, Ganesan A, Landrum ML, Crum-Cianflone NF, et al. Virologic response differences between African Americans and European Americans initating highly active antiretroviral therapy with equal access to care. JAIDS. 2009;52:574–80.
Brodine SK, Starkey MJ, Shaffer RA, Ito SI, Tasker SA, Barile AJ, et al. Diverse HIV-1 subtypes and clinical, laboratory and behavioral factors in a recently infected US military cohort. AIDS. 2003;17:2521–7.
Simoni JM, Kurth AE, Pearson CR, Pantalone DW, Merrill JO, Frick PA. Self-report measures of antiretroviral therapy adherence: a review with recommendations for HIV research and clinical management. AIDS Behav. 2006;10:227–45.
Arnsten JH, Demas PA, Farzadegan H, Grant RW, Gourevitch MN, Chang CJ, et al. Antiretroviral therapy adherence and viral suppression in HIV-infected drug users: comparison of self-rpeort and electronic monitoring. Clin Infect Dis. 2001;33:1417–23.
Martin S, Elliott-Desorbo DK, Calabrese S, Wolters PL, Roby G, Brennan T, et al. A comparison of adherence assessment methods utilized in the united states: perspectives of researchers, HIV-infected children, and their caregivers. AIDS Patient Care STDS. 2009;23:593–603.
Acknowledgements
The content of this publication is the sole responsibility of the authors and does not necessarily reflect the views or policies of the NIH or the Department of Health and Human Services, the DoD or the Departments of the Army, Navy or Air Force. Mention of trade names, commercial products, or organizations does not imply endorsement by the U.S. Government.
Funding
Support for this work (IDCRP-000-03) was provided by the Infectious Disease Clinical Research Program (IDCRP), a Department of Defense (DoD) program executed through the Uniformed Services University of the Health Sciences. This project has been funded in whole, or in part, with federal funds from the National Institute of Allergy and Infectious Diseases, National Institutes of Health (NIH), under Inter-Agency Agreement Y1-AI-5072.
Availability of data and materials
The authors confirm that all data underlying the findings are fully available without restriction. Data for this study is located at and can be requested from Infectious Disease Clinical Research Program (IDCRP), headquartered at the Uniformed Services University (USU), Department of Preventive Medicine and Biostatistics. Address: 11300 Rockville Pike, Suite 600, Rockville, MD 20852; Email: idcrp@idcrp.org.
Authors’ contributions
All authors participated in the design of the study and manuscript preparation. OM and SHW performed the statistical analysis. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent to publish
Not applicable.
Ethics approval and consent to participate
This study (IDCRP 000–03) was approved by the Uniformed Services University of the Health Sciences central IRB and all participants provided informed written consent.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Bello, K.J., Mesner, O., O’Bryan, T.A. et al. Factors associated with 10 years of continuous viral load suppression on HAART. BMC Infect Dis 16, 351 (2016). https://doi.org/10.1186/s12879-016-1677-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-016-1677-x