Abstract
Background
The recent emergence of azithromycin-resistant (AZM-R) N. gonorrhoeae isolates that have coevolved decreased susceptibility to extended-spectrum cephalosporins has caused great concern. Here we investigated the prevalence of decreased susceptibility to ceftriaxone (CROD) in AZM-R isolates and genetically characterized AZM-R isolates in Guangzhou, China from 2009 to 2013.
Methods
The minimum inhibitory concentration (MIC) of AZM and ceftriaxone was determined using an agar-dilution method. All AZM-R isolates were screened for mutations in 23S rRNA, mtrR and penA genes and genotyped using N. gonorrhoeae multi-antigen sequence typing (NG-MAST).
Results
Of the 485 identified N. gonorrhoeae isolates, 445 (91.8 %) were isolated from male urethritis subjects, and 77 (15.9 %) were AZM-R (MIC ≥ 1 mg/L), including 33 (6.8 %) with AZM low-level resistant (AZM-LLR, MIC = 1 mg/L) and 44 (9.1 %) with AZM middle-level resistant (AZM-MLR, MIC ≥ 2 mg/L). Significantly more CROD (MIC ≥ 0.125 mg/L) showed in AZM-MLR isolates (43.2 %, 19/44) as compared with that in AZM-LLR isolates (18.2 %, 6/33) (p < 0.05). For the 23S rRNA, mtrR, penA or combined 23S rRNA/MtrR/penA mutations, no significant difference was found between AZM-LLR isolates and AZM-MLR isolates (P > 0.05); similar results were detected between combined AZM-LLR/CROD isolates and combined AZM-MLR/CROD isolates (P > 0.05). No mutation A2059G or AZM high-level resistant (AZM-HLR, MIC ≥ 256 mg/L) isolate was detected. Among 77 AZM-R isolates, 67 sequence types (STs) were identified by NG-MAST, of which 30 were novel. Most STs were represented by a single isolate.
Conclusions
The AZM-R together CROD isolates are now present in Guangzhou, China, which deserve continuous surveillance and the mechanism of concurrent resistance needs further study.
Similar content being viewed by others
Background
The global spread of multidrug-resistant Neisseria gonorrhoeae (N. gonorrhoeae) is a growing public health threat. Worryingly, clinical treatment failures with the extended-spectrum cephalosporins (ESCs) [1], the last remaining options for empirical first-line monotherapy, have recently been reported. Accordingly, dual antimicrobial therapies have been introduced in several countries [2, 3], including China [4]. These consist of ceftriaxone (250–500 mg intramuscularly) or cefixime (400 mg orally, if ceftriaxone is not an option) together with azithromycin (AZM, 1–2 g orally) for treatment of uncomplicated gonorrhea. AZM was recommended for patients with gonorrhea or coinfection with Chlamydia trachomatis in China around the year 2000 [5], and since then has been broadly used because of its wide availability and ease of administration. In China, AZM-resistant (AZM-R) N. gonorrhoeae were first identified during 2001–2003 [6], and the first AZM-R isolates were identified in Guangzhou in 2009 [7]. Treatment failures with 2 g of AZM and high-level AZM resistant N. gonorrhoeae isolates with a minimum inhibitory concentration (MIC) ≥ 256 mg/L have been verified in several countries [8, 9]. Recently, a surveillance of antimicrobial resistance in gonococci from Canada resulted in two high-level AZM-R isolates (MIC ≥ 2048 mg/L), which may be due to mutation A2143G (N. gonorrhoeae numbering) in the four copies of the 23S rRNA gene [9].
Mutations at various genes such as 23S rRNA, mtrR and penA (encoding penicillin-binding protein 2, PBP2), have been identified associating with chromosomally mediated resistance to AZM [10, 11] and ESCs [12] in N. gonorrhoeae. Globally, AZM-R together decreased susceptibility to ESCs in N. gonorrhoeae has only rarely been reported [9, 13]. In this study, we investigated the prevalence of decreased susceptibility to ceftriaxone (CROD) in AZM-R N. gonorrhoeae isolates, and the molecular characteristics of AZM-R N. gonorrhoeae isolates from January 2009 to November 2013 in Guangzhou, China.
Methods
Gonococcal isolates and susceptibility testing
Clinical N. gonorrhoeae isolates were consecutively collected from urethral or cervical specimen of one per patient with gonorrhea attending sexually transmitted infection (STI) clinics in Guangzhou, China between January 2009 and November 2013. The demographic and clinical information of patients such as gender, age, and symptoms was collected by completing a questionnaire. Each isolate was cultured, verified, and preserved as described [14]. MIC for AZM and ceftriaxone were determined by the agar dilution method, according to recommendations from the WHO [15]. Antimicrobial susceptibility for AZM was interpreted using the European Committee on Antimicrobial Susceptibility Testing (EUCAST) guidelines (http://www.eucast.org/), and ceftriaxone susceptibility was interpreted according to criteria defined by WHO in 2012 [15]. Briefly, isolates with MIC ≥ 1.0 mg/L for AZM were classified as resistant, and isolates with MIC ≥ 0.125 mg/L for ceftriaxone were classified as having decreased susceptibility. N. gonorrhoeae ATCC 49226 and strains G, L, and P of the 2008 WHO N. gonorrhoeae reference strain panel were used as quality control strains. To compare with a previous report [5] and better analyze the results, AZM-R N. gonorrhoeae isolates (MIC ≥ 1.0 mg/L) were divided into AZM low-level resistant (AZM-LLR) N. gonorrhoeae isolates (MIC = 1.0 mg/L), AZM middle-level resistant (AZM-MLR) N. gonorrhoeae isolates (MIC ≥ 2.0 mg/L), and AZM high-level resistant (AZM-HLR) N. gonorrhoeae isolates (MIC ≥ 256 mg/L) in this study based on the previous studies [9, 10].
Sequence-based molecular epidemiologic studies
Bacterial genome DNA from each identified AZM-R isolate was extracted using the TIANamp Bacterial DNA kit (TIANGEN, Beijing, China). As previously described, mutations in the four alleles of the 23S rRNA [16], mtrR and penA genes [12], and polymorphisms in porB and tbpB [17] were amplified by PCR. The PCR products were purified and sequenced by Shenggong Co., Ltd. (Shanghai, China). DNA sequences were aligned using BLAST and GenBank programs (http://www.ncbi.nlm.nih.gov) to identify mutations in the 23S rRNA gene. DNA sequences of mtrR and penA genes were translated into deduced amino acid sequences, which were then aligned with their respective prototypes in N. gonorrhoeae using Proteomics and Sequence Tools (http://ca.expasy.org/). N. gonorrhoeae isolates were typed using the N. gonorrhoeae multi-antigen sequence typing (NG-MAST) method [17]. NG-MAST allele numbers of porB and tbpB and STs were obtained using a publicly accessible database on the NG-MAST website (www.ng-mast.net). A phylogenetic tree was created using ClustalX software (version 1.83; http://www.clustal.org/download/1.X/ftp-igbmc.u-strasbg.fr/pub/ClustalX. html) and Mega software (version 6.0.5; http://www.megasoftware.net/mega.php) based on the more variable segments of porB (490 bp) and tbpB (390 bp) as analyzed by NG-MAST.
Statistical analysis
Statistical significance was assessed using SPSS 13.0 (SPSS Inc, Chicago, IL). Chi-square tests were used for statistical analyses. A P-value < 0.05 was considered to be significant.
Ethics approval
The study protocol was approved by the Medical Ethics Committee at the Institute of Dermatology, the Chinese Academy of Medical Sciences & Peking Union Medical College and the National Center for Sexually Transmitted Disease Control, Nanjing, China (approval number 2011-KY-003). Written informed consent was obtained from all participating subjects.
Results
Antimicrobial susceptibility testing
A total of 485 N. gonorrhoeae isolates were identified in Guangzhou from 2009 to 2013 (Table 1). Of these, the mean age of the patients was 31.6 years (range from 17 to 69 years), 91.8 % (445/485) isolates were isolated from male patients with urethritis. Among all the isolates, 15.9 % (77/485) showed AZM-R, including 6.8 % (33/485) AZM-LLR and 9.1 % (44/485) AZM-MLR. The proportion of AZM-LLR isolates decreased from 14.0 % (24/171) in 2009–2010 to 2.9 % (9/314) in 2011–2013 (p < 0.05), whereas AZM-MLR isolates increased from 4.7 % (8/171) in 2009–2010 to 11.5 % (36/314) in 2011–2013 (p < 0.05). In the 2011–2013 study period, seven isolates with MIC > 8 mg/L appeared for the first time and accounted for 2.2 % (7/314) of the examined isolates (Fig. 1). The percentage of CROD isolates was 22.3 % (108/485) in all identified N. gonorrhoeae isolates, 18.2 % (6/33) in AZM-LLR isolates, and 43.2 % (19/44) in AZM-MLR isolates which was a significant increase compared with the percentage of all identified N. gonorrhoeae isolates or AZM-LLR isolates (both p < 0.05, Table 2).
23S rRNA, mtrR and penA mutations in AZM-R N. gonorrhoeae isolates
Thirty-two of the 33 AZM-LLR isolates (97.0 %) contained the wild-type sequence in domain V of all four 23S rRNA alleles, except one isolate (3.0 %, 1/33) that contained mutation C2611T (Escherichia coli numbering; also known as C2599T, N. gonorrhoeae numbering) in a single allele (Table 2 and Additional file 1: Table S1, S2). Thirty-eight of the 44 AZM-MLR isolates (86.4 %) contained the wild-type sequence in all four 23S rRNA alleles, whereas only one isolate (2.2 %, 1/44; its AZM MIC = 2 mg/L) contained mutation C2611T in a single allele and five isolates (11.4 %, 5/44; their AZM MICs = 4, 8, 8, 8 and 64 mg/L, respectively) contained mutation C2611T in all four alleles. All seven AZM-R isolates that contained the mutation C2611T showed reduced susceptibility to ceftriaxone (MIC ≥ 0.125 mg/L).
The presence of a single nucleotide deletion (A) in the 13 bp inverted repeat of the mtrR promoter did not different between AZM-LLR (87.9 %, 29/33) and AZM-MLR (95.5 %, 42/44) isolates (P > 0.05) (Table 2 and Additional file 1: Table S1, S2). A wild type (WT) in the coding region of mtrR only displayed in combined AZM-LLR/susceptibility to ceftriaxone (CROS) (n = 2) and combined AZM-MLR/CROS (n = 2), but not in combined AZM-LLR/CROD or combined AZM-MLR/CROD isolates. The combined mutations (double or triple) such as A39T/F62L, A40D/T86A, T86A/H105Y, A40D/T86A/H105Y or D79N/T86A/H105Y were only present in AZM-MLR isolates (Table 2).
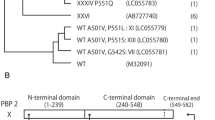
All the AZM-R isolates (n = 77) in this study had an Asp-346 insertion and contained F504L, A510V and A516G mutations in PBP2 (data shown in Additional file 1: Table S1-S3). Thirteen mutation patterns in this study included three new mutation patterns (New 1: A501V, F504L A501V, A516G, H541N, P552V, I556V, I566V; New 2: F504L, A501V, A516G, Y554H; New 3: A501V, F504L, A510V, A516G, H541N, I566V) were shown in Table 2. The patterns V (18.2 %), XVIII (15.2 %) and XXI (21.2 %) were the most prevalent in AZM-LLR isolates, similar to the most prevalent patterns (V, 18.2 %; XVIII, 29.4 %; XXI, 18.2 %) in AZM-MLR isolates. No different mutation patterns were found between AZM-LLR isolates and AZM-MLR isolates or between combined AZM-LLR/CROD isolates and combined AZM-MLR/CROD isolates (both P > 0.05).
In addition, combined 23S rRNA/mtrR/penA mutation patterns had no significant association with AZM-MLR isolates or combined AZM-MLR/CROD isolates (Table 2).
NG-MAST and phylogenetic analysis based on porB and tbpB DNA sequences
A total of 67 STs (29 STs in AZM-LLR isolates and 38 STs in AZM-MLR isolates) were identified by NG-MAST among the 77 AZM-R isolates, of which 30 STs (15 STs in AZM-LLR isolates and 15 STs in AZM-MLR isolates) were first identified by the current study (Table 3 and Additional file 1: Table S1, S2 and S3). The most prevalent STs were ST1766 (n = 3), ST1866 (n = 2), and ST421 (n = 2) in AZM-LLR isolates and ST1766 (n = 3), ST6987 (n = 2), ST1055 (n = 2), ST304 (n = 2), and a new ST consisting of porB allele 822 and tbpB allele 156 (n = 2) in AZM-MLR isolates. Of the remaining STs, most were represented by a single isolate. The phylogenetic tree, built from DNA sequences of por (490 bp) and tbpB (390 bp), displayed the significant diversity of strains with 29 different STs in AZM-LLR isolates (Additional file 2: Figure S1), as well as 38 different STs in AZM-MLR isolates (Additional file 3: Figure S2).
Discussion
The present study combines antimicrobial susceptibility determinations with molecular-based analysis of AZM-R in N. gonorrhoeae isolated from 2009 to 2013 in Guangzhou, China. As observed in other countries worldwide [9, 13, 18], an upward shift in MIC by year and a high percentage of AZM-R were identified in this study, which was also in line with a previous report in two Chinese cities, Nanjing and Chongqing, between 2008 and 2009 [5]. The WHO recommends discontinuation of the empirical use of an antibiotic once 5 % of locally acquired gonococcal isolates are resistant [19]. Accordingly, AZM has not been recommended as a monotherapy for gonococcal urethritis or cervicitis in China, as well as in many other countries worldwide. To improve treatment efficacy and to delay the further selection of cephalosporin-resistant N. gonorrhoeae, most current guidelines now recommend ESCs and AZM in combination as the first-line treatment for gonorrhea [2–4, 9]. However, more recently, AZM-R N. gonorrhoeae has been rarely and sporadically reported to also have reduced susceptibility to ESCs [9, 13], threatening the future efficacy of current therapeutic recommendations. Similarly, the present study showed that the prevalence of combined AZM-MLR/CROD isolates significantly increased as compared with that in all identified N. gonorrhoeae isolates.
Previous studies investigating AZM-R and CROD have focused on the mutations of three genes: 23S rRNA, mtrR and penA [9–12]. Mutations at various positions within the central loop of domain V of the 23S rRNA gene are thought to lead to resistance by reducing the ability of the 23S rRNA protein to bind the antibiotics such as AZM [10]. Previous reports have shown that the mutation C2611T in any of the four alleles of the 23S rRNA can result in a lower level of resistance to AZM [10]. In addition, the mutation A2059G (Escherichia coli numbering) in at least three of the four alleles can confer AZM-HLR, and AZM-sensitive isolates containing this single allele mutation can quickly develop high-level resistance in the presence of erythromycin [10]. In the current study, only seven AZM-R isolates contained mutation C2611T, whereas the remaining large number of AZM-R isolates contained four wild-type alleles. These findings contrast, however, with other reports from Canada [9], the United States [11, 20] and the United Kingdom [10], which most of the AZM-MLR isolates contained this mutation was more than 80 %. Notably, all the above-mentioned seven AZM-R isolates that contained the mutation C2611T showed reduced susceptibility to ceftriaxone. The mutation A2059G, which is linked to AZM-HLR, was not detected in the present study. In the mtrR gene, specific mutations in the promoter or coding region can lead to decrease the MtrCDE efflux pump repression and subsequently increase export of the antimicrobials [20]. Loss of the MtrCDE efflux pump can significantly increase susceptibility to AZM, ESCs, penicillin, ciprofloxacin, and solithromyc in N. gonorrhoeae isolates [21]. In this study, a single nucleotide deletion in the mtrR promoter showed over 85 % in AZMR-R isolates, but not significantly difference between combined AZMR-R/CROS isolates and combined AZMR-R/CROD isolates, in line with a previous report that such a deletion may not implicate in CROD [12]. H105Y, the most prevalent single mutation, was not significantly difference in AZM-LLR isolates as compared to AZM-MLR isolates. Interestingly, the combined mutation in mtrR was only observed in AZM-MLR isolates, but not in in AZM-LLR isolates. Mutation in penA has been associated with decreased susceptibility or resistance to a number of beta-lactam agents, especially to ESCs [22]. The mutations G545S, I312M, and V316T in mosaic alleles of PBP2 were early suggested as important for the increased ESCs resistance [23]. However, a recent study revealed that these three mutations had only a little to effect on resistance, and their capacity to increase resistance to ESCs was dependent on the presence of other mutations in the mosaic alleles [24]. Mutation patterns XIII, XVII and XVIII have been reported to only present in CROD isolates in China [12] and Australia [22]. These three patterns contained G542S, P551S and/or P551L mutations, which have been associated with increased MIC of CRO [25]. However, their effects on the ceftriaxone MIC have not yet been proven by site-directed penA mutations in isogenic strain backgrounds [26] and the present study showed that these three patterns were present in both CROS and CROD isolates (data not shown). The most prevalent mutation pattern in AZMR-R isolates from Canada was XXXIV, which was showed to AZM-R together with reduced susceptibility to ESCs [9]. By comparison, this study revealed the most prevalent mutation patterns (V, XVIII and XXI) were the same in AZMR-LLR, AZMR-MLR, and combined AZMR-R/CROD isolates, respectively. Overall, the results of our study showed that the mutations of these three genes had the considerable diversity, and that either one of these three genes alone or combined mutation patterns of these three genes cannot account for AZM-MLR or combined AZM-R/CROD in our N. gonorrhoeae isolates.
NG-MAST analysis and the resulting development of a phylogenetic tree in this study also indicated a high degree of genetic diversity of N. gonorrhoeae in Guangzhou from 2009 to 2013. This observation may be due to the highly limited epidemiologic information of this study because our data do not represent the whole country, or the flow of large numbers of temporary population in Guangzhou, which lead to great opportunity for transport of new STs [27]. Also, AZM is extensively used in China [5] and has long elimination half-life. Thus we postulate that the diversity of STs developed, in part, in response to antibiotic pressure. Some STs that were observed in the current study (ST3356, ST1866, ST1766, and ST4313) had been noted in a previous report of emerging AZM-R N. gonorrhoeae in Nanjing and Chongqing, China [5], but these did not include STs (ST470, ST649, ST3158, ST1704, ST359, and ST696) that were reported previously in other countries and have been shown to account for most of the resistance or high-level resistance to AZM [9, 18, 28–30].
Conclusions
AZM-R N. gonorrhoeae isolates are increasing and, in combination with CROD, have now been detected in Guangzhou. The combined AZM-R/CROD in N. gonorrhoeae is a relatively new phenomenon, and the mechanism for the emergence of these AZM-R/CROD isolates remains unknown and needs further studied. Therefore, antimicrobial susceptibility/resistance and the molecular epidemiology of AZM-R and/or CROD deserve continuous surveillance, which will be critical in providing valuable information for current and future therapeutic options in China.
Availability of data and materials
The sequencing datasets of porB, tbpB, 23S rRNA, mtrR and penA genes supporting the conclusions of this article are available in the Dryad Digital Repository: http://dx.doi.org/10.5061/dryad.cp3d8.
Abbreviations
- AZM:
-
azithromycin
- AZM-HLR:
-
azithromycin high-level resistant
- AZM-LLR:
-
azithromycin low-level resistant
- AZM-MLR:
-
azithromycin middle-level resistant
- AZM-R:
-
azithromycin-resistant
- CROD :
-
decreased susceptibility to ceftriaxone
- CROS :
-
susceptibility to ceftriaxone
- ESCs:
-
extended-spectrum cephalosporins
- MIC:
-
minimum inhibitory concentration
- NG-MAST:
-
N. gonorrhoeae multi-antigen sequence typing
- PBP2:
-
penicillin-binding protein 2
- STI:
-
sexually transmitted infection.
References
Kovari H, de Melo Oliveira MD, Hauser P, Lauchli S, Meyer J, Weber R, Zbinden R. Decreased susceptibility of Neisseria gonorrhoeae isolates from Switzerland to Cefixime and Ceftriaxone: antimicrobial susceptibility data from 1990 and 2000 to 2012. BMC Infect Dis. 2013;13:603.
Centers for Disease C, Prevention. Update to CDC’s Sexually transmitted diseases treatment guidelines, 2010: oral cephalosporins no longer a recommended treatment for gonococcal infections. MMWR Morb Mortal Wkly Rep. 2012;61(31):590–4.
Bignell C, Unemo M, European STIGEB. 2012 European guideline on the diagnosis and treatment of gonorrhoea in adults. Int J STD AIDS. 2013;24(2):85–92.
Chen SC, Yin YP, Dai XQ, Unemo M, Chen XS. Antimicrobial resistance, genetic resistance determinants for ceftriaxone and molecular epidemiology of Neisseria gonorrhoeae isolates in Nanjing, China. J Antimicrob Chemother. 2014;69(11):2959–65.
Yuan LF, Yin YP, Dai XQ, Pearline RV, Xiang Z, Unemo M, Chen XS. Resistance to azithromycin of Neisseria gonorrhoeae isolates from 2 cities in China. Sex Transm Dis. 2011;38(8):764–8.
Yu LH, Qu Y. Analysis of antimicrobial susceptibilities of 201 Neisseria gonorrhoeae strains [in Chinese]. Zhejiang Pract Med. 2004;9:60–1.
Cao WL, LI XD, Bi C, Liang YH, Song WZ, Lin LY, Wu DB, Zhang L. Analysis of the drug-resistance of Neisseria gonorrhoeae to 6 types of antibiotics in certain area. Int J Lab Med. 2011;32(19):2205–6.
Morita-Ishihara T, Unemo M, Furubayashi K, Kawahata T, Shimuta K, Nakayama S, Ohnishi M. Treatment failure with 2 g of azithromycin (extended-release formulation) in gonorrhoea in Japan caused by the international multidrug-resistant ST1407 strain of Neisseria gonorrhoeae. J Antimicrob Chemother. 2014;69(8):2086–90.
Allen VG, Seah C, Martin I, Melano RG. Azithromycin resistance is coevolving with reduced susceptibility to cephalosporins in Neisseria gonorrhoeae in Ontario, Canada. Antimicrob Agents Chemother. 2014;58(5):2528–34.
Chisholm SA, Dave J, Ison CA. High-level azithromycin resistance occurs in Neisseria gonorrhoeae as a result of a single point mutation in the 23S rRNA genes. Antimicrob Agents Chemother. 2010;54(9):3812–6.
Wu A, Buono S, Katz KA, Pandori MW. Clinical Neisseria gonorrhoeae isolates in the United States with resistance to azithromycin possess mutations in all 23S rRNA alleles and the mtrR coding region. Microb Drug Resist. 2011;17(3):425–7.
Liao M, Gu WM, Yang Y, Dillon JA. Analysis of mutations in multiple loci of Neisseria gonorrhoeae isolates reveals effects of PIB, PBP2 and MtrR on reduced susceptibility to ceftriaxone. J Antimicrob Chemother. 2011;66(5):1016–23.
Katz AR, Komeya AY, Soge OO, Kiaha MI, Lee MV, Wasserman GM, Maningas EV, Whelen AC, Kirkcaldy RD, Shapiro SJ et al. Neisseria gonorrhoeae with high-level resistance to azithromycin: case report of the first isolate identified in the United States. Clin Infect Dis. 2012;54(6):841–3.
Cao WL, Liang JY, Li XD, Bi C, Yang RD, Liang YH, Li P, Zhong DQ, Ye XD, Zhang XB. Trends in antimicrobial resistance in Neisseria gonorrhoeae isolated from Guangzhou, China, 2000 to 2005 and 2008 to 2013. Sex Transm Dis. 2015;42(1):27–9.
World Health Organization. Global action plan to control the spread and impact of antimicrobial resistance in Neisseria gonorrhoeae. 2012. Available at: http://www.who.int/reproductivehealth/publications/rtis/9789241503501/en/. (19 October 2015, date last accessed).
Ng LK, Martin I, Liu G, Bryden L. Mutation in 23S rRNA associated with macrolide resistance in Neisseria gonorrhoeae. Antimicrob Agents Chemother. 2002;46(9):3020–5.
Martin IM, Ison CA, Aanensen DM, Fenton KA, Spratt BG. Rapid sequence-based identification of gonococcal transmission clusters in a large metropolitan area. J Infect Dis. 2004;189(8):1497–505.
Starnino S, Stefanelli P, Neisseria gonorrhoeae Italian Study G. Azithromycin-resistant Neisseria gonorrhoeae strains recently isolated in Italy. J Antimicrob Chemother. 2009;63(6):1200–4.
Kaiser NC, Liang LJ, Melrose RJ, Wilkins SS, Sultzer DL, Mendez MF. Differences in anxiety among patients with early- versus late-onset Alzheimer’s disease. J Neuropsychiatry Clin Neurosci. 2014;26(1):73–80.
Centers for Disease C, Prevention. Neisseria gonorrhoeae with reduced susceptibility to azithromycin--San Diego County, California, 2009. MMWR Morb Mortal Wkly Rep. 2011;60(18):579–81.
Golparian D, Shafer WM, Ohnishi M, Unemo M. Importance of multidrug efflux pumps in the antimicrobial resistance property of clinical multidrug-resistant isolates of Neisseria gonorrhoeae. Antimicrob Agents Chemother. 2014;58(6):3556–9.
Whiley DM, Limnios EA, Ray S, Sloots TP, Tapsall JW. Diversity of penA alterations and subtypes in Neisseria gonorrhoeae strains from Sydney, Australia, that are less susceptible to ceftriaxone. Antimicrob Agents Chemother. 2007;51(9):3111–6.
Takahata S, Senju N, Osaki Y, Yoshida T, Ida T. Amino acid substitutions in mosaic penicillin-binding protein 2 associated with reduced susceptibility to cefixime in clinical isolates of Neisseria gonorrhoeae. Antimicrob Agents Chemother. 2006;50(11):3638–45.
Tomberg J, Unemo M, Davies C, Nicholas RA. Molecular and structural analysis of mosaic variants of penicillin-binding protein 2 conferring decreased susceptibility to expanded-spectrum cephalosporins in Neisseria gonorrhoeae: role of epistatic mutations. Biochemistry. 2010;49(37):8062–70.
Whiley DM, Goire N, Lambert SB, Ray S, Limnios EA, Nissen MD, Sloots TP, Tapsall JW. Reduced susceptibility to ceftriaxone in Neisseria gonorrhoeae is associated with mutations G542S, P551S and P551L in the gonococcal penicillin-binding protein 2. J Antimicrob Chemother. 2010;65(8):1615–8.
Unemo M, Shafer WM. Antimicrobial resistance in Neisseria gonorrhoeae in the 21st century: past, evolution, and future. Clin Microbiol Rev. 2014;27(3):587–613.
Wenling C, Xibao Z, Shi F, Minchang W, Ping L, Debiao W, Jinlan Y. Analysis of the antibiotic sensitivity of Neisseria gonorrhoeae in Guangzhou, Peoples Republic of China. Sex Transm Dis. 2000;27(8):480–2.
Palmer HM, Young H, Winter A, Dave J. Emergence and spread of azithromycin-resistant Neisseria gonorrhoeae in Scotland. J Antimicrob Chemother. 2008;62(3):490–4.
Chisholm SA, Neal TJ, Alawattegama AB, Birley HD, Howe RA, Ison CA. Emergence of high-level azithromycin resistance in Neisseria gonorrhoeae in England and Wales. J Antimicrob Chemother. 2009;64(2):353–8.
Galarza PG, Alcala B, Salcedo C, Canigia LF, Buscemi L, Pagano I, Oviedo C, Vazquez JA. Emergence of high level azithromycin-resistant Neisseria gonorrhoeae strain isolated in Argentina. Sex Transm Dis. 2009;36(12):787–8.
Acknowledgments
We are grateful for the collaboration of the heads and staff at STI clinics in Guangzhou, China.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
JYL and WLC contributed to the design of the analysis and wrote the draft of the manuscript. YRD, XDY and XXC provided N. gonorrhoeae isolates and clinical information. XDL, CB, YHL and PL identified N. gonorrhoeae isolates and tested antimicrobial susceptibility. XBZ is the corresponding author, supervised the research and edited the manuscript. All authors read and approved the final manuscript.
Additional files
Additional file 1:
Table S1. Characteristics of AZM-LLR N. gonorrhoeae isolates identified in Guangzhou in 2009-2013 (n = 33). Table S2. Characteristics of AZM-MLR N. gonorrhoeae isolates identified in Guangzhou in 2009-2013 (n = 44). Table S3. The classification of mutation patterns of the PBP2 proteins based on amino acids 500 to 570. (DOCX 46.2 kb)
Additional file 2:
Figure S1. A neighbor-joining phylogenetic tree was constructed using the concatenated sequences of por (490 bp) and tbpB (390 bp) alleles, which were identified by the NG-MAST method, from 33 AZM-LLR N. gonorrhoeae isolates in Guangzhou, China in 2009–2013. (DOCX 1475 kb)
Additional file 3:
Figure S2. A neighbor-joining phylogenetic tree was constructed using the concatenated sequences of por (490 bp) and tbpB (390 bp) alleles, which were identified by the NG-MAST method, from 44 AZM-MLR N. gonorrhoeae isolates in Guangzhou, China in 2009–2013. (DOCX 1372 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Liang, JY., Cao, WL., Li, XD. et al. Azithromycin-resistant Neisseria gonorrhoeae isolates in Guangzhou, China (2009–2013): coevolution with decreased susceptibilities to ceftriaxone and genetic characteristics. BMC Infect Dis 16, 152 (2016). https://doi.org/10.1186/s12879-016-1469-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-016-1469-3