Abstract
Background
Ethiopia is one of the most seriously HIV affected countries in Sub-Saharan Africa. Anemia is a known predictor of disease progression and death among HIV infected patients. In this study, we investigated the magnitude and correlates of anemia among HIV infected patients receiving HAART at a referral hospital in Ethiopia.
Methods
A retrospective cohort study was conducted from November 2011 to February 2012 in Zewditu Memorial Hospital, Addis Ababa, Ethiopia. Records of 1061 patients on HAART were selected using simple random sampling technique. Socio-demographic and clinical characteristics of the study patients were collected using standardized data extraction instrument. Data were analyzed using STATA version 11.0. Odds ratios with 95% confidence intervals were used to quantify the strength of association between anemia and its potential predictors.
Results
The prevalence of anemia at baseline was 42.9%. However, the prevalence significantly decreased to 20.9% at 6 months (p < 0.001) and to 14.3% at 12 months (p = 0.001) after HAART initiation. At baseline, male sex (AOR = 1.55; 95% CI: 1.18-2.03), clinical stage III/IV (AOR = 2.03; 95% CI: 1.45-2.83) and TB co-infection (AOR = 1.52; 95% CI: 1.08-2.13) were independently associated with the odds of being anemic. After 6 months of HAART, male sex (AOR = 1.59; 95% CI: 1.13-2.23), baseline anemia (AOR = 2.38; 95% CI: 1.71-3.33) and TDF-based HAART (AOR = 2.87; 95% CI: 1.80-4.60) were independently associated with the odds of being anemic. Besides, anemia was independently associated with older age at 6 months. After 12 months of HAART, baseline anemia (AOR = 2.01; 95% CI: 1.36-2.97), age group 25–34 years (AOR = 5.92; 95% CI: 1.39-25.15), age group 45–54 years (AOR = 4.78; 95% CI: 1.07-21.36), CD4 count below 200 cells/mm3 (AOR = 2.15; 95% CI: 1.21-3.82) and 200–350 cells/mm3 (AOR = 1.91; 95% CI: 1.13-3.25) were independently associated with the odds of being anemic.
Conclusions
Although a remarkable reduction in the prevalence of anemia was observed following initiation of HAART, a significant proportion of HIV patients remained anemic after 12 months of HAART suggesting the need for routine screening and proper treatment of anemia to mitigate its adverse effects.
Similar content being viewed by others
Background
Complications of human immunodeficiency virus (HIV) infection include hematological abnormalities manifested by pancytopenia, anemia being the leading abnormality [1-3]. However, the prevalence of anemia in HIV patients varies considerably, ranging from 1.3% to 95% [4]. Several factors including stage of HIV, age and sex are said to account for the variations in HIV prevalence [4]. The causes of anemia have been reported to be multifactorial. Direct effects of HIV and its viral proteins as well as immune dysregulations during HIV infection were found to be responsible for bone marrow suppression [5,6]. Moreover, opportunistic infections of the bone marrow with pathogens such as Mycobacterium avium complex, Parvovirus B-19, Cytomegaloviruses, Cryptococcus neoformans and Histoplasma capsulatum were reported to cause abnormalities in blood cell counts [6,7]. Drugs used to treat HIV infection and its complications are also known to cause bone marrow suppression [7,8]. It is widely known that AZT alone and AZT based highly active antiretroviral treatment (HAART) regimen is associated with significant reduction of hemoglobin (Hgb) level [7,9,10].
Anemia is associated with impaired physical functioning, psychological distress and poor quality of life [7]. Besides, independent of CD4 and viral load counts, anemia has been reported to predict HIV progression to acquired immune deficiency syndrome (AIDS) with poor survival [4,7,11,12]; on the other hand, treatment of anemia was observed to be associated with reversal of increased risk of death [13]. In addition, anemia was reported to be strongly and consistently associated with HIV disease progression and death despite HAART initiation [8], suggesting the need for routine screening and treatment of anemia in HIV patients on HAART. Prevalence of anemia among Ethiopian men and women aged 15–49 years was documented to be 11% and 17%, respectively [14]. Regional differences were remarkable and the prevalence of anemia in men and women aged 15–49 years in Addis Ababa were 3% and 9%, respectively [14]. In addition, recent study reported a considerably higher prevalence of anemia among HIV-infected antiretroviral-naïve adult Ethiopians (38% for men and 62% for women) [15]. Ethiopians’ normal immunohematological profile is known to be lower than the corresponding values in Caucasians [16]. Besides, AZT-based HAART is one of the first line regimens recommended for treating HIV infected adults [17]. However, the magnitude of anemia and its risk factors among HIV patients on HAART are not well document in Ethiopia. Thus, this study investigated the prevalence of anemia and its associated factors among HIV infected patients receiving HAART in a referral hospital in Ethiopia.
Methods
Study setting and study population
A retrospective cohort study was conducted by reviewing hospital data of patients who were receiving HAART at the HIV clinic of Zewditu Memorial Hospital, Addis Ababa, Ethiopia from November 2011 to February 2012. The Hospital launched Antiretroviral Therapy (ART) in July 2003 as the first pilot site in the country. Among 15,000 HIV infected adults on care at the Hospital, 9,287 were on ART during data collection. Among those on ART, a total of 1061 HIV infected adults were randomly selected and included in this study. Sample size was estimated using a single population proportion formula, taking p=46% (expected prevalence of anemia at baseline) [1], 3% level of precision (d) with 95% confidence interval. Patients transferred in from other health institutions, patients who started ART in the hospital before March 1, 2005 or after November 30, 2010 and patients who were pregnant at baseline or during the follow up visits were excluded from the study.
Data collection
The data was extracted using a standardized instrument by three ART nurses. The collected information includes socio-demographics, clinical characteristics, medication use and immunohematological profile of patients at baseline, 6 and 12 months after initiation of HAART. Hemoglobin (Hgb) values, red blood cell count, white blood cell counts with absolute CD4 cells and CD8 cells, and platelets were determined using the hematology analyzer Cell-Dyn 1800 (Abbott Laboratories Diagnostics Division, USA) whereas CD4+ T cells were assayed using the BD FACSCOUNT system (Becton Dickenson and Company, California, USA). To ensure good quality data, training of data collectors, pre- testing of data extraction instrument and continuous supervision of the data collection process was carried out. Data were checked for missed values and outliers during data management.
Definition of outcome variable and statistical analysis
Data were computerized using Epidata version 3.1 and STATA version 11 (StataCorp LP, college station, TX) was used for data analysis. Anemia was defined based on hematological reference values for adult Ethiopian population [16]. Accordingly, anemia was defined as Hgb concentration less than or equal to 13.9 g/dl for adult males and less than or equal to 12.2 g/dl for adult females. It was further classified into mild (10–12.2 g/dl for females and 10–13.9 g/dl for males), moderate (8–10 g/dl) and severe (<8 g/dl) for both sexes.
The effect of different risk factors on the odds of being anemic were investigated at baseline, at 6 months and at 12 months following initiation of HAART. Odds ratio with 95% confidence interval was used to quantify the strength of association between anemia and its potential predictors. Variables that were found significantly associated with the outcome variable (p < 0.05) in the bivariate analysis as well as variables that were reported to be associated with anemia in previous studies and that were clinically relevant for the occurrence of anemia were included in the multivariable logistic regression model to obtain adjusted effects. Since height was not recorded for the majority of the study participants, missing values for body mass index (BMI) were coded as a separate category before including BMI in multivariable logistic regression so that data from all study participants can be used.
Ethical consideration
Study protocol was approved by the Institutional Review Board of Aklilu Lemma Institute of Pathobiology, Addis Ababa University and Addis Ababa City Administration Health Bureau. Identifiers of the study participants were not collected to maintain confidentiality.
Results
Baseline characteristics of patients
Demographic and clinical characteristics of the study patients at treatment initiation are presented in Table 1 and Table 2, respectively. Of the total 1061 study patients, 60% were females, 76.0% were in the age range of 25–49 years and the overall age range was 17–88 years. Majority (62.6%) of the patients were classified as WHO clinical stage III/IV and 79.4% had a CD4 cell count of less than 200 cells/mm3. The mean Hgb value was 12.9 (sd = 2.4 g/dl) while the mean CD4 cell count was 139.8 (sd = 78.8) cells/mm3. Five hundred and forty-four (52.0%) of the study patients were co-infected with different types of opportunistic infections.
Anemia before HAART initiation
A total of 455 (42.9%) patients were anemic at baseline of which 360 (34.0%) had mild, 71 (6.7%) had moderate and 24 (2.3%) had severe anemia. The overall prevalence of anemia was higher in males (50.4%) than in females (37.8%) (p < 0.001). Significantly higher proportion of females had moderate and severe forms of anemia compared to males: moderate anemia was 7.9% among females and 4.9% among males (p < 0.001) and severe anemia (2.9% among females and 1.4% among males (p < 0.001).
Different factors were observed to be associated with being anemic before HAART initiation (Table 3). In univariable analysis, increased risk of anemia at baseline was associated with male sex (OR = 1.67; 95% CI: 1.30-2.14), age greater than 55 years (OR = 2.40; 95% CI: 1.06-5.41), clinical stage III/IV (OR = 2.35; 95% CI: 1.81-3.06), BMI <18.5 (OR = 2.32; 95% CI: 1.24-4.36) and the presence of opportunistic infections such as TB (OR =2.07; 95% CI: 1.54-2.80) and candidiasis (OR = 1.44; 95% CI: 1.08-1.91). CD4 count <200 cells/mm3 and 200-350 cells/mm3 are associated with decreased odds of being anemic. In multivariable logistic regression analysis, male sex, clinical stage III/IV and TB co-infection were independently associated with increased odds of being anemic whereas CD4 count <200 cells/mm3 and 200-350 cells/mm3 were independently associated with reduced odds of being anemic in the multivariable analysis.
Anemia after HAART initiation
A total of 980 (92.4%) of the study participants had Hgb measurements at 6 months of HAART initiation. Of these, 970 (99%) had Hgb measurements at baseline. And of the 896 (84.4%) patients who had Hgb measurements at 12 month, 888 (99.1%) had Hgb measurements both at baseline and at 6 months of HAART treatment. Patients with missing Hgb measurements at 6 month (81 patients) were more likely to be those in the age group of 25-34 years, those having a CD4 cell counts of ≥350 cells/mm3, those who were not on co-trimoxazole prophylactic treatment and those who were receiving d4T based HAART regimen. However, there was no statistically significant difference in the sex, BMI values, fluconazole treatment status, TB treatment status and anti-microbial treatment status between patients included and excluded from the study of anemia at the 6 month. During the study period, changes were made to the regimen of 85 patients. Of the 60 patients for whom drug regimen was changed in the first 6 months, 25(41.7%) were those who were anemic at baseline. Treatment regimen was changed for 40 of the patients who were on AZT based regimen (15 (37.5%) were anemic at baseline), for 16 of those on d4T- based regimen (9(56.3%) were anemic at baseline) and for 4 of those on TDF- based regimen (1(25.0%) were anemic at the baseline). After 6 months, 25 patients have changed their treatment regimens of whom 18 (72%) were patients on d4T- based regimen and 7 (28%) were those on AZT- based regimen. The mean (sd) Hgb values of the study patients at 6 and 12 months were 14.0 (2.3) g/dl and 14.4 (1.9) g/dl, respectively.
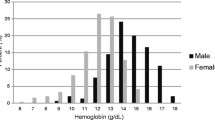
The overall prevalence of anemia significantly decreased after HAART initiation. The prevalence declined from 42.9% at baseline to 20.9% at 6 months (p < 0.001) and to 14.3% at 12 months (p = 0.001). There was also a consistent decrease in the prevalence of mild, moderate and severe anemia after treatment with HAART (Figure 1). Similar to the baseline level, anemia remained to be more prevalent among males compared to females after 6 months of treatment with HAART. At 6 months following initiation of HAART, 25.4% of males and 17.9% of females were anemic. At the same time, more males than females had mild anemia (24.2% versus 15.4%), moderate anemia (2.4% versus 1.2%) and severe anemia (0.2% versus 0.0%) (p = 0.002). However, there was no statistically significant difference in the prevalence of anemia between males and females at 12 months of HAART.
Risk factors for anemia after initiation of HAART are shown in Table 4. At 6 months of HAART, male sex (AOR = 1.59; 95% CI: 1.13-2.23), anemia at baseline (AOR = 2.38; 95% CI: 1.71-3.33), and TDF- based HAART regimen (AOR = 2.87; 95% CI: 1.80-4.60) were independent predictors of anemia. Besides, at 6 months, older age was independently associated with increased odds of being anemic. At 12 months, anemia at baseline (AOR = 2.01; 95% CI: 1.36-2.97), being in the age range of 25–34 years (AOR = 5.92; 95% CI: 1.39-25.15), being in the age range of 45–54 years (AOR = 4.78; 95% CI: 1.07-21.36), CD4 count below 200 cells/mm3 (AOR = 1.91; 95% CI: 1.13-3.25) and 200–350 cells/mm3 (AOR = 2.15; 95% CI: 1.21-3.82) were independently associated with increased odds of being anemic.
Discussion
In this study, we investigated the prevalence of anemia and its associated factors in a large cohort of HIV infected patients taking HAART over 12 months. A large proportion of our study patients had anemia at baseline and subsequent follow-up time points. The prevalence of anemia before initiation of HAART in this study was comparable with the prevalence reported in other studies [1,18,19]. However, it was much higher compared to the prevalence reported by Gedefaw et al. from Ethiopia [20], Firnhaber et al. [21] and Mata-Marín et al. [22] elsewhere, who reported a prevalence of 29.9%, 12.0% and 20.0%, respectively. The reasons for the observed difference might be due to the heterogeneity of study population and differences in the study settings in terms of nutritional status, stages of HIV infection and health interventions including treatment of hematological abnormalities. For example, both Firnhaber et al. [21] and Mata-Marin et al. [22] excluded patients with illnesses including opportunistic infections who could have contributed to higher anemia prevalence. Furthermore, the patients in Firnhaber et al. study were from nine countries with diverse geographic settings. A direct comparison of prevalence of anemia in different studies is difficult because of differences in the study population, presentation of data and definition used for anemia. This study used the definition that was proposed specifically for Ethiopian population to define anemia [16].
Results from this study show a remarkable reduction in the prevalence of anemia after initiation of HAART. In agreement with our observation, in other studies, the prevalence of anemia in HAART naïve was significantly higher compared to HAART experienced patients [1,23]. The reduction in opportunistic infections including TB, candidiasis and others, as well as the reduction of inflammatory cytokines such as tumor necrosis factor (TNF) that are implicated in the suppression of erythropoiesis could be mechanisms that may account for the improvement of anemia after initiation of HAART [24,25]. Despite a significant reduction in the prevalence of anemia at 12 months, close to 15% of the patients had anemia implying the need for routine screening of anemia and subsequent investigation of its causes. In this study, based on the data we have, we were not able to determine the specific reasons why these patients had anemia despite treatment with HAART. After 12 months of HAART, low CD4 count was a predictor of anemia suggesting poor recovery and probably high viral load in those patient with anemia after 12 months of HAART. Data on viral load would have been useful but this test is not routinely done at the study site and we were not able to include in the analysis.
Similar to this study, some studies reported a high prevalence of anemia in males compared to females and attributed it to the fact that lower Hgb level is used to define anemia in women than men [26,27]. However, many previous studies reported a high prevalence of anemia in females compared to male HIV infected patients [8,28]. The proposed reason was the presence of menstrual blood loss and to the drains on iron stores that occur with pregnancy and delivery in women. However, none of the above studies described the prevalence of anemia according to severity grades. In our study, moderate and severe forms of anemia were higher in females compared to males both before and after 6 months on HAART. The absence of significant difference in the risk of anemia at 12 months on HAART between male and female patients seen in this study may suggest the role of HAART to improve anemia after 12 months.
We observed an increase in the risk of anemia with age. The hematopoietic stem cell displays increasing erythropoietin (EPO) resistance with increasing age and further aging is associated with increased pro-inflammatory cytokine expression many of which contributing to EPO resistance [29], thereby resulting in anemia.
Different studies reported association between increased incidence of low blood cell counts with progressive immunologic deterioration and advanced disease due to HIV [2,8,20]. It was suggested that increasing viral burden as HIV disease progresses could cause hematological abnormality by increasing cytokine mediated myelosuppression [25]. In this study, low CD4 cell count was associated with anemia at baseline although the reasons for such association are not clear. At baseline, the presence of opportunistic infections such as TB and fungal infections like candidiasis might play a major role in the pathogenesis of anemia than the deterioration in immunity as proposed by Scadden and his group [30]. However, an increasing risk in anemia with decreasing values of CD4 cell count was seen at 12 months; and the observed association between anemia and lower CD4 cell count at 12 month might be related to poor immunological recovery and high viral load rather than to opportunistic infections. Increased risk of anemia in patients who were on anti-TB drugs has been observed in this study and it may be related to the anti-TB drugs. More importantly, TB is a chronic infection known to cause moderate degree of anemia [31] which is reversible on treatment.
The absence of significant association between treatment with AZT and anemia in the current study despite its frequent association with bone marrow suppression has also been previously described [32,33]. The effect of AZT may be modest when taken as HAART than administered as a single dose. However, the association of anemia with TDF-based regimen in this study, despite its low cytotoxicity towards erythroid progenitor cells and its effectiveness in terms of viral suppression, CD4 response and reduced adverse events compared to AZT and d4T [34], is largely unexplained and needs further study.
This study is based on a large cohort of HIV patients on HAART. However, data were collected for routine clinical care, and hence, other important variables, notably viral load are lacking. Moreover, the majority of patients had no data on BMI. Nevertheless, this study highlights the burden of anemia among HIV patients before and after HAART.
Conclusions
In conclusion, anemia is a common manifestation of HIV infection both before and after initiation of HAART in the study setting. The treatment of HIV infected patients with HAART has resulted in a remarkable reduction in the prevalence of anemia after 12 months. However, a substantial proportion of patients had anemia after 12 months of HAART, suggesting the need for routine screening of anemia, investigating its causes and instituting appropriate treatment to mitigate the adverse effects of anemia. Considering the high burden even after a prolonged HAART, there is a need for developing a comprehensive screening, treatment and monitoring protocol for anemia.
Abbreviations
- AIDS:
-
Acquired immune deficiency syndrome
- OR:
-
Odds ratio
- AOR:
-
Adjusted odds ratio
- ART:
-
Anti-retroviral therapy
- AZT:
-
Zidovudine
- CD4:
-
Cluster of differentiation 4
- d4T:
-
Stavudine
- HAART:
-
Highly active antiretroviral treatment
- Hgb:
-
Hemoglobin
- HIV:
-
Human immunodeficiency virus
- TB:
-
Tuberculosis
- TDF:
-
Tenofovir disoproxil fumarate
References
Owiredu WK, Quaye L, Amidu N, Addai-Mensah O. Prevalence of anaemia and immunological markers among ghanaian HAART-naive HIV-patients and those on HAART. Afr Health Sci. 2011;11(1):2–15.
Dikshit B, Wanchu A, Sachdeva RK, Sharma A, Das R. Profile of hematological abnormalities of Indian HIV infected individuals. BMC Blood Disord. 2009;9:5.
Dhurve SA, Dhurve AS. Bone marrow abnormalities in HIV disease. Mediterr J Hematol Infect Dis. 2013;5(1):e2013033.
Belperio PS, Rhew DC. Prevalence and outcomes of anemia in individuals with human immunodeficiency virus: a systematic review of the literature. Am J Med. 2004;116(Suppl 7A):27S–43.
Re MC, Zauli G, Furlini G, Giovannini M, La Placa M. HIV-1 infection and hematologic picture. Microbiologica. 1991;14(2):165–76.
Bain BJ. Pathogenesis and pathophysiology of anemia in HIV infection. Curr Opin Hematol. 1999;6(2):89–93.
Moyle G. Anaemia in persons with HIV infection: prognostic marker and contributor to morbidity. AIDS Rev. 2002;4(1):13–20.
Sullivan PS, Hanson DL, Chu SY, Jones JL, Ward JW. Epidemiology of anemia in human immunodeficiency virus (HIV)-infected persons: results from the multistate adult and adolescent spectrum of HIV disease surveillance project. Blood. 1998;91(1):301–8.
Moh R, Danel C, Sorho S, Sauvageot D, Anzian A, Minga A, et al. Haematological changes in adults receiving a zidovudine-containing HAART regimen in combination with cotrimoxazole in Cote d’Ivoire. Antivir Ther. 2005;10(5):615–24.
Forna F, Moore D, Mermin J, Brooks JT, Were W, Buchacz K, et al. Hematologic changes associated with Zidovudine following single-drug substitution from stavudine in a home-based AIDS care program in rural Uganda. J Int Assoc Physicians AIDS Care. 2009;8(2):128–38.
Mocroft A, Kirk O, Barton SE, Dietrich M, Proenca R, Colebunders R, et al. Anaemia is an independent predictive marker for clinical prognosis in HIV-infected patients from across Europe. EuroSIDA study group. AIDS. 1999;13(8):943–50.
Adias TC, Uko E, Erhabor O. Anaemia in human immunodeficiency virus infection: a review. Niger J Med. 2006;15(3):203–6.
Moore RD. Anemia and human immunodeficiency virus disease in the era of highly active antiretroviral therapy. Semin Hematol. 2000;37(4 Suppl 6):18–23.
CSA. Ethiopian demographic and health survey 2011. Maryland, USA: ICF Internationa; 2012.
Ferede G, Wondimeneh Y. Prevalence and related factors of anemia in HAART-naive HIV positive patients at Gondar University Hospital. Northwest Ethiopia BMC Hematol. 2013;13(1):8.
Tsegaye A, Messele T, Tilahun T, Hailu E, Sahlu T, Doorly R, et al. Immunohematological reference ranges for adult Ethiopians. Clin Diagn Lab Immunol. 1999;6(3):410–14.
MOH. Guideline for pediatric HIV/AIDS care and treatment in Ethiopia. Addis Ababa: MOH; 2007.
Semba RD, Shah N, Vlahov D. Improvement of anemia among HIV-infected injection drug users receiving highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2001;26(4):315–19.
Kyeyune R, Saathoff E, Ezeamama AE, Loscher T, Fawzi W, Guwatudde D. Prevalence and correlates of cytopenias in HIV-infected adults initiating highly active antiretroviral therapy in Uganda. BMC Infect Dis. 2014;14:496.
Gedefaw L, Yemane T, Sahlemariam Z, Yilma D. Anemia and risk factors in HAART naive and HAART experienced HIV positive persons in south west Ethiopia: a comparative study. PLoS One. 2013;8(8):e72202.
Firnhaber C, Smeaton L, Saukila N, Flanigan T, Gangakhedkar R, Kumwenda J, et al. Comparisons of anemia, thrombocytopenia, and neutropenia at initiation of HIV antiretroviral therapy in Africa, Asia, and the Americas. Int J Infect Dis. 2010;14(12):e1088–92.
Mata-Marin JA, Gaytan-Martinez JE, Martinez-Martinez RE, Arroyo-Anduiza CI, Fuentes-Allen JL, Casarrubias-Ramirez M. Risk factors and correlates for anemia in HIV treatment-naive infected patients: a cross-sectional analytical study. BMC Res Notes. 2010;3:230.
Denue BA, Kida IM, Hammagabdo A, Dayar A, Sahabi MA. Prevalence of anemia and immunological markers in HIV-infected patients on highly Active antiretroviral therapy in Northeastern Nigeria. Infect Dis. 2013;6:25–33.
Idigbe EO, Adewole TA, Eisen G, Kanki P, Odunukwe NN, Onwujekwe DI, et al. Management of HIV-1 infection with a combination of nevirapine, stavudine, and lamivudine: a preliminary report on the Nigerian antiretroviral program. J Acquir Immune Defic Syndr. 2005;40(1):65–9.
Redig AJ, Berliner N. Pathogenesis and clinical implications of HIV-related anemia in 2013. Hematol Am Soc Hematol Educ Program. 2013;2013:377–81.
Behler C, Shade S, Gregory K, Abrams D, Volberding P. Anemia and HIV in the antiretroviral era: potential significance of testosterone. AIDS Res Hum Retroviruses. 2005;21(3):200–6.
Omoregie R, Omokaro EU, Palmer O, Ogefere HO, Egbeobauwaye A, Adeghe JE, et al. Prevalence of anaemia among HIV-infected patients in Benin City. Nigeria Tanzan J Health Res. 2009;11(1):1–4.
Wills TS, Nadler JP, Somboonwit C, Vincent A, Leitz G, Marino K, et al. Anemia prevalence and associated risk factors in a single-center ambulatory HIV clinical cohort. AIDS Read. 2004;14(6):305–10. 313–305.
Vanasse GJ, Berliner N. Anemia in elderly patients: an emerging problem for the 21st century. Hematology Am Soc Hematol Educ Program. 2010:271–275
Scadden DT, Zon LI, Groopman JE. Pathophysiology and management of HIV-associated hematologic disorders. Blood. 1989;74(5):1455–63.
Lee SW, Kang YA, Yoon YS, Um SW, Lee SM, Yoo CG, et al. The prevalence and evolution of anemia associated with tuberculosis. J Korean Med Sci. 2006;21(6):1028–32.
Kiragga AN, Castelnuovo B, Nakanjako D, Manabe YC. Baseline severe anaemia should not preclude use of zidovudine in antiretroviral-eligible patients in resource-limited settings. J Int AIDS Soc. 2010;13:42.
Renner LA, Dicko F, Koueta F, Malateste K, Gueye RD, Aka E, et al. Anaemia and zidovudine-containing antiretroviral therapy in paediatric antiretroviral programmes in the IeDEA paediatric west African database to evaluate AIDS. Int AIDS Soc. 2013;16:18024.
Gallant JE, DeJesus E, Arribas JR, Pozniak AL, Gazzard B, Campo RE, et al. Tenofovir DF, emtricitabine, and efavirenz vs. zidovudine, lamivudine, and efavirenz for HIV. N Engl J Med. 2006;354(3):251–60.
Acknowledgements
This study was financed by Addis Ababa University, Aklilu Lemma Institute of Pathobiology. We would like to acknowledge data collectors, and staff of ART clinic of Zewditu Memorial Hospital especially Sr. Tizita Woldeyes for collecting the data.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
This manuscript emanated from MSc thesis of MA, and WE, MB and GM were supervisors of MA. MA and WE designed the study and MA collected the data and drafted the manuscript. AS facilitated data collection. MA, WE, GM and MB involved in the analysis and interpretation of the data. MB made a major revision after the first draft. WE, GM and AS reviewed the manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Assefa, M., Abegaz, W.E., Shewamare, A. et al. Prevalence and correlates of anemia among HIV infected patients on highly active anti-retroviral therapy at Zewditu Memorial Hospital, Ethiopia. BMC Hematol 15, 6 (2015). https://doi.org/10.1186/s12878-015-0024-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12878-015-0024-6