Abstract
Background
Frailty is associated with poor prognosis in a wide range of illnesses. However, its prognostic implications for older patients with community-acquired pneumonia (CAP) are not adequately addressed.
Methods
In this study, patients were classified into 3 groups according to the frailty index based on standard laboratory tests (FI-Lab) score: robust (FI-Lab < 0.2), pre-frail (FI-Lab 0.2–0.35), and frail (FI-Lab ≥ 0.35). The relationships between frailty and all-cause mortality and short-term clinical outcomes (length of stay, duration of antibiotic therapy, in-hospital mortality) were examined.
Results
Finally, 1164 patients were included, the median age was 75 years (interquartile range: 69, 82), and 438 patients (37.6%) were women. According to FI-Lab, 261(22.4%), 395(33.9%), and 508(43.6%) were robust, pre-frail, and frail. After adjustment for confounding variables, frailty was independently associated with prolonged antibiotic treatment (p = 0.037); pre-frailty and frailty were independently associated with longer inpatient days (p < 0.05 for both). The risk of in-hospital mortality was independently increased in frail patients (HR = 5.01, 95% CI = 1.51–16.57, p = 0.008) but not pre-frail patients (HR = 2.87, 95% CI = 0.86–9.63, p = 0.088) compared to robust patients. During a median follow-up of 33.9 months (interquartile range: 32.8 to 35.1 months), 408 (35.1%) patients died, of whom 29 (7.1%) were robust, 112 (27.5%) were pre-frail, and 267 (65.9%) were frail. Compared to robust patients, frail and pre-frail were significantly associated with increased risk for all-cause death (HR = 4.29, 95%CI: 1.78–10.35 and HR = 2.42 95%CI: 1.01–5.82, respectively).
Conclusions
Frailty is common among older patients with CAP and is strongly associated with increased mortality, longer length of stay, and duration of antibiotics. A routine frail assessment at the admission of elderly patients with CAP is necessary as the first step for appropriate multidisciplinary interventions.
Similar content being viewed by others
Introduction
Community-acquired pneumonia (CAP) is the most prevalent infectious disease in older adults and is associated with poor prognosis and high medical costs worldwide [1, 2]. CAP-associated morbidity and mortality increase with age. Despite medical advances, mortality in elderly patients with CAP is still high [3]. Identifying high-risk patients based on dynamic clinical indicators is essential to perform interventions on these variables to reduce the risk.
Frailty, a geriatric syndrome, is an age-related disease characterized by a decline in functions across multiple physiological systems and an increased vulnerability to stressors. This increases the risk of adverse clinical outcomes, including falls, hospitalization, and death. Frailty is also associated with advanced age, disabilities, and comorbidities [4, 5]. Frailty can be evaluated using various tools, while it currently lacks a universally accepted standard definition [6]. The frailty index (FI) is one of the most used tools for defining frailty and predicting patient death [7]. The frailty index based on laboratory test (FI-lab), defined as the proportion of aberrant results from the total of measured tests, is one method to assess frailty [8, 9]. With readily available laboratory test data in electronic medical records, frailty by the FI-lab might be evaluated objectively and uniformly. In elderly patients, a higher FI-Lab has been linked to death, readmissions, and longer hospital stays [10,11,12].
Previous research demonstrated that frailty provides additional value to disease-specific severity measures predicting mortality following acute medical hospitalizations [13, 14]. In older persons, frailty influenced the susceptibility and severity of pneumonia [15]. Compared to other clinical factors, frailty has the advantage that it is a modifiable risk factor on which physicians could act. However, the relationship between frailty and clinical events in older patients with CAP has not been adequately addressed.
In this study, we aim to evaluate the association of FI-Lab, created at admission with routine laboratory tests, with short-term outcomes (i.e., length of stay, duration of antibiotic therapy) and long-term outcomes (i.e., all-cause mortality) in a contemporary cohort of elderly patients with CAP.
Methods
Study population
This is a single-center retrospective observational cohort study, which initially included 1359 patients aged ≥ 65 years with a principal diagnosis of CAP admitted consecutively between January 2018 and December 2019 to the First Affiliated Hospital of Nanjing Medical University (NJMU). The diagnosis of CAP was established according to the Chinese Guidelines for Adult CAP (2016 Edition) [16]. The exclusion criteria were patients without medical records or routine laboratory variables (here, routine blood tests, blood biochemistry, and coagulation tests) or readmission or patients with missing data on follow-up. The research was approved by the Ethics Committee of the First Affiliated Hospital of NJMU, and the ethics number is 2020-SR-072.
Data collection
Data were independently collected from electronic medical records by two researchers and cross-checked. Included indicators were as follows: age; height; weight; sex; smoking and drinking history; severity of CAP as measured by the CURB-65; comorbidities as measured by the age-adjusted Charlson Comorbidity Index (aCCI); laboratory results from the first 24 h of admission, routine blood tests, blood biochemistry, and coagulation tests, high sensitivity C-reactive protein, eGFR, procalcitonin; length of stay during hospitalization; duration of antibiotic therapy.
Frailty assessment
Frailty was outlined by FI-Lab for this investigation. Following prior investigations, we constructed FI-Lab based on 44 laboratory variables evaluated from a fasting blood sample, including routine blood tests, blood biochemistry tests, and coagulation tests [8, 17] (Supplementary Table S1). Consistent with a previous study, we required at least 70% or 31 of the 44 variables to generate a valid FI-Lab score [9]. The cut-off points of the FI-Lab were robust/non-frail (< 0.2), pre-frail (0.2–0.35), and frail (≥ 0.35), according to earlier investigations [18, 19]. Furthermore, we also analyzed the FI-Lab score as a continuous variable.
Endpoints and follow-up
The primary endpoint was all-cause mortality. The secondary endpoint was the length of hospital stay, antibiotic therapy duration and in-hospital mortality. Patients were followed up since the date of CAP admission. We obtained the information from electronic medical records, and conducted telephone interviews with patients for whom lacked system information, and the death information includes the status of survival and the time of death until January 1, 2022.
Statistical analysis
Continuous data are expressed as a median with an interquartile range (25th to 75th percentiles), while categorical data are expressed as n (%). One-way ANOVA were performed to evaluate differences among groups. The chi-square test was used to compare proportions among groups. FI-Lab scores were evaluated as a categorical variable (robust, pre-frailty and frailty). Multiple linear regression was performed to assess the associations of FI-Lab with the length of hospital stay and duration of antibiotic therapy. Univariable Cox proportional regression evaluated the association between FI-Lab (categorical and continuous) and plausible confounding variables with in-hospital mortality and all-cause mortality. The variables based on a threshold p-value < 0.05 in the univariable analysis were considered in the multivariable Cox proportional regression analysis and a stepwise method was used. Time-to-event data are presented graphically using Kaplan–Meier curves. Log-rank tests were used to compare survival between groups. The binary Logistic regression model was used to predict the probability of death. The predictive accuracy of the indexes was validated using receiver operating characteristic (ROC) and quantified by the area under the curve (AUC) and 95% CIs. The SPSS 22.0, R version 4.1.2, and Prism 8 were applied for all statistical analyses and plots. The statistical significance was set as two-tailed with p at < 0.05.
Results
Patient characteristics
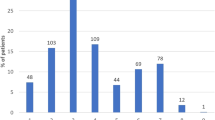
A cohort of 1164 older patients was finally included in this study by enrollment and exclusion criteria (Fig. 1). Among the patients, frail and pre-frail patients were older than robust patients (median age 77.0 vs. 77.0 vs. 71.0, p < 0.001). Robust patients had more female than pre-frail and frail groups (52.1% vs. 39.0% vs. 29.1%, p < 0.001). The inflammation-related indicators hs-CRP and PCT were significantly higher in the frail group than in the pre-frail or robust group (67.6 vs. 30.0 vs. 5.0, p < 0.001, 0.39 vs. 0.10 vs. 0.08, p < 0.001). Patients in the frail and pre-frail groups suffered more number of chronic diseases (aCCI score, 6 vs. 5 vs. 4, p < 0.001) and a higher burden of disease (CURB-65 score, 2 vs. 1 vs. 1, p < 0.001) than in the robust group. Smoking and drinking history did not differ significantly within groups (Table 1).
Frailty and short-term outcomes
We observed a longer duration of antibiotic therapy and increased hospital stay among frail and pre-frail patients compared to robust patients (11.0 vs. 9.0 vs. 7.0 days, p < 0.001, 12.0 vs. 11.0 vs. 8.0 days, p < 0.001; Table 1).
In the multiple linear regression analysis, after adjustment for confounding variables, frailty was independently associated with prolonged antibiotic treatment (p = 0.037; Supplementary Table S2), while pre-frail and frail groups were independently associated with longer inpatient days (p < 0.05 for both; Supplementary Table S3). As continuous variables, the FI-Lab score was independently associated with a longer duration of antibiotic therapy and increased length of hospital stay after adjusting for confounding factors (p = 0.021, Supplementary Table S2; p < 0.001; Supplementary Table S3).
The risk of in-hospital mortality was dramatically and independently increased in frail patients (HR = 5.01, 95% CI = 1.51–16.57, p = 0.008) but not pre-frail patients (HR = 2.87, 95% CI = 0.86–9.63, p = 0.088) compared to robust patients(Supplementary Table S4).
Mortality according to FI-Lab
During a median follow-up of 33.9 months (interquartile range: 32.8 to 35.1 months), 408 (35.1%) patients died (Table 1). The risk of all-cause mortality was dramatically increased in frail patients (HR = 6.81, 95% CI = 4.64–10.00, p < 0.001) and pre-frail patients (HR = 2.86, 95% CI = 1.90–4.30, p < 0.001) compared to robust patients. The prognostic role of frailty and pre-frailty for all-cause mortality were still significant after adjusting for potential confounding variables (HR = 3.61, 95%CI = 2.41–5.40, p < 0.001; HR = 2.02, 95% CI = 1.34–3.05, p = 0.001; respectively, Table 2). Equally, as continuous variables, after adjusting for confounding factors, the increment of the FI-Lab score was associated with an increased risk of mortality (adjusted HR per 0.10 increment in score 1.58, 95% CI 1.36–1.83; Table 3).
Figure 2 shows the survival curves of the study population according to their FI-Lab-based frailty status, and the curves differ significantly among the three groups (log-rank p < 0.001).
Given that the CURB-65 score is an index of severity for pneumonia, we compared the FI-Lab to CURB-65 for the prediction of death after CAP hospitalization. The FI-Lab score outperformed the CURB-65 at predicting all-cause mortality, as was seen by the ROC curve (AUC 0.75 vs. 0.66, p < 0.001; Fig. 3a). For mortality risk prediction, the FI-Lab score provided a significant incremental prognostic value on the CURB-65 score (AUC 0.77 vs. 0.66, p < 0.001; Fig. 3b).
Discussion
As defined by FI-Lab, frailty is common in older patients with CAP and is associated with a poor prognosis regardless of the CURB-65, aCCI, and other risk factors. With FI-Lab-based frailty provided a significant increase in the statistical accuracy of the CURB-65, frailty may be a critical, potentially modifiable risk and therapeutic target in older patients with CAP.
The first issue that should be evaluated is the prevalence of frailty. Based on the FI-Lab scores, 47.3% of our study’s elderly patients with CAP were labeled as frailty, and 33.9% were pre-frailty. Few studies have analyzed the prevalence of frailty in older patients with CAP. Luo et al. [20] reported that 66.8% of elderly patients with CAP were frail, using the Fried frailty phenotype in a cohort of 256 patients ages ≥ 65 years. However, clinical physicians are not aware of the prevalence of frailty. Despite its increasing importance, frailty is often not recognized and untreated. Accordingly, the first lesson that can be drawn from our study is the need to screen for frailty in older patients admitted for CAP. The five most commonly used methods for the assessment of frailty were CSF, FI, frailty phenotype, frail scale, EFS, and FI-lab was one of FI [21]. The FI-Lab scores analyzed are simple to calculate and useful to identify patients at risk for frailty. Frailty was more prevalent in men in our study, which is consistent with previous studies [8, 22]. However, most studies reported that women were more likely to be frail than men, even though women typically live longer [23, 24]. This phenomenon might be attributed partly to the frailty assessments being based on comprehensive geriatric assessments, which may not include all factors affecting life expectancy in older people [23]. In addition, we found that frail patients had significantly older age, greater hs-CRP and PCT, more comorbidities, and higher CURB-65 scores.
The second point to highlight is the relationship between FI-Lab-based frailty and short-term outcomes, including prolonged antibiotic treatment duration, longer length of stay and in-hospital death. We found that, regardless of clinical variables, frailty was still associated with adverse clinical events. This is consistent with Ellis et al. [11], who reported that higher CFS and FI-Lab scores were associated with more days in hospital. The FI-Lab can assist in identifying complex older adults at hospital admission who have accumulated multiple health deficits and are at an increased risk of adverse outcomes.
The third aspect of remarking is the relationship between frailty and all-cause mortality. Investigations have shown that high and moderate FI-LAB scores were associated with worse in-hospital and post-hospital outcomes, and FI-LAB can stratify older adults at increased risk of death alone [25], we proved this. According to a study using a large general older population hospitalized for pneumonia, frailty, measured by the Hospital Frailty Risk Score, was associated with mortality [26]. A strong relation between mortality and FI-Lab-based frailty was discovered in another investigation among acutely admitted older medical patients [12]. We found that, regardless of CURB-65, aCCI, and other risk variables, death in older CAP patients was independently influenced by FI-Lab-based frailty. CURB-65 scores were used for patients with pneumonia to predict mortality. Consistent with a prior study [13], we found that the FI-Lab combined with CURB-65 largely improved death prediction compared with CURB-65 alone. Several factors may explain the relationship in our study. Firstly, frailty represents the accumulation of cellular, tissue, and organ deficits damaged at those levels but not removed or repaired [9, 27]. The highest FI-Lab score with the significantly decreased survival point to the lethality of clinical deficits. Secondly, FI-Lab represents a more accurate and objective assessment than CGA-based frailty indices when predicting patient mortality [8, 9, 28].
All these findings strongly support the need for physicians to integrate in their daily practice the identification of frailty. Screening older patients with CAP for frailty might identify patients at high risk of adverse clinical outcomes, which might benefit from secondary prevention programs to improve their prognosis. Various multidisciplinary strategies have been developed to help prevent and treat frailty, including lifestyle changes, physical activities, and nutritional support [29, 30]. Clinicians should stay abreast of the most recent scientific evidence to provide helpful and practical patient guidance. The intervention should begin during CAP hospitalization because of the patient’s greater vulnerability to change in that period and also continue even after discharge. Meanwhile, preventing frailty to avoid elderly patients with CAP from experiencing a decline in their functional status and general health may be even more critical. Well-designed and well-executed future studies are needed to arrive at a reasonable evaluation of the impact of an intervention on frailty and CAP.
Our study has several limitations. First, this is a single-center, retrospective cohort study with a limited sample size and inevitable selection bias. Second, we did not compare the prognostic value of FI-Lab with other comprehensive frailty assessments, such as the physical frailty phenotype and the FI of accumulative deficits complex. This is relevant because frailty is a complicated issue, especially in older adults, because of various etiologies and determinants. Confirmation of our findings by more researchers and in other countries with various health care and social systems would be welcome.
Conclusions
Frailty assessed by routine laboratory data could allow clinicians to identify older patients with CAP at elevated risk for in-hospital and all-cause mortality, a longer hospital stay, and prolonged duration of antibiotics. Adequate assessment of frailty status can help improve the prognosis of elderly patients with CAP, selecting those who may benefit from support. This information can be translated into future trials to optimize the outcomes of older patients with CAP who are frail or pre-frail.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Rothberg MB. Community-Acquired Pneumonia. Ann Intern Med. 2022;175(4):ITC49–64.
Aliberti S, Dela Cruz CS, Amati F, Sotgiu G, Restrepo MI. Community-acquired pneumonia. Lancet. 2021;398(10303):906–19.
Cilloniz C, Rodriguez-Hurtado D, Torres A. Characteristics and Management of Community-Acquired Pneumonia in the Era of Global Aging. Med Sci (Basel). 2018;6(2):35.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. The Lancet. 2013;381(9868):752–62.
Linda P. Fried LF, Jonathan Darer,Jeff D. Williamson and Gerard Anderson: Untangling the Concepts of Disability, Frailty, and Comorbidity: Implications for Improved Targeting and Care. Journal of Gerontology: MEDICAL SCIENCES 2004, 59(3):255–263.
Dent E, Kowal P, Hoogendijk EO. Frailty measurement in research and clinical practice: A review. Eur J Intern Med. 2016;31:3–10.
Kojima G, Iliffe S, Walters K. Frailty index as a predictor of mortality: a systematic review and meta-analysis. Age Ageing. 2018;47(2):193–200.
Ritt M, Jager J, Ritt JI, Sieber CC, Gassmann KG. Operationalizing a frailty index using routine blood and urine tests. Clin Interv Aging. 2017;12:1029–40.
Susan E, Howlett MRR. Arnold Mitnitski and Kenneth Rockwood: Standard laboratory tests to identify older adults at increased risk of death. BMC Med. 2014;2014(12):171.
Blodgett JM, Theou O, Howlett SE, Rockwood K. A frailty index from common clinical and laboratory tests predicts increased risk of death across the life course. Geroscience. 2017;39(4):447–55.
Ellis HL, Wan B, Yeung M, Rather A, Mannan I, Bond C, Harvey C, Raja N, Dutey-Magni P, Rockwood K, et al. Complementing chronic frailty assessment at hospital admission with an electronic frailty index (FI-Laboratory) comprising routine blood test results. CMAJ. 2020;192(1):E3–8.
Klausen HH, Petersen J, Bandholm T, Juul-Larsen HG, Tavenier J, Eugen-Olsen J, Andersen O. Association between routine laboratory tests and long-term mortality among acutely admitted older medical patients: a cohort study. BMC Geriatr. 2017;17(1):62.
Park CM, Kim W, Lee ES, Rhim HC, Cho KH, Kim JH, Kim DH. Comparison of Frailty Index to Pneumonia Severity Measures in Older Patients With Pneumonia. J Am Med Dir Assoc. 2022;23(1):165–9.
Jeon K, Yoo H, Jeong BH, Park HY, Koh WJ, Suh GY, Guallar E. Functional status and mortality prediction in community-acquired pneumonia. Respirology. 2017;22(7):1400–6.
Iwai-Saito K, Shobugawa Y, Aida J, Kondo K. Frailty is associated with susceptibility and severity of pneumonia in older adults (A JAGES multilevel cross-sectional study). Sci Rep. 2021;11(1):7966.
Cao B, Huang Y, She DY, Cheng QJ, Fan H, Tian XL, Xu JF, Zhang J, Chen Y, Shen N, et al. Diagnosis and treatment of community-acquired pneumonia in adults: 2016 clinical practice guidelines by the Chinese Thoracic Society Chinese Medical Association. Clin Respir J. 2018;12(4):1320–60.
Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr. 2008;8:24.
Cohen HJ, Smith D, Sun CL, Tew W, Mohile SG, Owusu C, Klepin HD, Gross CP, Lichtman SM, Gajra A, et al. Frailty as determined by a comprehensive geriatric assessment-derived deficit-accumulation index in older patients with cancer who receive chemotherapy. Cancer. 2016;122(24):3865–72.
Wang Y, Zhang R, Shen Y, Su L, Dong B, Hao Q. Prediction of chemotherapy adverse reactions and mortality in older patients with primary lung cancer through frailty index based on routine laboratory data. Clin Interv Aging. 2019;14:1187–97.
Luo J, Tang W, Sun Y, Jiang C. Impact of frailty on 30-day and 1-year mortality in hospitalised elderly patients with community-acquired pneumonia: a prospective observational study. BMJ Open. 2020;10(10):e038370.
Dent E, Morley JE, Cruz-Jentoft AJ, Woodhouse L, Rodriguez-Manas L, Fried LP, Woo J, Aprahamian I, Sanford A, Lundy J, et al. Physical Frailty: ICFSR International Clinical Practice Guidelines for Identification and Management. J Nutr Health Aging. 2019;23(9):771–87.
Hao Q, Sun X, Yang M, Dong B, Dong B, Wei Y. Prediction of mortality in Chinese very old people through the frailty index based on routine laboratory data. Sci Rep. 2019;9(1):221.
Hubbard RE, Rockwood K. Frailty in older women. Maturitas. 2011;69(3):203–7.
Tembo MC, Holloway-Kew KL, Sui SX, Dunning T, Low ACH, Yong SJ, Ng BL, Brennan-Olsen SL, Williams LJ, Kotowicz MA, et al. Prevalence of Frailty in Older Men and Women: Cross-Sectional Data from the Geelong Osteoporosis Study. Calcif Tissue Int. 2020;107(3):220–9.
Ysea-Hill O, Gomez CJ, Mansour N, Wahab K, Hoang M, Labrada M, Ruiz JG. The association of a frailty index from laboratory tests and vital signs with clinical outcomes in hospitalized older adults. J Am Geriatr Soc. 2022;70(11):3163–75.
Kundi H, Wadhera RK, Strom JB, Valsdottir LR, Shen C, Kazi DS, Yeh RW. Association of Frailty With 30-Day Outcomes for Acute Myocardial Infarction, Heart Failure, and Pneumonia Among Elderly Adults. JAMA Cardiol. 2019;4(11):1084–91.
Mitnitski A, Song X, Rockwood K. Assessing biological aging: the origin of deficit accumulation. Biogerontology. 2013;14(6):709–17.
Rockwood K, McMillan M, Mitnitski A, Howlett SE. A Frailty Index Based on Common Laboratory Tests in Comparison With a Clinical Frailty Index for Older Adults in Long-Term Care Facilities. J Am Med Dir Assoc. 2015;16(10):842–7.
Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. The Lancet. 2019;394(10206):1376–86.
Lochlainn M Ni, Cox NJ, Wilson T, Hayhoe RPG, Ramsay SE, Granic A, Isanejad M, Roberts HC, Wilson D, Wilson D, Welch C, et al. Nutrition and Frailty: Opportunities for Prevention and Treatment. Nutrients. 2021;13(7):2349.
Acknowledgements
This work has not been previously published and is not being considered for publication elsewhere, in whole or in part, in any language.
Funding
This study was supported by grants from the National Key R&D Program of China (No. 2018YFC2002100, 2018YFC2002102), the National Natural Science Foundation of China (Nos. 81871115), the Natural Science Foundation of Jiangsu Province (No. BK20211377), the Cadre Health Care Research Project of Jiangsu Province (No. BJ20018), the Natural science research project of colleges and universities in Jiangsu Province (No. 20KJB320002), the Outstanding Young and Middle-aged Talents Support Program of the First Affiliated Hospital with Nanjing Medical University, the Six Talent Peaks Project in Jiangsu Province (No. 2018-WSN-003). All the above grants had no role in the collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
HZ designed the study, interpreted the data, and drafted the manuscript. JT contributed to the statistical analysis. QS and ML collected the epidemiological and clinical data, interpreted the data, and drafted the manuscript. JT, KW, WZ and PH contributed to the data analysis and interpretation and revised the manuscript. JW and BC designed the study, interpreted the data, and revised the manuscript. All authors reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the First Affiliated Hospital of NJMU (2020-SR-072). This study was conducted in accordance with the Declaration of Helsinki. Informed consent for telephone follow-up in this study was provided verbally by all successfully followed subjects, as it was not feasible to obtain written consent during telephone follow-up, which was also approved by the Ethics Committee of the First Affiliated Hospital of NJMU (2020-SR-072).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary Table S1. Laboratory variables for frailty index. Supplementary Table S2. Association of frailty and duration of antibiotic therapy by multiple liner regression analyses. Supplementary Table S3. Association of frailty and length of stay by multiple liner regression analyses. Supplementary Table S4. Risk factors associated with in-hospital death (FI-Lab as categorical variable).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhao, H., Tu, J., She, Q. et al. Prognostic significance of frailty in hospitalized elderly patients with community-acquired pneumonia: a retrospective cohort study. BMC Geriatr 23, 308 (2023). https://doi.org/10.1186/s12877-023-04029-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04029-3