Abstract
Background
Population aging has become an escalating issue in China resulting in increasing healthcare demand. Smart senior care has the potential to help older adults live independently and relieve the pressure of healthcare including home-based care. This study aimed to explore Chinese older adults’ preferred access models and service content of smart senior care and factors affecting their willingness to choose smart senior care.
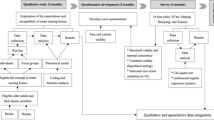
Methods
This was a cross-sectional study. A total of 760 community-dwelling older adults from Xuzhou, China were included in this study. Their demographics, family support, health status, smart senior care use, and willingness to choose smart senior care were collected. The Chi-square test was used for single factor analysis of each variable. The statistically significant variables were included in the logistics regression model to analyze factors influencing older adults’ willingness to choose smart senior care. The chi-square goodness of fit test was used to analyze the preferred content and access models of smart senior care; the Bonferroni method was used to correct the results.
Results
The finding indicated that participants’ age, number of children, frequency of children visiting parents, adequate senior care, self-reported health, chronic diseases, smartphone use, and attitude toward smart senior care were significantly associated with their willingness to choose the smart senior care (p < 0.05). For smart senior care access models, participants preferred the remote monitoring model, telephone call model, and the community site model over the health smart home model and the smart application platform model. There was no statistical difference among these three preferred access models (p’ > 0.005). Regarding service content, participants desired medical care service the most (p’ < 0.005).
Conclusions
Chinese older adults’ willingness to choose smart senior care is affected by personal, family, health, and other factors. To develop China’s senior care, we should consider their demand and preference for smart senior care. It is important to enrich the content of smart senior care, especially on medical care services, and maintain the dynamic balance between supply and demand using a diverse supply approach.
Similar content being viewed by others
Introduction
The increasing proportion of older adults worldwide is a problem now and an inevitable challenge for the future. It poses challenges to economics, people’s livelihood, and social welfare. This issue is particularly prominent in China, a country with improved life expectancy and lowered fertility [1, 2]. China has become an aging society since 1999. In 2021, there were 264 million people aged 60 years or above in China, representing 18.7% of the total population. It is predicted that China will be a super-aged society in 2050, with older adults occupying 34.1% of the total population [3, 4]. With the population aging, the demand for home care and chronic disease management increases [5]. To meet the increasing healthcare demand of older adults in China, the Chinese government has issued the “9073” elderly-care policy and indicated that senior care in China should consist of 90% home care, 7% community care, and 3% institutional care [6]. Therefore, meeting older adults’ home-based senior care needs has become a strategic priority in China.
In recent years, the fourth scientific and technological revolution characterized by the Internet of Things (IoT), Information Technology, Big Data, and Cloud Computing has significantly promoted China’s aging industry [7]. At the same time, a series of policies have been issued to link the internet industry with the aging industry. In this context, the concept of smart senior care emerged and was seriously regarded by the government [8].
Smart senior care refers to the use of information and scientific technology, including health records, medical interventions, and home care to improve the quality of life for older adults [9, 10]. Specifically, through a variety of sensors and network systems remotely monitoring older adults’ daily life, their activities will be recorded and transmitted to healthcare institutions or third-party service companies. Then clinicians can provide online or onsite healthcare interventions including home care assistance [11]. The application of smart senior care has the potential to significantly improve the independence, safety, and quality of life of community-dwelling older adults. This is especially important during the COVID-19 pandemic, when older adults stay home longer and their disconnection from external services increases [12]. Therefore, scientifically developing smart senior care in China is critical.
Through literature review, we found that developed countries have formed relatively large-scale and well-established smart senior care systems [13,14,15]. In general, their smart senior care models can be divided into five categories: (1) In the remote monitoring model, wearable sensors are used to measure various health parameters of older adults [16, 17]. (2) In the health smart homes model, various forms of assisted living are established to monitor older adults’ daily activities, health status, home environment, assisted mobility, and safety [18, 19]. (3) In the smart application platform or telephone call model, older adults select smart senior services through mobile applications or telephone calls. Then healthcare institutes or third-party service companies can provide online or offline services accordingly [20, 21]. (4) In the community site model, older adults register for services at community stations that provide long-term supervision on disease prevention and emergency treatment [22] (5). In the artificial intelligence model, humanoid robots are used to take care of older adults [23, 24]. All these models allow older adults to live in their familiar environment for as long as possible.
While the development of smart senior care is dominated by technology, evidence emphasizes that it is important to consider older adults’ willingness and demand to choose smart senior care [25]. Lifestyles, health knowledge, cost of services, health status, and safety are likely to be factors influencing the willingness of older adults to choose smart senior care. World Health Organization (WHO) has also proposed to comprehensively consider the dimensions of “health”, “participation”, and “security” to improve the quality of life of older adults and achieve active aging [26]. However, the results of observational and qualitative studies on the influencing factors of older adults’ willingness to choose smart senior care were inconsistent [1, 27, 28]. To the best of our knowledge, there is no cross-sectional study on older adults’ willingness to choose smart senior care in China. Furthermore, two reviews proposed the importance of expanding the content of smart senior care and building a smart senior care access model based on the willingness of older adults [29, 30]. Thus, to promote the development of smart senior care in China, understanding older adults’ willingness to choose smart senior care is essential. Therefore, this study aimed to explore Chinese older adults’ preferred access models and service content of smart senior care and factors affecting their willingness to choose smart senior care. The findings of this study will provide implications for policymakers and providers to better provide smart senior care and meet the growing healthcare demand of older adults in China.
Methods
Sampling and inclusion criteria
We used stratified cluster sampling to recruit community-dwelling older adults in Xuzhou, China. Eleven counties and districts in Xuzhou were stratified into three regions based on their economic development and population size. In each region, three communities were randomly selected. The number of distributed questionnaires was proportional to the population size of each selected community. The inclusion criteria were people who (1) were aged 60 or older, (2) were living in communities at the time of the survey; (3) could have rational conversations with researchers. The exclusion criteria were people with cognitive impairment such as dementia or limited vernal ability such as speech disorders. The survey was conducted from June to October 2021. A pilot study was conducted for 1 week prior to the commencement of the study to revise the questionnaire. Two researchers distributed the survey in the communities. To achieve a high response, face-to-face interviews were used to collect the data. A total of 768 participants were recruited, and eight incomplete questionnaires were excluded. Finally, 760 valid questionnaires were collected.
Questionnaire design
Since there is currently no existing validated survey on older adults’ willingness to choose smart senior care, a structured questionnaire was developed to obtain relevant information. To measure older adults’ willingness to choose smart senior care, the question of “Do you have the willingness to choose smart senior care?” was used. The response was a binary variable (yes or no). Meanwhile, multiple-choice questions were used to investigate participants’ preferred access models and service content of smart senior care. Five categories of smart senior care access models were identified, guided by the current literature [16,17,18,19,20,21,22, 27, 28], and were incorporated into the questionnaire, including the remote monitoring model, the health smart homes model, the smart application platform model, the telephone call model, and the community site model. Moreover, we also included questions on five areas of smart senior care service content, including medical care service, home care service, social entertainment service, meal delivery service, and psychological counseling services in the questionnaire.
Factors expected to influence older adults’ willingness to choose smart senior care were summarized in Table 1. In addition to the demographic characteristics of older adults, we added additional independent variables based on the three dimensions of the theory of active aging, including “security”, “health”, and “participation” [26]. 1) Demographic characteristics included age (60–69, 70–79, and 80+), gender (male and female), registered residence (rural and urban), years of education (no education, 1–6 years, and 7+ years), pre-retirement occupation (have a formal job or others). 2) Security dimension included national health insurance enrollment (urban employer medical scheme, urban resident medical scheme, or new rural cooperative medical scheme), monthly income in RMB (< 1000, 1000-1999, 2000-2999, 3000-3999, and more than 4000), live with a spouse (yes or no), number of children (One child, two children, three children, or four or more children), frequency of children visiting parents (every day, weekly, semimonthly, or monthly+), primary caregiver (spouse, children, self, or others), and perceived adequacy of senior care received (yes or no). 3) Health dimension included self-reported health (bad or good), hospitalization within 1 year (yes or no), any chronic diseases (yes or no), frequency of physical examination (half a year, annually, biennial, or more than 2 years), and any disability in instrumental activities of daily living (IADLs) (yes or no). IADLs were measured based on eight self-reported activities: (a) visiting neighbors, (b) shopping, (c) cooking, (d) washing clothes, (e) walking 1 kilometer, (f) lifting 5 kg, (g) crouching, and standing up three times, and (h) taking public transportation. 4) Participation dimension covered the key factors of older adults’ participation in smart senior care, included smartphone use (yes or no), familiarity with smart senior care (know very well, heard of, or never heard of), and attitude towards smart senior care (supportive or not). Smartphone was defined as a type of mobile phone with an independent operating system and running space where users can install applications developed by third-party service providers and achieve wireless network access through mobile communication networks [31].
Procedure and statistical analysis
The study proposal was ethically reviewed and approved by the Human-related Research Ethical Committee of the Affiliated Hospital of Xuzhou Medical University (XYFY2021-KL157–01). When consenting participants for enrollment, we explained the purpose of the study to them. The confidentiality of data storage was also emphasized, and their written informed consent was obtained. After the questionnaire was returned to us, we confirmed on site if there were any questions that participants did not understand and checked with them. Two researchers imported the data into SPSS 25.0 statistical software. Missing values for a small number of questionnaires were handled by multiple imputations by SPSS 25.0 software.
The Chi-square test was used to examine the correlations between the independent variables and dependent variable. Then, logistic regression was constructed to analyze factors affecting older adults’ willingness to choose smart senior care. The Hosmer-Lemeshow test was applied to assess the goodness of fit of the logistic regression model [32]. The null hypothesis H0 (the model provides a good fit) and alternative hypothesis H1 (the model does not fit the data) were tested, respectively. We also performed variance inflation factor (VIF) calculations of the independent variables to determine whether multicollinearity existed among the variables. Finally, we used count data to calculate participants’ preferences on the smart senior care access models and service content. The chi-square goodness of fit test was used to test whether there were statistical differences among different groups. Due to the increased risk of a type I error when making multiple statistical tests, the Bonferroni correction method was adopted when we examined the difference in probability (p’) values of multiple groups [33, 34]. All statistical tests were two-sided, with p < 0.05 considered statistically significant.
Results
Characteristics of the participants
Participants’ characteristics were reported in Table 2. Most participants aged between 70 and 79 (41.7%) were females (51.2%), rural residents (58.3%), and did not have a formal job before retirement (55.4%). The participants were poorly educated- only 32.4% had over 7 years of education. On the type of medical insurance, most participants (42.2%) used the new rural cooperative medical system (NRCMS). Most participants (30.1%) had a monthly income between 2000 and 2999 RMB (about 292.61 ~ 438.76 USD), and 21.4% of the participants had a monthly income of less than 1000 RMB (about 146.30 USD).
Regarding family support, most participants lived with a spouse (79.6%). One-third of the participants’ primary caregivers (36.3%) were their spouses, followed by the participants themselves (32.0%). One-third of the participants (36.6%) had two children, and 33.9% could see their children daily. Over half of the participants could not get adequate senior care (65.4%). In addition, most participants (60.4%) were in good health. One-third of the participants (30.4%) were hospitalized in the past year. More than half of the participants (56.1%) had chronic diseases or any IADL disability (64.7%). About half of the participants (42.8%) had an annual physical examination.
Regarding the participation dimension, more than half of the participants (58.0%) used a smartphone. After the researcher explained the purpose of the study and the content of smart senior care, 90.3% of the participants were willing to choose smart senior care. However, many participants (63.8%) had never heard of smart senior care before this study.
The logistic regression analysis result
Table 2 presented the results of correlation analysis between the independent variables and dependent variable. We found that age, registered residence, years of education, pre-retirement occupation, type of national health insurance enrollment, monthly income, number of children, frequency of children visiting parents, perceived adequacy of senior care received, self-reported health, hospitalization within a year, any chronic diseases, physical examination frequency, smartphone use, familiarity with smart senior care, and attitude towards smart senior care were significantly related the participants’ willingness to choose smart senior care. We included these statistically significant correlated variables in the logistic regression model. The result displayed that the p-value of the Hosmer-Lemeshow test exceeded 0.05 for the models. Thus, this binary logistic regression model fits well with no statistical deviation between the agreement fitting model and the actual model [35]. And the VIF values were all less than 10. Thus, there was no multicollinearity among the independent variables.
The logistic regression results (Table 3) revealed that participants’ age, number of children, frequency of children visiting parents, perceived adequacy of senior care, self-reported health, chronic diseases, smartphone use, and attitude towards smart senior care were found to be significantly associated with the participants’ willingness to choose the smart senior care (p < 0.05). Specifically, the participants who were over 80 years old (OR = 0.457), had more than one child, had more child visiting time, and received adequate senior care (OR = 0.569) were less willing to choose smart senior care than the intra-group reference people. Moreover, the participants who had worse self-reported health (OR = 2.332), lived with chronic diseases (OR = 2.378), used smartphones (OR = 1.674), and were supportive of smart senior care (OR = 13.493) were more willing to choose smart senior care than the intra-group reference people.
The chi-square goodness of fit test results
Additional file 1: Supplement Table 1 showed the chi-square goodness of fit test results of the five smart senior care access models. The results showed that the remote monitoring model was the most popular access model among the participants (selected by 448 participants). The least popular access model was the smart application platform model (selected by 278 participants). After Bonferroni correction, we found that the remote monitoring model, the telephone call model, and the community site model were more popular among participants than the other two models. In addition, there was no statistical difference among the three access models. The health smart homes model had a statistical difference from the remote monitoring model. Still, there was no statistical difference between the health smart homes model, the telephone call model, and the community site model. The smart application platform model was the least selected and statistically different from other access models. Figure 1 showed a comparison of the participants’ willingness to choose the five access models.
Additional file 1: Supplement Table 2 showed the chi-square goodness of fit for the five smart senior care service types. After Bonferroni correction, we found that medical care services were the most popular service content (selected by 513 participants) with a statistical difference from other types of service content. Four hundred twenty-three participants chose home care services; 364 chose social entertainment services, and there was no statistical difference between them. Psychological counseling service was the least popular (selected by 251 participants), and there was no statistical difference between it and meal delivery service. Figure 2 showed a comparison of the participants’ willingness to choose the five service contents.
Discussion
To the best of our knowledge, there are few cross-sectional study examining older adults’ demands and willingness to choose smart senior care in China. In this study, we found that the health of older adults in Xuzhou, China was poor, and their quality of life was not high. Our finding on older adults’ health status was dissimilar to the findings of the Chinese Longitudinal Healthy Longevity Survey (CLHLS) [36, 37]. While 56.1% of the participants suffered from chronic diseases in our study, the latter was 60.53%. While more than 60% had varying degrees of IADL disorders in our study, the latter was 49.91%. One reason for this discrepancy may be that our participants had a more advanced age than those in the Chinese Longitudinal Healthy Longevity Survey [38]. The family structure change, the anticipated increasing burden of chronic disease, and the possible attenuation of filial care increased demand for home-based care in China. At the same time, we found that the demand for information services for older adults was growing. 58.0% of the participants used smartphones, which is higher than what the China Internet Network Information Center (CNNIC) reported in December 2021 (43.2%) [39]. The difference may be due to the different samples in the two studies. In addition, as reported in the CNNIC, 80.8% of older adults who use mobile phones will actively seek Internet lifestyle care services [39]. And in this study, 90.3% of participants supported smart senior care. This condition created an excellent opportunity for developing smart senior care in China.
In terms of the participants’ willingness to choose smart senior care, we found that older adults’ willingness to choose smart senior care was affected by many aspects. Firstly, compared with younger older adults, the participants over 80 years old had less willingness to choose smart senior care. This may be due to the influence of traditional culture and their limited ability to accept new things, resulting in their lowered willingness to choose smart senior care. Thus, companies should consider the older adults’ age when promoting smart senior care. Compared with older adults with advanced age, younger older adults are more likely to accept smart senior care, are the main consumers of smart senior care, and have more demands for smart senior care.
Secondly, regarding the living security dimension, the number of children, frequency of children visiting parents, and perceived adequacy of senior care received influenced participants’ willingness to choose smart senior care. Specifically, the participants with only one child, who were visited less frequently by their children, and did not receive adequate senior care at home were more willing to choose smart senior care than those with more than one child. Gordana Dermody et al. have also indicated that family support affects older adults’ willingness to choose smart senior care. Older adults with less family support were more likely to receive smart senior care [27]. It is not hard to tell that the “4 + 2 + 1″ family model (A family unit that consists of four old adults, two adults, and one child) due to the one-child policy poses severe challenges to China’s current home care situation [40, 41]. Older adults who did not receive adequate living security were more willing to choose smart senior care. Therefore, when implementing smart senior care, we should pay special attention to older adults who live alone or have empty nesters. In addition, the government should develop customized technology solutions for older adults with low living security to meet their healthcare need.
Thirdly, the participants with poor self-reported health or chronic conditions were more willing to choose smart senior care. In another study in South Korea, researchers reported that older adults’ health was related to their willingness to choose smart senior care [1]. Older adults have paid more attention to their health with improved living standards. Those with poor physical conditions have become willing to promote their health through the new healthcare model. Thus, we should develop telemedicine to meet older adults’ healthcare demands. The government could also consider incorporating smart senior care into residents’ medical insurance to reduce the burden of family health care.
Fourthly, some factors in the participation dimension also affect older adults’ willingness to choose smart senior care. The results showed that the participants who have used smartphones were more willing to choose smart senior care. Yuanyuan Cao et al. also reported that older adults with rich experience using smart products were more likely to choose smart senior care [28]. Thus, improving older adults’ information technology levels is another crucial task at present. We can try to let older adults experience the convenience of smart senior care. In addition, through digital training or intelligent experience, we can help them better use smart products.
Concerning the smart senior care access models, we found that older adults preferred the remote monitoring, telephone call, and community site access models over the smart application platform model or health smart homes model. On the one hand, it is related to the fact that participants could not use smart products or were not proficient in using them. On the other hand, older adults may worry about their limited learning ability, resulting in poor, smart product operation. Nthubu Badziili has also indicated that more consideration should be given to the interaction among users, sensors, and data when integrating smart products into the home environment of older adults [30]. Therefore, to develop smart senior care in China, we must overcome the “digital divide” problem among older adults. Companies offering smart senior care should implement customer-oriented strategies and take the initiative to achieve user-friendliness for older adults. Eventually, we hope to promote the popularity of smart senior care and benefit older adults by optimizing their access to smart senior care.
On participants’ willingness for service content, we found that old adults’ smart senior care willingness for medical care services was highlighted. Majumder, Sumit et al. also pointed out the importance of medical care services in smart senior care [29]. Therefore, smart senior care should take advantage of information technology to ensure the supply of medical care service resources. Combined with the analysis results of the smart senior care access model, we can collect dynamic data such as vital signs by wearing wearable devices on older adults’ bodies and then monitor their physical state remotely. Of course, if we need to establish smart senior care base stations in communities, relevant staff should manage health records and track the life trajectories of older adults at home in the region. In addition, alarm-calling devices should be installed at home to facilitate old adults in need of timely contact with healthcare institutions. Through a series of measures, we will find a suitable way to develop smart senior care in China so that more old adults can understand and accept smart senior care.
Limitations
This study has some limitations. To start with, the sample size of this study is relatively small. Only 760 older adults were included in the study, and all were from Xuzhou, China. Thus, our study has limited generalizability. In addition, we acknowledge that some variables, such as health status, were assessed using self-report. Future studies are needed to expand the scope of the survey to make the study population more representative and use validated questionnaires to assess the variables.
Conclusions
The findings of this study indicate that older adults’ willingness to choose smart senior services was affected by their personal, family, health, and other factors. Thus, we should consider the characteristics of older adults and provide them with tailored smart senior care. At the same time, we should adopt diverse supply methods, expand service content, and utilize the latest technologies, such as the Internet of Things, big data, and cloud computing, to introduce smart senior care to older adults and their family members. With the support and cooperation of all sectors of society, we hope to gradually establish smart senior care suitable for China.
Availability of data and materials
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Abbreviations
- IoT:
-
Internet of Things
- WHO:
-
World Health Organization
- IADL:
-
Instrumental activities of daily living
- UEMS:
-
Urban Employer Medical Scheme
- URMS:
-
Urban Resident Medical Scheme
- NRCMS:
-
New Rural Cooperative Medical System
- CLHLS:
-
Chinese Longitudinal Healthy Longevity Survey
- CNNIC:
-
China Internet Network Information Center
References
Yu J, de Antonio A, Villalba-Mora E. Older adult segmentation according to residentially-based lifestyles and analysis of their needs for smart home functions. Int J Environ Res Public Health. 2020;17(22):8492.
Hu Y, Wang J, Nicholas S, et al. The sharing economy in China's aging industry: applications, challenges, and recommendations. J Med Internet Res. 2021;23(7):e27758.
National Bureau of Statistics. Bulletin of the Seventh National Population Census. Available at: http://www.stats.gov.cn/tjsj/tjgb/rkpcgb/qgrkpcgb/202106/t20210628_1818824.html. Accessed 11 May 2021.
World Health Organization. World report on ageing and health. Geneva: WHO Press; 2015.
Zhang X, Dupre ME, Qiu L, et al. Urban-rural differences in the association between access to healthcare and health outcomes among older adults in China. BMC Geriatr. 2017;17(1):151.
National Health Commission of the People's Republic of China. Available at: http://www.nhc.gov.cn/xcs/s3574/202104/0c1cf92f2b7b4cfe890234a1c3d5593f.shtml. Accessed 20 Mar 2022.
Wang B, Xu L. Construction of the "internet plus" community smart elderly care service platform. J Healthc Eng. 2021;2021:4310648.
Meng Q, Hong Z, Li Z, et al. Opportunities and challenges for Chinese elderly care industry in smart environment based on Occupants' needs and preferences. Front Psychol. 2020;11:1029.
Kang HJ, Han J, Kwon GH. Determining the intellectual structure and academic trends of smart home health care research: Coword and topic analyses. J Med Internet Res. 2021;23(1):e19625.
Sánchez VG, Taylor I, Bing-Jonsson PC. Ethics of SMART house welfare technology for older adults: a systematic literature review. Int J Technol Assess Health Care. 2017;33(6):691–9.
Reeder B, Chung J, Lyden K, et al. Older women's perceptions of wearable and smart home activity sensors. Inform Health Soc Care. 2020;45(1):96–109.
Kawamura K, Kamiya M, Suzumura S, et al. Impact of the coronavirus disease 2019 outbreak on activity and exercise levels among older patients. J Nutr Health Aging. 2021;25(7):921–5.
Shen J, Naeim A. Telehealth in older adults with cancer in the United States:the emerging use of wearable sensors. J Geriatr Oncol. 2017;8(6):437–42.
Costa A, Rincon JA, Carrascosa C, et al. Activities suggestion based on emotions in AAL environments. Artif Intell Med. 2018;86:9–19.
Lee LN, Kim MJ. A critical review of smart residential environments for older adults with a focus on pleasurable experience. Front Psychol. 2019;10:3080.
Banbury A, Nancarrow S, Dart J, et al. Adding value to remote monitoring: co-design of a health literacy intervention for older people with chronic disease delivered by telehealth - the telehealth literacy project. Patient Educ Couns. 2020;103(3):597–606.
Evans J, Papadopoulos A, Silvers CT, et al. Remote health monitoring for older adults and those with heart failure: adherence and system usability. Telemed J E Health. 2016;22(6):480–8.
Nagapuri S, Maeder AJ, Williams PAH. Health smart homes: user perspectives. Stud Health Technol Inform. 2019;266:127–35.
Maeder AJ, Williams PAH. Health smart homes: new challenges. Stud Health Technol Inform. 2017;245:166–9.
Liu N, Yin J, Tan SS, et al. Mobile health applications for older adults: a systematic review of interface and persuasive feature design. J Am Med Inform Assoc. 2021;28(11):2483–501.
Paiva JOV, Andrade RMC, de Oliveira PAM, et al. Mobile applications for elderly healthcare: a systematic mapping. PLoS One. 2020;15(7):e0236091.
Gaines JM, Poey JL, Marx KA, et al. Health and medical services use: a matched case comparison between CCRC residents and national health and retirement study samples. J Gerontol Soc Work. 2011;54(8):788–802.
Klamroth-Marganska V. Stroke rehabilitation: therapy robots and assistive devices. Adv Exp Med Biol. 2018;1065:579–87.
Koutentakis D, Pilozzi A, Huang X. Designing socially assistive robots for Alzheimer's disease and related dementia patients and their caregivers: where we are and where we are headed. Healthcare (Basel). 2020;8(2):E73.
Zhang Q, Li M, Wu Y. Smart home for elderly care: development and challenges in China. BMC Geriatr. 2020;20(1):318.
Report of the World Health Organization. Active ageing: a policy framework. Aging Male. 2002;5(1):1–37.
Gordana D, Roschelle F, Courtney G, et al. Factors influencing community dwelling older adults' readiness to adopt smart home technology: a qualitative exploratory study. J Adv Nurs. 2021;77(12):4847–61.
Yuanyuan C, Mojisola E, Caroline R, et al. Decision-making factors toward the adoption of smart home sensors by older adults in Singapore: mixed methods study. JMIR Aging. 2022;5(2):e34239.
Sumit M, Emad A, Moein N, et al. Smart homes for elderly healthcare-recent advances and research challenges. Sensors (Basel, Switzerland). 2017;17(11):2496.
Nthubu B. An overview of sensors, design and healthcare challenges in smart homes: future design questions. Healthcare (Basel, Switzerland). 2021;9(10):1329.
Jung LS, Joo CM, Hye YS, et al. Development and evaluation of smartphone usage management system for preventing problematic smartphone use. Digital health. 2022;8:20552076221089095.
Nattino G, Pennell ML, Lemeshow S. Assessing the goodness of fit of logistic regression models in large samples: a modification of the Hosmer-Lemeshow test. Biometrics. 2020;76(2):549–60.
Ranstam J. Multiple P-values and Bonferroni correction. Osteoarthritis Cartilage. 2016;24(5):763–4.
Armstrong RA. When to use the Bonferroni correction. Ophthalmic Physiol Opt. 2014;34(5):502–8.
Kramer AA, Zimmerman JE. Assessing the calibration of mortality benchmarks in critical care: the Hosmer-Lemeshow test revisited. Crit Care Med. 2007;35(9):2052–6.
Peking University Open Research Data. Available at: https://opendata.pku.edu.cn/dataverse/pku. Accessed 03 Apr 2020.
Xu H, Dupre ME, Danan G, et al. The impact of residential status on cognitive decline among older adults in China: results from a longitudinal study. BMC Geriatr. 2017;17(1):107.
People's Government of Jiangsu Province. Available at: http://www.jiangsu.gov.cn/art/2021/10/13/art_33718_10081138.html. Accessed 12 Dec 2021.
China Internet Network Information Center. Available at: http://www.cnnic.net.cn/hlwfzyj/hlwxzbg/. Accessed 21 Jul 2022.
Han WJ, Whetung T, Mao X, Roof O. Three generations: grandparental co-residence and child outcomes in China. Fam Process. 2020;59(3):1144–60.
Song Y. Losing an only child: the one-child policy and elderly care in China. Reprod Health Matters. 2014;22(43):113–24.
Acknowledgements
Not applicable.
Funding
The research was supported by the National Key R&d Program of China (2020 YFC2006600).
Author information
Authors and Affiliations
Contributions
QH conceived the study, and drafted the manuscript. YL and XT collected data, conducted data analysis, and SG, ZQ, AW and XW were involved in discussing earlier versions of the text. All authors participated in its design and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Human-related Research Ethical Committee of the Affiliated Hospital of Xuzhou Medical University (XYFY2021-KL157–01). All methods were performed in accordance with the Declarations of Helsinki. All participants were provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huang, Q., Li, Y., Wu, X. et al. The willingness and influencing factors to choose smart senior care among old adults in China. BMC Geriatr 22, 967 (2022). https://doi.org/10.1186/s12877-022-03691-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03691-3