Abstract
Objectives
Previous studies had reported that insulin resistance (assessed by estimated glucose disposal rate; eGDR) was associated with higher risk of cardiovascular events (CVD) in diabetes patients. The aim of present study was to investigate the potential association between eGDR and CVD in general population.
Methods
The China Health and Retirement Longitudinal Study with 8,267 individuals were included in analysis. Participants were divided into four subgroups according to eGDR quartile. Cox proportional hazards regression models were used to examine the associations of eGDR with CVD (stroke or cardiac events).
Results
During 6 years of follow-up, a total of 1,476 respondents experienced a CVD (494 stroke and 1,110 cardiac events). In multivariable-adjusted analyses, the corresponding hazard ratio (95% confidence intervals) for the highest eGDR versus lowest quartile of eGDR was 0.58(0.49–0.67) for CVD. Each 1-SD increase of eGDR was associated with 16% (HRs = 0.84; 0.79–0.88) decreased risk of CVD. There was also a significant linear association between eGDR and CVD (P for linearity < 0.001). Similar associations were also found between eGDR and stroke and cardiac events.
Conclusion
A higher eGDR (a measure of insulin resistance) was associated with a decreased risk of CVD, stroke and cardiac events in general Chinese population, suggesting that eGDR could be considered as a preferential predictor and treatment target of CVD. Future well-designed prospective clinical studies are needed to verify our findings and to assess the effect of eGDR interventions in CVD prevention and therapy.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is still the leading cause of mortality worldwide and responsible for 18.6 million deaths in 2019, which was estimated to account for 32.3% of all-cause global deaths [1,2,3]. Atherosclerosis is the major cause of CVD and stroke [4]. Insulin resistance and the ensuing hyperinsulinemia/hyperglycemia are crucial link between atherosclerosis and CVD [5,6,7]. Previous studies reported that preventing insulin resistance would prevent almost 40% of atherosclerotic disease regardless of hypertension, hyperlipidemia, hyperglycemia or obesity, involved in the insulin resistance state [8].
In clinic, the gold standard technique measuring insulin resistance is the euglycaemic hyperinsulinaemic clamp method [9], while the homeostasis model assessment of insulin resistance (HOMA-IR) is widely used as a valid surrogate of the gold standard [10]. However, the above detection methods were invasive and costly, and therefore not suitable for large-scale daily clinical use. In recent years, a validated score against the euglycaemic hyperinsulinaemic clamp based on the readily available clinical factors waist circumference, hypertension, and glycosylated hemoglobin A1c (HbA1c) was developed to estimate the glucose disposal rate (eGDR) in patients with type 1 diabetes and type 2 diabetes, which has been proven to have a high precision when compared to the euglycaemic hyperinsulinaemic clamp method [10, 11]. Several previous studies had investigated the utility of eGDR and results indicated this metric was significant associated with preclinical carotid atherosclerosis [10], coronary artery disease [12], stroke [13] and mortality [14] in individuals with type 1 diabetes (T1D) or type 2 diabetes (T2D). Evidence from a cross-sectional study also indicated that eGDR could improve the identification of prevalent ischemic heart disease in the Chinese rural general population [15]. However, whether grade of insulin resistance predicts CVD in general population is not well known.
In current study, we aimed to evaluate the association between insulin resistance (IR, assessed by eGDR) and risk of CVD (stroke or cardiac events) among middle aged and older Chinese adults based on the data from the China Health and Retirement Longitudinal Study (CHARLS).
Methods
Study population
CHARLS is an ongoing nationally representative and population-based study, that uses a multistage clustering sample method to select participants and conducted to collect a series of data regarding sociodemographic and lifestyle factors and health-related information in Chinese citizens aged 45 years or older [16, 17]. In CHARLS 2011, a total of 17,708 participants in 10,257 households were recruited from 150 counties or districts and 450 villages within 28 provinces in China. All participants were followed up every 2 years after the baseline survey [18]. The ethics application for collecting data on human subjects in CHARLS was approved by the Biomedical Ethics Review Committee of Peking University (IRB00001052-11,015), and performed in accordance with s the Declaration of Helsinki. Furthermore, all CHARLS participants provided written informed consent. The details of the CHARLS data are available at its website (http://charls.pku.edu.cn/en).
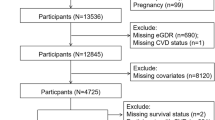
In current study, a total of 17,708 individuals were included in the baseline survey of around 450 basic communities from 28 provinces in China. The exclusion criteria were as follows: 1) individuals < 45 years old (N = 484); 2) individuals without complete information about waist circumference, hypertension and Hemoglobin A1c (HbA1c) (N = 7520); 3) individuals who reported stroke and cardiac events in baseline or lost to followed-up (N = 1437). Finally, a total of 8,267 individuals were eligible for subsequent analysis (Fig. 1).
Blood sample collection and measurement of HbA1c
Every participant was demanded to fast overnight, and their blood samples were collected by medically trained staff. Then the samples were transported to the local laboratory timely and stored at 4 °C. The blood samples were centrifugated and stored at -20 °C before been transported to the central laboratory in Beijing and frozen at—80 °C before analysis [19]. All study laboratories had the standardized certification. The fasting plasma glucose (FPG) concentrations were measured using an enzymatic colorimetric test method, whereas the HbA1c assay was performed using the boronate affinity high performance liquid chromatography method [19].
Estimated glucose disposal rate measurement and outcome assessments
In current study, the eGDR (mg/kg/min) was calculated as previously described according to the following formula: eGDR = 21.158-(0.09 * WC) -(3.407 * HT) -(0.551* HbA1c) [WC = waist circumference (cm), HT = hypertension (yes = 1/no = 0), and HbA1c = HbA1c (%DCCT)] [20].
The primary outcome in current study was new-onset CVD (stroke or cardiac events), and the secondary outcomes were new-onset stroke and cardiac events, separately. The new-onset stroke or cardiac events were assessed by the following questions: “Have you been told by a doctor that you have been diagnosed with a heart attack, angina, coronary heart disease, heart failure, or other heart problems?” or “Have you been told by a doctor that you have been diagnosed with a stroke?” [21, 22]. Special conditions were employed to improve the accuracy of estimation of the onset time of stroke, as the exact time of stroke development was not available for all participants. They were considered as follows: First, if the participants did not develop stroke in any of the follow-up wave surveys (the time to event was calculated as follows: the time of the last survey—the time of baseline investigation); the follow-up time was not available (the approximate estimated time to event is defined as follows: the integer number years of the time of the last survey—the time of baseline investigation). Second, if they developed stroke (the time to event was defined as: the time of specific wave with stroke information/2—the time of interval wave/2 + the time of interval wave—the time of baseline investigation); the follow-up time was not available (the approximate time to event is defined as the integer number years of the time of specific wave with stroke information/2—the time of interval wave/2 + the time of interval wave—the time of baseline investigation). The same calculation is also used for cardiac events.
Covariates assessments
The covariates were collected at baseline including age, sex, place of residence (rural vs. urban), smoking status (ever smoking vs. never smoking), educational level (illiteracy; primary school; middle school; high school or above), drinking status (ever drinking vs. never drinking), body mass index (BMI; the weight in kilograms divided by the square of the height in meters), the presence or absence of other chronic diseases (dyslipidemia, chronic lung disease) and medications (anti-hypertensive and anti-dyslipidemic). Diabetes was defined as fasting glucose 126 mg/dl, or glycosylated hemoglobin (HbA1c) 6.5%, or treatment for diabetes mellitus, or self-reported history of diabetes. Dyslipidemia was defined as triglycerides 150 mg/dl, TC 240 mg/dl, HDL-C < 40 mg/dl, LDL-C 160 mg/dl, current use of the lipid-lowering medications, or self-reported history of dyslipidemia. Respondents were defined as having doctor-diagnosed chronic lung diseases if they answered yes to the question (“Have you been diagnosed with chronic lung diseases (excluding tumors, or cancer)”). The definition of smoking, drinking and hypertension has been described in previous study [18].
Statistical analysis
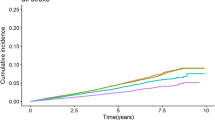
Participants were divided into four subgroups according to eGDR (mg/kg/min) quartiles. Data was given in the form of means ± standard deviations (SD) for continuous variables of the normal distribution or as median (interquartile range) for continuous variables of the abnormal distribution, and as frequency (percentage) for categorical variables. Pearson’s χ2 test was performed to compare the distribution of categorical variables, and ANOVA or Kruskal–Wallis test was performed to compare the continuous variables. Cox proportional hazards model was used to calculate the hazard ratios (HRs) and 95% confidence intervals (CIs) for new-onset CVD, stroke and cardiac events before and after adjusting for covariates. Kaplan–Meier curves and the log-rank test were used to compare the cumulative risk of CVD, stroke and cardiac events among four subgroups. In multivariable-adjusted model, both age, sex, place of residence, education level, smoking, drinking, systolic blood pressure, fasting plasma glucose, physical activity, chronic diseases (dyslipidemia, chronic lung disease) and medications (anti-hypertensive and anti-dyslipidemic) were included in the multivariable models. Furthermore, restricted cubic splines were used to examine the shape of the association between eGDR and CVD, stroke and cardiac events with four knots (at the 5th, 35th, 65th, and 95th percentiles) [23].
Subgroup analyses were further performed to evaluate the association between eGDR levels and the risk of CVD according to sex, diabetes, age, place of residence, smoking, drinking, education level and anti-diabetes/hypertension drugs subgroups. In sensitivity analysis 1, we calculated eGDR using BMI instead of waist circumferences. The eGDRBMI based on BMI was calculated according to the following formula: eGDRBMI = 19.02- (0.22* BMI)- (3.26*HT)- (0.61*HbA1c) (BMI = body mass index(kg/m2), HT = hypertension (yes = 1/no = 0), and HbA1c = HbA1c (%)) [13]. Two tailed P < 0.05 was considered to be statistically significant. In sensitivity analysis 2, those with anti-diabetes/hypertension drugs use were excluded in analysis. In sensitivity analysis 3, we further evaluate the effect of longitudinal changes of eGDR on CVD, stroke and cardiac events. Change in eGDR over time was calculated as the difference in eGDR between wave 1 and wave 3. All statistical analyses were conducted using SAS statistical software (version 9.4, Cary, NC).
Results
In the current study, a total of 8,267 participants (3,916 men and 4,351 women) were included in the analysis, and the average age was 58.90 ± 9.40 years. The median value of eGDR was 10.41(8.92–11.26) mg/kg/min. Baseline characteristics between the included and excluded participants were shown in Supplemental Table 1. As shown in Table 1, baseline characteristics, such as age, living place, education level, dyslipidemia, smoking, blood glucose, BMI, SBP and DBP were significantly different among the four subgroups.
After 6 years of follow-up (Wave 2 to Wave 4), a total of 1,476 respondents experienced (494 stroke and 1110 cardiac events). Event rates for CVD, stroke and cardiac events are shown in Table 2. Kaplan–Meier analysis showed that participants in the top quartile of eGDR had significantly lower cumulative incidence rates of CVD, stroke and cardiac events (all log-rank P < 0.001; Fig. 2). After adjustment for age, sex and other variables, the HRs (95%CIs) for the highest quartile of eGDR was 0.58(0.50–0.67) for CVD, 0.66(0.50–0.88) for stroke and 0.58(0.48–0.69) for cardiac events, respectively, compared with the lowest quartile. Moreover, each 1-SD increase of eGDR was associated with 19% (95%CIs, 11%-23%), 12%(95%CIs, 3%-19%) and 16%(95%CIs, 11%-20%) decreased risk of CVD, stroke and cardiac events, respectively (Table 2). Multivariable-adjusted restricted cubic spline analyses presented linear associations between eGDR with CVD, stroke and cardiac events (all P for linearity < 0.001) (Fig. 3).
Association of eGDR quartlies with risk of CVD, stroke and cardiac events. Hazard ratios and 95% CIs derived from restricted cubic spline regression, with knots placed at the 5th, 35th, 65th, and 95th percentiles of the distribution of remnant cholesterol. The reference point for remnant cholesterol is the midpoint (7.38 mg/kg/min) of the reference group from categorical analysis. The lowest 1% and highest 1% of participants were not shown in the figures for small sample sizes. Hazard ratios were adjusted for the same variables as multivariable-adjusted model in Table 2
In the subgroup analysis, significant associations between eGDR with risk of CVD were observed in all subgroups. Significant interactions between eGDR and sex, age and anti-diabetes/hypertension drugs on risk of CVD were also observed (Table 3). In sensitivity analysis 1, we calculated eGDR using BMI instead of waist circumferences. The results based on eGDRBMI were very similar to the results from the main analyses using eGDR based on waist circumference. After multiple adjustment of risk factors, the eGDRBMI was significantly associated with CVD, stroke and cardiac events. Similarly, each 1-SD increase of eGDRBMI was associated with decreased risk of CVD, stroke and cardiac events (Table 4). When we excluded participants with anti-diabetes/hypertension drugs use, significant associations between eGDR and CVD, stroke and cardiac events were also found (Table 4). In sensitivity analysis of longitudinal changes of eGDR on CVD risk, we found a higher decline of eGDR were associated with 19% (95%CIs, 11%-23%), 12%(95%CIs, 3%-19%) and 16%(95%CIs, 11%-20%) risk of CVD, stroke and cardiac events, respectively (Supplemental Table 2).
Discussion
Our nationwide study provided population-based novel evidence of eGDR and CVD in general population. Results suggested that eGDR was positively correlated with the occurrence of CVD, stroke and cardiac events. We found higher eGDR (decreased insulin resistance) was associated with lower risk of CVD, stroke and cardiac events, and there were liner relationships. In addition, subgroup and sensitivity analysis supported the stable association between eGDR and CVD, stroke and cardiac events. Furthermore, a higher decline of eGDR were associated with increased risk of CVD, stroke and cardiac events. Our findings supported the hypothesis that eGDR may be an important predictor of CVD, and potential target for CVD prevention in general population.
Insulin resistance is of utmost importance as an underlying mechanism for increased risk of CVD. Systemic insulin resistance produces atherogenic lipid phenotypes by increasing very low-density lipoprotein particles, which are metabolized into residual lipoproteins that promote atherosclerosis. Pro-inflammatory and procoagulant states caused by insulin resistance also play an important role in the formation of atherosclerosis [7]. Furthermore, insulin resistance was significantly correlated with vascular function, hypertension and macrophage accumulation [5]. Thus, evaluation of insulin resistance has emerged as an additional and significant CVD risk factor in the assessment of chronic vascular complications and mortality in general population and individuals with specific diseases [24,25,26]. Consideration the invasiveness and expenditure of traditional techniques in large-scale population studies, the eGDR was developed and proven to have a high precision of insulin resistance.
Since the eGDR was released, the score has been used in several investigations for the assessment of clinical diabetic chronic complications in both the T1D and T2D population [5]. In a study of 191 T1D participants with no prior CVD, the eGDR was independently related to ≥ 2 plaques (P = 0.018) and maximum plaque height (P < 0.01), suggesting that eGDR may be a predictor of preclinical carotid atherosclerosis for CVD risk [27]. In another study of 2,151 T1D participants, results indicated that eGDR was strongly associated with the presence of both microvascular and macrovascular complications than BMI, and the relationship was independent of HbA1c [28]. When it comes to T2D, Zabala et al. demonstrated that a higher eGDR was associated with a decreased risk of stroke (HRs = 0.60: 0.48–0.76) and death (HRs = 0.60: 0.48–0.76) in individuals with T2D. In addition, no statistically significantly different from the participants with or without insulin treatment [13]. In present study, our extended the current literature of eGDR on CVD in general population by showing positive associations of eGDR and CVD, stroke and cardiac events. Furthermore, we found significant interactions between eGDR and sex, age and anti-diabetes/hypertension drugs on risk of CVD. However, significant associations between eGDR with risk of CVD were observed in all subgroups, which was consistent with previous reported studies [29,30,31]. The present study provides a more valid appraisal of the relationship between eGDR and CVD, stroke and cardiac events.
Obesity was a well-known risk factor for multiple disease conditions including CVD and stroke [32]. In the eGDR formula, when waist circumference was used in place of waist-to-hip ratio, a similar pattern of results was obtained. In current study, after replacement the BMI in the eGDR formula, instead of waist circumference, there were robust association between eGDRBMI and CVD risk. Most former publications reported various complications in both T1D and T2D patients. In our subgroup analysis according to diabetes, it is noteworthy that the significant associations were found in participants with or without diabetes. Therefore, IR indicators (assessed by eGDR) seem to be not merely associated with complications in diabetes patients, but also has a certain predictive value in people without diabetes. According to previous reports, in the eGDR formula, the explained highest attributable relative risk for CVD was hypertension, followed by BMI, HbA1c, and waist circumference, all of which are well-known risk factors for CVD [13, 33]. Thus, the potential mechanisms under eGDR on CVD may indirect mediate thorough its effect on other variables such as blood pressure, lipidemia and glycaemia. Future well-designed experimental research and prospective clinical studies are certainly warranted to clarify the potential biological mechanisms. In addition, future studies are required to certify the optimal cut-off of eGDR that been applicable for implemented in routine clinical practice, and to formulate relevant management strategies of eGDR in both diabetes and non-diabetes patients.
The present study was based on the data from the CHARLS study, which is a large nationally representative cohort study with a high response rate, and potential confounders were collected and controlled in the multivariable models. Our findings provided extra evidence of eGDR in clinical application that incorporating eGDR into routine practice may help healthcare professionals and patients appreciate the importance of risk factors other than glucose levels, potentially improving long-term outcome in people with or without diabetes, particularly those whom are insulin resistant. However, there some limitations. First, the eGDR is a measure of insulin resistance developed for individuals with T1D, although the correlation between euglycaemic hyperinsulinaemic clamp and eGDR were good. We cannot conclude that eGDR can be replaced with the gold standard clamp technique. Second, the study outcome of CVD was based on self-reported doctor’s diagnosis of stroke or cardiac events, which may cause information bias. However, self-reported history of disease has been proven to possess relatively good reliability [34]. Third, there was significant difference between included and excluded groups in most of the baseline characteristics, which may reduce the credibility of the results. Finally, the present study was not a prespecified analysis. This observational analysis could be influenced by potential biases and confounding factors. Therefore, our study may only generate hypotheses for future studies.
In conclusion, our findings indicated that individuals with a low eGDR (a simple measure of insulin resistance), was associated with an increased risk of CVD, stroke and cardiac events in general Chinese population. Consequently, eGDR could emerge as a chief non-glycaemic variable for the early detection of individual with high risk of CVD, stroke and cardiac events in general Chinese population.
Availability of data and materials
The details of the CHARLS data are available at its website (http://charls.pku.edu.cn/en).
Abbreviations
- eGDR:
-
Estimated glucose disposal rate
- CVD:
-
Cardiovascular disease
- HOMA-IR:
-
Homeostasis model assessment of insulin resistance
- HbA1c:
-
Glycosylated hemoglobin A1c
- CHARLS:
-
China Health and Retirement Longitudinal Study
- FPG:
-
Fasting plasma glucose
- BMI:
-
Body mass index
References
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76:2982–3021.
Yang G, Wang Y, Zeng Y, Gao GF, Liang X, Zhou M, et al. Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet (London, England). 2013;381:1987–2015.
Liu S, Li Y, Zeng X, Wang H, Yin P, Wang L, et al. Burden of Cardiovascular Diseases in China, 1990–2016: Findings From the 2016 Global Burden of Disease Study. JAMA Cardiol. 2019;4:342–52.
Stevens RJ, Kothari V, Adler AI, Stratton IM. The UKPDS risk engine: a model for the risk of coronary heart disease in Type II diabetes (UKPDS 56). Clinical science (London, England: 1979). 2001;101:671–9.
Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuñiga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17:122.
Aminot-Gilchrist DV, Anderson HD. Insulin resistance-associated cardiovascular disease: potential benefits of conjugated linoleic acid. Am J Clin Nutr. 2004;79:1159s–63s.
Mather K, Anderson TJ, Verma S. Insulin action in the vasculature: physiology and pathophysiology. J Vasc Res. 2001;38:415–22.
Eddy D, Schlessinger L, Kahn R, Peskin B, Schiebinger R. Relationship of insulin resistance and related metabolic variables to coronary artery disease: a mathematical analysis. Diabetes Care. 2009;32:361–6.
DeFronzo RA, Tobin JD, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979;237:E214-223.
Emoto M, Nishizawa Y, Maekawa K, Hiura Y, Kanda H, Kawagishi T, et al. Homeostasis model assessment as a clinical index of insulin resistance in type 2 diabetic patients treated with sulfonylureas. Diabetes Care. 1999;22:818–22.
Komosinska-Vassev K, Gala O, Olczyk K, Jura-Półtorak A, Olczyk P. The Usefulness of Diagnostic Panels Based on Circulating Adipocytokines/Regulatory Peptides, Renal Function Tests, Insulin Resistance Indicators and Lipid-Carbohydrate Metabolism Parameters in Diagnosis and Prognosis of Type 2 Diabetes Mellitus with Obesity. Biomolecules. 2020;10:1304.
Orchard TJ, Olson JC, Erbey JR, Williams K, Forrest KY, Smithline Kinder L, et al. Insulin resistance-related factors, but not glycemia, predict coronary artery disease in type 1 diabetes: 10-year follow-up data from the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes Care. 2003;26:1374–9.
Zabala A, Darsalia V, Lind M, Svensson AM, Franzén S, Eliasson B, et al. Estimated glucose disposal rate and risk of stroke and mortality in type 2 diabetes: a nationwide cohort study. Cardiovasc Diabetol. 2021;20:202.
Helmink MAG, de Vries M, Visseren FLJ, de Ranitz WL, de Valk HW, Westerink J. Insulin resistance and risk of vascular events, interventions and mortality in type 1 diabetes. Eur J Endocrinol. 2021;185:831–40.
Xuan J, Juan D, Yuyu N, Anjing J. Impact of estimated glucose disposal rate for identifying prevalent ischemic heart disease: findings from a cross-sectional study. BMC Cardiovasc Disord. 2022;22:378.
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43:61–8.
Han L, Shen S, Wu Y, Zhong C, Zheng X. Trajectories of depressive symptoms and risk of cardiovascular disease: Evidence from the China Health and Retirement Longitudinal Study. J Psychiatr Res. 2021;145:137–43.
Zheng X, Han L, Shen S. Hypertension, remnant cholesterol and cardiovascular disease: evidence from the China health and retirement longitudinal study. J Hypertens. 2022;40:2292–8.
Zhang L, Yang J, Liao Z, Zhao X, Hu X, Zhu W, et al. Association between Diabetes and Cognitive Function among People over 45 Years Old in China: A Cross-Sectional Study. Int J Environ Res Public Health. 2019;16:1294.
Williams KV, Erbey JR, Becker D, Arslanian S, Orchard TJ. Can clinical factors estimate insulin resistance in type 1 diabetes? Diabetes. 2000;49:626–32.
Shi Z, Nicholls SJ, Taylor AW, Magliano DJ, Appleton S, Zimmet P. Early life exposure to Chinese famine modifies the association between hypertension and cardiovascular disease. J Hypertens. 2018;36:54–60.
Li H, Qian F, Hou C, Li X, Gao Q, Luo Y, et al. Longitudinal Changes in Depressive Symptoms and Risks of Cardiovascular Disease and All-Cause Mortality: A Nationwide Population-Based Cohort Study. J Gerontol A Biol Sci Med Sci. 2020;75:2200–6.
Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8:551–61.
Paneni F, Costantino S, Cosentino F. Insulin resistance, diabetes, and cardiovascular risk. Curr Atheroscler Rep. 2014;16:419.
Chan DT, Watts GF, Irish AB, Dogra GK. Insulin resistance and vascular dysfunction in chronic kidney disease: mechanisms and therapeutic interventions. Nephrol Dial Transplant. 2017;32:1274–81.
Kim KS, Lee YM, Lee IK, Kim DJ, Jacobs DR Jr, Lee DH. Paradoxical Associations of Insulin Resistance With Total and Cardiovascular Mortality in Humans. J Gerontol A Biol Sci Med Sci. 2015;70:847–53.
Pané A, Conget I, Boswell L, Ruiz S, Viñals C, Perea V, et al. Insulin resistance is associated with preclinical carotid atherosclerosis in patients with type 1 diabetes. Diabetes Metab Res Rev. 2020:e3323.
Helliwell R, Warnes H, Kietsiriroje N, Campbell M, Birch R, Pearson SM, et al. Body mass index, estimated glucose disposal rate and vascular complications in type 1 diabetes: Beyond glycated haemoglobin. Diabetic Med. 2021;38:e14529.
Nishtala R, Kietsiriroje N, Karam M, Ajjan RA, Pearson S. Estimated glucose disposal rate demographics and clinical characteristics of young adults with type 1 diabetes mellitus: A cross-sectional pilot study. Diab Vasc Dis Res. 2020;17:1479164120952321.
Šimonienė D, Platūkiene A, Prakapienė E, Radzevičienė L, Veličkiene D. Insulin Resistance in Type 1 Diabetes Mellitus and Its Association with Patient’s Micro- and Macrovascular Complications, Sex Hormones, and Other Clinical Data. Diabetes Ther. 2020;11:161–74.
Epstein EJ, Osman JL, Cohen HW, Rajpathak SN, Lewis O, Crandall JP. Use of the estimated glucose disposal rate as a measure of insulin resistance in an urban multiethnic population with type 1 diabetes. Diabetes Care. 2013;36:2280–5.
Upadhyay J, Farr O, Perakakis N, Ghaly W, Mantzoros C. Obesity as a Disease. Med Clin North Am. 2018;102:13–33.
O’Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet (London, England). 2010;376:112–23.
St Sauver JL, Hagen PT, Cha SS, Bagniewski SM, Mandrekar JN, Curoe AM, et al. Agreement between patient reports of cardiovascular disease and patient medical records. Mayo Clin Proc. 2005;80:203–10.
Acknowledgements
This analysis uses data or information from the Harmonized CHARLS dataset and Codebook, Version C as of April 2018 developed by the Gateway to Global Aging Data. The development of the Harmonized CHARLS was funded by the National Institute on Ageing (R01 AG030153, RC2 AG036619, R03 AG043052). For more information, please refer to www.g2aging.org.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Xiaowei Zheng conceived and designed the research; Minaglan Jiang, Xiao Ren and Longyang Han wrote the manuscript; and and Xiaowei Zheng performed the data analysis. All authors reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethics application for collecting data on human subjects in CHARLS was approved by the Biomedical Ethics Review Committee of Peking University (IRB00001052-11015), and all CHARLS participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplemental Table 1.
Baseline characteristics between the included and excluded groups. Supplemental Table 2. Association between eGDR change and risks for CVD, stroke and cardiac events (N=4075)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ren, X., Jiang, M., Han, L. et al. Estimated glucose disposal rate and risk of cardiovascular disease: evidence from the China Health and Retirement Longitudinal Study. BMC Geriatr 22, 968 (2022). https://doi.org/10.1186/s12877-022-03689-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03689-x