Abstract
Background
Frailty is a common condition in older adults that is characterized by transitions between frailty states in both directions (progression and reversion) over time. Loneliness has been reported to be associated with the incidence of frailty, but few studies have explored the impact of persistent loneliness over time on frailty. In this study, we aimed to whether and how two different types of loneliness, transient and chronic, were associated with changes in frailty status in older adults.
Methods
The analytic sample contained 2961 adults aged ≥ 60 years who completed interviews for both the 2011 and 2015 waves of the China Health and Retirement Longitudinal Study. The logistic regression model was used to examine the relationship between transient and chronic loneliness and progression and reversion of frailty. Demographics (age, sex, education level, marital status, urban–rural residence), living alone, chronic conditions, physical function, and depressive symptoms from the 2011 wave were adjusted.
Results
After four years, 21% of the studied sample reported progression, 20% reported reversion in frailty, 31% reported transient loneliness, and 14% reported chronic loneliness. There was no significant difference in participants who reported transient loneliness (OR = 1.10, 95% CI [0.89,1.37]), or chronic loneliness (OR = 1.14, 95% CI [0.84,1.57]) on the progression of frailty, compared with no report of loneliness. Participants reporting chronic loneliness (OR = 0.68, 95% CI [0.50,0.93]) were less likely to report reversion in their level of frailty compared to participants who did not report loneliness but not transient loneliness (OR = 0.87, 95% CI [0.70,1.08]).
Conclusions
Roughly the same percentage, a fifth, of older Chinese adults progressed or reversed in frailty status without active intervention. Chronic loneliness was related to a lower probability of reversion in the frail group than in the no loneliness group, but not in the transient loneliness group. More attention should be given to older adults with chronic loneliness.
Similar content being viewed by others
Introduction
Frailty is a common condition in older adults that characterizes their susceptibility to poor homeostasis resolution after an abrupt change in health status. According to Fried’s phenotype model [1], frailty is the presence of at least three of five criteria: slow gait speed, inactivity, weakness (grip strength), self-reported exhaustion, and unintentional weight loss. In this model, frailty status was categorized as robustness(or nonfrailty), prefrailty, and frailty. Frailty will become more prevalent as the population ages, putting a greater strain on health and well-being. This in turn will have a significant impact on health and social care resources and result in a huge burden on clinical practice and public health [2]. As a result, it is crucial to determine how to slow the onset of frailty.
The frailty process is not a steady state but is characterized by transitions between frailty states in both directions (progression and reversion) over time [3]. A meta-study pooled data from 42,775 community-dwelling older adults and showed that transitions between adjacent states (one-step transitions) are prevalent [4, 5]. Frailty transitions have been demonstrated to be influenced by a variety of health and psychosocial variables, such as loneliness in recent research [6].
Loneliness is a subjective distressing feeling generated by an individual’s impression of a gap between their actual and desired social relationships [7]. Although loneliness may affect people of any age, it has a particularly negative influence on older adults [8]. A recent study systemtatically reviewed 57 studies from 113 countries or territories and reported a 21% to 24% of prevalence of loneliness in older adults, which was approximately 10 times that in young adults [9]. Increasing evidence indicates that the onset of the COVID-19 pandemic, along with the constainment measures — such as social distancing restrictions; the ‘stay at home’ order; and the closure of cafes, restaurants, and gyms — have disproportionately affected older adults, increasing the incidence of loneliness [10]. Loneliness is influenced by external circumstances (for example, bereavement and migration) and the human characteristics of the individual such as health status and personality [11]. As a result, the level of loneliness experienced by older adults is likely to change over time (referred to here as “transient” loneliness) in some people, while it remains constant in others (referred to here as “chronic” loneliness) [12].
An increasing number of studies have explored the association between loneliness and frailty in older adults. In general, older adults with frailty appear to have fewer social networks and greater rates of loneliness [13]. In return, loneliness is also a risk factor for the incidence of frailty [14]. To date, most research has concentrated on the association between frailty progression and severe/regular loneliness [6, 15]. Few concern the impact of persistent loneliness over time. Only a four-year cohort study found that older adults with chronic loneliness had a higher risk of death than those with transient loneliness [16]. However, it is unclear whether transient and chronic loneliness have distinct effects on older adults’ frailty status changes. Hence, in this study, we aimed to identify the prevalence and explore the potentially different impacts of transient and chronic loneliness on the progression and reversion of frailty by using data from the China Health and Retirement Longitudinal Study (CHARLS).
Methods
Data and sample
Data were obtained from the ongoing CHARLS. For geriatric and health policy research, the CHARLS gathered a nationwide representative cohort of Chinese residents aged over 45 and older to collect a wide range of personal health information as well as social and economic data. Approximately 150 regions (counties) were chosen according to population size from 28 Chinese provinces, and three villages/communities were then selected from each county as primary sample units (PSUs). Each of the 450 PSUs had eighty households picked at random, with 24 being investigated. If there were people in the family who were 45 or older, one of them was chosen at random as a respondent, and both the respondents and their spouses were interviewed. There are currently four waves of data available, including at baseline (wave 1 in 2011) and follow-ups every two years at wave 2 (2013), wave 3 (2015) and wave 4 (2018). At the baseline of the study, a total of 17,708 people from 10,257 households were enrolled. The details of the cohort have been described elsewhere [17]. The CHARLS was approved by the ethical review committee at Peking University. The participants in the CHARLS were interviewed face-to-face using a standardized questionnaire.
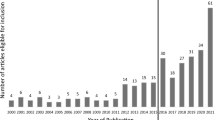
Since the measurement of frailty was lacking in 2018, the data from 2011 and 2015 included in this study to obtain the longest follow-up. The inclusion criteria of this study’s cohort were as follows: (1) adults aged 60 and above in 2011 and (2) respondents who reported data on four or more frailty components in 2011 and 2015. The exclusion criteria were as follows: (1) no data on loneliness and (2) diagnosis of Alzheimer’s disease, Parkinson’s disease, stroke or brain atrophy. Ultimately, the total sample size was 2961, and a detailed flow chart is shown in Fig. 1.
Measures
Dependent variables: progression and reversion of frailty
Frailty was measured with the modified Frailty Phenotype Criteria (PFC) which have been rigorously validated using CHARLS data [1]. If three or more of the following five criteria are met, older adults were identified as frail (coded “2”): slow walking speed, weakness, exhaustion, shrinking, and inactivity. Older adults who met one or two criteria were identified as prefrail (coded “1”), and those who met none were coded 0 for robust. There were two binary variables to identify progression cases and reversion cases separately. Individuals who were initially robust or prefrail (in 2011) and progressed to severe status (prefrail or frail) in 2015 were identified as cases of “progression” (coded “1”), while others were coded “0” in the “progression” variable. Individuals who were initially prefrail or frail and reversed to mild status (prefrail or robust) were identified as cases of “reversion” (coded “1”), while others were coded “0” in the “reversion” variable.
Slow walking speed was defined as the average time of two walking tests on a 2.5-m track that was slower than the 20% percentile adjusted for sex and height. Weakness was defined as the maximal grip strength of each hand (two tests), assessed by a Yuejian™ WL-1000 mechanical dynamometer, which was lower than the 20th percentile adjusted for sex and BMI. Exhaustion was identified if the participants reported a moderate amount of time or all of the time to either of two questions (“I could not get moving” and “I felt like everything I did was an effort”). Shrinking was defined as self-reported weight reduction of 5 kg or more in the previous year or a current BMI of less than 18.5 kg/m2. Inactivity was identified by an item asking individuals if they walked for 10 min or more constantly throughout a typical week.
Independent variables: loneliness
Loneliness was measured with a single item (how often did you feel lonely) of the Centre for Epidemiological Studies Depression Scale (CESD) in 2011 and 2015. Responses were scored on a 4-point Likert scale from 0 (never) to 3 (always). Following the previous study [18], individuals responding “some of the time”, “occasionally”, or “always” were recorded as “lonely”. This measurement has been widely used in the Chinese population [19]. Following previous research [20], transient loneliness was defined if individuals reported “lonely” in one of waves, and chronic loneliness if they reported “lonely” in both waves and not lonely if they reported not lonely in both waves.
Covariates
Age, sex, education level, marital status, current residence location, living alone, chronic conditions, physical function (activities of daily living (ADLs) and instrumental activities of daily living (IADLs)), and depressive symptoms were adjusted as covariates. There were three levels of educational attainment, including no formal education, elementary or middle school, and high school or above. Marital status was categorized as “married/partnered” or “unmarried”. The current resident location was categorized as residing in a rural area or an urban area. A chronic condition was considered present if the participant had been diagnosed with one or more of the following chronic diseases: diabetes, cancer, heart attack, chronic lung diseases, and liver disease. Physical function was assessed by ADLs and IADLs. ADLs were considered present if the older adults had difficulties in eating, bathing, dressing, controlling their urine, using the toilet, or getting in and out of bed with a range of 0–6. The IADLs with a range of 0–6 were measured if older adults had difficulties with housework, preparing hot meals, grocery shopping, making phone calls, taking medication, or manging money. Depressive symptoms were measured by the modified Chinese version of the CES-D [21] excluding two items for identifying exhaustion (in the frailty) and one item for measuring loneliness with a range of 0–21.
Statistical analysis
The demographic characteristics were summarized by using descriptive statistics. Logistic regression models were used to examine the impact of independent variables either on the progression or reversion of frailty status. A low proportion (2.7%) of respondents had at least 1 missing value on covariates, and those respondents were excluded from the Logistic regression model analysis. Multiple imputation was applied in the sensitivity analysis. A total of 30 imputed data set were obtained and the results were pooled by Rubin’s rule [22]. The consistent results were found and details of the sensitivity analysis are shown in the Supplementary Information. The hazard ratio (HR) and corresponding 95% confidence intervals (95% CI) were reported. Statistical analyses were conducted using R version 4.0.4.
Results
Table 1 presents the descriptive chracteristics for the whole sample differentiated by frailty status (in 2011). Participants had an average age of 67 at the baseline; 49% were female, a majority had no formal education (55.3%), 81.6% were married, and 31.9% lived in urban areas. Among them, 967 (32.7%) were robust, 1848 (62.4%) were pre-frail, and 146 (4.9%) were frail.
After four years, 21% (611/2961) of subjects reported progression, and 20% (601/2961) reported reversion of frailty. The distribution of progression and reversion according was shown in Fig. 2. Among participants reported progression, 82% (499/601) were progressed from robust to prefrailty while 16% (102/601) were progressed from prefrailty to frailty and 2% (10/601) from robust to frailty. Among participants reported reversion, 81% (484/601) were reversed from prefrailty to robust while 18% (109/601) were reversed from frailty to prefrailty and 1% (8/601) from frailty to robust.
After four years, 31% (927/2961) reported transient loneliness, and 14% (426/2961) reported chronic loneliness. The results of the adjusted logistic regression model regarding progression and reversion are shown in Fig. 3. There was no significant difference in participants who reported transient loneliness (OR = 1.10, 95% CI [0.89,1.37]) or chronic loneliness (OR = 1.14, 95% CI [0.84,1.57]) on the progression of frailty, compared with no loneliness. Participants reporting chronic loneliness (OR = 0.68, 95% CI [0.50,0.93]) were less likely to report reversion in their level of frailty compared to participants who did not report loneliness, while there was no significant difference in transient loneliness (OR = 0.87, 95% CI [0.70,1.08]) and no loneliness.
Results for the adjusted Cox Proportional Hazards Model of Progression and Reversion of Frailty. Note: Models were adjusted by age, sex, education level, marital status, current residence location, the presence of the chronic condition, ADLs, IADLs, living alone, and depressive symptoms. ADLs refer to Activities of Daily Living (ADLs) and IADLs refer to Instrumental activities of daily living (IADLs)
Discussion
To our best knowledge, this study was the first to investigate the association between different types of loneliness and progression and reversion of frailty in older Chinese adults. The findings from this representative Chinese community-dwelling sample indicated that approximately one-fifth of the sample progressed their frailty status and the roughly same percentage of older adults reversed their status, which is similar to a previous study in Europe [6]. Although some older adults reported reversion without intervention, a majority of older adults remained the same status or reported progression when the participants had already been frail or prefrail. It means that the early intervention is still warranted to prevent or reduce the level of frailty in older adults.
We found that chronic loneliness was related to a lower probability of reversion in the frail group than in the no loneliness group but not in the transient loneliness group. These findings highlight that chronic loneliness may act as an obstacle to spontaneous reversion. This might be because people with loneliness may have higher immune functioning, such as higher levels of tumor necrosis factor alpha (TNF-α) and interleukin-6 (IL-6) [23], which have also been found to be high in frail older adults [24]. This effect may require accumulation [25], which may lead to no significant effect on the transient loneliness group. Another potential mechanism is that chronic loneliness may provide a further obstacle to successfully modifying social networks in accordance with individuals’ abilities and may then contribute to a series of physical and mental health conditions, including stroke, chronic stress, depression, and cognitive decline [26], all of which may decrease the likelihood of spontaneous reversion. Our findings further underlying that there is a difference in the effects of subtypes of loneliness. On the other hand, we also found that both transient loneliness and chronic loneliness had no association with the progression of frailty, in contrast to a previous study conducted by Gale and colleagues [15]. This may be because Gale’s study only measured the level of loneliness at the baseline instead of a dynamic condition measured in our study. A further systematic review of the association between the two subtypes of loneliness and frailty might be warranted.
Our findings have some key implications for the management of frailty. First, our study provides an overview of the frailty transition among older adults in China. Although the frailty in older adults could be spontaneously reversed, a majority of older adults remained the same status or reported progression when the participants had already been frail or prefrail. Early intervention for older adults is still important. Second, our study highlights that chronic loneliness may prevent reversion in those who might otherwise improve their frailty status. Although health and social care providers place a strong premium on diet and physical activity, social interaction elements, such as loneliness, have received less attention. Our study identifies a vulnerable group, chronically lonely older adults, and suggests that this vulnerable group is more likely to be helped by early interventions to increase the probability of reversing frailty, which might reduce the healthcare burden for older adults.
The strengths of our study include the use of a large sample size and long-term follow-up. This study also explored the differential impact of transient and chronic loneliness on changes in frailty status. There are some limitations to interpreting the results. First, our sample only included respondents who had reported in 2011 and 2015 and a number of subjects were excluded because of death or being lost to follow-up. Selection bias might occur since participants included in the analysis were more likely to be healthier than those who were excluded. Second, loneliness was assessed by one item, although this measurement has been widely used in the Chinese population [19] and has strong correlations with multiple items. This single-item measurement may be less reliable than a measure with multiple aspects of loneliness [27]. Third, loneliness was measured in a relatively short period. In this study, participants reported their psychosocial condition in the last week, which may not reflect the fluctuation during the 4-year follow-up period. A long-term measurement of loneliness might be warranted in future studies.
In conclusion, one-fifth of older Chinese adults progressed, and the roughly same percentage of older adults reversed their frailty status. Chronic loneliness was related to a lower probability of reversion in the frail group than in the no loneliness group but not in the transient loneliness group. Attention should be given to older adults with constant loneliness, which should be addressed.
Availability of data and materials
The datasets used in the current study are accessed in the CHARLS website (http://forum.charls.pku.edu.cn/) after the users apply in their website.
Abbreviations
- ADLs:
-
Activities of Daily Living
- CES-D:
-
Epidemiological Studies-Depression
- CHARLS:
-
China Health and Retirement Longitudinal Study
- HR:
-
Hazard Ratio
- IADLs:
-
Instrumental Activities of Daily Living
- IL-6:
-
Interleukin-6
- PFC:
-
Frailty Phenotype Criteria
- PSUs:
-
Primary Sample Units
- TNF- α:
-
Tumor Necrosis Factor Alpha
References
Wu C, Smit E, Xue Q-L, Odden MC. Prevalence and correlates of frailty among community-dwelling Chinese older adults: the China health and retirement longitudinal study. J Gerontol Series A. 2018;73(1):102–8.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. lancet. 2013;381(9868):752–62.
Lorenzo-López L, López-López R, Maseda A, Buján A, Rodríguez-Villamil JL, Millán-Calenti JC. Changes in frailty status in a community-dwelling cohort of older adults: The VERISAÚDE study. Maturitas. 2019;119:54–60.
Kojima G, Taniguchi Y, Iliffe S, Jivraj S, Walters K. Transitions between frailty states among community-dwelling older people: a systematic review and meta-analysis. Ageing Res Rev. 2019;50:81–8.
Bentur N, Sternberg SA, Shuldiner J. Frailty transitions in community dwelling older people. Isr Med Assoc J. 2016;18(8):449–53.
Jarach CM, Tettamanti M, Nobili A, D’avanzo B. Social isolation and loneliness as related to progression and reversion of frailty in the Survey of Health Aging Retirement in Europe (SHARE). Age Ageing. 2021;50(1):258–62.
Hawkley LC, Cacioppo JT. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40(2):218–27.
Gorenko JA, Moran C, Flynn M, Dobson K, Konnert C. Social isolation and psychological distress among older adults related to COVID-19: a narrative review of remotely-delivered interventions and recommendations. J Appl Gerontol. 2021;40(1):3–13.
Surkalim DL, Luo M, Eres R, Gebel K, van Buskirk J, Bauman A, et al. The prevalence of loneliness across 113 countries: systematic review and meta-analysis. BMJ. 2022;376:e067068.
Greig F, Perera G, Tsamakis K, Stewart R, Velayudhan L, Mueller C. Loneliness in older adult mental health services during the COVID‐19 pandemic and before: Associations with disability, functioning and pharmacotherapy. Int J Geriatr Psychiatry. 2022;37(1):1–8.
Victor CR, Bowling A. A longitudinal analysis of loneliness among older people in Great Britain. J Psychol. 2012;146(3):313–31.
Martín-María N, Caballero FF, Miret M, Tyrovolas S, Haro JM, Ayuso-Mateos JL, et al. Differential impact of transient and chronic loneliness on health status A longitudinal study. Psychol Health. 2020;35(2):177–95.
Hoogendijk EO, Suanet B, Dent E, Deeg DJ, Aartsen MJ. Adverse effects of frailty on social functioning in older adults: Results from the Longitudinal Aging Study Amsterdam. Maturitas. 2016;83:45–50.
Davies K, Maharani A, Chandola T, Todd C, Pendleton N. The longitudinal relationship between loneliness, social isolation, and frailty in older adults in England: a prospective analysis. Lancet Healthy Longevity. 2021;2(2):e70–7.
Gale CR, Westbury L, Cooper C. Social isolation and loneliness as risk factors for the progression of frailty: the English Longitudinal Study of Ageing. Age Ageing. 2018;47(3):392–7.
Shiovitz-Ezra S, Ayalon L. Situational versus chronic loneliness as risk factors for all-cause mortality. Int Psychogeriatr. 2010;22(3):455–62.
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. 2014;43(1):61–8.
Yu B, Steptoe A, Chen Y, Jia X. Social isolation, rather than loneliness, is associated with cognitive decline in older adults: the China Health and Retirement Longitudinal Study. Psychol Med. 2021;51(14):2414–21.
Guo L, An L, Luo F, Yu B. Social isolation, loneliness and functional disability in Chinese older women and men: a longitudinal study. Age Ageing. 2021;50(4):1222–8.
Zhong B-L, Chen S-L, Conwell Y. Effects of transient versus chronic loneliness on cognitive function in older adults: Findings from the Chinese Longitudinal Healthy Longevity Survey. Am J Geriatr Psychiatry. 2016;24(5):389–98.
Yu S-C, Lin Y-H, Hsu W-H. Applying structural equation modeling to report psychometric properties of Chinese version 10-item CES-D depression scale. Qual Quant. 2013;47(3):1511–8.
Royston P. Multiple imputation of missing values. Stand Genomic Sci. 2004;4(3):227–41.
Jaremka LM, Fagundes CP, Peng J, Bennett JM, Glaser R, Malarkey WB, et al. Loneliness promotes inflammation during acute stress. Psychol Sci. 2013;24(7):1089–97.
Walston J, McBurnie MA, Newman A, Tracy RP, Kop WJ, Hirsch CH, et al. Frailty and activation of the inflammation and coagulation systems with and without clinical comorbidities: results from the Cardiovascular Health Study. Arch Intern Med. 2002;162(20):2333–41.
Hawkley LC, Cacioppo JT. Loneliness and pathways to disease. Brain Behav Immun. 2003;17(1):98–105.
Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol Aging. 2010;25(2):453.
Teguo MT, Simo-Tabue N, Stoykova R, Meillon C, Cogne M, Amiéva H, et al. Feelings of loneliness and living alone as predictors of mortality in the elderly: the PAQUID study. Psychosom Med. 2016;78(8):904–9.
Acknowledgements
We would like to thank all the participants and staffs in the China Health and Retirement Longitudinal Study (CHARLS).
Funding
There is no fund for this study.
Author information
Authors and Affiliations
Contributions
ZW and CLB conceived of the presented idea. ZW conducted the data analyses. CLB and ZW wrote and reviewed the main manuscript. All of the authors approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The data were from the China Health and Retirement Longitudinal Study, which was approved by the Ethical Review Committee of Beijing University (IRB00001050-11015) and signed informed consent was obtained from all participants. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table1.
Adjusted Cox Proportional-Hazards Model of Progression and Reversion ofFrailty After Multiple Imputation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chu, BL., Zhang, W. Impact of transient and chronic loneliness on progression and reversion of frailty in community-dwelling older adults: four-year follow-up. BMC Geriatr 22, 642 (2022). https://doi.org/10.1186/s12877-022-03283-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03283-1