Abstract
Background
Falls represent important drivers of intrinsic capacity losses, functional limitations and reduced quality of life in the growing older adult’s population, especially among those presenting with frailty. Despite exercise- and cognitive training-based interventions have shown effectiveness for reducing fall rates, evidence around their putative cumulative effects on falls and fall-related complications (such as fractures, reduced quality of life and functional limitations) in frail individuals remains scarce. The main aim of this study is to explore the effectiveness program combining an individualized exercise program and an executive function-based cognitive training (VIVIFRAIL-COGN) compared to usual care in the prevention of falls and fall-related outcomes over a 1-year follow-up.
Methods
This study is designed as a four-center randomized clinical trial with a 12-week intervention period and an additional 1-year follow-up. Three hundred twenty frail or pre-frail (≥ 1 criteria of the Frailty Phenotype) older adults (≥ 75 years) with high risk of falling (defined by fall history and gait performance) will be recruited in the Falls Units of the participating centers. They will be randomized in a 1:1 ratio to the intervention group (IG) or the control group (CG). The IG will participate in a home-based intervention combining the individualized Vivifrail multicomponent (aerobic, resistance, gait and balance and flexibility) exercise program and a personalized executive function-based cognitive training (VIVIFRAIL-COGN). The CG group will receive usual care delivered in the Falls Units, including the Otago Exercise Program. Primary outcome will be the incidence of falls (event rate/year) and will be ascertained by self-report during three visits (at baseline, and 6 and 12 weeks) and telephone-based contacts at 6, 9 and 12 months after randomization. Secondarily, effects on measures of physical and cognitive function, quality of life, nutritional, muscle quality and psychological status will be evaluated.
Discussion
This trial will provide new evidence about the effectiveness of an individualized multidomain intervention by studying the effect of additive effects of cognitive training and physical exercise to prevent falls in older frail persons with high risk of falling. Compared to usual care, the combined intervention is expected to show additive effects in the reduction of the incidence of falls and associated adverse outcomes.
Trial registration
NCT04911179 02/06/2021.
Similar content being viewed by others
Introduction
Background
Approximately, 1 out of 3 adults aged 65 or over experience at least one fall per year and among them, 10% suffer a significant injury such as a fracture or traumatic brain injury [1]. These figures rocket in those aged 80 years or more, with half of them falling over the course of a year [2]. Around 10% of falls result in a fracture [3, 4]. In the European Union, it has been estimated that 36,000 older adults die because of a fall yearly, whereas the figures of hospital admission and emergency department visits approximate to 1.5 million and 2.3 million, respectively [5].
Although most fall-related injuries (bruising, lacerations, sprains…) are not severe, they represent important drivers of decline of the intrinsic capacity (physical and cognitive capacities of the individual) [6], functional limitations development, reduced quality of life and the development of psychosocial issues (anxiety, fear of falling and depression) [7, 8]. Therefore, falls constitute a significant sentinel event for older adults by threatening their health and well-being. With the population of older adults increasing worldwide [9], falls will continue to represent an increasing health and economic burden on the public health system. Consequently, prevention of falls has become an international public health priority [10, 11].
Most of the clinical practice guidelines recommend managing older frail adults with repeated falls in specialized Falls and Fracture Units [12]. Ideally management of falls should consist of a multidimensional comprehensive assessment [13] followed by tailored multidomain interventions lead by an interdisciplinary team (physician, nurse, physiotherapist and occupational therapist) and focused to identify and tackle risk factors [12, 14].
Among them, progressive cognitive and physical function decline stand out, both as targets of falls preventive and mitigating interventions, given their tight relation with their occurrence [15,16,17]. Impairments in the physical domain, such as muscle strength [18], gait performance [19] and balance [20], are strong risk factors for falls, whereas decreases in the cognitive abilities, especially in the executive function domain [21], have been associated with the odds of falling [22] and suffering fall-related injuries [23]. Executive function is a cognitive domain composed of a broad set of cognitive processes integrating information from multitude cortical systems to generate goal-directed behavior [24]. It constitutes an integral function and one of the most important components of daily-living navigating [25]. In addition, robust evidence supports the relationship between cognition and motor function, with common anatomical substrates and neural pathways. Allocated in the prefrontal cortex, executive functions play a key role in neural control of gait [26, 27], especially under challenging circumstances. For instance, when an attention-demanding cognitive task is performed during a walking task, known as dual-task, the performance of either one or both tasks may decrease compared to each individual task as a result of competence for common neural pathways [28]. This motor-cognitive crosstalk also explains the higher risk of falls among persons with cognitive and physical impairment, therefore interventions targeting both might be key to reduce falls risk [29].
Loss of capacities constitute manifestations of the progressive loss of reserve at multi-systemic physiological levels, leading to increased vulnerability when facing stressors, a state that was decades ago termed frailty [30,31,32]. Frail individuals present with the highest risk of suffering falls and related outcomes [33, 34]. Consequently, frail individuals might benefit the most from interventions oriented to falls prevention trough combined interventions, but the number of studies in this population is limited [35].
In this sense, physical exercise stands out as an effective cornerstone in falls prevention among geriatric patients [13, 36]. Exercise has been shown to concurrently positively impact both physical and cognitive function of older adults [37,38,39,40], which might result in the observed reductions in the risk and rate of falls both in community-dwelling [41, 42] and residential populations [43]. In addition, exercise has shown to beneficially impact fall-related issues such as fear of falling [44]. Previous evidence has shown that multicomponent physical exercise programs combining strength and balance exercises might confer the greatest benefits in older adults with high risk of falling [36, 42]. Nevertheless, so far, the features of an exercise program as a single intervention that might maximize effectiveness remain to be elucidated [36].
Given that cognitive impairments are associated with falls occurrence [45], cognitive training, usually involves a guided practice on a set of specific tasks designed to engage targeted cognitive functions [46], might be beneficial in falls prevention [47]. Cognitive training interventions like dual task training, improve attention, executive function and memory in older persons with cognitive decline but also in healthy older adults [48]. A reduced number of emerging studies have shown cumulative effects in fall risk parameters of combined exercise and cognitive training interventions compared to interventions focused exclusively in motor function [49]. Both animal- and human-based studies have shown greater neurophysiological (neurogenesis, neuroplasticity and increased brain blood flow) and functional (physical and cognitive performance) [50, 51] after the combined intervention, compared to single intervention-based approaches [52, 53]. Putatively, programs combining physical exercise and cognitive training focused in executive function tasks might constitute the optimal approach to maximize reductions in fall risk and associated complications [12, 54], but whether available evidence translate to reductions in falls incidence remains to be elucidated [55, 56].
The OTAGO exercise program (OEP), that was developed in the 1960s in New Zealand [57], is considered the gold-standard exercise-based intervention in falls prevention. It consists of several strength, endurance, flexibility and balance exercises supervised by a physical therapist. It has shown to be effective in improving fall-related risk factors [58,59,60] and preventing falls [61, 62] and related consequences [63, 64]. Notably, several adaptations have been performed since it was firstly designed, leading to a high degree of heterogeneity, with mixed results obtained from different delivery fashions [65,66,67]. In addition, falls and fall-related outcomes have been poorly registered in available studies, and how exercise programs impact fall-related fractures, healthcare utilization, psychological and social issues remains scarcely investigated [68]. Consequently, well-powered studies with long follow-up periods and comprehensive evaluation of falls consequences are needed in order to capture the real potential of exercise programs in different populations of older adults [42].
Recently, the VIVIFRAIL Project (www.vivifrail.com) was developed by world experts in the field of physical exercise and frailty aiming to provide necessary knowledge to prescribe individualized physical exercise in the prevention of frailty and falls in older persons. Within the VIVIFRAIL philosophy, exercise prescription is based on the functional status and fall risk of the individual, evaluated through performance-based measures [69]. This approach aligns with the recently proposed function-based healthy ageing paradigm [70]. So far, this exercise program has been proven safe and effective to reverse the hospitalization-associated functional decline in very old patients [71] and to promote functional gains in cognitively impaired frail community-dwellers [72], but its effectiveness to reduce falls and health related-consequences, and whether its combination with cognitive training have added effects remain uncertain.
In this context, the main objective of this study is to evaluate the effectiveness of a combined individualized multicomponent exercise and cognitive training (VIVIFRAIL-COGN) program on the reduction in fall-incidence in a sample of community-dwelling frail older adults with high fall risk, compared to usual care (including the OEP). Secondarily, we will investigate the impact on fall-related consequences, such as need for medical assistance, psychological issues (fear of falling and depression), physical and cognitive capacities and quality of life.
Methods
Study design and setting
The present study is a multicenter randomized clinical trial to be conducted in the Falls Unit of the geriatrics department of four tertiary hospitals in Spain. Its main aim will be to explore the effectiveness of a multicomponent exercise program combined with a cognitive stimulation program in the reduction of falls and related outcomes among frail older adults. Falls units are specialized clinical environments, to which older adults with recurrent falls are referred from Primary Care or other medical specialties. In these Units, falls etiology and potential management are studied by a multi-disciplinary team. Interventions include physical exercise programs, polypharmacy reduction, environmental adequation in accordance with published international and national guidelines [73].
Patients who meet the inclusion criteria for this study will be randomly assigned to usual care or an intervention consisting in the combination of individualized exercise and cognitive stimulation program. Prior to randomization, the attending geriatrician will review the absolute and relative contraindications to participate in exercise programs and will provide general information about the study. Patient recruitment will begin with the normal visit of the patient to the clinic, in which inclusion criteria will be ascertained and informed consent obtained. Later, subjects will be randomly assigned (as explained later) to either the intervention or the usual care (control group).
Study participants and eligibility criteria
The study will include outpatients of the Falls Units of the University Hospital of Navarra in Pamplone, the Hospital of Guadalajara, the Hospital Perpetuo Socorro in Albacete and the Parc Sanitari Pere Virgili in Barcelone (all in Spain) recruited between June 2021 and August 2023. Inclusion criteria include:
-
Age ≥ 75 years or older
-
Referral to the Falls Unit
-
Ability to ambulate independently with or without technical aids
-
Barthel Index ≥ 60
-
Pre-frailty (1–2 criteria) or Frailty according to the Frailty Phenotype by Fried et al. [30]
-
High risk of falling defined by one or more of the following criteria
-
Gait disorders captured through physical performance measures (Time Up and Go Test ≥ 20 s and/or Usual Gait Speed (GS) < 0,8 m/s [74]
-
≥ 2 self-reported falls in the previous year
-
≥ 1 self-reported falls requiring medical assistance in the previous year
-
Relative/caregiver willingness to supervise the exercise/cognitive stimulation sessions
-
Capability and willingness to provide informed consent
Subjects will be excluded from participation based on the following exclusion criteria
-
Unwillingness to either complete the study requirements or to be randomized into the control or the intervention group
-
Life expectancy ≤ 3 months
-
Terminal illness
-
No possibility of follow-up
-
Institutionalization or awaiting institutionalization
-
Major cognitive disorder according to GDS Reisberg (GDS) classification: 5 or higher
-
Severe visual o hearing deprivation
-
Any contraindications for physical exercise or testing procedures, including but not limited to:
-
myocardial infarction in the past 3 months
-
unstable angina pectoris
-
uncontrolled arrhythmia
-
unstable cardiovascular disease or other unstable medical condition
-
uncontrolled arterial hypertension
-
recent pulmonary thromboembolism
-
upper or lower extremity fracture in the past 3 months
Randomization and blinding
Included subjects will be randomized by using a randomization list generated electronically (www.randomizer.org) into the combined intervention group and the usual care group (control group) following a simple randomization procedure, in a 1:1 ratio without restriction. Participants will be explicitly informed and reminded not to disclose their randomization assignment to the assessment team, which will be blinded to the participants’ group membership. It will not be possible to conceal the group assignment from the staff involved in the training of the intervention group. Patients (or their families) will be informed of their random inclusion in one group but will not be informed regarding to which group they belong.
Data collection
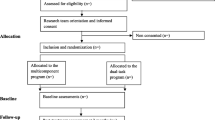
Data from both the combined intervention and the usual care group will be obtained by the research team (physiotherapist, sport sciences specialist and geriatrician) at three different times: at baseline (T0) and at the 6-week (T1) and 12-week (T2) follow-up visits (Fig. 1). A telephone-based follow-up visit, and a review of the electronic clinical chart will be conducted at 6, 9 and 12 months after the start of the participation for gathering data on falls incidence, functional status and exercise continuation (Table 1). All adverse events, including those related to exercise such as muscle pain, fatigue and general aches and pain, will be recorded in an “adverse events diary” during follow-up visits and telephone calls by the training and testing staff, and by self-report during the study period.
The multidisciplinary research team have well-known previous experience in functional geriatric assessment and in the prescription of exercise in frail aged participants in different clinical settings [71, 75, 76].
Sample size and statistics
Study main outcome is the falls rate/year. For its estimation we will use a negative binomial distribution (over-dispersed Poisson distribution). Assuming an alpha error of α = 5%, an average fall rate of 1,8 falls/year in the usual care group and a mean follow-up of 0.9 years, the sample size required for each group will be 129 to have an 80% power to detect a 30% reduction in the one-year fall rate in the combined intervention group. Considering a withdrawal of 20% during the follow-up, the final simple size per group will be 155. Assumptions are based on results from the Actions Seniors Secondary Falls Prevention in Community Senior Fallers Study [77].
All the participant centers have a remarkable clinical activity attending around 1000 patients every year. It is expected than 15% of these patients in every center can be potentially eligible participants. If not reaching the defined sample size, the inclusion period will be extended for a further 3 months.
Baseline characteristics of the sample will be described by using the central tendency (mean and median) and dispersion (standard deviation, standard error, interquartile ranges and confidence intervals) for continuous variables and absolute (counts) and relative (percentages) frequencies for categorical variables. For comparisons between groups at baseline, t tests or Mann–Whitney U tests will be used for continuous variables, upon normality, which will be checked for each using the Kolmogorov–Smirnov test and normal probability plots, and the chi-square test or Fisher’s test will be used for categorical variables.
Main analyses will focus on the detection of differences in the rate of falling between groups. Study main outcome is the fall rate/year. For its estimation we will use a negative binomial regression (Poisson model extension that allows for the presence of overdispersion). Randomization group will be included as the exposure and factors potentially distorting the estimations as covariates. Robust standard errors consistent with heteroskedasticity will be employed by using the “sandwich” package in R (R 3.4.1 (R Core Team, Vienna, Austria). Falls incident rate ratios and their 95% confidence intervals will be estimated by model coefficients and absolute in the rates will be estimated from the results.
Data management
Completed personal data or other documents containing protected personal health information will be kept in a locked file at the principal investigator office in every center. Data will be entered into an electronic de-identified database (RedCap) by authorized study team members and checked for completeness and accuracy. Access to data with identifiers will be restricted to authorized study team members and authorities. Electronic data will be kept on a server regulated by the local research institute (IDISNA).
Data will be destroyed 10 years after study finalization or 5 years after last publication.
Detailed description of the intervention
Usual care group (control group)
Participants randomized to the control group will receive normal outpatient care in the Fall Unit. Briefly, it includes a detailed multidimensional assessment performed by the multidisciplinary team (geriatrician, nurse, physiotherapist, occupational therapist) to identify potential intrinsic and extrinsic factors related with falling. Frequently, causality of falling is multifactorial and interventions in the Falls Units are based on the identification of individual risk factors. General approach includes medical review of high risk of falling medications, nutritional interventions like vitamin D in deficient patients, environmental modifications and prescription of the OEP, deemed the gold-standard exercise program in falls management and therefore, part of the usual care delivered to frail older fallers.
Subjects in this group will partake in a home-based exercise program based on the OEP lasting 12-weeks. A physiotherapist will provide a comprehensive explanation of the program, as well as fall risk, safety and adherence information at the baseline visit and will monitor progression during the study visits. Subjects will be encouraged to perform cardiovascular, strength, flexibility and balance exercises 3-times/week. Both volume and intensity will be adjusted by the physiotherapist based on participant’s self-reported feelings. Subjects will be provided with a booklet with instructions (Additional File 1) and an adherence log (Additional File 2) that will be filled in by the participant or a proxy.
Intervention group (VIVIFRAIL-COGN)
Participants assigned to this group will participate in a 12-week home-based program combining the VIVIFRAIL multicomponent physical exercise and an individualized cognitive training programme (VIVIFRAIL-COGN).
-
B1- Multicomponent VIVIFRAIL exercise group
The multicomponent physical exercise program will be based on the VIVIFRAIL programme which was developed in Europe (Erasmus + programme of the European Union).
The VIVIFRAIL multicomponent exercise intervention program includes individualized sets of resistance training, gait and balance training, which appear to be the best strategy for falls rate reduction in older individuals and to maintaining functional capacity during ageing [78]. This type of intervention has also been proven as the most effective to delay disability, cognitive impairment and depression [79] as well as effective to reverse the functional decline associated with acute hospitalization in very old patients [71]. The VIVIFRAIL exercise program was originally designed with the aim of providing guidance in exercise prescription to professionals managing frail older adults with or without falls older than 70 years [78]. The programme is tailored to the older person’s functional capacity evaluated by the SPPB and a UGS test and the risk of falling, aligning with the new functional-based older adult’s health perception proposed by the WHO [70] Different standardized programs oriented to the functional level of the individual were designed and description of the performance, intensity, volume, frequency and monitoring are described in the materials published. Recently, a new user-friendly simplified version and a simple mobile app with interactive videos have been produced to ease adoption and maximize adherence. (see www.vivifrail.com).
In VIVIFRAIL, subjects are assessed before the start of participation to rule out the presence of any contraindication to exercise (see above). Afterwards, functional capacity is assessed by means of physical performance tests to classify the older individual into one of the four exercise programs proposed. These physical performance tests are the SPPB and the 6-m UGS test (Table 2) with each leading to the recommendation of a certain customized multicomponent physical exercise program (see Table 2). If a high risk of falling is detected by the presence of recurrent falls (≥ 2 falls in the previous year or at least one fall requiring medical attention), reduced performance in the Up-and-Go Test (≥ 20 s) or the UGS (< 0.8 m/s) or a diagnosis of dementia, the balance component of the program is reinforced (indicated by the addition of “ + ” to the program name).
Once the individual has been assigned to an exercise program, they will partake in a 12-week exercise program with a frequency of 3 sessions/week. All the programs in Vivifrail share the following characteristics:
-
Resistance training:
▪ Sets and repetitions
Subjects will be encouraged to perform 3-4 exercises (depending on the program), with a volume of 3 series of 12 repetition. A 1 to 3 minute-break will be encouraged between exercises.
▪ Intensity and progression:
The intensity will be that allowing the completion of all the series with a feeling of moderate effort at the end of each series. Resistance will be adjusted accordingly along the duration of the program.
-
Cardiovascular training:
▪ Volume
Walking activities-based cardiovascular training will be recommended to improve cardiorespiratory fitness. Depending on the functional capacity of the individuals, walking bouts ranging from 5-10 seconds to 45 minutes will be prescribed.
▪ Intensity and progression
Subjects will be instructed to maintain a moderate effort during walking bouts and to progressively increase both the duration and the cost of walking.
-
Balance training:
Balance training will include both static and dynamic exercises adapted to individual abilities of the person.
▪ Volume
During static exercises, subjects will be instructed to remain in the same position for ten seconds in different conditions (one-foot stand, semi-tandem stand with eyes open/closed or in unstable surfaces). After resting, they will repeat three times.
In the case of dynamic exercises, subjects will perform different tasks (walking over obstacles, in different directions, paying attention to external stimulus…) in different conditions that should challenge their balance by demanding postural corrections. They will repeat the task 2-3 times.
In the case of the presence of high risk of falling (see above) the number, frequency and volume of balance exercises is increased.
▪ Intensity and progression
Subjects will progress towards more challenging situations (both in terms of feature of the exercises, difficulty or conditions) when current exercises do not require enough effort from them.
Safety recommendations will be provided to prevent falls during balance exercises.
-
Flexibility
Subjects will be instructed to perform a series of stretching exercises at the end of the sessions.
▪ Volume
They will perform 2-3 stretching exercises, with 2-3 repetitions per exercise lasting 10 seconds. They will be told to stretch until they feel a bit of tension and remain in the same position without discomfort.
Materials will be provided to allow correct execution and progression of the exercises and to maximize adherence. The latest Vivifrail update includes a passport-like booklet that allows to follow the session and have access to the graphical and textual descriptions of the exercises, as well as information relative to volume, frequency, intensity, and duration. In addition, it includes a section for registering adherence and the adherence log, respectively (see www.vivifrail.com).
During the baseline visit, the participant and a proxy will be informed about the features of the program and potential side effects, as well as safety and adherence measures and booklet functioning. The research team will also provide adaptable ankle weights.
-
B2-Cognitive training
The cognitive training program will last 12 weeks as well and will consist in twice weekly sessions combined with the above-mentioned physical exercise program (Table 3). Before the start of the intervention, cognitive status will be assessed through a global cognition test -Montreal Cognitive Test (MoCA) [80]- in order to individualize cognitive training exercises with the aim of maximizing benefits. The MoCA is a screening test with scores from 0 (worse cognitive function) to 30 (better cognitive function) and assesses different cognitive functions (including executive functions). In addition, adds other type of tasks as the clock test, a part of the Trail Making Test (part B), verbal fluency and denomination, items normally evaluated in a general assessment of cognition. For all these reasons the MoCA test is consider a more complete and sensitive screening test in older adults to monitor intervention than Mini-mental State Examination( MMSE) [81].
Based on the score of the MoCA and normative values in the Spanish population over 75 [81] years old, subjects will receive an intervention from the following:
-
Program A. MoCA 26–30. High cognitive performance. Normal cognitive function
-
Program B. MoCA 20–25. Intermediate cognitive performance. No evidence of clinical cognitive decline
-
Program C. MoCA 13–19. Low cognitive performance. Mild cognitive decline
-
Program D. MoCA ≤ 12. Very low cognitive performance. Mild dementia
In every session a combination of one exercise from Set A (attentional activities) and one exercise from Set B (executive function activities) will be performed (see Table 3). An initial training session will be performed to explain the programme to the participants and their relatives or caregiver (the support of one person during sessions will be needed due to characteristics of the cognitive training exercises).
To guarantee adherence to the program and appropriate execution of cognitive training exercises, a videoconference session will be performed at week 3 and 9 of the program by the occupational therapists. The purpose of this monitoring is to resolve doubts, adapt difficulty and provide support.
Either the participant and the companion will be instructed in the general and individual characteristics of both physical and cognitive programs (VIVIFRAIL-COGN). Also, all participants will receive instructions, printed materials and audiovisual support of the cognitive sessions with the VIVIFRAIL-COGN material.
Table 4 shows the recommended distribution of both the physical and cognitive components of the intervention. Adherence to the cognitive training program will be registered together with the exercise in the VIVIFRAIL booklet.
Outcome measures
Primary outcome
The primary outcome is the change in the number of auto-reported falls during the study period. Falls, number of falls and its consequences will be registered by the participants /relatives /caregivers with a diary register according with ProFANE group (Prevention of Falls Network Europe) recommendations on reporting of fall prevention programs’ outcomes [62, 82]. Participants/relatives/caregivers will be instructed to use the diary register (Additional File 3) and will be reviewed by the investigator team during T0, T1 and T2 assessments. During follow-up (6, 9 and 12 months after the start of the intervention) a telephone call and a review of the electronic clinical chart will be conducted to register falls and associated events.
Secondary outcomes
The secondary measures will be assessments that evaluate fall-related constructs such as fall-related healthcare system utilization, cognitive and physical capacities, psychological and muscle size and quality by echography. Additionally, instrumented measurements of frailty-related kinematic parameters will be performed during the physical performance measures by using inertial sensors (Table 1).
Fall-related outcomes
In addition to fall occurrence along 1-year follow-up, in this study, we will assess a set of core outcomes recommended by the ProFANE initiative and that have been poorly reported in previous studies [68, 82]. During follow-up and telephone visits, fall-related healthcare system use (contacts, admissions, emergency visits) and central/peripheral fall-related fracture (radiologically confirmed) will be ascertained and later confirmed by medical records check. In addition, fall related psychological consequences will be assessed through the assessment of the presence of fear of falling [83]. Health-related quality of life (HRQoL) will be measured through the Spanish version of the EuroQoL-5D [84]. Physical activity levels will be evaluated through the Spanish version of the Brief Physical Activity questionnaire [85].
Fall risk
An increased risk of falling will be considered according to national and international recommendations (one or more of the following criteria): 2 or more falls or 1 fall with medical attention in the last twelve months or a significative gait disorder assessed by performance tests (TUG > 20 s and or UGS test < 0.8 m/s) [14, 86]. The TUG test is a classic test to assess risk of falls. Participant must raise from a chair without help, walk three meters, turn back and sit again. A time of > 20 s is indicative high risk of falls [87].
Physical function endpoints
Physical function of the participants will be evaluated by the SPPB [88], which evaluates, balance, gait ability and leg strength using a single tool. Total score ranges from 0 (worst) to 12 points (best). The SPPB validity for frailty screening and predicting disability, institutionalization and mortality. A total score of less than 10 is deemed indicative of frailty and a high risk of disability and falls. A 1-point change in SPPB is deemed a meaningful clinical change [89].
Isometric handgrip strength will be measured using a manual dynamometer in two attepms in both dominant and non-dominants hands. The best of both will be recorded. Handgrip asimmetry has recently been proposed as a early marker of future falls [90].
Maximal dynamic lower limb strength (in kilograms) will beassessed using the 1 repetition maximum (1RM) test in the bilateral leg press exercise using exercise machines (Matrix, Johnson Health Tech, Ibérica, S.L., Torrejón de Ardoz, Spain; and Exercycle S.L., BH Group, Vitoria, Spain). In the first assessment, subjects will be instructed on the exercise execution and they will warm-up with specific movements for the leg press. Subject’s maximal load will be established in no more than five attempts, with a recovery period lasting 3 min between attempts. After the 1RM values are determined, the maximal power output will be measured (in watts) by the performance of 10 repetitions at maximal velocity at an intensity of 50% of 1RM by using a linear velocity transducer connected to the weight plates (Vitruve linear Encoder System,Vitoria, Spain). During all neuromuscular performance tests, strong verbal encouragement will be given to each subject to motivate them to perform each test actionas optimally and rapidly as possible.
Sarcopenia-related measures
Sarcopenia clinical probability will be measured using the definition proposed by the European Working Group on Sarcopenia in Older People (EWGSOP) [91]. In these criteria clinical suspiction is present in subjects with a > 4 in the SARC-F scale, and probable sarcopenia is confirmed with a 5-repetition chair test time > 15 s or a dominant handgrip strength < 27 kg in men or < 16 kg in women. Muscle quality (echo-intensity) and size (muscle thickness) of the rectus anterior muscle and eminence thenar will be assessed with a portable ultrasound system (Philips Healthcare Lumify C5-2 Transductor, Philips Ultrasound, Bothell, WA,USA) operated by a trained member of the researcher’s team [92].
Fracture risk
Risk of fracture will be assessed with the Garvan fracture risk calculator (https://www.garvan.org.au). This tool allows to estimate 5- and 10-years fracture risk by equations based on anthropometric data, previous fractures since the age of 50, falls in the last year and optionally bone mineral density data. It has been validated very recently in Spanish population [93].
Neuropsychological assessment
The MoCA [80] test will be used to assess changes in cognitive function and to individualize cognitive intervention. MoCA has been explained in detail before (see paragraph B2). The Trail Making Test (TMT), part A, will be used to assess executive function. In TMT-A, the participant is asked to connect randomly arranged circles containing numbers from 1 to 25 following the number sequence, and doing it as quickly as possible [94]. Mood will be assessed through the Yesavage GDS [95], a 15-item scale used to screen for depressive symptoms in older adults.
Dual-task GS
Worsening of the performance in the GS while performing a dual-task test (dual-task cost) may be early predictors of fall risk, and may be useful tools for functional evaluations in frail older patients. The dual-task paradigm will be used in the 5-m usual GS. Two trials will be conducted to assess GS while the patient is performing a verbal fluency and a counting task (verbal GS and arithmetic GS, respectively) [96, 97]. Participants will be instructed to walk one trial over 5-m as a single-task.
During the verbal dual-task condition (verbal GS), we will measure GS while participants are naming animals aloud. During the arithmetic dual task condition (arithmetic GS), we will assess GS while participants are counting backwards aloud from 100 in ones. Besides the dual task-cost (relative increase in time to complete the 5-m walk under dual-task conditions with respect to single-task), the cognitive accuracy will be measured by counting the number of animals named (dual-task with verbal performance) or determining how many numbers were correctly counted backwards (dual-task with arithmetic performance).
Kinematic parameters assessment
During functional tasks (such as balance, gait and rising from a chair) and dual task walk, an inertial sensor unit (XSENS, Xsens Technologies B.V. Enschede, Netherlands) will be attached over the lumbarspine (L3) to record raw acceleration data. Afterwards, the raw signal we be processed to compute kinematic parameters related to physical frailty [98,99,100] by using the software designed by Movalys (Movalsys SL, Pamplona, Spain).
Study protocol
The protocol employs relevant standard protocol items for clinical trials according to the SPIRIT 2013 statement (Additional File 4) [29] and follows the CONSORT statement [30] for transparent reporting. The trial is registered at ClinicalTrials.gov (ID number NCT04911179), and the status is on recruitment.
Discussion
The main objective of the proposed study is to assess the efficacy of VIVIFRAIL-COGN, a program that combines the individualized multicomponent exercise plan-VIVIFRAIL- with an individualized cognitive training focused on improving executive function to reduce auto-reported falls rates and risk of falling, compared with a standard intervention. To our knowledge, this is the first trial that will investigate the direct effect of combined physical exercise with cognitive training on falls in a frail population of older persons with high risk of falling.
We have just started the decade of Healthy Ageing 2020–2030, an important opportunity to bring together governments, civil society, international agencies, professionals, academia, the media, and the private sector for ten years of concerted, catalytic and collaborative action to improve the lives of older people, their families, and the communities in which they live [101]. Healthy ageing is defined by the World Health Organization (WHO) as the maintaining of functional capacity, recently renamed as intrinsic capacity, as the central objective and focus of all health systems and policies for elderly populations [70]. Among 10 priority strategies to develop in this decade, WHO highlights (priority 4) to promote research that addresses the current and future needs of older people [102]. Our study is perfectly aligned with this strategy. Actually, falls constitute an extraordinary prevalent geriatric syndrome. Globally, a third of people aged 65 years and older fall at least once per year, with 5% of these falls resulting in a fracture [103]. WHO considers falling as a major public health problem and points out the importance to prioritize specific research [104]. Thus, the clinical impact of our study can be significant given its potential to help change the actual healthcare paradigm of frail patients to a more centered and functional perspective.
Nowadays healthcare actions to prevent falls in frail older persons with high risk of falling remain scarce, isolated and usually fragmented, despite the efforts that are being made by policymakers, reflected in the recent availability of evidence-based public national/international recommendations [12, 73, 86]. In those recommendations, physical exercise appears as the most evaluated intervention. It is very well known that it is an effective and safe intervention to reduce risk and rate of falls [37, 41, 42]. Our research group very recently showed that the VIVIFRAIL program (www.vivifrail.com) [75] is feasible and effective to improve functional capacity in frail older persons with cognitive problems [72] but we did not explore its potential in falls prevention. It is possible that more integrated and multidomain interventions, as proposed in the present study protocol, are needed in the case of frail older persons. Specifically, if our hypothesis is correct and we show that VIVIFRAIL-COGN intervention is more effective in terms of rate, risk of falls and functional improvement in this population, a new therapeutic window is opened: falls and risk of falls may be improved (and potentially the burdensome consequences of falls, such as fractures) through combined physical-cognitive interventions.
One of the strengths of our study is the multidisciplinary nature of the project (geriatricians, physiotherapists, occupational therapists, psychologists, nurses). This is a remarkable opportunity to establish new protocols and share our results with the scientific community and healthcare professionals with interest in frail older persons with high risk of falling.
Another important aspect of our study is the non-exclusion of frail older patients with cognitive problems. Falls are very prevalent in cognitive decline frail older persons and cognitive decline it is a very well-known risk factor of falling and fractures. The non-exclusion of frail participants with high risk of falling and cognitive problems improves external validity and makes the trial unique in comparison with previous trials in this research area.
In summary, this trial will provide new evidence about the effectivity of an individualized multidomain interventions on falls by studying the effect of additive effects of cognitive training and physical exercise to prevent falls in older frail persons with high risk of falling.
Dissemination
We will disseminate the results of our study via presentations at international conferences and articles in peer reviewed journals. The study will be carried out and reported in following the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) guidelines.
Future directions
This project offers the opportunity to test a novel multidomain intervention (VIVIFRAIL-COGN). Following the VIVIFRAIL methodology of individualize physical exercise prescription according to functional status , this intervention is a step forward to prescribe more individualized and person-centered interventions of frail older persons with high risk of falling. We expect to translate this methodology to others Falls Units in Spain and in the next future disseminate this integrative and novel model to other clinical geriatric and non-geriatric units attending these patients. Finally, we expect to translate our model to rutinary clinical practice and as a global strategy to implement in the Spanish Governmental Strategy of Falls and Frailty.
Trial status
The trial began recruitment in July 2021 and is currently open for recruitment. Recruitment will cease when 310 participants have been randomized. It is anticipated that this target will be reached by September 2023.
Availability of data and materials
Individual deidentified participant data (including data dictionaries) that underline the results reported in this article (text, tables, figures and appendices) will be shared. Other documents as Study Protocol, Statistical Analysis Plan and Analytic code will be available. Data will be become available beginning 3 months and ending 5 years following article publication. Access criteria data will be shared to researchers who provide a methodologically sound proposal to achieve aims in the in the approval proposal. Proposals should be directed to alvaro.casas.herrero@navarra.es. Data are available for 5 years at a thirdly party website ( www.idisina.es).
Change history
19 January 2023
A Correction to this paper has been published: https://doi.org/10.1186/s12877-022-03535-0
Abbreviations
- BI:
-
Barthel Index
- EQ-5D:
-
EuroQoL-5D
- EWGSOP:
-
European Working Group on Sarcopenia in Older People
- GDS:
-
Geriatric Depression Scale
- GS:
-
Gait Speed
- HR-QoL:
-
Health-related Quality of Life
- MNA:
-
Mini-Nutritional Assessment
- MoCA:
-
Montreal Cognitive Assessment
- MMSE:
-
Mini-Mental State Examination
- OEP:
-
Otago Exercise Program
- ProFANE:
-
Prevention of Falls in Europe
- RM:
-
Repetition Maximum
- SPPB:
-
Short Physical Performance Battery
- STAC:
-
Síndrome de Temor a Caerse
- TMT:
-
Trail Making Test
- TUG:
-
Up-and-Go Test
- UGS:
-
Usual Gait Speed
- WHO:
-
World Health Organization
References
Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35 Suppl 2:ii37-41.
O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137(3):342–54.
Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Falls prevention over 2 years: a randomized controlled trial in women 80 years and older. Age Ageing. 1999;28(6):513–8.
Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–7.
Haagsma JA, Olij BF, Majdan M, van Beeck EF, Vos T, Castle CD, et al. Falls in older aged adults in 22 European countries: incidence, mortality and burden of disease from 1990 to 2017. Inj Prev. 2020;26(Suppl 2):i67-74.
Trevisan C, Ripamonti E, Grande G, Triolo F, Ek S, Maggi S, et al. The Association Between Injurious Falls and Older Adults’ Cognitive Function: The Role of Depressive Mood and Physical Performance. J Gerontol A Biol Sci Med Sci. 2021;76(9):1699–706.
Stenhagen M, Ekström H, Nordell E, Elmståhl S. Accidental falls, health-related quality of life and life satisfaction: a prospective study of the general elderly population. Arch Gerontol Geriatr. 2014;58(1):95–100.
Gill TM, Murphy TE, Gahbauer EA, Allore HG. Association of injurious falls with disability outcomes and nursing home admissions in community-living older persons. Am J Epidemiol. 2013;178(3):418–25.
World Population Prospects 2019: Data Booklet. [cited 2020 Mar 17]. Available from: https://www.un-ilibrary.org/population-and-demography/world-population-prospects-2019-data-booklet_3e9d869f-en
Davis JC, Robertson MC, Ashe MC, Liu-Ambrose T, Khan KM, Marra CA. International comparison of cost of falls in older adults living in the community: a systematic review. Osteoporos Int. 2010;21(8):1295–306.
WHO global report on falls prevention in older age. [cited 2022 Feb 9]. Available from: https://www.who.int/publications-detail-redirect/9789241563536
Montero-Odasso MM, Kamkar N, Pieruccini-Faria F, Osman A, Sarquis-Adamson Y, Close J, et al. Evaluation of Clinical Practice Guidelines on Fall Prevention and Management for Older Adults: A Systematic Review. JAMA Netw Open. 2021;4(12): e2138911.
Hopewell S, Adedire O, Copsey BJ, Boniface GJ, Sherrington C, Clemson L, et al. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2018;7:CD012221.
Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–57.
Rivan NFM, Singh DKA, Shahar S, Wen GJ, Rajab NF, Din NC, et al. Cognitive frailty is a robust predictor of falls, injuries, and disability among community-dwelling older adults. BMC Geriatr. 2021;25(21):593.
Yuan J-L, Zhao R-X, Ma Y-J, Li X-D, Zhou X-M, Wang X-F, et al. Prevalence/potential risk factors for motoric cognitive risk and its relationship to falls in elderly Chinese people: a cross-sectional study. Eur J Neurol. 2021;28(8):2680–7.
Enderlin C, Rooker J, Ball S, Hippensteel D, Alderman J, Fisher SJ, et al. Summary of factors contributing to falls in older adults and nursing implications. Geriatr Nurs. 2015;36(5):397–406.
Menant JC, Weber F, Lo J, Sturnieks DL, Close JC, Sachdev PS, et al. Strength measures are better than muscle mass measures in predicting health-related outcomes in older people: time to abandon the term sarcopenia? Osteoporos Int. 2017;28(1):59–70.
Deandrea S, Bravi F, Turati F, Lucenteforte E, La Vecchia C, Negri E. Risk factors for falls in older people in nursing homes and hospitals. A systematic review and meta-analysis. Arch Gerontol Geriatr. 2013;56(3):407–15.
Lusardi MM, Fritz S, Middleton A, Allison L, Wingood M, Phillips E, et al. Determining Risk of Falls in Community Dwelling Older Adults: A Systematic Review and Meta-analysis Using Posttest Probability. J Geriatr Phys Ther. 2017;40(1):1–36.
Herman T, Mirelman A, Giladi N, Schweiger A, Hausdorff JM. Executive Control Deficits as a Prodrome to Falls in Healthy Older Adults: A Prospective Study Linking Thinking, Walking, and Falling. J Gerontol A Biol Sci Med Sci. 2010;65A(10):1086–92.
Zhang C, Dong X, Ding M, Chen X, Shan X, Ouyang H, et al. Executive Control, Alerting, Updating, and Falls in Cognitively Healthy Older Adults. Gerontology. 2020;66(5):494–505.
Booth V, Hood V, Kearney F. Interventions incorporating physical and cognitive elements to reduce falls risk in cognitively impaired older adults: a systematic review. JBI Database System Rev Implement Rep. 2016;14(5):110–35.
Blair C. Educating executive function. Wiley Interdiscip Rev Cogn Sci. 2017 Jan;8(1–2).
Brown TI, Chrastil ER. Editorial: Spatial Navigation: Memory Mechanisms and Executive Function Interactions. Front Hum Neurosci. 2019;13:202.
Yogev-Seligmann G, Hausdorff JM, Giladi N. The role of executive function and attention in gait. Mov Disord. 2008;23(3):329–42 quiz 472.
Holtzer R, Verghese J, Xue X, Lipton RB. Cognitive processes related to gait velocity: results from the Einstein Aging Study. Neuropsychology. 2006;20(2):215–23.
Hausdorff JM, Schweiger A, Herman T, Yogev-Seligmann G, Giladi N. Dual-task decrements in gait: contributing factors among healthy older adults. J Gerontol A Biol Sci Med Sci. 2008;63(12):1335–43.
Montero-Odasso M, Verghese J, Beauchet O, Hausdorff JM. Gait and cognition: a complementary approach to understanding brain function and the risk of falling. J Am Geriatr Soc. 2012;60(11):2127–36.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146-156.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–95.
Angulo J, El Assar M, Rodríguez-Mañas L. Frailty and sarcopenia as the basis for the phenotypic manifestation of chronic diseases in older adults. Mol Aspects Med. 2016;50:1–32.
Kojima G. Frailty as a Predictor of Future Falls Among Community-Dwelling Older People: A Systematic Review and Meta-Analysis. J Am Med Dir Assoc. 2015;16(12):1027–33.
Ge M-L, Simonsick EM, Dong B-R, Kasper JD, Xue Q-L. Frailty, With or Without Cognitive Impairment, Is a Strong Predictor of Recurrent Falls in a US Population-Representative Sample of Older Adults. J Gerontol A Biol Sci Med Sci. 2021;76(11):e354–60.
Chittrakul J, Siviroj P, Sungkarat S, Sapbamrer R. Multi-System Physical Exercise Intervention for Fall Prevention and Quality of Life in Pre-Frail Older Adults: A Randomized Controlled Trial. Int J Environ Res Public Health. 2020 May [cited 2022 Feb 9];17(9). Available from: https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC7246743/
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012 Sep 12;(9):CD007146.
García-Hermoso A, Ramirez-Vélez R, Sáez de Asteasu ML, Martínez-Velilla N, Zambom-Ferraresi F, Valenzuela PL, et al. Safety and Effectiveness of Long-Term Exercise Interventions in Older Adults: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Sports Med. 2020;50(6):1095–106.
Rossi PG, Carnavale BF, Farche ACS, Ansai JH, de Andrade LP, Takahashi AC de M. Effects of physical exercise on the cognition of older adults with frailty syndrome: A systematic review and meta-analysis of randomized trials. Arch Gerontol Geriatr. 2021;93:104322.
Giné-Garriga M, Roqué-Fíguls M, Coll-Planas L, Sitjà-Rabert M, Salvà A. Physical Exercise Interventions for Improving Performance-Based Measures of Physical Function in Community-Dwelling, Frail Older Adults: A Systematic Review and Meta-Analysis. Arch Phys Med Rehabil. 2014;95(4):753-769.e3.
Sáez de Asteasu ML, Martínez-Velilla N, Zambom-Ferraresi F, Casas-Herrero Á. Role of physical exercise on cognitive function in healthy older adults: A systematic review of randomized clinical trials. Ageing Res Rev. 2017;37:117–34.
Tricco AC, Thomas SM, Veroniki AA, Hamid JS, Cogo E, Strifler L, et al. Comparisons of Interventions for Preventing Falls in Older Adults: A Systematic Review and Meta-analysis. JAMA. 2017;318(17):1687–99.
Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;1:CD012424.
de Souto BP, Rolland Y, Vellas B, Maltais M. Association of Long-term Exercise Training With Risk of Falls, Fractures, Hospitalizations, and Mortality in Older Adults: A Systematic Review and Meta-analysis. JAMA Intern Med. 2019;179(3):394–405.
Kendrick D, Kumar A, Carpenter H, Zijlstra GAR, Skelton DA, Cook JR, et al. Exercise for reducing fear of falling in older people living in the community. Cochrane Database Syst Rev. 2014 Nov 28;(11):CD009848.
Tyrovolas S, Koyanagi A, Lara E, Santini ZI, Haro JM. Mild cognitive impairment is associated with falls among older adults: Findings from the Irish Longitudinal Study on Ageing (TILDA). Exp Gerontol. 2016;75:42–7.
Bahar-Fuchs A, Clare L, Woods B. Cognitive training and cognitive rehabilitation for persons with mild to moderate dementia of the Alzheimer’s or vascular type: a review. Alzheimers Res Ther. 2013;5(4):35.
Segev-Jacubovski O, Herman T, Yogev-Seligmann G, Mirelman A, Giladi N, Hausdorff JM. The interplay between gait, falls and cognition: can cognitive therapy reduce fall risk? Expert Rev Neurother. 2011;11(7):1057–75.
Nouchi R, Taki Y, Takeuchi H, Sekiguchi A, Hashizume H, Nozawa T, et al. Four weeks of combination exercise training improved executive functions, episodic memory, and processing speed in healthy elderly people: evidence from a randomized controlled trial. Age (Dordr). 2014;36(2):787–99.
Phirom K, Kamnardsiri T, Sungkarat S. Beneficial Effects of Interactive Physical-Cognitive Game-Based Training on Fall Risk and Cognitive Performance of Older Adults. Int J Environ Res Public Health. 2020;17(17):E6079.
Fabre C, Chamari K, Mucci P, Massé-Biron J, Préfaut C. Improvement of cognitive function by mental and/or individualized aerobic training in healthy elderly subjects. Int J Sports Med. 2002;23(6):415–21.
Halvarsson A, Franzén E, Ståhle A. Balance training with multi-task exercises improves fall-related self-efficacy, gait, balance performance and physical function in older adults with osteoporosis: a randomized controlled trial. Clin Rehabil. 2015;29(4):365–75.
Fabel K, Wolf SA, Ehninger D, Babu H, Leal-Galicia P, Kempermann G. Additive Effects of Physical Exercise and Environmental Enrichment on Adult Hippocampal Neurogenesis in Mice. Frontiers in Neuroscience. 2009 [cited 2022 Feb 9];3. Available from: https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC2858601/
Train the Brain Consortium. Randomized trial on the effects of a combined physical/cognitive training in aged MCI subjects: the Train the Brain study. Sci Rep. 2017;3(7):39471.
Lipardo DS, Tsang WW. Effects of combined physical and cognitive training on fall prevention and risk reduction in older persons with mild cognitive impairment: a randomized controlled study. Clin Rehabil. 2020;34(6):773–82.
Lipardo DS, Aseron AMC, Kwan MM, Tsang WW. Effect of Exercise and Cognitive Training on Falls and Fall-Related Factors in Older Adults With Mild Cognitive Impairment: A Systematic Review. Arch Phys Med Rehabil. 2017;98(10):2079–96.
Turunen KM, Tirkkonen A, Savikangas T, Hänninen T, Alen M, Fielding RA, et al. Effects of Physical and Cognitive Training on Falls and Concern about Falling in Older Adults: Results from a Randomized Controlled Trial. J Gerontol A Biol Sci Med Sci. 2021 Dec 15;glab375.
Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997;315(7115):1065–9.
Chiu H-L, Yeh T-T, Lo Y-T, Liang P-J, Lee S-C. The effects of the Otago Exercise Programme on actual and perceived balance in older adults: A meta-analysis. PLoS ONE. 2021;16(8): e0255780.
Jahanpeyma P, Kayhan Koçak FÖ, Yıldırım Y, Şahin S, Şenuzun AF. Effects of the Otago exercise program on falls, balance, and physical performance in older nursing home residents with high fall risk: a randomized controlled trial. Eur Geriatr Med. 2021;12(1):107–15.
Martins AC, Guia D, Saraiva M, Pereira T. Effects of A ‘Modified’ Otago Exercise Program on the Functional Abilities and Social Participation of Older Adults Living in the Community-The AGA@4life Model. Int J Environ Res Public Health. 2020;17(4):E1258.
Aranda-Reneo I, Albornos-Muñoz L, Rich-Ruiz M, Cidoncha-Moreno MÁ, Pastor-López Á, Moreno-Casbas T, et al. Cost-Effectiveness of an Exercise Programme That Provided Group or Individual Training to Reduce the Fall Risk in Healthy Community-Dwelling People Aged 65–80: A Secondary Data Analysis. Healthcare (Basel). 2021;9(6):714.
Skelton DA, Becker C, Lamb SE, Close JCT, Zijlstra W, Yardley L, et al. Prevention of Falls Network Europe: a thematic network aimed at introducing good practice in effective falls prevention across Europe. Eur J Ageing. 2004;1(1):89–94.
Ángeles CMM, Laura AM, Consuelo CSM, Manuel RR, Eva AC, Covadonga GPA, et al. The effect that the Otago Exercise Programme had on fear of falling in community dwellers aged 65–80 and associated factors. Arch Gerontol Geriatr. 2022;99.
Bjerk M, Brovold T, Skelton DA, Liu-Ambrose T, Bergland A. Effects of a falls prevention exercise programme on health-related quality of life in older home care recipients: a randomised controlled trial. Age Ageing. 2019;48(2):213–9.
Albornos-Muñoz L, Moreno-Casbas MT, Sánchez-Pablo C, Bays-Moneo A, Fernández-Domínguez JC, Rich-Ruiz M, et al. Efficacy of the Otago Exercise Programme to reduce falls in community-dwelling adults aged 65–80 years old when delivered as group or individual training. J Adv Nurs. 2018;74(7):1700–11.
Benavent-Caballer V, Rosado-Calatayud P, Segura-Orti E, Amer-Cuenca JJ, Lison JF. Effects of three different low-intensity exercise interventions on physical performance, muscle CSA and activities of daily living: a randomized controlled trial. Exp Gerontol. 2014;58:159–65.
Pettersson B, Lundin-Olsson L, Skelton DA, Liv P, Zingmark M, Rosendahl E, et al. Effectiveness of a self-managed digital exercise programme to prevent falls in older community-dwelling adults: study protocol for the Safe Step randomised controlled trial. BMJ Open. 2020;10(5): e036194.
Copsey B, Hopewell S, Becker C, Cameron ID, Lamb SE. Appraising the uptake and use of recommendations for a common outcome data set for clinical trials: a case study in fall injury prevention. Trials. 2016;17(1):131.
Izquierdo M, Rodriguez-Mañas L, Sinclair AJ. Editorial: What Is New in Exercise Regimes for Frail Older People - How Does the Erasmus Vivifrail Project Take Us Forward? J Nutr Health Aging. 2016;20(7):736–7.
WHO | World report on ageing and health 2015. WHO. World Health Organization; [cited 2021 Feb 10]. Available from: http://www.who.int/ageing/events/world-report-2015-launch/en/
Martínez-Velilla N, Casas-Herrero A, Zambom-Ferraresi F, Sáez de Asteasu ML, Lucia A, Galbete A, et al. Effect of Exercise Intervention on Functional Decline in Very Elderly Patients During Acute Hospitalization: A Randomized Clinical Trial. JAMA Intern Med. 2019 01;179(1):28–36.
Casas-Herrero Á, Sáez de Asteasu ML, Antón-Rodrigo I, Sánchez-Sánchez JL, Montero-Odasso M, Marín-Epelde I, et al. Effects of Vivifrail multicomponent intervention on functional capacity: a multicentre, randomized controlled trial. J Cachexia Sarcopenia Muscle. 2022 Feb 11;
4 The Guideline Development Group, Internal Clinical Guidelines Team, and NICE project team 2013 | Falls in older people: assessing risk and prevention | Guidance | NICE [Internet]. NICE; [cited 2022 Feb 9]. Available from: https://www.nice.org.uk/guidance/cg161/chapter/4-the-guideline-development-group-internal-clinical-guidelines-team-and-nice-project-team-2013
Abellan van Kan G, Rolland Y, Andrieu S, Bauer J, Beauchet O, Bonnefoy M, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009 Dec;13(10):881–9.
Casas-Herrero A, Anton-Rodrigo I, Zambom-Ferraresi F, Sáez de Asteasu ML, Martinez-Velilla N, Elexpuru-Estomba J, et al. Effect of a multicomponent exercise programme (VIVIFRAIL) on functional capacity in frail community elders with cognitive decline: study protocol for a randomized multicentre control trial. Trials. 2019 Jun 17;20(1):362.
Billot M, Calvani R, Urtamo A, Sánchez-Sánchez JL, Ciccolari-Micaldi C, Chang M, et al. Preserving Mobility in Older Adults with Physical Frailty and Sarcopenia: Opportunities, Challenges, and Recommendations for Physical Activity Interventions. Clin Interv Aging. 2020;15:1675.
Liu-Ambrose T, Davis JC, Best JR, Dian L, Madden K, Cook W, et al. Effect of a Home-Based Exercise Program on Subsequent Falls Among Community-Dwelling High-Risk Older Adults After a Fall: A Randomized Clinical Trial. JAMA. 2019;321(21):2092–100.
Izquierdo M. [Multicomponent physical exercise program: Vivifrail]. Nutr Hosp. 2019 Jul 1;36(Spec No2):50–6.
Tarazona-Santabalbina FJ, Gómez-Cabrera MC, Pérez-Ros P, Martínez-Arnau FM, Cabo H, Tsaparas K, et al. A Multicomponent Exercise Intervention that Reverses Frailty and Improves Cognition, Emotion, and Social Networking in the Community-Dwelling Frail Elderly: A Randomized Clinical Trial. J Am Med Dir Assoc. 2016;17(5):426–33.
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9.
Ojeda N, del Pino R, Ibarretxe-Bilbao N, Schretlen DJ, Peña J. Test de evaluación cognitiva de Montreal: normalización y estandarización de la prueba en población española. Revista de Neurología. 2016;63(11):488–96.
Lamb SE, Jørstad-Stein EC, Hauer K, Becker C, Prevention of Falls Network Europe and Outcomes Consensus Group. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005 Sep;53(9):1618–22.
Olmos Zapata P, Abad Mateos MÁ, Pérez-Jara J. Síndrome de temor a caerse en personas mayores de 65 años con mareos de repetición: estudio descriptivo. Rev Esp Geriatr Gerontol. 2010;45(5):274–7.
Badia X, Roset M, Montserrat S, Herdman M, Segura A. [The Spanish version of EuroQol: a description and its applications. European Quality of Life scale]. Med Clin (Barc). 1999;112 Suppl 1:79–85.
Puig-Ribera A, Martín-Cantera C, Puigdomenech E, Real J, Romaguera M, Magdalena-Belio JF, et al. Screening Physical Activity in Family Practice: Validity of the Spanish Version of a Brief Physical Activity Questionnaire. PLoS ONE. 2015;10(9): e0136870.
Ministerio de Sanidad - Profesionales - ESTRATEGIA DE PROMOCION DE LA SALUD Y PREVENCION - FRAGILIDAD Y CAIDAS - PERSONA MAYOR [Internet]. [cited 2022 Feb 9]. Available from: https://www.sanidad.gob.es/profesionales/saludPublica/prevPromocion/Estrategia/Fragilidadycaidas.htm
[Frailty detection and prevention: a new challenge in elderly for dependence prevention] - PubMed [Internet]. [cited 2022 Feb 9]. Available from: https://pubmed.ncbi.nlm.nih.gov/19592045/
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85-94.
Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55(4):M221-231.
McGrath R, Clark BC, Cesari M, Johnson C, Jurivich DA. Handgrip strength asymmetry is associated with future falls in older Americans. Aging Clin Exp Res. 2021;33(9):2461–9.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412–23.
Perkisas S, Bastijns S, Baudry S, Bauer J, Beaudart C, Beckwée D, et al. Application of ultrasound for muscle assessment in sarcopenia: 2020 SARCUS update. Eur Geriatr Med. 2021;12(1):45–59.
Reyes Domínguez AI, Sosa Cabrera N, Saavedra Santana P, Gómez de Tejada Romero MJ, Jódar Gimeno E, Sosa Henríquez M, et al. Valoración de la capacidad predictiva de la calculadora Garvan del riesgo de fractura a 10 años en una población española. Revista de Osteoporosis y Metabolismo Mineral. 2017 Jun;9(2):55–61.
Llinàs-Reglà J, Vilalta-Franch J, López-Pousa S, Calvó-Perxas L, Torrents Rodas D, Garre-Olmo J. The Trail Making Test. Assessment. 2017;24(2):183–96.
Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982 1983;17(1):37–49.
Beauchet O, Annweiler C, Dubost V, Allali G, Kressig RW, Bridenbaugh S, et al. Stops walking when talking: a predictor of falls in older adults? Eur J Neurol. 2009;16(7):786–95.
Lundin-Olsson L, Nyberg L, Gustafson Y. ‘Stops walking when talking’ as a predictor of falls in elderly people. Lancet. 1997;349(9052):617.
Martinikorena I, Martínez-Ramírez A, Gómez M, Lecumberri P, Casas-Herrero A, Cadore EL, et al. Gait Variability Related to Muscle Quality and Muscle Power Output in Frail Nonagenarian Older Adults. J Am Med Dir Assoc. 2016;17(2):162–7.
Millor N, Lecumberri P, Gomez M, Martinez-Ramirez A, Izquierdo M. Kinematic parameters to evaluate functional performance of sit-to-stand and stand-to-sit transitions using motion sensor devices: a systematic review. IEEE Trans Neural Syst Rehabil Eng. 2014;22(5):926–36.
Martínez-Ramírez A, Martinikorena I, Gómez M, Lecumberri P, Millor N, Rodríguez-Mañas L, et al. Frailty assessment based on trunk kinematic parameters during walking. J Neuroeng Rehabil. 2015;24(12):48.
Decade of Healthy Ageing 2021 – 2030 [Internet]. [cited 2022 Mar 1]. Available from: https://www.euro.who.int/en/health-topics/Life-stages/healthy-ageing/news/news/2021/01/decade-of-healthy-ageing-2021-2030
10 Priorities for a Decade of Action on Healthy Ageing [Internet]. [cited 2022 Mar 1]. Available from: https://www.who.int/news-room/feature-stories/detail/10-priorities-for-a-decade-of-action-on-healthy-ageing
Hill KD, Suttanon P, Lin S-I, Tsang WWN, Ashari A, Hamid TAA, et al. What works in falls prevention in Asia: a systematic review and meta-analysis of randomized controlled trials. BMC Geriatr. 2018;18(1):3.
Step Safely: Strategies for preventing and managing falls across the life-course [Internet]. [cited 2022 Mar 1]. Available from: https://www.who.int/publications-detail-redirect/978924002191-4
Acknowledgements
Authors would like to acknowledge staff involved in dissemination, recruitment and evaluation of the study results in the different Geriatrics Units of participant centers. We would like to recognize the support received from the Clinical Trials Unit team in Navarrabiomed/Fundación Miguel Servet.
Role of sponsors
Sponsor and funding agencies will not have any role in the design, data acquisition, management and/or analysis, results interpretation or publication. They will not take part in decision of any previously mentioned actions.
Funding
The present study is funded by a grant from the Spanish Ministry of Science and Innovation and the Instituto de Salud Carlos III (PI20/01546) co-financed by FEDER funding. Funder Agencies do not play any role in the conducting of the study. Instituto de Salud Carlos III,PI20/01546,Alvaro Casas-Herrero
Author information
Authors and Affiliations
Contributions
JSS and ACH performed the literature review and conceived and designed the study. CU, MEV, AMR, IBM, DMC, IME, FRE, MSL, AGS, BMM and REB will conduct the recruitment, intervention and evaluation of the subjects. JLS will manage data. JLS and ACH drafted the manuscript. All authors reviewed and approved present publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Study Protocol was approved by the different Ethics Committees of the participating centers (Navarra, Albacete, Barcelona and Guadalajara) and aligns with the principles of the Declaration of Helsinki. All participants will sign informed consents prior to their participation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: in the Funding section, “co-financed by FEDER funding", was added.
Supplementary Information
Additional file 1.
Protocol contributors.
Additional file 2.
OTAGO adherence log.
Additional file 3.
Falls log.
Additional file 4.
Spirit checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sánchez-Sánchez, J.L., Udina, C., Medina-Rincón, A. et al. Effect of a multicomponent exercise program and cognitive stimulation (VIVIFRAIL-COGN) on falls in frail community older persons with high risk of falls: study protocol for a randomized multicenter control trial. BMC Geriatr 22, 612 (2022). https://doi.org/10.1186/s12877-022-03214-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03214-0