Abstract
Background
Many hospitalized older adults cannot be discharged because they lack the health and social support to meet their post-acute care needs. Transitional care programs (TCPs) are designed to provide short-term and low-intensity restorative care to these older adults experiencing or at risk for delayed discharge. However, little is known about the contextual factors (i.e., patient, staff and environmental characteristics) that may influence the implementation and outcomes of TCPs. This scoping review aims to answer: 1) What are socio-demographic and/or clinical characteristics of older patients served by TCPs?; 2) What are the core components provided by TCPs?; and 3) What patient, caregiver, and health system outcomes have been investigated and what changes in these outcomes have been reported for TCPs?
Methods
The six-step scoping review framework and PRISMA-ScR checklist were followed. Studies were included if they presented models of TCPs and evaluated them in community-dwelling older adults (65+) experiencing or at-risk for delayed discharge. The data synthesis was informed by a framework, consistent with Donabedian’s structure-process-outcome model.
Results
TCP patients were typically older women with multiple chronic conditions and some cognitive impairment, functionally dependent and living alone. The review identified five core components of TCPs: assessment; care planning and monitoring; treatment; discharge planning; and patient, family and staff education. The main outcomes examined were functional status and discharge destination. The results were discussed with a view to inform policy makers, clinicians and administrators designing and evaluating TCPs as a strategy for addressing delayed hospital discharges.
Conclusion
TCPs can influence outcomes for older adults, including returning home. TCPs should be designed to incorporate interdisciplinary care teams, proactively admit those at risk of delayed discharge, accommodate persons with cognitive impairment and involve care partners. Additional studies are required to investigate the contributions of TCPs within integrated health care systems.
Similar content being viewed by others
Background
Many older adults live with multiple complex health problems or experience unforeseen circumstances (e.g., falls) that result in acute care hospital admissions. Among hospitalized older adults, some cannot be discharged once intensive medical treatments are completed because they lack sufficient health and social supports (e.g., community services, nursing home beds) to meet their post-acute care needs [1]. Delayed discharges—episodes where patients have to stay in an acute care bed for longer than medically necessary—present critical challenges for many health care systems [2]. In Canada, patients who experience delayed discharge are referred to as Alternate Level of Care (ALC), and they occupy 8 to 10% of acute care hospital beds [3].
Delayed discharges are an important health issue on both an individual and health system levels. McCloskey and colleagues [4] found that mean age of this group was 79 years; 65% were women; had a mean of 4.6 chronic conditions (mainly hypertension, heart disease and diabetes); and were on multiple medications. During their hospital stay, most showed functional decline (reduced mobility and ability to perform basic activities of daily living); had inadequate home support both prior to admission and following discharge from hospital; and were waiting for transfer to a long-term care facility [5]. These older patients often developed complications (e.g., poor oral intake, confusion, infections), felt socially isolated [1] and, alongside their care partners, reported increased depressive [3], anxiety, and stress symptoms [5, 6]. Also, some hospitals charge patients with a daily co-payment for prolonged delayed discharge, which may contribute to a substantial financial burden on individuals and families [6]. At the system level, delayed discharges reduce patient flow, leading to emergency department overcrowding, cancelled elective outpatient surgeries, and poor coordination of care resources across healthcare settings [1, 3].
To address these issues, healthcare systems globally have introduced programs to provide primarily restorative care, to older patients either experiencing, or at risk for, delayed discharge. These programs serve as a means to maintain continuity of care in the interface between acute care and other settings such as residential care or an individual’s home. These programs include Intermediate Care Models (ICMs) in the UK and Europe; sub-acute care, post-acute care or skilled nursing facilities (SNFs) in the US; and Transitional Care Programs (TCPs) in Australia and Canada, which will all hereafter collectively be referred to as TCPs. TCPs are designed to provide short term, low intensity, restorative care to older adults (aged 65+) who are medically fit to leave the hospital but are unable to do so due to multiple issues including hospital acquired deconditioning and lack of social supports in the community [3]. Differences in TCPs across countries makes it difficult to describe and compare the patient populations they serve, the services they offer, the resources required to deliver them, and their expected outcomes [7]. To address this concern, Sezgin et al. [8] identified and defined the characteristics of ICMs based on the results of a scoping review and an international expert consultation (Delphi study and consensus meeting); the study identified key defining features of ICMs, including time-limited care delivered by interdisciplinary teams that promote recovery, restore independence and act as the interface between acute care services and home. In a subsequent review focused on the effectiveness of ICMs, Sezgin et al. [9] found that while some researchers reported reduced hospital utilisation, evidence was limited on the ICMs’ effectiveness in reducing emergency readmissions, institutionalization and cost, or improving older adults’ function. The inconsistent findings may be attributable to contextual factors (i.e., characteristics of patients, staff and environment) that may influence the implementation and outcomes of TCPs [10]. Contextual factors may impact the actual delivery of the TCPs’ core components which are aimed at reducing and preventing delayed hospital discharges in older adults, and with achieving best outcomes for this population.
This scoping review was conducted to describe contextual factors and core components of TCPs, and outcomes used to evaluate TCPs. The review was informed by Donabedian’s structure-process-outcome framework [11]. Structures are defined as attributes or characteristics that are within the health care team, organization, or patient that influence the implementation of the core components or services and the outcomes of TCPs. For example, in the current context, the patient structure covers the characteristics of older patients admitted to TCPs, and the resources (i.e., healthcare team) needed for providing high-quality services. Processes represent the core components and specific services offered, as well as the behaviours or actions reflecting collaboration between the individuals and their surroundings. For TCPs, examples of processes include the range of physical and psycho-social services provided by the TCP staff. Potential outcomes targeted at patients include functional status for patients, and the healthcare system outcomes such as discharge destinations, as healthcare system outcomes. Specifically, the purpose of this review was to identify research evidence and knowledge gaps related to the structures, processes and outcomes of TCPs. The specific review questions were:
-
1)
What are the socio-demographic and clinical characteristics of older patients served by TCPs?
-
2)
What are the core components provided by TCPs?
-
3)
What patient, caregiver, and health system outcomes have been investigated and what changes in these outcomes have been reported for TCPs?
Method
A scoping review (ScR) is the most suitable method for knowledge synthesis to address our exploratory research questions [12]. We followed the ScR methodology framework outlined by Arksey and O’Malley [13] and refined by Levac et al. [14], Colquhoun et al. [12], and Daudt et al. [15] as outlined in the published study protocol [7]. We followed the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols extension for ScRs statement (see Additional file 1). The ScR framework includes six steps: 1) identifying the research questions (listed above); 2) identifying relevant literature; 3) study selection; 4) charting the data; 5) collating, summarizing and reporting the results; 6) consulting with key stakeholders and translating knowledge. Below we briefly summarize each step.
Search strategy
Based on the descriptive aims of the review, the following key words and Medical Subject Headings (MeSH) terms were included in the search to identify relevant literature: aged or Indigenous persons and transitional care programs or intermediate care facilities or post or sub-acute facilities. We included Indigenous persons in our search to capture programs that might serve their unique needs and to help guide effective planning in this population [16]. A comprehensive search strategy was developed in conjunction with a health sciences librarian and subsequently refined in consultation with stakeholders and the research team. The strategy was validated by ensuring the retrieval of a key set of relevant studies. Searches were conducted in MEDLINE(R) (in Ovid, including Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily), Embase (in Ovid, including Embase Classic), Emcare (Ovid), PsycINFO (Ovid) and CINAHL (in EBSCO). All searches were conducted on May 28th, 2019 and updated on January 3rd, 2020. Search strategies included the use of text words and subject headings (e.g., MeSH, Emtree) related to (1) alternate levels of care, sub-acute, SNF, (2) aged populations and (3) Indigenous populations. Searches were limited to descriptive and evaluative studies of TCPs targeting older adults (55+), and reported in English, French, Dutch and German languages, when possible. For a more comprehensive search narrative and Medline search strategy, see Additional file 1 for the full Medline search strategy.
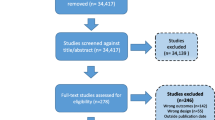
Study selection
Titles and abstracts were independently reviewed by two researchers against the selection criteria below. Then, two reviewers independently assessed all potentially relevant full text articles against inclusion and exclusion criteria (see Fig. 1 PRISMA flow diagram). In cases of disagreement between reviewers, the principal investigator (KM) resolved the conflict.
Studies were eligible for inclusion if they reported models of TCPs that served community-dwelling older adults (aged 65 years or older) experiencing or at risk for delayed discharges and if they reported examining processes and/or outcomes used to evaluate the programs. Studies that focused on standards of care in transitioning from acute care to home (e.g., rehabilitation post fracture or stroke) or involved home-based TCPs were excluded.
Data abstraction
A data abstraction form was created with specific codes based on Donabedian categorizations. The form was pilot tested by two members of the study team (KM, SV) to ensure clarity of content and consistency in documentation. Data extracted included study characteristics (i.e., type of study or design, aim, country, target population, sample size, setting, response rate); patient characteristics (age, sex, ethnicity, location, number and types chronic conditions); TCP features (location, staff mix, goals, patient admission criteria, and core components or services provided); and outcomes investigated. We used TIDier checklist to abstract data on elements of the TCPs reported in the selected articles [17].
Finally, we organized a stakeholder consultation meeting on 24 February 2020. Participants included representatives of: family caregivers (n = 1), health care practitioners (n = 3), hospitals (n = 6), community support service agencies (n = 5), provincial health care policy organisations (n = 4), local health regions (n = 2), and private service providers (n = 2). They provided feedback on the results, which are summarized below.
Results
Characteristics of included studies
Table 1 provides a summary of the studies selected for review. Although we aimed to include evidence involving Indigenous persons, we did not find any applicable research. Forty-nine percent of the studies were conducted in Europe [18, 19, 29,30,31,32,33, 35,36,37,38,39, 42, 43, 45, 51, 53, 55, 57], 27% in the U.S.A. [20,21,22,23, 25, 26, 44, 52, 54, 56], 11% in Australia [24, 27, 28, 48], 8% in Asia [40, 41, 49], and 5% in Canada [46, 50]. Different study designs were used, with the most common being retrospective cohort or chart audit designs (n = 9) [20, 21, 25, 27, 30, 39, 46, 49, 52]; followed by prospective cohort design (n = 7) [18, 19, 24, 26, 41, 44, 45]; RCTs (n = 7) [23, 28, 33, 35, 38, 53, 55]; non-randomized design (n = 4) [22, 29, 40, 57]; case study (n = 2) [31, 32]; pre-test post-test (n = 2) [48, 50]; and other designs (n = 6) [37, 42, 43, 51, 54, 56].
We used TIDier checklist to abstract data on elements of the TCPs reported in the selected articles [17]. Generally, TCPs were established to reduce the demand of hospital beds and provide post-acute care including rehabilitation to older adults who were unable to be discharged home safely. Four of 37 studies specifically identified that the goal of the TCP was to offload patients from the hospital beds to wait in the TCP until admission to a LTCH. Most of TCPs were staffed by teams of health professionals, mainly physicians, nurses and physiotherapists or occupational therapists, whereas two TCPs involved only rehabilitation therapists and two were run by only nurses and general physicians. Eleven TCPs were led by nurses, out of which three were nurse practitioner (NP) led. Only eight of 37 studies reported involvement of geriatricians as part of the team. The dose was represented in the TCP length of stay, which ranged from 1 to 151 days; in all articles, the dose of specific services or treatments provided to patients was not mentioned. The components and services provided by the TCPs varied widely, details of which are provided in the processes section below (See Table 2 for the list of components). Finally, data on intervention fidelity was not presented in all articles.
Structures
Characteristics of participants
The mean age of participants ranged from 72 [55] to 86 years [46]. The percentage of females ranged from 40% [42] to 76% [44], and of participants living alone from 26% [20] to 74% [18]. The majority of participants were functionally dependent. Most participants had mild levels of cognitive impairment; and had an average of 1.92 [56] to 8 [30] chronic illnesses.
Characteristics of staff
Staff working in TCPs included physiotherapists (across-studies average n = 26), nurses (n = 25), physicians (n = 22), occupational therapists (n = 20), and social workers (n = 17). Additional staff included dieticians (n = 10), geriatricians (n = 9), speech language pathologists (n = 9), pharmacists (n = 4); nurse practitioners (n = 4); clinical nurse specialists (n = 3); hearing services (n = 2); therapeutic recreation (n = 3); patient/health care assistants (n = 2); respiratory therapist (n = 1); and chiropodist (n = 1).
Characteristics of settings
TCPs were housed in long-term care homes (LTCH) in 12 studies, acute care hospitals in 10 studies, SNFs in five studies, community and rural hospitals in five studies, purpose-built intermediate and transitional care facilities in four studies, and multiple sites in two studies (Table 1). The TCPs were mentioned under a variety of different terms, with the most common being “Skilled Nursing Home Network Program” or “SNHN”; “University interprofessional care team” or “U-Team”; “Subacute demonstration unit”; “Transition care programs”; and “Post-acute care (PAC) facilities”, to name a few.
Processes
Core components and services provided by TCPs
While the TCPs’ five core components were similar, the specific services comprising the components varied based on the main goals of the programs and the population they served. The five core components included in most TCPs were: assessment; care planning and monitoring; treatment; discharge planning; and patient, family and staff education. The specific services within each component are listed in Table 2.
Assessment
A variety of assessments have been identified as a core care component of TCPs in 29 of 37 studies. Fourteen studies described completing a comprehensive assessment, of which only five specifically mentioned comprehensive geriatric assessment (CGA) [18, 19, 21, 44, 50]. The majority of programs focused on more specific assessments including: function; cognition and delirium [37, 40, 41, 48, 57]; nutrition [37, 40, 41]; pain [40, 41]; confidence in coping and motivation; social supports; home environment [48, 57]; medication review [48]; dental health, elimination, hearing and vision [57].
Care planning and monitoring
Fourteen studies incorporated care planning and monitoring as one of the main components of TCPs. In 11 studies, the investigators reported having weekly discussions with multidisciplinary team members that in some cases included patients and/or families [21, 28, 30, 33, 37, 38, 42, 46, 48, 50, 57]. These discussions served as a means to provide patient updates and accordingly revise care plans and prepare patients and families for discharge.
Treatment
One of the core components offered in TCPs included treatment delivery. However, there was a wide variety of treatments offered to patients as reported in 31studies. The most frequently reported treatments were mobility and rehabilitation training including transfers, stair climbing, strength and balance exercises, and provision of mobility aids [24, 29, 30, 32, 33, 38, 40, 42, 45, 48, 49, 52, 57]. Whereas functional training involving both activities of daily living (ADL) and instrumental activities of daily living (IADL), was identified as a main treatment in seven studies [33, 41, 46, 48, 53, 57]. The next most common treatment involved acute episodic and general medical care [21, 23, 29, 33, 38, 44, 45, 52,53,54], followed by specialized interventions such as pain management and terminal care [20, 21, 24, 30, 36, 38, 40, 42, 48].
To support the delivery of these treatments, nursing case management [32, 36, 37, 40, 42, 46, 49, 51, 56], geriatric consultation [37, 42, 46, 53, 55], and medication reconciliation [21, 22, 38, 55] were offered. Additional psychosocial services were provided to patients such as recreational activities [23, 24, 40, 45, 46]. Interestingly, only two studies reported having specialized rehabilitation professionals deliver interventions, including speech language pathologists, as well as hearing and dental care practitioners [53, 54].
Discharge planning
Twenty-two of 37 studies incorporated some form of discharge planning as a core component of TCPs. Discharge planning most commonly involved multidisciplinary team members planning the individualized discharge, which was responsive to patients’ needs [21,22,23,24, 28, 36, 38, 39, 42, 52, 54, 56]. Only three of 37 studies identified completing a follow up by phone call or home visit by a physiotherapist (PT) or a nurse to reinforce treatment recommendations; as well as provide new recommendations; problem solving, counselling, support, follow up on previously initiated referrals and address issues identified by caregivers [19, 27, 56].
Patient, family and staff education
Of 37 studies, only 10 reported on interventions to address educational and training needs of patients, family and/or clinical staff. Authors in three studies identified that care partners’ education and training needs were assessed and addressed by various health team members, most frequently nurses and PTs [56].
In terms of supporting staff to work in TCPs, education was identified as an important element for the effective implementation and delivery of the TCP [21,22,23, 46, 54]. The education was provided by NPs [21, 22], family physicians [46], and other clinicians with expertise in specialized geriatric care [23, 54]. Education included specific topics on the care of older adults, such as dementia management, medication deprescribing, as well as increasing staff’s awareness of the TCP, its goals and processes for its successful implementation [23, 54].
Outcomes
There was a wide variety of outcomes investigated in the studies. The outcomes are meaningfully classified as patient-related outcomes and health services related outcomes. The specific categories within each of the two domains are listed in Table 3.
Patient-related outcomes
Patient-related outcomes were classified into four categories: functional status, psychological status, health status and quality of life. These reflected patient-centered or patient-oriented outcomes measured using different instruments that were completed by patients or observers. The specific outcomes and respective measures are presented next.
Functional status
The functional status category is composed of functional status measures, ADL measures, and IADL measures. Functional status was measured 18 times [24, 26, 28,29,30,31,32, 35, 36, 40, 44,45,46, 48, 50, 53, 55, 56]. The most common evaluation tool was Barthel Index (BI) (n = 9). The majority of the studies reported improvements in functional status of patient admitted to TCPs [26, 29,30,31,32, 35, 36, 41, 44,45,46, 48, 54,55,56]. However, four studies reported no significant difference in functional status improvements between the intervention and the control groups [28, 29, 35, 56].
Psychological status
The psychological status category includes cognitive status and psychological wellbeing, evaluated as outcomes in 5 studies using a variety of instruments [30, 40, 45, 48, 53]. One study reported significant improvements in cognitive status of patients in transitional care units [40], and two studies reported significant improvements in psychological wellbeing [40, 45]. However, two studies reported no significant difference in improvements made in psychological wellbeing between the intervention and the control groups [30, 53], and one reported no significant change in cognitive status [30].
Health status
The health status category consisted of outcomes such as mortality, change in severity of disease, post discharge care needs, change in nutritional status and medication prescriptions, as listed in Table in 3. Seven studies examined mortality as a main outcome [18, 28, 29, 33, 35]. The mortality rates reported ranged from 10 to 28%. One study reported significantly lower mortality for transitional care unit patients 12 months following discharge [33]. Only one study reported significant change in disease severity from 31% of participants with low level of severity at baseline to 97% of participants at the time of discharge from the TCP [30]. One study looked at patient care needs, assessed using the Residential Care Scale, however, no significant difference in care needs was seen between the intervention and the control groups [28]. Significant positive changes in nutrition, evaluated using the Mini Nutritional Assessment (MNA), were reported in one study [40].
Quality of life
Quality of life measures were evaluated in three studies [28, 31, 45], whereas, two studies evaluated pain [21, 40], one examined fear of falling [50] and one explored the confidence to return home [48]. Two studies reported significant differences in quality of life of transitional care patients: one study reported that patients who were transferred to TCP had significantly lower scores on all domains of the SF-36 tool [25], and another study reported significantly greater improvements in EQ-5D scores in patients serviced by TCPs with an interdisciplinary team [49] [31, 45]. One study reported no significant changes in quality of life [28]. One of two studies that examined pain reported a significant decrease in pain [40].
Health services related outcomes
Health services related outcomes were grouped into three categories: 1) discharge destination; 2) health services use and cost analysis; 3) hospital stay.
Discharge destination
Discharge destination was measured as a main outcome in 15 studies [18, 19, 23, 24, 27, 32, 35, 39, 44, 46, 49,50,51, 54, 55]. More than two thirds of studies (80%) reported that the majority of patients in TCPs were discharged to community [18, 19, 23, 27, 32, 35, 39, 41, 44, 50, 51, 54]. One study reported significantly more discharges home and to assisted living facilities than to residential care facilities for patients in the intervention (i.e., exposed to TCP) group (30%), when compared to control group (12%) [46]. Only two studies reported lower chances of patients being discharged home from TCPs: patients with dementia as primary disease (24.4% discharged home) [49]; patients who had high level residential care assessments and were in a program with a lower physiotherapy staffing [24].
Health services use and cost
Four studies evaluated health services use for patients discharged from the TCPs [33, 37, 50, 51]; whereas 9 studies analysed costs associated with TCPs [22, 23, 31, 35,36,37, 46, 51, 53]. Only one of these studies examined the cost of care in relation to different types of staff mix, demonstrating that having an extra category of staff was significantly associated with lower cost [31]. Six of 9 studies found TCPs to be cost effective [22, 23, 46, 51, 53]. Studies that found TCPs to be more expensive primarily attributed the differences in cost to longer hospital stay [35, 36, 53].
Hospital stay
Hospital stay was examined in 20 studies [20,21,22,23, 25, 28, 29, 31, 33, 35, 40, 43, 46, 48, 50,51,52, 54,55,56]. Hospital stay was frequently assessed as length of stay prior to TCP transfer (n = 15 studies) and yielded mixed results. Seven studies reported TCP patients to have a significantly shorter length of hospital stay [22, 25, 28, 29, 31, 43, 54]: 6.6 days less for intervention group in one study [22], and 10.9 days less in another study [28]. Four studies showed TCP patients to have a significantly longer stay [23, 33, 35, 36]: 3.26 days more for intervention group in one study [23]; and 10.9 days more in another study [35]; and 4 studies reported no significant differences between intervention and control groups [46, 48, 50, 55]. Hospital readmission was investigated in eight studies [20, 21, 28, 29, 33, 50,51,52], three of which reported significantly lower rates of readmissions for patients in the intervention groups [21, 33, 52].
Stakeholder consultation
After reviewing these findings, stakeholders identified that the TCP services incorporating mobility and strength training as well as social connection resonated with their experience. However, they also discussed the variability of TCPs based on location and resource availability. Nurses, NPs and physicians typically provided care in the TCPs, however, specialist care (e.g., geriatricians) was usually not available. In contrast to the literature, where TCPs are described as a transition point to return home, TCPs in Ontario are generally viewed as the waiting area after acute care hospitalization but before LTCH placement. In the review, TCP services were described as connecting patients to resources outside the unit; stakeholders acknowledged that, to improve patient outcomes, TCPs in Ontario should be integrated with community supports services.
When examining the TCP patient outcomes, stakeholders noted that quality of life may be more appropriate than functional outcomes for the subset of patients who are waiting for LTCH placement. However, currently, data collection is limited to mandated data such as length of stay, volume and flow of patients through the TCP. Further, as TCPs exist in a variety of settings (e.g., LTCHs, acute care hospitals, group homes, etc.) data collection is not uniform and makes comparisons across programs difficult.
Stakeholders agreed that the healthcare team staffing, resource availability, and program length, would all impact TCP patient outcomes. For example, programs staffed mainly with health care aides might focus on maintaining function whereas programs that included physiotherapists might emphasize regaining function and preventing decline. There was also discussion about refining criteria for admission to TCPs and, in doing so, distinguish suitability for TCPs from that of other programs (e.g., convalescent care, slow-stream rehabilitation, etc.) and develop processes for proactively assessing hospitalized older adults’ need for TCPs before they are designed ALC. Stakeholders identified an opportunity to establish a community of practice in this area, where approaches to defining and assessing eligibility, case management and care coordination can be shared.
Discussion
Despite TCPs being developed globally, how TCPs are defined, funded and what services they provide vary widely [58,59,60]. Our review identified 37 articles describing and assessing TCPs for older adults. Within these studies, five types of programs were reported: intermediate, sub-acute and post-acute care; skilled nursing facilities and TCPs. Collectively, these programs provide short term, low intensity, restorative care to older adults who are at risk of, or designated as, delayed discharge; they are intended to promote recovery, restore independence, and provide the interface between acute care services and home [3, 8].
The papers included in this review suggest TCPs typically serve older women with multiple chronic conditions and some cognitive impairment, but who were living alone and functionally dependent before admission. This is consistent with a recent review [8] showing that these programs serve frail older adults with complex health needs, and they also found that this cohort can benefit from these services and that they can offer optimal health care services prior to transfer to the most suitable setting. Few studies reported if and how family members were involved in care and discharge planning. Given that most of these older adults were discharged home and, with limited resources in the community, family members are often involved in sustaining care once back home, this can be seen as a gap in service. Only three studies described follow-up care, either by phone call or home visit, to reinforce treatment recommendations or ongoing care (e.g., new treatments, counselling, referrals and care partner support).
Our review delineated common core components that have been integrated in TCPs internationally, including assessment, care planning, treatment, discharge planning, and education. However, the variability in the specific services offered within each component was interesting given that the programs had similar purposes. In terms of assessments, comprehensive geriatric assessments are the gold standard [61] when caring for older adults with multiple comorbid conditions yet only four TCPs were found to use them. Given the population served by TCPs, further research should focus on the benefits of integrating the comprehensive geriatric assessments and a more holistic approach to care.
The individual services offered in the treatment component of TCPs were also highly variable and were specific to the goals of and the population targeted by the program within the health care organization. The most frequently reported treatment focused on rehabilitation and included a focus on transfers, stair climbing, strength, and balance exercises. These activities are essential to regain function [9] and are foundational in TCPs. Missing from many of TCPs were services focused on patients’ social and mental health needs. Social vulnerability stemming from the accumulation of multiple and varied social problems, such as inequities , loss of social support and networks and socioeconomic status is a concern, in part because of the impact on health [62]. Future studies of TCPs should account for these social vulnerabilities, including in planning for discharge.
Staff delivering the intervention were of diverse disciplines and the staff mix or complement varied according to the specific treatments delivered. The most frequently cited staff working in the programs were physiotherapists and nurses. A review of intermediate models of care suggest that care should be delivered by an interdisciplinary team within an integrated health and social care system where a single contact point optimises services access, communication and coordination [8]. Notably absent from the teams were hearing and vision specialists; given the increasing number of older adults and age-related increased risk of dual sensory loss and its associated challenges [63], more screening and services are required.
As reported in the articles reviewed, the TCPs share goals similar to those of geriatric rehabilitation (GR) programs, including to improve functional capacity, promote activity and preserve functional reserve and societal participation [64]. We advocate the integration of the core principles of GR that also utilizes reablement approach [65] in the design of TCPs to enhance patient outcomes, in addition to refinement to the staff complement and processes currently in use in existing TCPs. Reablement approach not only focuses on improving functional abilities but also on maintaining current abilities and independence. Accordingly, TCPs should entail: 1) provision of person-centered care where the patients and care partners are actively involved in goal setting and care planning taking into account psychosocial and environmental factors. If older adults have reached a stage where they have lost their ability to participate in advance care planning (ACP) and goals of care discussions due to advanced stages of neurodegenerative diseases, their care partners should be engaged in such conversations while keeping the patients’ best interest at the core. Furthermore, goals should be operationalized with an appreciation of person’s abilities so that they are achievable, realistic and meaningful for patients and care partners [65]; 2) conduct of comprehensive geriatric assessments which incorporate the perspectives of patients as well as care partners to help tailor rehabilitation interventions to patients’ physical and social needs; 3) involvement of interdisciplinary team members (nurses, PT, OT, SLP and social workers) and clinicians who have training and experience in care of older adults with in-house ready access to providers such as NPs and/or geriatricians to assess and treat acute changes in conditions; 4) use of strategies utilizing restorative and compensatory methods [65]. TCPs are sometimes used to offload older adults from the hospital beds to another less expensive care setting without providing the care that is required, demanding careful attention to potential misuse of these programs [59]. Therefore, a careful review of the patients’ goals of care must be articulated in acute care prior to admission to the TCP to ensure patients are in the best location.
There was significant variability in the patient-level outcomes measured to evaluate the impact of TCPs, including functional, cognitive, quality of life and health status measures. Health system outcomes included discharge destination, costs and hospital stay (length of stay, readmission rates). These results are consistent with a recent review that found similar outcomes being used to evaluate ICMs [9]. Our review corroborates the finding that comparisons between various TCPs may be difficult given the multiple outcomes used to evaluate them [8, 9]. Moving forward, we emphasize the importance of clarifying the conceptualization of TCPs and mapping the outcomes to the TCP components; this would facilitate the identification of core outcomes that should be carefully and consistently operationalized to enable meaningful comparisons across TCPs within and across countries.
It is about time we pose the question, why do we continue to build TCPs that are often related to restoring excess disability that was caused by acute care? Is it not time to focus on improving the hospital experience for older adults, especially those with dementia? Based on a review of acute care practices [66], ageism exists and better acute care practices can occur upstream instead of focusing on repairing losses that occurred in hospitals. A focus on better home care options [67] may also reduce the need for these ever-increasing TCPs which are currently being developed worldwide. TCPs, regardless of their name or design should not serve as holding places for these complex, frail and vulnerable individuals waiting for LTC admission, but should include staff who can work with older adults to attain their unique and full restorative potential in maintaining their independence if there is potential to do so, while also meeting their holistic and social care needs which may include helping them come to terms with their lost function and end of life. The strengths of the scoping review include a comprehensive and systematic search of the literature which identified factors that may influence the implementation and outcomes of TCPs in addressing delayed hospital discharges for older adults. Still, there were limitations; in particular, some relevant articles may have been excluded by limiting the search to four languages.
Conclusion
TCPs can influence outcomes for hospitalized older adults, including helping them go back home. This review highlights the need to design TCPs to be delivered by interdisciplinary teams, accommodating persons with cognitive impairment and actively involving care partners. Clinicians, administrators and policymakers should collaborate to establish TCPs that proactively admit older adults at risk for delayed discharge, focus on optimizing functional ability, and incorporate individualized care planning and care coordination. Additional studies are required to investigate the contributions of TCPs within integrated health care systems.
Availability of data and materials
All data analysed during this study are included in this published article.
Abbreviations
- TCP:
-
Transitional care program
- QoL:
-
Quality of life
- ALC:
-
Alternate level of care
- ICMs:
-
Intermediate care models
- SNFs:
-
Skilled nursing facilities
- ScR:
-
Scoping review
- MeSH:
-
Medical subject headings
- SNHN:
-
Skilled nursing home network
- PAC:
-
Post-acute care
- CGA:
-
Comprehensive geriatric assessment
- ADL:
-
Activities of daily living
- IADL:
-
Instrumental activities of daily living
- PT:
-
Physiotherapist
- BI:
-
Barthel Index
- MNA:
-
Mini nutritional assessment
- LTCH:
-
Long term care home
- MCC:
-
Multiple comorbid conditions
References
Landeiro F, Roberts K, Gray AMI, Leal J. Delayed hospital discharges of older patients: a systematic review on prevalence and costs. Gerontologist. 2019;59:e86–97.
Costa AP, Poss JW, Peirce T, Hirdes JP. Acute care inpatients with long-term delayed-discharge: evidence from a Canadian health region. BMC Health Serv Res. 2012;12:1.
Rojas-García A, Turner S, Pizzo E, Hudson E, Thomas J, Raine R. Impact and experiences of delayed discharge: a mixed-studies systematic review. Health Expect. 2018;21:41–56.
McCloskey R, Jarrett P, Stewart C, Nicholson P. Alternate level of care patients in hospitals: what does dementia have to do with this? Can Geriatr J. 2014;17:38.
Bender D, Holyoke P. Why some patients who do not need hospitalization cannot leave: a case study of reviews in 6 Canadian hospitals. Healthc Manag Forum. 2018;4:121–5.
Kuluski K, Im J, McGeown M. “It’s a waiting game” a qualitative study of the experience of carers of patients who require an alternate level of care. BMC Health Serv Res. 2017;17:1.
McGilton KS, Vellani S, Babineau J, Bethell J, Bronskill SE, Burr E, et al. Understanding transitional care programmes for older adults who experience delayed discharge: a scoping review protocol. BMJ Open. 2019;9:e032149.
Sezgin D, O’Caoimh R, O’Donovan MR, Salem MA, Kennelly S, Samaniego LL, et al. Defining the characteristics of intermediate care models including transitional care: an international Delphi study. Aging Clin Exp Res. 2020;32:2399–410.
Sezgin D, O'Caoimh R, Liew A, et al. The effectiveness of intermediate care including transitional care interventions on function, healthcare utilisation and costs: a scoping review. Eur Geriatr Med. 2020;11(6):961–74. https://doi.org/10.1007/s41999-020-00365-4.
Medical Research Council. Implementation science. 2019. https://mrc.ukri.org/funding/science-areas/global-health-and-international-partnerships/applied-global-health-research-board/our-science-and-contacts/implementation-science/. Accessed 20 May 2019.
Donabedian A. Evaluating the quality of medical care. Milbank Q. 2005;44:166–206.
Colquhoun HL, Levac D, O’Brien KK, Straus S, Tricco AC, Perrier L, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67:1291–4.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol Theory Pract. 2005;8:19–32.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:1–9.
Daudt HML, Van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med Res Methodol. 2013;13:1–9.
Webkamigad S, Rowe R, Peltier S, Froehlich Chow A, McGilton KS, Walker JD. Identifying and understanding the health and social care needs of indigenous older adults with multiple chronic conditions and their caregivers: a scoping review. BMC Geriatr. 2020;18:1–33.
Hoffman T, Glasziou P, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDier) checklist and guide. BMJ. 2014;348:1687.
Abrahamsen JF, Haugland C, Nilsen RM, Ranhoff AH. Predictors for return to own home and being alive at 6 months after nursing home intermediate care following acute hospitalization. Eur Geriatr Med. 2014;5:108–12.
Abrahamsen J, Haugland C, Nilsen R, Ranhoff A. Three different outcomes in older community-dwelling patients receiving intermediate care in nursing home after acute hospitalization. J Nutr Health Aging. 2016;20:446–52.
Anderson MA, Tyler D, Helms LB, Hanson KS, Sparbel KJ. Hospital readmission from a transitional care unit. J Nurs Care Qual. 2005;20:26–35.
Bergman-Evans B. Weaving a safety net. An NP-led subacute care program. Adv Nurse Pract. 2010;18:39–40,42.
Blewett LA, Johnson K, McCarthy T, Lackner T, Brandt B. Improving geriatric transitional care through inter-professional care teams. J Eval Clin Pract. 2010;16:57–63.
Bowcutt M, Andrews BC, Kaye J. Subacute care: A competitive response to providing geriatric care. J Nurs Adm. 2000;30:300–3.
Brusco NK, Taylor NF, Hornung I, Schaffers S, Smith A, De Morton NA. Factors that predict discharge destination for patients in transitional care: a prospective observational cohort study. Aust Health Rev. 2012;36:430–6.
Burke RE, Juarez-Colunga E, Levy C, Prochazka AV, Coleman EA, Ginde AA. Patient and hospitalization characteristics associated with increased Postacute care facility discharges from US hospitals. Med Care. 2015;53:492–500.
Buurman BM, Han L, Murphy TE, Gahbauer EA, Leo-Summers L, Allore HG, et al. Trajectories of disability among older persons before and after a hospitalization leading to a skilled nursing facility admission. J Am Med Dir Assoc. 2016;17:225–31.
Chan DKY, Zhang S, Liu Y, Upton C, Kurien PE, Li R, et al. Effectiveness and analysis of factors predictive of discharge to home in a 4-year cohort in a residential transitional care unit. Aging Med. 2019;2:162–7.
Crotty M, Whitehead CH, Wundke R, Giles LC, Ben-Tovim D, Phillips PA. Transitional care facility for elderly people in hospital awaiting a long term care bed: randomised controlled trial. BMJ. 2005;331:1110–3.
Dahl U, Steinsbekk A, Johnsen R. Effectiveness of an intermediate care hospital on readmissions, mortality, activities of daily living and use of health care services among hospitalized adults aged 60 years and older - a controlled observational study. BMC Health Serv Res. 2015;15(1):1–11.
Del Giudice E, Ferretti E, Omiciuolo C, Sceusa R, Zanata C, Manganaro D, et al. The hospital-based, post-acute geriatric evaluation and management unit: the experience of the acute geriatric unit in Trieste. Arch Gerontol Geriatr. 2009;49:49–60.
Dixon S, Kaambwa B, Nancarrow S, Martin GP, Bryan S, Dixon S, et al. The relationship between staff skill mix, costs and outcomes in intermediate care services. BMC Health Serv Res. 2010;10:221.
Elbourne H, Le May A. A multidisciplinary approach to person-centred practice. Nurs Resid Care. 2012;14:199–202.
Garåsen H, Windspoll R, Johnsen R. Intermediate care at a community hospital as an alternative to prolonged general hospital care for elderly patients: a randomised controlled trial. BMC Public Health. 2007;7:1–9.
Garåsen H, Windspoll R, Johnsen, R. Long-term patients’ outcomes after intermediate care at a community hospital for elderly patients: 12-month follow-up of a randomized controlled trial. Scand J Public Health. 2008; 36:197–204.
Griffiths P, Harris R, Richardson G, Hallett N, Heard S, Wilson-Barnett J. Substitution of a nursing-led inpatient unit for acute services: randomized controlled trial of outcomes and cost of nursing-led intermediate care. Age Ageing. 2001;30:483–8.
Harris R, Richardson G, Grifffiths P, Hallett N, Wilson-Barnett J. Economic evaluation of a nursing-led inpatient unit: the impact of findings on management decisions of service utility and sustainability. J Nurs Manag. 2005;13:419–27.
Heim N, Rolden H, van Fenema EM, Weverling-Rijnsburger AW, Tuijl JP, Jue P, et al. The development, implementation and evaluation of a transitional care programme to improve outcomes of frail older patients after hospitalisation. Age Ageing. 2016;45:643–51.
Herfjord JK, Heggestad T, Ersland H, Ranhoff AH. Intermediate care in nursing home after hospital admission: a randomized controlled trial with one year follow-up. BMC Res Notes. 2014;7(1):1–10.
Hilton C, Madaras A, Qureshi M. An intermediate care unit for older people with both physical and psychiatric disorders: naturalistic outcome study. Int Psychogeriatrics. 2013;25:895–900.
Lee W, Peng L, Cheng Y, Liu C, Chen L, Yu H. Effectiveness of short-term interdisciplinary intervention on postacute patients in Taiwan. J Am Med Dir Assoc. 2011;12:29–32.
Lee YS, Lin CS, Jseng YH, Luo TW, Hung PJ, Wu MC, et al. Predictive factors for patients discharged after participating in a post-acute care program. J Cli n Gerontol Geriatr. 2012;3:25–8.
Lees L, Dowling C, Day M. Factors that contribute to the diversion of patients from long-term care. Nurs Older People. 2013;25:19–24.
Levin KA, Crighton E. Measuring the impact of step down intermediate care on delayed discharge: an interrupted time series analysis. J Epidemiol Community Health. 2019;73(7):674–9.
Likourezos A, Si M, Kim WO, Simmons S, Frank J, Neufeld R. Health status and functional status in relationship to nursing home subacute rehabilitation program outcomes. Am J Phys Med Rehabil. 2002;81:373–9.
Luthy C, Cedraschi C, Rutschmann OT, Kossovsky MP, Allaz AF. Managing postacute hospital care: a case for biopsychosocial needs. J Psychosom Res. 2007;62:513–9.
Manville M, Klein MC, Bainbridge L. Improved outcomes for elderly patients who received care on a transitional care unit. Can Fam Physician. 2014;60:e263–71.
Michael, R and Wheeler, B and Wichmann, H and Horner, B and Downie, J. The Healthy Ageing Unit: A comparative controlled intervention. JARNA. 2005;8 (2):9–15.
Michael R, Wichmann H, Wheeler B, Horner B, Downie J. A multidisciplinary model of transitional rehabilitation in acute aged care. J Aust Rehabil Nurs Assoc. 2004;7:10–6.
Nakanishi M, Shindo Y, Niimura J. Discharge destination of dementia patients who undergo intermediate Care at a Facility. J Am Med Dir Assoc. 2016;17:92–e1.
O’Brien K, Welsh D, Barnable A, Wiseman G, Colbourne A. The impact of introducing restorative care on client outcomes and health system effectiveness in an integrated health authority. Home Health Care Manag Pract. 2017;29:13–9.
Orvik A, Nordhus GE, Axelsson SB, Axelsson R. Interorganizational collaboration in transitional care - a study of a post-discharge programme for elderly patients. Int J Integr Care. 2016;16:11.
Parsons PL, Gifford C. Characteristics and outcomes of elderly patients receiving transitional care. Outcomes Manag. 2002;6:182–5.
Richardson G, Griffiths P, Wilson-Barnett J, Spilsbury K, Batehup L. Economic evaluation of a nursing-led intermediate care unit. Int J Technol Assess Health Care. 2001;17:442–50.
Richardson H, Kovner AR. Implementing swing-bed services in small rural hospitals. J Rural Health. 1986;2:46–60.
Steiner A, Walsh B, Pickering RM, Wiles R, Ward J, Brooking JI, et al. Therapeutic nursing or unblocking beds? A randomised controlled trial of a post-acute intermediate care unit. BMJ. 2001;322:453–60.
Tappen RM, Hall RF, Folden SL. Impact of comprehensive nurse-managed transitional care. Clin Nurs Res. 2001;10:295–313.
Trappes-Lomax T, Ellis A, Fox M, Taylor R, Power M, Stead J, et al. Buying time I: a prospective, controlled trial of a joint health/social care residential rehabilitation unit for older people on discharge from hospital. Health Soc Care Commun. 2006;14:49–62.
Hang J, Francis-Coad J, Naseri N, Hill A. Effects of facility-based transitional care programs on health-related outcomes in older adults: a systematic review protocol. JBI Evid Synth. 2020;18:2425–34.
Flint L, Daivid D, Smith A. Rehabbed to death. N Engl J Med. 2019;380:5.
The Medicare Payment Advisory Commission. Post-acute care. 2020; retrieved http:// medpac.gov/-research-areas-/post-acute-care
Ellis G, Gardner M, Tsiachristas A, Langhorne P, Burke O, Harwood RH, et al. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev. 2017;9:CD006211.
Andrew MK, Mitnitski AB, Rockwood K. Social vulnerability, frailty and mortality in elderly people. PLoS One. 2008;3:e2232.
Heine C, Browning C. Dual sensory loss in older adults: a systematic review. Gerontologist. 2015;55:913–28.
Grund S, Gordon A, van Balen R, Bachmann S, Cherubini A, Landi F, et al. European consensus on core principles and future priorities for geriatric rehabilitation: consensus statement. Eur Geriatr Med. 2020;11:233–8.
Poulos C, Bayer A, Beaupre L, Claire L, Poulos R, Wang R, et al. Alzheimer’s & Dementia. TRCI. 2017;3:450–8.
McGilton KS, & Lemay G. Chapter 5: Hospitalization of persons with dementia (pages 109-136) In, Garcia, L., Drummond, N., & McCleary, L. (Eds.) (2020). Evidence based approaches to dementia transitions: riding the waves. Cambridge: Academic Press Books, Elsevier Inc.
Achterberg WP, Cameron ID, Bauer JM, Schols JM. Geriatric Rehabilitation-State of the Art and Future Priorities. J Am Med Dir Assoc. 2019;20(4):396–8.
Acknowledgements
We wish to acknowledge librarian Jessica Babineau for her assistance with the literature review and family caregiver Margaret Keatings for her interest and guidance during the design and the conduct of this scoping review.
Funding
This work is supported by the Canadian Institutes of Health Research (CIHR) Operating Grant: Transitions in Care - Best and Wise Practices Grants (CIHR Funding Number BWP-163068). KSM is supported by the Walter and Maria Schroeder Institute for Brain Innovation & Recovery. The funders had no role in study design, data collection, analysis and interpretation of data, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Authors (KSM, SS & SV) have been involved in the design of the study. In addition to authors KSM, SS, SV, other authors (AK, SR, CI, AC, JB, MP) were substantially involved in the acquisition, analysis and interpretation of data and drafting manuscript. All authors (KSM, SV, AK, SR, CI, AC, JB, EB, MK, SM, KN, MP, AS & SS) were involved in critically revising the manuscript for important intellectual content and approval of final submitted version; as well agree to be personally accountable for all aspects of their contribution towards the completion of this manuscript. Author KSM was also involved in the conception of the study. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Authors declare no completing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Medline search strategy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
McGilton, K.S., Vellani, S., Krassikova, A. et al. Understanding transitional care programs for older adults who experience delayed discharge: a scoping review. BMC Geriatr 21, 210 (2021). https://doi.org/10.1186/s12877-021-02099-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-021-02099-9