Abstract
Background
Total physical activity is positively associated with brain volume and cognition in older adults. While we have ample evidence that recreational physical activity influences brain health, the contributions of other daily activities are less understood. In particular, the associations between household physical activity and brain health in older adults is underexplored. The purpose of this study was to identify associations between household physical activity, brain volume, and cognition in a sample of cognitively unimpaired older adults.
Methods
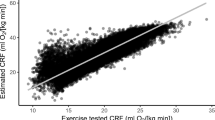
We report data from 66 cognitively unimpaired older adults (71 ± 4 years) who participated in a health evaluation, cognitive assessment, and structural brain imaging. Physical activity was assessed using the Phone-FITT questionnaire and separated into household and recreational physical activity. We quantified whole brain volume, gray matter volume, and white matter volume, and assessed cognitive performance in four domains: memory, working memory/attention, processing speed, and executive function. Associations between physical activity, brain volume, and cognition were investigated in an omnibus approach using two multivariate analysis of variance (MANOVA) models. The first model assessed the associations between physical activity and brain volume adjusting for age, sex, Framingham Risk score (FRS) and intracranial volume. The second model assessed the associations between physical activity and overall cognitive performance adjusting for age, sex, FRS and education. Post hoc regression analyses were conducted to investigate significant MANOVA results. We also conducted further regression analyses to investigate associations with hippocampal and frontal lobe volume.
Results
Household, but not recreational, physical activity was positively associated with brain volume measurements (F = 3.07, p = .035), specifically gray matter volume (t = 2.51, p = .015). Further exploratory analyses identified that household physical activity was associated with hippocampal (p = .015) and frontal lobe (p = .010) volume. No significant relationships were observed between household or recreational physical activity and cognition.
Conclusion
Time spent engaging in household physical activity was positively associated with brain volume, specifically gray matter volume, in older adults. Highlighting the benefits associated with household chores may motivate older adults to be more active by providing a more attainable, low risk form of physical activity.
Similar content being viewed by others
Background
Alzheimer’s disease and related dementias top the world’s most prevalent and costly medical conditions [1] and prevention and treatment of these disorders has been deemed a public health priority by the World Health Organization [2]. It has become widely accepted that unhealthy lifestyle behaviours contribute to an increased prevalence of cognitive impairment and dementia worldwide [3] and that engaging in physical activity is an effective strategy for preserving brain health in older adults [4,5,6,7,8]. Broadly defined, physical activity is any activity that involves bodily movements and the use of skeletal muscles. This includes everyday activity that is not structured, such as occupational or household activity, as well as recreational physical activity, such as exercise, which is structured and intended to improve fitness [9]. The actions by which physical activity affect the brain are suspected to be both indirect, such as improving health conditions, as well as more direct, including increasing brain neurotrophins [6, 10], improving cerebrovascular function [11, 12], and enhancing brain plasticity [13, 14]. Understanding how different forms of physical activity (i.e., recreational activity vs. household activity) contribute to brain health is crucial for developing strategies to reduce the risk of cognitive decline and dementia in older adults.
Much of the research in this regard has focused on recreational physical activities, in particular the effects of higher intensity exercise. Moderate to vigorous intensity exercise and higher aerobic fitness have been positively associated with whole brain volume, gray matter volume, and improved white matter integrity [5, 6, 15,16,17,18,19]. Moreover, exercise interventions have demonstrated effectiveness at increasing whole brain volume and gray matter volume in older adults [20,21,22]. Similar findings are also evident with low intensity forms of exercise independent of moderate to vigorous intensity activity [23,24,25,26]. A comprehensive review of the literature by Erickson et al. (2014) concluded that physical activity and fitness levels were routinely associated with larger hippocampal and prefrontal cortex volumes, and that exercise interventions were able to evoke positive changes in these regions specifically [6]. Cognitive function in older adults is also positively associated with cardiovascular fitness and in some studies has been shown to improve following exercise interventions [4, 27] with greatest benefits being apparent in executive function and attentional control. Not all studies show this effect, however. For example, a recent review of physical activity interventions concluded that evidence for cognitive improvement following interventions was insufficient, largely due to the heterogeneous cognitive measures used across studies, and underpowered sample sizes [28].
We know that not all brain benefits are derived from recreational physical activity exclusively. Total physical activity is associated with reduced cognitive decline and dementia risk [29,30,31], decreased brain atrophy [32], as well as increases in brain volume [33,34,35,36]. While ample evidence exists that recreational physical activity contributes to these associations, less is known about how other everyday physical activities such as household activity contribute to brain health. Household activities may be particularly interesting to study, because these types of activities (e.g., cleaning chores, meal preparation) are inherent aspects of many people’s daily life, providing some degree of physical activity and decreasing sedentary behaviour naturally. Studies examining the role of household physical activity on brain health are limited, however. Engagement in household physical activity has been shown to be negatively associated with frailty [37] and leisure time activity incorporating household chores has been found to be associated with decreased dementia risk [38, 39]. The purpose of this study was to assess how household physical activity specifically correlates with brain volume and cognition among a sample of cognitively unimpaired older adults. We hypothesized that household physical activity would be positively associated with both brain volume and cognition.
Methods
Study design and overview
Participants attended three assessment visits at Baycrest Hospital in Toronto involving a health evaluation, cognitive assessment, and structural brain imaging. Additional demographic, medical, and cognitive screening questions were administered by telephone before individuals were invited to participate. A physical activity questionnaire was administered to assess participants’ levels of household and recreational physical activity. The work described was carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans and was approved by the Research Ethics Board at Baycrest. All participants provided written informed consent.
Participants
We recruited 70 cognitively unimpaired older adults through advertisements and the Baycrest research participant pool. Participants were required to be 65–85 years of age, cognitively unimpaired and free from significant medical, neurological, or psychiatric conditions. Participants were excluded from entering the study if they met any of the following criteria: a score < 30 on the Telephone Interview for Cognitive Status– modified version (TICS-m) [40] to exclude individuals with possible dementia; use of insulin to treat type 2 diabetes; self-report of major diabetic complications, such as gastroparesis, retinopathy, nephropathy, or neuropathy; other significant medical or mental health disorders affecting cognition, such as previous myocardial infarction, stroke (self-report or evident from structural scans), or major depressive disorder; current or recent use of central nervous system-active medications, including those for the treatment of depression, sleep disorders, and migraine headaches; major inflammatory disorders, heart failure, and chronic lung disease; hormone replacement therapy in female participants; or contraindications to magnetic resonance imaging (e.g. claustrophobia, obesity, implanted metal from a surgery or injury). Two participants were removed from the analysis as outliers, one for presenting with a low intracranial volume (2.7 standard deviations below the mean) and the other for having a high FRS value (4.3 standard deviations above the mean). An additional two participants did not complete the cognitive test battery. Our final analysis includes 66 participants.
Health evaluation
Resting blood pressure was assessed (BPTru Medical Devices) and the average of four seated measurements was recorded. A fasting blood sample was collected for measurement of triglycerides, cholesterol (total, low density lipoprotein [LDL], and high density lipoprotein [HDL]), glucose, insulin, and HbA1c. Cardiovascular burden was assigned using the Framingham Risk Score (FRS). FRS was calculated using the Cox model formula [41] which includes age (years), sex (male/female), treatment of systolic blood pressure (yes/no), systolic blood pressure (mmHg), total cholesterol (mg/dL), HDL (mg/dL), smoking (yes/no), and diabetes mellitus (yes/no). FRS estimates each participant’s probability of developing cardiovascular disease (including cerebrovascular events) over a 10-year period [42]. Participants were asked to continue their usual diet, medications, and physical activity for the remainder of their involvement in the study.
Cognitive assessment
All participants were administered a battery of neuropsychological tests comprising four domains; memory, attention/working memory, executive function, and processing speed. Memory tests included the California Verbal Learning Test II immediate and delayed recall [43], Wechsler Memory Scale-Revised (WMS-R) Visual and Verbal Paired Associates learning and delayed recall [44], and the Wechsler Memory Scale-III (WMS-III) Faces immediate recall [45]. Attention/working memory tests included the WMS-III Mental Control [45], WMS-III Letter-Number Sequencing [45], Wechsler Adult Intelligence Scale-III (WAIS-III) backwards Digit Span [46], WAIS-III forward Digit Span [46], and Wechsler Adult Intelligence Scale – Revised (WAIS-R) Arithmetic [47]. Executive functioning tests included the Wisconsin Card Sorting test – Modified (number of errors) [48], Controlled Oral Word Association (COWA) test - Phonemic fluency (FAS) [49], and the Halstead-Reitan Trail Making Test version B [50]. Processing speed tests included the Halstead-Reitan Trail Making Test version A [50] and WAIS-III Digit Symbol Coding [46]. Neuropsychological test scores are reported as raw scores. Composite scores for each domain were created by calculating z scores for each test relative to the current sample (n = 66) and averaging them.
Structural imaging
Images were acquired on a 3 Tesla Magnetom Trio Siemens scanner with a 12-channel head coil. Each participant’s head was restrained using a vacuum pillow that fit inside the head coil. High-resolution structural images (T1-weighted three-dimensional magnetization-prepared rapid gradient-echo sequence; 3D-MPRAGE) were acquired with the following parameters: TR/TE = 2000/2.63, FOV = 256 mm, slice thickness = 1 mm, number of slices = 160. Cortical reconstruction and volumetric segmentation on the native-space anatomical images were performed with the Freesurfer image analysis suite (version 5.3.0; http://surfer.nmr.mgh.harvard.edu/). Before data extraction, an in-house quality assurance protocol was implemented based on recommended procedures from the Freesurfer website. Briefly, each brain was assigned a rating of 1, 2, or 3 based on the overall quality of the output. Brains with few, minor issues (e.g., tiny inclusions of skull/meninges in the pial surface, minute errors in labeling the white/gray matter interface) were assigned a rating of 3 (n = 53). Brains with more frequent or slightly larger errors were assigned a rating of 2 (n = 13), and brains with the most issues were assigned a rating of 1 (n = 0). Within the present sample there were no brains with errors considered substantial enough to require manual correction or exclusion. For analyses, we then extracted estimates of intracranial volume, whole brain volume, gray matter volume, and white matter volume. Hippocampal and frontal lobe volumes were also extracted, using the Desikan-Killiany atlas [51]. To account for variability in head size in our analyses, all of the brain volumetric measures were adjusted for intracranial volume (ICV) [52].
Physical activity
Physical activity was assessed using the Phone-FITT, a valid and reliable telephone questionnaire for community dwelling older adults which gathers information on frequency, duration, and intensity of all physical activities performed over the past month [53]. The Phone-FITT questionnaire can be found in Gill et al. [53]. The questionnaire accounts for seasonal variance, allows individuals to report on activities not specifically listed, and separates activities into household and recreational physical activity. Household physical activity includes: light housework (tidying, dusting), meal preparation/clean up, shopping, heavy housework, home maintenance (e.g., yard work and home repairs), and care giving. Recreational physical activity includes: arm strengthening, leg strengthening, stretching and balance exercises, walking for exercise, dancing, swimming, bicycling, golf, gardening, and any other activities reported by the individual. Frequency is measured as number of times the activity was performed per week and duration for each activity is scored categorically as 1 (1 to 15 min), 2 (16–30 min), 3 (31–60 min), or 4 (60+ minutes). Intensity is measured by asking respondents whether they were breathing normally, slightly out of breath, or breathing too hard to carry on a conversation (scored as 1, 2, and 3, respectively) when performing the activity. The authors suggested that frequency and duration scores be used exclusively [53] as intensity measures tend to decrease response reliability. Within our sample, we found that household activities done multiple times per day (e.g., preparing meals, tidying) overinflated total scores so we chose to analyze the duration scores only. Therefore, the scores used are the sum of duration scores from each activity regardless of frequency or intensity, and hereafter are referred to as household and recreational physical activity.
Analyses
We performed statistical analyses using R (v.3.3.1) [54]. Significance was set at p < .05. First, we examined the effect of potential confounding variables of age, education, and FRS on brain volume and cognition using Pearson correlation. FRS was included as a covariate in our models due to the abundance of research indicating that FRS is negatively associated with brain structure and function in cognitively unimpaired older adults [55]. Relationships with brain volume measurements were assessed by partial correlation adjusting for ICV. T-tests were used to assess sex differences in household and recreational physical activity scores. Sex differences between brain volumes and cognition were assessed using analysis of covariance (ANCOVA) and adjusted for age, FRS, and ICV in brain volume analysis, and age, FRS, and education in cognition analysis.
We tested the relationships between physical activity, brain volume, and cognition in an omnibus approach using two multivariate analysis of variance (MANOVA) models [56]. Household and recreational physical activity scores were entered together as independent variables in both models. The dependent variable in the first model was brain volume, which was comprised of 3 measurements: whole brain, gray matter, and white matter volume. The dependent variable in the second model was cognition, which was comprised of composite z scores for four cognitive domains: memory, attention/working memory, executive function, and processing speed. Age, sex, FRS, and intracranial volume were used as covariates in the model examining brain volume. Age, sex, FRS, and education were used as covariates in the model examining cognition. Post-hoc multiple regression models were used to further explore dependent variables from significant MANOVA models. The Bonferroni method was used to adjust for multiple comparisons. Statistical threshold for significance was set at <.017 for individual brain volumes (.05/3) and < .0125 for individual cognitive domains (.05/4). Due to the well-established literature associating hippocampal and frontal lobe volume with physical activity [6], we also conducted exploratory regression analyses to investigate these relationships in our sample.
Results
Table 1 describes the demographic, neuroimaging, and cognitive characteristics of the study sample.
Bivariate correlations between variables are displayed in Table 2. Age was negatively associated with gray matter volume (r = −.40, p < .001). Years of education was positively associated with attention/working memory (r = .33, p = .006) and executive function (r = .39, p = .001). FRS was negatively associated with whole brain (r = −.28, p = .026), white matter volume (r = −.28, p = .024), memory (r = −.39, p = .001), and executive function (r = −.30, p = .015). There were no significant sex differences in physical activity or brain volume measurements; however, memory performance was better in women (p < .001).
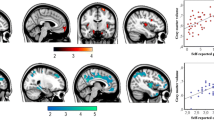
The MANOVA revealed that household physical activity (F (3, 57) = 3.07, p = .035), but not recreational physical activity (F (3, 57) = 0.32, p = .812) was significantly associated with brain volume measurements. Age (p = .043), sex (p = .003), and FRS (p = .025) were significant covariates in this analysis. Neither household (F (4, 56) = .1.52, p = .210) nor recreational physical activity (F (4, 56) = .74, p = .571) were associated with overall cognitive performance, but women had better cognitive performance (p < .001). Table 3 displays the results from the post hoc multiple regression analysis. Household physical activity was positively associated with gray matter volume (p = .015) and age was the only significant covariate (p = .008).
Exploratory regression analyses revealed that household physical activity was significantly associated with hippocampal (p = .015) and frontal lobe (p = .010) volumes (Table 4). To investigate the lack of relationship between recreational physical activity and brain volume, an additional analysis was conducted excluding light intensity activities (e.g., light walking, stretching/balance exercises, gardening, golf) from our recreational measure. As with the previous analyses, recreational physical activity was not associated with gray (p = .598) or white (p = .149) matter volumes.
Discussion
This study investigated the associations between household physical activity, brain volume, and cognition in a sample of cognitively unimpaired older adults. These results supported our hypothesis that household physical activity is positively associated with brain volume, however no significant associations with cognition were observed. The overarching association with brain volume was driven by gray matter volume, but not white matter volume. We believe that this was reflected in the trend towards a significant association with total brain volume, however this association failed to reach statistical significance after Bonferroni correction. The hippocampus and frontal lobe have been identified as brain areas that are particularly sensitive to exercise [6] and our work supports this notion in the context of household physical activity. Surprisingly, no associations were observed between recreational physical activity and brain volume or cognition.
This is the first study to identify an association between household physical activity and gray matter volume, and contributes to the growing body of research helping to guide physical activity recommendations for older adults. Our work uniquely points to an association with previously unexplored components of total physical activity. While there is ample evidence for the benefits of recreational physical activity, we now show how a specific type of activity that is an inherent aspect of many people’s daily life relates to brain health. Highlighting the brain benefits associated with household chores (e.g., cooking, cleaning, home maintenance) may motivate older adults to be more active by providing a more sustainable, low risk form of physical activity.
It is commonly hypothesized that increases in brain volume result from improved fitness and enhanced blood flow following exercise [11]. Total physical activity is associated with enhanced cardiorespiratory fitness and decreased incidence of cardiovascular disease and mortality [57]. It has been suggested that the vascular effects from non-structured everyday activities may be similar to those resulting from low intensity aerobic exercise [58]. For example, Sanchez-Lopez et al. [59] observed positive associations between non-structured physical activity and brain activity, and posited that results may have been due to vascular mechanisms based on hematological differences between study subjects. Another potential mechanism linking household physical activity to brain volume is enhanced neuroplasticity resulting from the planning and organization required for completing household chores. Interventions focusing on goal management and multitask training have shown to be effective at improving brain function in older adults [60,61,62,63]. Housework includes a wide range of tasks and may share many of the same features as cognitive training interventions [64]. On the contrary, it may be that individual's brain volume influences their level of household physical activity engagement. For example, someone experiencing greater than normal atrophy may be less likely to engage in household tasks. Lastly, an intriguing consideration is that the increased household physical activity scores in our sample may reflect lower levels of sedentary behavior. Approximately 67% of older adults report sitting for more than 8.5 h per day [65] and sedentary time is associated with adverse health outcomes despite regular exercise engagement [66, 67]. Prolonged sitting increases venous pooling and coagulation factors which in turn disrupt blood flow [68] and can lead to spikes in blood glucose and plasma triglycerides that are detrimental to the vasculature [69]. Sedentary behavior is associated with brain atrophy [29, 70] and research suggests that replacing sedentary time with light activity may promote optimal brain health [71,72,73]. We did not collect measures of sedentary behavior in this study but is an important measure to consider in future trials exploring the link between household physical activity and brain volume.
We proposed that our main results may be explained by the cognitive involvement of household chores, however physical activity was not associated with cognition in our sample. It is possible that more sensitive measures of planning and multitasking are required to confirm this association. Not all research supports the link between physical activity and cognition. A recent systematic review by Brasure et al. [28] concluded that evidence of a link between physical activity and dementia prevention is insufficient. The authors acknowledged limitations of the existing studies, including heterogeneous protocols and cognitive measures, as well as underpowered sample sizes. We may not have had sufficient power to observe the relationship between physical activity and cognition that has been reported in the literature [27,28,29,30,31]. While associations between physical activity and cognition were not apparent in our sample, brain volumetric measurements are strong predictors of longitudinal cognitive change [74, 75].
The lack of association between recreational physical activity and indicators of brain health in our sample was unexpected, but is perhaps explained by the removal of intensity scores from the analysis. We chose not to analyze intensity scores as per the recommendations of the Phone-FITT authors over concerns about the reliability of self-reported exercise intensity. Furthermore, although Phone-FITT recreational physical activity scores incorporate moderate to vigorous intensity physical activities, several low intensity activities such as gardening, golf, tai chi, stretching, and balance exercises are included in the questionnaire. The inclusion of these activities may have attenuated associations between recreational physical activity, brain volume, and cognition. Exploratory analyses were conducted on our dataset by removing light intensity activities (light walking, stretching, golf, and gardening) however these analyses did not lead to significant changes to our results. The removal of intensity scores may also help to explain the lack of associations with white matter volume. White matter abnormalities are a hallmark sign of cerebral small vessel disease, a condition that is attributable to poor cardiovascular health [3]. It is likely that white matter volume would show greater associations with participation in higher intensity exercise aimed at improving cardiovascular health and fitness. When light intensity activities were excluded form recreational physical activity scores, a closer association was observed between recreational physical activity and white matter volume, however, it still failed to reach significance.
As the first study to explore the relationships between household physical activity and brain volume, we first investigated more general areas of the brain, but conducted exploratory analysis to reveal regional associations. Consistent with the literature, associations were observed between hippocampal and frontal lobe volume. Further work with larger samples would allow for more precise characterizations of areas of the brain associated with household physical activity. Furthermore, while we proposed several mechanisms that may explain our results, we were unable to test these notions statistically. We did not collect measures of sedentary behaviour or quantify the cognitive involvement relating to household physical activity. Although we did calculate cardiovascular burden (FRS), larger studies with higher power are needed to test how cardiovascular health mediates the relationship between household physical activity and brain volume. It would be a worthwhile objective for future studies to investigate these potential mechanisms as mediators.
Like all self-report measures, the Phone-FITT is prone to social desirability and recall bias. Using the previous month as the recall period may avoid some of the difficulty with recalling behaviour over longer time periods but it is still likely that individuals feel the need to overestimate healthy behaviors. The Phone-FITT also provides an arbitrary score that cannot be translated to common physical activity parameters and objective measures such as accelerometers are preferred when assessing physical activity levels. Furthermore, the cross sectional design of this study does not allow for the determination of causal relationships. Household physical activity may influence brain volume or brain volume may influence engagement in household physical activity. Future research examining the direction of this relationship is needed. For example, longitudinal studies assessing engagement in household physical activity and brain volumetric changes over time or interventions studies focused on increasing engagement in household physical activity. Aside from the mentioned limitations, strengths of this study include objective measures of cardiovascular risk, the use of advanced neuroimaging techniques, and the assessment of household and recreational physical activity separately.
In conclusion, household physical activity was positively associated with brain volume, specifically total gray matter volume in our sample. This is the first study to highlight associations with previously unexplored components of total physical activity and contributes to the growing body of literature guiding physical activity recommendations for older adults.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Prince MJ, Wimo A, Guerchet MM, Ali GC, Wu YT, Prina M. World Alzheimer report 2015 - the global impact of dementia: an analysis of prevalence, incidence, cost and trends. London: Alzheimer’s Disease International; 2015.
Wortmann M. Dementia: a global health priority - highlights from an ADI and World Health Organization report. Alzheimers Res Ther. 2012;4(5):40.
Gorelick PB, Scuteri A, Black SE, Decarli C, Greenberg SM, Iadecola C, et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:2672–713.
Bherer L, Erickson KI, Liu-Ambrose T. A review of the effects of physical activity and exercise on cognitive and brain functions in older adults. J Aging Res. 2013;2013:657508.
Erickson KI, Raji CA, Lopez OL, Becker JT, Rosano C, Newman AB, et al. Physical activity predicts gray matter volume in late adulthood. Neurology. 2010;75:1415–22.
Erickson KI, Leckie RL, Weinstein AM. Physical activity, fitness, and gray matter volume. Neurobiol Aging. 2014;35:S20–8.
Liu-Ambrose T, Barha CK, Best JR. Physical activity for brain health in older adults. Appl Physiol Nutr Metab. 2018;43:1105–12.
Rovio S, Spulber G, Nieminen LJ, Niskanen E, Winblad B, Tumilehto J, et al. The effect of midlife physical activity on structural brain changes in the elderly. Neurobiol Aging. 2010;31(11):1927–36.
Caspersen C, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–31.
Lista I, Sorrentino G. Biological mechanisms of physical activity in preventing cognitive decline. Cell Mol Neurobiol. 2010;30(4):493–503.
Chapman SB, Aslan S, Spence JS, DeFine LF, Keebler MW, Didehbani N, et al. Shorter term aerobic exercise improves brain, cognition, and cardiovascular fitness in aging. Front Aging Neurosci. 2013;5:75.
MacIntosh BJ, Crane DE, Sage MD, Saeed Rajab A, Donahue MJ, Mcllroy WE, et al. Impact of a single bout of aerobic exercise on regional brain perfusion and activation responses in healthy young adults. PLoS One. 2014;9(1):e85163.
Ma CL, Ma XT, Wang JJ, Liu H, Chen YF, Yang Y. Physical exercise induces hippocampal neurogenesis and prevents cognitive decline. Behav Brain Res. 2017;317:332–9.
Van Praag H, Shubert T, Zhao C, Gage FH. Exercise enhances learning and hippocampal neurogenesis in aged mice. J Neurosci. 2005;25(38):8680–5.
Bugg JM, Head D. Exercise moderates age-related atrophy of the medial temporal lobe. Neurobiol Aging. 2011;32(3):506–14.
Voss MW, Nagamatsu LS, Liu-Ambrose T, Kramer AF. Exercise, brain, and cognition across the lifespan. J Appl Physiol. 2011;111:1505–13.
Burns JM, Cronk BB, Anderson HS, Donnelly JE, Thomas GP, Harsha A, et al. Cardiorespiratory fitness and brain atrophy in early Alzheimer’s disease. Neurology. 2008;71(3):210–6.
Colcombe SJ, Erickson KI, Raz N, Webb AG, Cohen NJ, McAuley E, et al. Aerobic fitness reduces brain tissue loss in aging humans. J Gerontol A Biol Med Sci. 2003;58(2):176–80.
Zhu N, Jacobs DR Jr, Schreiner PJ, Launer LJ, Whitmer RA, Sidney S, et al. Cardiorespiratory fitness and brain volume and white matter integrity: the CARDIA study. Neurology. 2015;84(23):2347–53.
Colcombe SJ, Erickson KI, Scalf PE, Kim JS, Prakash R, McAuley E, et al. Aerobic exercise training increases brain volume in aging humans. J Gerontol A Biol Med Sci. 2006;61(11):1166–70.
Mortimer JA, Ding D, Borenstein AR, DeCarli C, Guo Q, Wu Y, et al. Changes in brain volume and cognition in a randomized trial of exercise and social interaction in a community-based sample of non-demented Chinese elders. J Alzheimers Dis. 2012;30(4):757–66.
Voss MW, Heo S, Prakash RS, Erickson KI, Alves H, Chaddock L, et al. The influence of aerobic fitness on cerebral white matter integrity and cognitive function in older adults: results of a one-year exercise intervention. Hum Brain Mapp. 2013;34(11):2972–85.
Hamer M, Sharma N, Batty GD. Association of objectively measured physical activity with brain structure: UK biobank study. J Intern Med. 2018;284(4):439–43.
Abbott RD, White LR, Ross GW, Masaki KH, Curb JD, Petrovich H. Walking and dementia in physically capable elderly men. JAMA. 2004;292:1447–53.
Best JR, Rosano C, Aizenstein HJ, Tian Q, Boudreau RM, Ayonayon HN, et al. Long-term changes in time spent walking and subsequent cognitive and structural brain changes in older adults. Neurobiol Aging. 2017;57:153–61.
Spartano NL, Davis-Plourde KL, Himali JJ, Andersson C, Pase MP, Maillard P, et al. Association of accelerometer-measured light-intensity physical activity with brain volume: The Framingham Heart Study [published correction appears in JAMA Network Open. 2019;2(5):e195153]. JAMA Network Open. 2019;2(4):e192745.
Leckie RL, Oberlin LE, Voss MW, Prakash RS, Szabo-reed A, Chaddock-Heyman L, et al. BDNF mediates improvements in executive function following a 1-year exercise intervention. Front Hum Neurosci. 2014;8:985.
Brasure M, Desai P, Davila H, Nelson VA, Calvert C, Jutkowitz E, et al. Physical activity interventions in preventing cognitive decline and Alzheimer-type dementia: a systematic review. Ann Intern Med. 2018;168:30–8.
Hamer M, Chida Y. Physical activity and risk of neurodegenerative disease: a systematic review of prospective evidence. Psychol Med. 2009;39(1):3–11.
Middleton LE, Manini TM, Simonsick EM, Harris TB, Barnes DE, Tylavsky F, et al. Activity energy expenditure and incident cognitive impairment in older adults. Arch Intern Med. 2011;171(14):1251–7.
Stubbs B, Chen LJ, Chang CY, Sun WJ, Ku PW. Accelerometer-assessed light physical activity is protective of future cognitive ability: a longitudinal study among community dwelling older adults. Exp Gerontol. 2017;91:104–9.
Doi T, Makizako H, Shimada H, Tsutsumimoto K, Hotta R, Nakakubo S, et al. Objectively measured physical activity, brain atrophy, and white matter lesions in older adults with mild cognitive impairment. Exp Gerontol. 2015;62:1–6.
Alosco ML, Brickman AM, Spitznagel MB, Sweet LH, Josephson R, Griffith E, et al. Daily physical activity is associated with subcortical brain volume and cognition in heart failure. J Int Neuropsychol Soc. 2015;21(10):851–60.
Arnardottir NY, Koster A, Domelen DRV, Brychta RJ, Caserotti P, Eiriksdottir G, et al. Association of change in brain structure to objectively measured physical activity and sedentary behavior in older adults: age, gene/environment susceptibility-Reykjavik study. Behav Brain Res. 2016;296:118–24.
Gow AJ, Bastin ME, Muñoz Maniega S, Valdés Hernández MC, Morris Z, Murray C, et al. Neuroprotective lifestyles and the aging brain: activity, atrophy, and white matter integrity. Neurology. 2012;79(17):1802–8.
Halloway S, Arfanakis K, Wilbur J, Schoeny ME, Pressler SJ. Accelerometer physical activity is associated with greater gray matter volume in older adults without dementia or mild cognitive impairment. J Gerontol B Psychol Sci Soc Sci. 2018;74(7):1142–51.
Stephan AJ, Strobl R, Müller M, Holle R, Autenrieth CS, Thorand B, et al. A high level of household physical activity compensates for lack of leisure time physical activity with regard to deficit accumulation: results from the KORA-age study. Prev Med. 2016;86:64–9.
Podewills LJ, Guallar E, Kuller LH, Fried LP, Lopez OL, Carlson M, et al. Physical activity, APOE genotype, and dementia risk: findings from the cardiovascular health cognition study. Am J Epidemiol. 2005;161(7):639–51.
Verghese J, Lipton RB, Katz MJ, Hall CB, Derby CA, Kuslansky G, et al. Leisure activities and the risk of dementia in the elderly. N Engl J Med. 2003;348(25):2508–16.
Welsh KA, Breitner JCS, Magruder-Habib KM. Detection of dementia in elderly using telephone screening of cognitive status. NNBN. 1993;6(2):103–10.
Wilson PW. D’Agostino RB, levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–47.
D’Agostino RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care. Framingham Heart Study. Circulation. 2008;117:743–53.
Delis DC, Kramer JH, Kaplan E, Ober BA. Manual for the California verbal learning test, (CVLT-II). San Antonio: The Psychological Corporation; 2003.
Wechsler D. Manual for the Wechsler memory scale-revised. San Antonio: The Psychological Corporation; 1987.
Wechsler D. Wechsler memory scale–3rd edition manual. San Antonio: The Psychological Corporation; 1997.
Wechsler D. WAIS-III Administration and scoring manual. San Antonio: The Psychological Association; 1997.
Wechsler D. Manual for the Wechsler adult intelligence scale-revised. New York: Psychological Corporation; 1981.
Nelson HE. A modified card sorting test sensitive to frontal lobe defects. Cortex. 1976;12:313–24.
Spreen O, Strauss E. A compendium of neuropsychological tests: Administration, norms and commentary. 2nd ed. Oxford: Oxford University Press; 1998.
Reitan RM, Wolfson D. The Halstead-Reitan neuropsychological test battery: Theory and clinical interpretation. 2nd ed. Tucson: Neuropsychology Press; 1992.
Desikan RS, Segonne F, Fischl B, Quinn BT, Dickerson BC, Blacker D, et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage. 2006;3:968–80.
Voevodskaya O, Simmons A, Nordenskjöld R, Kullberg J, Ahlström H, Lind L, et al. The effects of intracranial volume adjustment approaches on multiple regional MRI volumes in healthy aging and Alzheimer's disease. Front Aging Neurosci. 2014;6(264):1–14.
Gill DP, Jones GR, Zou GY, Speechley M. The phone-FITT: a brief physical activity interview for older adults. J Aging Phys Act. 2008;16:292–315.
R Core Team. R: A Language and Environment for Statistical Computing. Vienna: R Core Team; 2019.
Meusel LC, Greenwood CE, Maione A, Tchistiakova E, MacIntosh BJ, Anderson ND. Cardiovascular risk and encoding-related hippocampal connectivity in older adults. BMC Neurosci. 2019;20(1):37.
Fox J, Weisberg S. An R Companion to Applied Regression. 3rd ed. Thousand Oaks; 2019.
Lear SA, Weihong H, Sumathy R, Gasevic D, Leong D, Iqbal R, et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet. 2017;390(10113):2643–54.
Ross R, Mcguire KA. Incidental physical activity is positively associated with cardiorespiratory fitness. Med Sci Sports Exerc. 2011;44(11):2189–94.
Sanchez-Lopez J, Silva-Pereyra J, Fernández T, Alatorre-Cruz GC, Castro-Chavira SA, González-López M, et al. High levels of incidental physical activity are positively associated with cognition and EEG activity in aging. PLoS One. 2018;13(1):e0191561.
Bherer L, Kramer AF, Peterson MS, Colcombe S, Erickson K, Becic E. Transfer effects in task-set cost and dual-task cost after dual-task training in older and younger adults: further evidence for cognitive plasticity in attentional control in late adulthood. Exp Aging Res. 2008;34:188–219.
Buitenweg JI, Murre JM, Ridderinkhof KR. Brain training in progress: a review of trainability in seniors. Front Hum Neurosci. 2012;6:183.
Kim H, Chey J, Lee S. Effects of multicomponent training of cognitive control on cognitive function and brain activation in older adults. Neurosci Res. 2017;124:8–15.
Stamenova V, Levine B. Effectiveness of goal management training in improving executive functions: a meta-analysis. Neuropsychol Rehabil. 2019;29:1–31.
Daminger A. The cognitive dimension of labor. Am Sociol Rev. 2019;84(4):609–33.
Harvey JA, Chastin SFM, Skelton DA. Prevalence of sedentary behavior in older adults: a systematic review. Int J Environ Res Public Health. 2013;10(12):6645–61.
Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162(2):123–32.
Patterson R, McNamara E, Tainio M, Herick de Sa T, Smith AD, Sharp SJ, et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol. 2018;33:811.
Leitzman MF. Sedentary behaviour epidemiology. 1st ed. Cham: Springer International Publishing; 2018.
Tremblay MS, Colley RC, Saunders TJ, Healy GN, Owen N. Physiological and health implications of a sedentary lifestyle. Appl Physiol Nutr Metab. 2010;24:725–40.
Klaren RE, Hubbard EA, Wetter NC, Sutton BP, Motl RW. Objectively measured sedentary behavior and brain volumetric measurements in multiple sclerosis. Neurodegener Dis Manag. 2017;7(1):31–7.
Falck RS, Davis JC, Liu-Ambrose T. What is the association between sedentary behaviour and cognitive function? A systematic review. Br J Sports Med. 2017;51(10):800–11.
Duvivier BMFM, Schaper NC, Koster A, van Kan L, Peters HPF, Adam JJ, et al. Benefits of substituting sitting with standing and walking in free-living conditions for cardiometabolic risk markers, cognition, and mood in overweight adults. Front Physiol. 2017;8:353.
Wheeler MJ, Dempsey PC, Grace MS, Ellis KA, Gardiner PA, Green DJ, et al. Sedentary behavior as a risk factor for cognitive decline? A focus on the influence of glycemic control for brain health. Alzheimers Dement. 2017;3(3):291–300.
Fletcher E, Gavett B, Harvey D, Tomaszewski Farias S, Olichney J, Beckett L, et al. Brain volume change and cognitive trajectories in aging. Neuropsychology. 2018;32(4):436–49.
Royle NA, Booth T, Valdéz Hernández MC, Penke L, Murray C, Gow AJ, et al. Estimated maximal and concurrent brain volume predict cognitive ability in old age. Neurobiol Aging. 2013;34(12):2726–33.
Acknowledgements
The authors would like to acknowledge the participants, imaging technologists, and volunteers that did quality checking on study data and MRI scans at Baycrest Health Science Centre.
Funding
This study was supported in part by an Operating Grant from the Canadian Institutes of Health Research (111244). The salary of NK was supported by a grant from the Canadian Consortium on Neurodegeneration in Aging, which is supported by the Canadian Institutes of Health Research with funding from several partners to CG.
Author information
Authors and Affiliations
Contributions
NK contributed to the data acquisition, analysis, interpretation and manuscript preparation and revision. LM contributed to data acquisition, analysis, interpretation, and manuscript revision. NA contributed to conception and design of work, data interpretation and manuscript revision. CG contributed to conception and design of work, data interpretation and manuscript revision. All authors gave final approval of the manuscript to be published and were accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The work described was carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans and was approved by the Research Ethics Board at Baycrest. All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Koblinsky, N.D., Meusel, LA.C., Greenwood, C.E. et al. Household physical activity is positively associated with gray matter volume in older adults. BMC Geriatr 21, 104 (2021). https://doi.org/10.1186/s12877-021-02054-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-021-02054-8