Abstract
Background
Hospitals are in need of valid and economic screening and assessment tools that help identifying older patients at risk for complications which require intensified support during their hospital stay.
Methods
Five hundred forty-seven internal medicine in-patients (mean age 78.14 ± 5.96 years; 54.7% males) prospectively received Identification of Seniors at Risk (ISAR) screening. If screening results were positive (ISAR score ≥ 2), a comprehensive geriatric assessment (CGA) was performed. We explored sensitivity and specificity of different ISAR and CGA cutoffs. Further, we analyzed the risk of falls and how patients got discharged from hospital.
Results
ISAR+/CGA abnormal patients spent more days in hospital (16.1 ± 14.5), received more nursing hours per day (3.0 ± 2.3), more hours of physiotherapy during their hospital stay (2.2 ± 3.2), and had more falls (10.1%) compared to ISAR+/CGA normal (10.9 ± 12.3, 2.0 ± 1.2, 1.2 ± 4.3, and 2.8%, respectively, all p ≤ 0.016) and ISAR- (9.6 ± 11.5, 2.3 ± 4.5, 0.7 ± 2.0, and 2.2%, respectively, all p ≤ 0.002) patients. ISAR+/CGA abnormal patients terminated their treatment regularly with being discharged back home less often (59.6%) compared to ISAR+/CGA normal (78.5%, p = 0.002) and ISAR- (78.2%, p = 0.056) patients. ISAR cutoff≥2 and CGA defined as abnormal in case of impairment of ADL plus another CGA domain achieved best sensitivity/specificity.
Conclusions
Abnormal geriatric risk screening and assessment are associated with longer hospital stay and higher amount of nursing and physiotherapy during hospital stay, greater risk of falling, and a lower percentage of successfully terminated treatment in older in-patients.
Similar content being viewed by others
Background
Due to ongoing demographic aging, hospitals face a constantly rising number of older patients with multimorbidity [1,2,3]. Although older people represent a challenge for the hospital setting, excellent medical attendance and high-quality care should be ensured. The use of screening tools allows for the identification of older patients at increased risk for poor health outcomes. Worldwide, geriatric societies demand the implementation of screening tools for the early identification of patients at increased risk for poor health outcomes [4,5,6]. The Identification of Seniors at Risk (ISAR) screening is one of the most commonly used tools with high sensitivity for the prediction of poor health outcomes in older patients entering emergency departments [7]. Created as a screening tool, ISAR requires a second-step diagnostic tool for patients with positive screening results. Comprehensive geriatric assessment (CGA) that evaluates impairments of activities of daily living (ADL), mobility, cognition, and mood as well as comorbidities is usually performed on patients with a positive screening result. Despite being only a diagnostic tool and not an intervention strategy, CGA preceded by ISAR screening has already been shown to reduce the risk for poor health outcomes in older patients attending emergency departments [8]. It further improves postoperative outcomes (mortality, delirium, and length of hospital stay) in older patients with colorectal carcinoma undergoing elective resection [9]. In addition, the probability of living at home one year after being released from hospital was about 16% higher in geriatric hospitalized patients undergoing CGA compared to those who received the usual care [1]. These data suggest that CGA leads to an improvement of individual patient health outcomes while lowering the costs associated with diseases, nursing, and health care [10].
Besides emergency department patients and in-patients undergoing surgery, patients admitted to internal medicine departments also challenge healthcare professionals to identify needs and risks for poor health outcomes. Since ISAR was originally designed as a screening tool in emergency departments, we herein extended ISAR’s utility and used the ISAR for defining the health outcome of older hospitalized internal medicine patients. We sought to determine the association between ISAR screening (with CGA if positive on screening) and length of stay, nursing and physiotherapy hours, risk of falls, and discharge disposition among older adults admitted to internal medicine departments. In sensitivity analyses, we explored the sensitivity and specificity of different ISAR and CGA cutoffs for identifying outcomes among older adults admitted to internal medicine departments.
Methods
Study cohort
Patients admitted to internal medicine wards of the University Hospital Essen via emergency departments or as selective inpatient admission or being transferred from another ward or hospital from July 2015 to February 2017 were included in the present study if they received ISAR screening and were (a) ≥75 years of age in the Department of Gastroenterology and Hepatology and the Department of Cardiology and Angiology or (b) aged ≥65 years in the Department of Nephrology. Nephrological patients were included based on a younger age criterion as their biological age appears to be higher than their chronological age [11, 12]. We decided to apply ISAR in these three departments because these departments cover all significant geriatric patient groups in our University Hospital within the internal medicine specialty. ISAR screenings were conducted by the nursing staff on admission and were only missed when there was a lack of time, language barriers or incompliant patients. Those who were not given ISAR were excluded from any further analyses. In case of a positive ISAR screening result, CGA was performed by a geriatric liaison service usually the day following ISAR screening and 3 days after admission the latest. The geriatric liaison service of the University Hospital Essen consisted of a geriatrician, an occupational therapist, and a psychologist. In all subjects, patient histories involving information about comorbidities and vascular risk factors were taken from the electronical Hospital Information System Cerner medico. The study was approved by the ethics committee of the University Duisburg-Essen and need for consent was waived.
Measurement methods
ISAR
In this study, we utilized a version of ISAR by Warburton [13] validated for patients aged ≥75 years which was a modification of the original test by McCusker et al. [14]. The ISAR consists of six items, each being a simple yes-no question about the following domains: Premorbid functional dependence, acute change in functional dependence within the last 24 h, recent hospitalization within the last 6 months, visual impairment, impaired memory and polypharmacy (≥6 medications). The ISAR score ranges from 0 to 6 points, with a cutoff ≥2 interpreted as positive (abbreviated as ISAR+) and indicating increased risk for poor health outcomes.
CGA
Since there is an ongoing discussion on which geriatric impairments are associated with deteriorated health condition, we analyzed different definitions of an abnormal CGA, which included the Barthel index for the assessment of impairment of ADL [15, 16], the Timed Up & Go [17] and the Tinetti Mobility Test [18] measuring impairment of mobility, the Mini-Mental State Examination Test (MMSE) [19] and the Clock-Drawing Test [20] assessing impairment of cognition, and the Geriatric Depression Scale (GDS) [21, 22] for the assessment of signs of depression. The Barthel index is a questionnaire assessing daily competences in which patients can reach a maximum score of 100 and scores < 90 are interpreted as abnormal [23]. Mobility was rated as impaired if Timed Up & Go was ≥20 s [24] or if patients had scores < 20 in the Tinetti Mobility Test [25]. Impaired cognition was defined as MMSE ≤27 [26, 27] or Clock-Drawing Test ≥3 [20] and a GDS score ≥ 6 [28] was interpreted as a sign of depression. If not noted differently, we interpreted CGA as abnormal in this study if Barthel index and one other domain (mobility, cognition, or signs of depression) were impaired (abbreviated as ISAR+/CGA abnormal) as suggested by Campbell et al. [29].
Health outcome variables
As indicators for poor health outcomes, we analyzed length of hospital stay, nursing hours per day, physiotherapy workload, falls during the hospitals stay, and type of discharge from hospital using data obtained from the electronical Hospital Information System Cerner medico. Nursing hours were operationalized using the “Leistungserfassung in der Pflege”, a scientifically valid tool documenting nursing workload (for further details see Gronewold et al. [30]).
We also reported the patients’ type of hospital discharge. We classified if patients terminated their treatment regularly with being discharged back home or being transferred to further medical care. Further medical care was split into planned or unplanned subsequent readmission, transfer to other hospitals, and transfer to rehabilitation or nursing institution. We also indicated whether treatment was terminated against medical advice and if the patients died while in hospital.
Statistical analysis
Continuous data are presented as mean ± SD values, categorical data as counts (%). Comparisons between negative ISAR screening (ISAR-), ISAR+/CGA normal and ISAR+/CGA abnormal groups regarding demographic data, risk factors and comorbidities, number of falls, type of discharge, length of hospital stay, and nursing and physiotherapy hours were done with (1) one-way ANOVA followed by Games Howell post-hoc tests for normally distributed continuous data (age), (2) Kruskal-Wallis tests and post-hoc Mann-Whitney u test (corrected for multiple comparisons where needed) for not normally distributed continuous data (length of hospital stay, hours of nursing per day and physiotherapy during hospital stay) and (3) Pearson’s chi-square or Fisher’s exact tests for categorical data.
Since CGA is costly and time-consuming, screening instruments with high sensitivity and specificity for the identification of patients needing further risk assessment are needed. Thus, we analyzed the sensitivity and specificity of different ISAR cutoffs for the prediction of length of hospital stay (≥7 days), nursing (above median) and receiving physiotherapy (yes/no). Further, we used receiver operating characteristics (ROC) including the area under the curve (AUC) and confidence intervals as well as Youden’s J statistics [sensitivity + specificity − 1]. Since there is no agreement on which tests a CGA should include and when a CGA should be interpreted as abnormal, we analyzed different definitions of an abnormal CGA. In line with published suggestions [31, 32], abnormal CGA was first defined as significant impairment of ADL combined with impairment of one other CGA test domain (cognition, mobility or signs of depression). In sensitivity/specificity analyses, we also evaluated alternative definitions. Again, we used these different alternative definitions of abnormal CGA for the prediction of length of hospital stay (≥7 days), nursing (above median) and receiving physiotherapy (yes/no) and calculated the Youden’s J statistics.
P values ≤0.05 indicate statistical significance and are shown in bold in the tables. All statistics were performed using Statistical Packing for Social Science 22 (SPSS 22) for Windows (SPSS, Chicago, IL, U.S.A.).
Results
Study cohort
Demographic and medical data
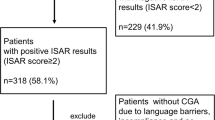
Of 1329 patients fulfilling the above inclusion criteria (76.62 ± 6.3 years, 55.7% males), 547 patients (41.2%) received ISAR screenings. Patients receiving ISAR screenings were 78.1 ± 6.0 years old (54.7% males) and stayed in hospital for 11.22 ± 13.9 days, patients not receiving ISAR screening were slightly younger (75.66 ± 6.40 years, 56.5% males) and stayed in hospital considerably shorter for 8.96 ± 11.9 days. Of the 547 screened patients, 318 (58.1%) had a positive screening result (ISAR score ≥ 2). Of these patients, 242 (76.1%) received a subsequent CGA, which was abnormal in 97 (40.1%) patients. The 76 ISAR+ patients who did not receive CGA did not differ significantly from ISAR+ patients who received CGA on patients’ characteristics in Table 1. Reasons for not performing a CGA despite positive screening results were transfer to another hospital or ward, discharge, foreign-language barriers or incompliance of patients.
Demographic and medical data including comorbidities and risk factors for the total cohort and split by ISAR and CGA results are shown in Table 1. Various diseases were coded as main medical diagnoses leading to hospital admission (Table 2). Nearly 80% of the cohort suffered from comorbid arterial hypertension and about half of the cohort suffered from hyperlipoproteinemia. Clinical diagnosis of dementia and depression known before the CGA had a rather low prevalence of 7 and 6% in the total cohort.
ISAR screening and CGA results
More than half of the total cohort showed recent hospitalization (61.2%) and polypharmacy (56.5%) whereas premorbid functional dependence (25.2%), acute change in functional dependence (20.1%), impaired vision (10.6%) and impaired memory (18.3%) were reported less often (Fig. 1). Looking at the domains affected, 47.3% of the total cohort had impaired ADL, 35.6% impaired mobility, 54.4% impaired cognition, and 11.6% showed signs of depression. Interestingly, even in patients without prior dementia diagnosis, 51.9% had impaired cognition in CGA and in patients without prior diagnosis of depression we found signs of depression in 11.4% in CGA.
Sensitivity and specificity analyses of different ISAR cutoffs for the prediction of length of hospital stay, nursing hours and physiotherapy
The ROC results for the ISAR screening for the prediction of a hospital stay ≥7 days, i.e., the precondition for geriatric rehabilitation in several countries including Germany, revealed an AUC = 0.593 (95% CI = 0.545–0.640), indicating poor discriminating ability of ISAR. Yet, compared to other cutoffs, the Youden’s J index still revealed best performance for the ≥2 cutoff as suggested in the literature [33], with a true positive rate (sensitivity) of 0.643 and false positive rate (1-specificity) of 0.520 (Fig. 2).
The analysis of the predictive value for the ISAR in predicting nursing hours split by the median (≥2 h) exposed an AUC of 0.632 (95% CI = 0.583–0.682). The Youden’s J index revealed a similar performance for an ISAR cutoff ≥2 and ISAR cutoff ≥3. However, sensitivity of the ISAR cutoff ≥3 was low, which is undesirable for a screening tool (Fig. 2). For the ISAR cutoff ≥2, the sensitivity was 0.696 with a false positive rate of 0.502.
Since only about one quarter of the total cohort (28.7%) received physiotherapy, we analyzed the predictive value of the ISAR score for receiving physiotherapy (yes/no) which resulted in an AUC of 0.603 (95% CI = 0.550–0.657), again with best performance for the ISAR cutoff ≥2 with a sensitivity of 0.691 and a false positive rate of 0.539.
Sensitivity and specificity analyses of different CGA abnormal definitions for the prediction of needs (length of hospital stay, nursing hours and physiotherapy)
The definition of an abnormal CGA in case of impairment of ADL plus one other test of the CGA was present in 40.9% of patients. This definition resulted in the best trade-off between sensitivity and false positive rate for the prediction of an increased length of hospital stay and receiving physiotherapy (Tables 3, 5). Only for the prediction of increased nursing, the definition of impairment of ADL plus impairment of cognition or signs of depression (alternative definition A, present in 33.1% of patients) achieved the best performance (Table 4). The definition of impairment of ADL plus impairment of mobility (alternative definition B, present in 28.5%) achieved the lowest performance for all outcomes (Tables 3, 4 and 5).
Associations of ISAR and CGA results with health outcome (length of hospital stay, nursing and physiotherapy hours, incident fall and type of discharge)
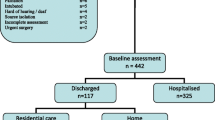
Using the ISAR ≥2 cutoff and definition of abnormal CGA as impairment of ADL plus another domain, ISAR+/CGA abnormal patients and ISAR+/CGA normal patients stayed significantly longer in hospital (17.35 ± 18.80 and 10.95 ± 11.85 days) than ISAR- patients (9.60 ± 11.46 days, both comparisons p < 0.001, Fig. 3).
Effects of ISAR and CGA results on length of hospital stay, nursing hours per day and total hours of physiotherapy during hopital stay. CGA, Comprehensive Geriatric Assessment; ISAR, Identification of Seniors at Risk; ISAR+, positive ISAR screening (score ≥ 2); ISAR-, negative ISAR screening (score < 2); CGA abnormal, impairment of ADL plus another domain of the CGA. *p ≤ 0.05 compared to ISAR-, †p ≤ 0.05 compared to ISAR+/ CGA normal
ISAR+/CGA abnormal patients also received significantly more hours of nursing care (2.98 ± 2.32) and physiotherapy (2.19 ± 3.19) than ISAR- patients (2.30 ± 4.46 and 0.67 ± 2.02, both p < 0.001) and ISAR+/CGA normal patients (1.97 ± 1.18 and 1.19 ± 4.30, both p < 0.001, Fig. 3).
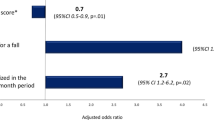
Incident falls occurred in 4.0% (n = 19) of the total cohort with a significantly higher number of falls in ISAR+/CGA abnormal patients (10.1%, n = 10) than in ISAR- (2.2%, n = 5, p = 0.002) and ISAR+/CGA normal (2.8%, n = 4, p = 0.016) patients.
Although in the total cohort most of the patients terminated their treatment regularly with discharge back home, fewer ISAR+/CGA abnormal patients terminated their treatment regularly with discharge back home (59.6%) compared to ISAR+/ CGA normal (78.5%, p = 0.002) and ISAR- (78.2%, p = 0.056) patients (see Table 6).
Discussion
While there is a growing interest in understanding the role of geriatric problems for poor health outcomes, there is little information on how geriatric risk screening followed by CGA affects health outcomes of patients hospitalized in internal medicine environments. We demonstrated that abnormal ISAR screening and CGA results were associated with longer hospital stay, more hours of nursing and physiotherapy, higher number of falls and a lower percentage of regularly terminated treatments. In line with previous suggestions [33], an ISAR cutoff ≥2 and the definition of an abnormal CGA as impairment of ADL plus impairment of another CGA domain best predicted patient health outcomes (length of hospital stay, nursing, and physiotherapy hours).
Almost 60% of our patient cohort had a positive ISAR screening, which is comparable to previous studies using similar patient cohorts from emergency departments. In 667 patients aged ≥70 years from emergency departments in the United Kingdom (mean age 80 years), 69% had a positive ISAR screening [34]. In 258 patients aged ≥65 years (mean age: 79 years) from a Canadian emergency department 61.2% screenings were positive [35]. About 40% of our cohort receiving CGA due to positive ISAR screening had an abnormal CGA defined as impairment of ADL plus another domain of the CGA.
In data from the Department of Orthopedics and Trauma Surgery of the University Hospital Essen, we observed a higher proportion of positive ISAR screenings and abnormal CGA results [30]. However, this study revealed similar associations of ISAR and GCA with length of hospital stay and amount of nursing hours indicating suitability of ISAR and CGA in different clinical specialties.
Our ROC results indicated a low discriminating ability of the ISAR tool for length of hospital stay, nursing hours and physiotherapy. This is in line with previous studies demonstrating that ISAR lacks sufficient prognostic validity for various short- and long-term outcomes [7] in contrast to the original development and validation study stating fair performance [36]. A Dutch study including 177 patients aged ≥65 years admitted to internal medicine departments, who were subjected to ISAR, showed sensitivity, specificity and AUC for functional decline measured by self-reported Katz ADL index of 92.9, 39.3% and 0.67, respectively [37, 38]. The different values, specifically for sensitivity, indicate that ISAR may be more suitable for predicting functional decline than length of hospital stay, nursing hours and physiotherapy. Since the present study is based on data available during hospital stay, information about long-term outcomes after the hospital stay including mortality, readmission to hospital or not being able to live at home independently is not available.
We must consider that we applied ISAR screening in internal medicine wards and not in emergency department setting, representing the original and validated setting. Including patients who were already hospitalized, we created a more homogenous patient cohort compared to emergency department setting. In the original studies by McCusker’s group [8, 14, 36], only 35% of the tested emergency department patients were subsequently admitted to the hospital. Further, ISAR was designed for patients aged ≥65 years. In our study cohort inclusion criterion was in most cases an age of ≥75 years, again creating a more homogenous patient group. The low performance of ISAR in ROC analyses could therefore lead to a misclassification which could result in over- or underuse of medical resources. Of course, older patients with higher risk require the provision of a sufficient amount and quality of care which a relevant and indispensable cost factor in hospital and health management [39]. However, since medical resources are valuable but limited, ISAR, alone or combined with CGA, can only be a single element in a process leading to the allocation of patient support.
To the best of our knowledge, this is the first study evaluating the predictive value of ISAR screening and CGA for hospitalized patients’ health outcomes in internal medicine departments. Based on our results, ISAR screening alone may not be suitable for identifying the needs of older hospitalized patients, whereas combination with CGA may allow for the detection of patients requiring longer hospital stay, requiring more hours of nursing and physiotherapy, exhibiting higher risk of falls and having a lower percentage of regularly terminated treatments. Thus, ISAR could help to decide time- and cost-efficiently, which patients should receive a CGA and subsequently be targeted by geriatric interventions [37, 40]. Our findings emphasize that ISAR screenings and CGA should be applied at the time point of a patient’s hospitalization since positive screening and abnormal CGA was associated with more falls during the subsequent hospital stay. The initial use of screening tools is in line with previous recommendations of international geriatric societies [41, 42].
As major limitation, only 41.2% of all eligible patients in our cohort received ISAR screening which, although comparable to other screening implementation trials [35], may not allow truly representative statements for older patient populations, which raises the need for cautious data interpretation. Further limitations are intrinsic to the nature of the ISAR and CGA instruments. It needs to be questioned whether ISAR can reliably be applied to patients with cognitive impairment, which is a common phenomenon in older patient cohorts, since these patients may not answer the ISAR item about memory problems correctly. Furthermore, our CGA did not differentiate the nature of cognitive deficits, which in the setting of acute hospitalized patients may either be related to mild cognitive impairment, dementia or delirious states. Additional influencing factors, such as nutritional status, psychosocial factors or lack of social support, were not assessed. Patients with short hospital stays were under-represented in the cohort receiving ISAR screening followed by CGA. The low ISAR completion rate of 41.2% mirrors some key barriers in the implementation of new screening procedures which requires the compliance of both, patients and staff.
Conclusions
Abnormal geriatric risk screening and assessment are associated with longer hospital stay and higher amount of nursing and physiotherapy during hospital stay, greater risk of falling, and a lower percentage of successfully terminated treatment in older in-patients. An ISAR cutoff ≥2 and the definition of an abnormal CGA as impairment of ADL plus impairment of another CGA domain best predicted patient health outcomes in our study. Further efforts are urgently needed to optimize geriatric patient management. By increasing the awareness of health professionals, we should be able to establish improved health support procedures that may prevent unfavorable patient outcomes.
Availability of data and materials
All relevant data are within the paper. If additional data is needed it can be made available from the ethical committee of the University Duisburg-Essen (ethikkommission@uk-essen.de) for researchers who meet the criteria for access to confidential data by contacting the corresponding author.
Abbreviations
- ADL:
-
Activities of daily living
- AUC:
-
Area under the curve
- CGA:
-
Comprehensive geriatric assessment
- CI:
-
Confidence interval
- GDS:
-
Geriatric Depression Scale
- ISAR:
-
Identification of Seniors at Risk screening
- ISAR-:
-
ISAR screening negative < 2
- ISAR+:
-
ISAR screening positive ≥ 2
- ISAR+/CGA abnormal:
-
ISAR screening positive ≥ 2, but abnormal results in CGA
- ISAR+/CGA normal:
-
ISAR screening positive ≥ 2, but normal results in CGA
- MMSE:
-
Mini Mental State Examination
- SD:
-
Standard deviation
- SPSS 22:
-
Statistical Packing for Social Science 22
References
Ellis G, Whitehead MA, O'Neill D, Langhorne P, Robinson D. Comprehensive geriatric assessment for older adults admitted to hospital. The Cochrane database of systematic reviews. 2011;7:Cd006211.
Aaldriks AA, Maartense E, le Cessie S, Giltay EJ, Verlaan HA, van der Geest LG, Kloosterman-Boele WM, Peters-Dijkshoorn MT, Blansjaar BA, van Schaick HW, et al. Predictive value of geriatric assessment for patients older than 70 years, treated with chemotherapy. Crit Rev Oncol Hematol. 2011;79(2):205–12.
Etman A, Burdorf A, Van der Cammen TJM, Mackenbach JP, Van Lenthe FJ. Socio-demographic determinants of worsening in frailty among community-dwelling older people in 11 European countries. J Epidemiol Community Health. 2012;66(12):1116–21.
Conroy S, Nickel CH, Jónsdóttir AB, Fernandez M, Banerjee J, Mooijaart S, Sjöstrand F, Devriendt E, Ganansia O, Martín Sánchez FJ, et al. The development of a European curriculum in geriatric emergency medicine. European Geriatric Medicine. 2016;7(4):315–21.
Sanders AB. Care of the elderly in emergency departments: conclusions and recommendations. Ann Emerg Med. 1992;21(7):830–4.
Thiem U, Greuel HW, Reingraber A, Koch-Gwinner P, Pullen R, Heppner HJ, Pfisterer M. Consensus for the identification of geriatric patients in the emergency care setting in Germany. Z Gerontol Geriatr. 2012;45(4):310–4.
Galvin R, Gilleit Y, Wallace E, Cousins G, Bolmer M, Rainer T, Smith SM, Fahey T. Adverse outcomes in older adults attending emergency departments: a systematic review and meta-analysis of the identification of seniors at risk (ISAR) screening tool. Age Ageing. 2017;46(2):179–86.
McCusker J, Verdon J, Tousignant P, de Courval LP, Dendukuri N, Belzile E. Rapid emergency department intervention for older people reduces risk of functional decline: results of a multicenter randomized trial. J Am Geriatr Soc. 2001;49(10):1272–81.
Indrakusuma R, Dunker MS, Peetoom JJ, Schreurs WH. Evaluation of preoperative geriatric assessment of elderly patients with colorectal carcinoma. A retrospective study. European Journal of Surgical Oncology (EJSO). 2015;41(1):21–7.
Ellis G, Gardner M, Tsiachristas A, Langhorne P, Burke O, Harwood RH, Conroy SP, Kircher T, Somme D, Saltvedt I, et al. Comprehensive geriatric assessment for older adults admitted to hospital. The Cochrane database of systematic reviews. 2017;9:Cd006211.
Kumar S, Bogle R, Banerjee D. Why do young people with chronic kidney disease die early? World J Nephrol. 2014;3(4):143–55.
Foley RN, Parfrey PS, Sarnak MJ. Clinical epidemiology of cardiovascular disease in chronic renal disease. American journal of kidney diseases : the official journal of the National Kidney Foundation. 1998;32(5 Suppl 3):S112–9.
Warburton RN, Parke B, Church W, McCusker J. Identification of seniors at risk: process evaluation of a screening and referral program for patients aged > or =75 in a community hospital emergency department. Int J Health Care Qual Assur Inc Leadersh Health Serv. 2004;17(6):339–48.
McCusker J, Bellavance F, Cardin S, Trepanier S, Verdon J, Ardman O. Detection of older people at increased risk of adverse health outcomes after an emergency visit: the ISAR screening tool. J Am Geriatr Soc. 1999;47(10):1229–37.
Mahoney FI, Barthel DW. Functional evaluation: the BARTHEL index. Maryland state medical journal. 1965;14:61–5.
Heuschmann PU, Kolominsky-Rabas PL, Nolte CH, Hunermund G, Ruf HU, Laumeier I, Meyrer R, Alberti T, Rahmann A, Kurth T, et al. The reliability of the german version of the barthel-index and the development of a postal and telephone version for the application on stroke patients. Fortschr Neurol Psychiatr. 2005;73(2):74–82.
Podsiadlo D, Richardson S. The timed “up & go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8.
Tinetti ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34(2):119–26.
Folstein MF, Folstein SE, McHugh PR. “mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Shulman KI, Pushkar Gold D, Cohen CA, Zucchero CA. Clock-drawing and dementia in the community: a longitudinal study. International journal of geriatric psychiatry. 1993;8(6):487–96.
Yesavage JA, Sheikh JI. 9/geriatric depression scale (GDS). Clin Gerontol. 1986;5(1–2):165–73.
Gauggel S, Birkner B. Validität und Reliabilität einer deutschen Version der Geriatrischen Depressionsskala (GDS). Z Klin Psychol Psychother. 1999;28(1):18–27.
Schulc E, Pallauf M, Mueller G, Wildbahner T, Them C. Is the Barthel index an adequate assessment tool for identifying a risk group in elderly people living at home? Int J Nurs Clin Pract. 2015;2015.
Lysack CL. Chapter 23 - Household and Neighborhood Safety, Mobility. In: Lichtenberg PA, editor. Handbook of Assessment in Clinical Gerontology (Second Edition). San Diego: Academic Press; 2010. p. 619–46.
Zemke J. Assessment Tinetti-test (performance oriented mobility assessment – POMA). GGP. 2018;02(01):13–5.
Kessler J, Markowitsch H, Denzler P. Mini-mental-status-test (MMST). Göttingen: Beltz Test GMBH. 2000;24.
Kukull WA, Larson EB, Teri L, Bowen J, McCormick W, Pfanschmidt ML. The mini-mental state examination score and the clinical diagnosis of dementia. J Clin Epidemiol. 1994;47(9):1061–7.
Sheikh JI, Yesavage JA: Geriatric depression scale (GDS): recent evidence and development of a shorter version. Clinical Gerontologist: The Journal of Aging and Mental Health 1986.
Campbell SE, Seymour DG, Primrose WR. A systematic literature review of factors affecting outcome in older medical patients admitted to hospital. Age Ageing. 2004;33(2):110–5.
Gronewold J, Dahlmann C, Jäger M, Hermann DM. Identification of hospitalized elderly patients at risk for adverse in-hospital outcomes in a university orthopedics and trauma surgery environment. PLoS One. 2017;12(11):e0187801.
Hernandez Torres C, Hsu T. Comprehensive Geriatric Assessment in the Older Adult with Cancer: A Review. European Urology Focus. 2017;3(4):330–9.
Hessen/DEGAM L: Hausärztliche Leitlinie- Geriatrisches Assessment in der Hausarztpraxis. Version 1.02. 2017.
Sutton M, Grimmer-Somers K, Jeffries L. Screening tools to identify hospitalised elderly patients at risk of functional decline: a systematic review. Int J Clin Pract. 2008;62(12):1900–9.
Edmans J, Bradshaw L, Gladman JR, Franklin M, Berdunov V, Elliott R, Conroy SP. The identification of seniors at risk (ISAR) score to predict clinical outcomes and health service costs in older people discharged from UK acute medical units. Age Ageing. 2013;42(6):747–53.
Asomaning N, Loftus C. Identification of seniors at risk (ISAR) screening tool in the emergency department: implementation using the plan-do-study-act model and validation results. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2014;40(4):357–364.e351.
McCusker J, Bellavance F, Cardin S, Belzile E, Verdon J. Prediction of hospital utilization among elderly patients during the 6 months after an emergency department visit. Ann Emerg Med. 2000;36(5):438–45.
Hoogerduijn JG, Schuurmans MJ, Korevaar JC, Buurman BM, de Rooij SE. Identification of older hospitalised patients at risk for functional decline, a study to compare the predictive values of three screening instruments. J Clin Nurs. 2010;19(9–10):1219–25.
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. Jama. 1963;185:914–9.
Bridel JE: Why measure workload? Professional nurse (London, England) 1993, 8(6):362–365.
van Loon IN, Goto NA, Boereboom FTJ, Bots ML, Verhaar MC, Hamaker ME. Frailty screening tools for elderly patients incident to Dialysis. Clinical journal of the American Society of Nephrology : CJASN. 2017;12(9):1480–8.
Decoster L, Van Puyvelde K, Mohile S, Wedding U, Basso U, Colloca G, Rostoft S, Overcash J, Wildiers H, Steer C, et al. Screening tools for multidimensional health problems warranting a geriatric assessment in older cancer patients: an update on SIOG recommendationsdagger. Annals of oncology : official journal of the European Society for Medical Oncology. 2015;26(2):288–300.
Extermann M, Aapro M, Bernabei R, Cohen HJ, Droz JP, Lichtman S, Mor V, Monfardini S, Repetto L, Sorbye L, et al. Use of comprehensive geriatric assessment in older cancer patients: recommendations from the task force on CGA of the International Society of Geriatric Oncology (SIOG). Crit Rev Oncol Hematol. 2005;55(3):241–52.
Acknowledgements
We thank Mrs. Nickel-Gögel for her contribution to CGA. We also thank the nursing staff of the Department of Cardiology and Angiology, Department of Gastroenterology and Hepatology, and Department of Nephrology for conducting ISAR screenings upon hospital admission. We thank Mrs. Lucie Winkler for language editing the paper.
Funding
The authors receive no specific funding for this work.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final version of the manuscript. ACS Data curation, Formal analysis, Methodology, Project administration, Visualization, Writing-original draft. JG Data curation, Formal analysis, Methodology, Project administration, Supervision, Visualization, Writing-original draft. CD Conceptualization Software, Project administration, Writing-review & editing. JS Data curation, Writing-review & editing. HF Conceptualization, Project administration, Writing-review & editing. AK Conceptualization, Project administration, Writing-review & editing. GG Conceptualization, Project administration, Writing-review & editing. TR Conceptualization, Project administration, Writing-review & editing. CK Conceptualization, Writing-review & editing. RD Conceptualization, Project administration, Writing-review & editing. DMH Conceptualization, Investigation, Methodology, Project administration, Supervision, Writing-original draft.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethics committee of the University Duisburg-Essen, need for consent was waived and the study was performed in accordance to the Declaration of Helsinki.
Consent for publication
Since there are no details on individuals reported within the manuscript consent for publication was waived.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Scharf, AC., Gronewold, J., Dahlmann, C. et al. Health outcome of older hospitalized patients in internal medicine environments evaluated by Identification of Seniors at Risk (ISAR) screening and geriatric assessment. BMC Geriatr 19, 221 (2019). https://doi.org/10.1186/s12877-019-1239-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-019-1239-3