Abstract
Objective
The aim of this study was to understand the prevalence and potential risk factors of Helicobacter pylori (H. pylori) infection in Hainan Province, China.
Methods
We conducted this study in 21 health service stations in 5 cities of Hainan Province from August 2022 to April 2023. We selected the various participants based on a stratified whole-group sampling method. The 14C-UBT was used to analyze H. pylori infection in 3632 participants. We also analyzed the possible relationship between variables and H. pylori infection based on chi-square test and multifactorial logistic regression. The model was evaluated by performing a Hosmer–Lemeshow goodness-of-fit test and plotting receiver operating characteristic(ROC) curves.
Results
In total, the results of 3632 eligible participants (age: 14 to 93 years) were included in the analysis. The total prevalence of H. pylori infection in Hainan Province was approximately 38.7%. The prevalence of H. pylori infection was found to increase with age, stabilized in the age group of 45 to 64 years, but peaked in the age group of 65 years and older. In multifactorial analysis, the prevalence of H. pylori infection was positively associated with middle-aged adults (45–64 years), older adults (≥ 65 years), drinking, farmers, natural labor, routinely share utensils, have habit of frequent betel nut consumption, upper gastrointestinal symptoms, and family history of gastric cancer. The factors negatively associated with prevalence included family size ≤ 3, washing hands often before meals, frequent exercise, regular meals, and frequent consumption of fruits and vegetables. In addition, the Hosmer–Lemeshow test showed a good fit (χ2 = 12.983, P = 0.112) and the area under ROC was 0.631 (95%CI: 0.613 ~ 0.649).
Conclusion
The prevalence of H. pylori infection in Hainan Province was observed to be moderate and closely related to age, local socioeconomic conditions, hygienic status and dietary habits.
Similar content being viewed by others
Introduction
Helicobacter pylori (H. pylori) is a Gram-negative bacillus, hat primarily colonizes in the gastric epithelium and was first discovered in 1983 by Marshall and Warren, for which they were awarded the Nobel Prize in Medicine [1]. H. pylori has been identified as a major cause of gastritis, peptic ulcers, as well as gastric cancer, and is the only bacterium classified as a class I carcinogen by the International Agency for Research on Cancer (IARC) [2, 3]. In addition, it has also been closely associated with several extra-gastrointestinal diseases [4].
H. pylori infects approximately half of the global population, but the prevalence varies widely between different countries and regions [5]. Although the prevalence is decreasing rapidly in most developed countries, it remains significantly high in most developing countries [6]. Epidemiological studies have revealed that the prevalence of H. pylori infection in China ranges from 28%-82% [5], and its overall prevalence is approximately 44.2% [7]. Accumulating evidences have suggested that different factors such as gender, age, occupation, education, socioeconomic status, diet, lifestyle, and number of family members can influence the prevalence of H. pylori in the population [8,9,10]. Age is an important variable that has been the focus of most published studies, but the age group associated with the highest prevalence has not yet reached a consensus. Additionally, some studies have reported that H. pylori infection can be acquired mainly in early childhood [11,12,13], whereas others have shown that the prevalence of infection increases significantly with age [14,15,16]. However, the potential correlation between these factors and H. pylori infection is inconclusive.
The relevant data on the prevalence of H. pylori in the southern coastal provinces of china are still lacking. Therefore, our aim was to determine the prevalence of H. pylori infection in Hainan Province and to assess the different risk factors associated with H. pylori infection based on the data collected from various regions of Hainan Province.
Materials and methods
Study population and design
We conducted this study from August 2022 to April 2023 in Hainan Province, China, which included 21 different health service stations from 5 cities (Haikou, Sanya, Qionghai, Dongfang, and Wuzhishan). Inclusion criteria: (1) each participant included in this study was 14 years old and above who were able to complete 14C-UBT and questionnaire; (2) each participant is a native of Hainan or has at least 10 years of residence history. Exclusion criteria included treatment for H. pylori within the past 3 months, antibiotic use within 1 month, and use of proton pump inhibitors and bismuth agents within 2 weeks. In addition, other exclusion criteria taken into consideration were severe cardiac, hepatic or renal insufficiency and contraindications to 14C-UBT. The objectives of this study were explained in detail to all participants, and also, partici-pating in this study was fully conscious and based on their desire. Further, written informed consent was obtained from each participant. Meanwhile, each participant provided a written or electronic informed consent form and the study was approved by the institutional ethics committee of the Second Hospital of Hainan Medical University (reference number: LW20221025).
Questionnaire and definition
The questionnaire from the previous studies in China was referred to and modified accordingly [8,9,10]. The content of the questionnaire mainly included questions related to the demographic characteristics (e.g., age, gender, ethnicity, occupation, marital status, and BMI), socioeconomic status (e.g., education level and annual personal income), hygiene habits (e.g., sharing utensils, absorption before meals, washing hands after the stools, frequency of brushing teeth), lifestyle (e.g., smoking, exercise, work stress, sleep status), dietary habits (eating out, drinking water, alcohol, tea, fruit and vegetable consumption, etc.) and family history of gastric cancer. The data was entered by two different individuals and double-checked to minimize errors. Gastrointestinal symptoms include nausea, vomiting, acid reflux, heartburn, abdominal pain, bloating, constipation and more. Smoking was defined as smoking at least one cigarette per day or having smoked in the past 1 year. Alcohol consumption was defined as consuming at least 100 g of alcohol per week in the past 1 year. "Regular" was defined as at least once a day, and "occasional" was defined as once every 2–3 days or more. Body Mass Index (BMI) is a person’s weight in kilograms (or pounds) divided by the square of height in meters (or feet). Based on BMI, < 18.5 was the low-weight group, ≥ 18.5 and < 24 were the normal weight group, ≥ 24 were overweight group or obese group.
Carbon-14 urea breath test (14C-UBT)
The subjects received 14C breath test in the morning on an empty stomach or fasted for more than 2 h. The test method was strictly in accordance with the instructions. The test was performed by swallowing a 14C urea capsule with an appropriate amount of pure water and then sitting for 15–20 min. It was followed by blowing into the breath card for about 3–5 min, and sampling was completed when the color of the indicator tablet changed from orange to yellow to indicate the presence of H. pylori infection.
Sample size calculation
This study focused on the prevalence of H. pylori infection as the main study index, and the overall prevalence in China is known to be approximately 44.2% based on the previously published literature [7]. Thus, by using the following formula, α = 0.05 (two-sided test) was selected, with an allowable error δ = ± 1.7%, Z_(1-α/2) = 1.96, and p = 44.2%. The calculation yielded the need to include 3279 cases. However, considering the shedding rate of 10%-20%, a total of 3665 cases were included in the study, which can ensure both the accuracy as well as scientific validity of the study results.
Statistical analysis
SPSS 25.0 software was used to analyze the data. The continuous variables were expressed as mean ± standard deviation (SD), and independent sample t-test was used for comparison between the groups. The categorical variables were expressed as frequencies and percentages [n(%)], and comparisons between the groups were made using chi-square tests or trend chi-square tests. All the variables with p < 0.05 in the univariate analysis were included in the multifactorial logistic regression analysis (stepwise regression analysis, SLS = 0.10, SLE = 0.05) to explore the potential relationship between H. pylori infection and risk factors. The results were expressed as the dominance ratio (OR) with a confidence interval (CI) of 95%. The model was evaluated by performing a Hosmer–Lemeshow goodness-of-fit test and plotting receiver operating characteristic (ROC) curves. The differences were considered statistically significant when the P value was less than 0.05.
Result
Demographic characteristics of the investigated population
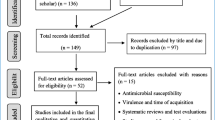
A total of 3665 subjects were initially recruited in this study, some of whom were excluded due to ineligible questionnaires or unwillingness to undergo the 14C urea breath test. Ultimately, 3632 eligible subjects were included in the final analysis. Among these, 1356 (37.3%) were male and 2276 (62.7%) were female, with an age range of 14–93 years and a mean age of 48.0 ± 14.8 years (Fig. 1).
H. pylori infection rate in the Hainan province
The total infection rate of H. pylori in Hainan Province was found to be 38.7% (Fig. 2). The prevalence of infection in each city and county, in descending order, was Wuzhishan (43.9%), Qionghai (42.8%), Dongfang (42.6%), Sanya (38.6%), and Haikou (32.5%) respectively with statistically significant differences (P < 0.001) (Fig. 3). The prevalence of H. pylori infection was observed to increase with age, with the highest rate of H. pylori infection in people over 65 years old (43.4%) and the lowest rate in people under 18 years old (20.7%), with a statistically significant difference (P < 0.001). The prevalence of infection was slightly higher in women (39.9%) in comparison to men (36.8%), but the difference was not statistically significant (P = 0.068) (Table 1).
Association between variables and H. pylori infection
Univariate analysis revealed that H. pylori prevalence was significantly associated with age, occupation, education, same bed, family size, personal monthly income, frequency of sharing utensils with others, brushing, washing hands before meals, washing hands after using the toilet, mode of delivery, family history of gastric cancer, dietary pattern, frequent exercise, alcohol consumption, frequency of eating fruits and vegetables, frequency of eating betel nut, and gastrointestinal symptoms. In addition, other variables were not significantly associated with H. pylori infection (Table 1).
Factors independently associated with H. pylori infection and prediction model
These significant variables were further assessed by including them in a multifactorial logistic regression model, as depicted in Table 2. Middle-aged adults (45–64 years) (odds ratio [OR]:2.154; 95% confidence interval [CI]:1.100–4.218), older adults (≥ 65 years) (OR:2.181, 95% CI:1.097–4.339), farmers (OR:1.266, 95% CI:1.062–1.509), natural labor (OR:3.622, 95% CI:2.544–5.156), frequently share utensils (OR:1.241, 95% CI:1.230–1.685), drinking (OR:1.385, 95% CI: 1.169–1.640), frequent betel nut consumption (OR:1.306, 95% CI:1.005–1.697), upper gastrointestinal symptoms (OR:1.501, 95% CI:1.289–1.747), and family history of gastric cancer (OR: 3.807, 95% CI: 2.666–5.438) were found to be positively associated with H. pylori infection. In addition, the factors negatively associated with prevalence included family size ≤ 3 (OR:0.695, 95% CI:0.594–0.813), washing hands often before meals (OR:0.775, 95% CI:0.638–0.941), frequent exercise (OR:0.565. 95% CI:0.479–0.667), regular meals (OR:0.481, 95% CI:0.384–0.603), and frequent consumption of fruits and vegetables (OR:0.601, 95% CI:0.529–0.752) (Table 2). In addition, the Hosmer–Lemeshow test showed a good fit (χ2 = 12.983, P = 0.112) and the area under ROC was 0.631 (95%CI: 0.613 ~ 0.649) (Fig. 4).
Discussion
This study was the first to investigate the prevalence of H. pylori and its associated risk factors in Hainan Province, China. We used 14C-UBT to detect H. pylori infection in people aged 14 years or older. The results indicated that the overall prevalence of H. pylori infection in Hainan Province was 38.7%, which was significantly lower than the overall prevalence of 44.2% in China (95% CI: 43.0–45.5%) and in line with the global trend of a continuous decrease in H. pylori infection in recent years [6, 7]. This is inextricably linked to China's high economic growth, high level of universal health coverage, and improved public health conditions [17]. However, we also noted that only 9.7% (355/3632) of the population had previously received H. pylori screening and eradication treatment. This observation suggests that good scientific knowledge of H. pylori can potentially help to improve the awareness of H. pylori and alleviate the existing situation of H. pylori infection.
The prevalence of H. pylori infection was found to increase sharply with age but plateaus in the middle-aged and older age groups above 45 years. This result was similar to several large-scale epidemiological surveys in China [9, 10]. There could be two possible reasons to explain these findings. On the one hand, the rapid economic and health development in China in the last two decades has resulted in relatively few risk factors associated with H. pylori exposure in young people, which has markedly reduced the risk of infection. On the other hand, middle-aged and elderly people have a relatively less stable gastric environment as well as weaker organism resistance, and all of these factors can favor the colonization of H. pylori. However, there is no conclusive evidence regarding the possible relationship between gender and H. pylori infection. For instance, in one study Moshkowitz et al. suggested that H. pylori were more likely to colonize the gastric mucosa in women [18], but our study did not find a significant correlation between the gender and H. pylori infection, and this finding was in agreement with conclusions of several previous studies [8, 9].
Occupation is an important factor influencing H. pylori infection, which was consistent with the results of previous studies [8,9,10,11,12,13,14,15,16,17,18,19]. It is generally believed that occupational groups working in agriculture have a relatively higher risk of H. pylori infection, and multiple reasons may be involved to explain this finding. First, farmers generally have a low level of education and often have poor hygiene habits and lifestyles; and second these individuals often have a low socioeconomic status as well as limited access to medical resources for H. pylori screening and eradication treatment. Moreover, we found regional differences in the prevalence of H. pylori infection in Hainan Province, with economically developed areas (e.g., Haikou City) having significantly higher rates of H. pylori infection in comparison to economically backward areas (e.g.,Wuzhishan City). This observation also indirectly indicated that socioeconomic status was closely related to H. pylori infection.
It is now recognized that oral-oral, fecal–oral is the main transmission route of H. pylori [20]. In China, sharing of meals is an important food culture, but this can effectively increase the risk of H. pylori transmission and infection [14]. This was confirmed in the present study as it was found that people who share tableware are more likely to be infected with H. pylori. In addition, poor hygiene practices can substantially increase the risk of H. pylori transmission and serve as an important factor influencing H. pylori infection [21]. In our study, frequent premeal hand washing was identified as independent protective factors for H. pylori infection. Therefore, introduction of meal sharing and the promotion of personal hygiene as well as health awareness could be useful public health measures for the prevention of H. pylori infection.
A good lifestyle seems to be effective in reducing the risk of H. pylori infection and gastric cancer development [22]. We found that the prevalence of H. pylori infection was significantly lower in participants who participated in regular exercise, had regular meals and maintained a regular diet of fruits and vegetables compared to other populations who did not had such healthy habits, and they were also independent protective factors for H. pylori infection. The possible reasons could be as following (i) the presence of chemicals such as isothiocyanate radicicicin and mustard oleoresin in fruits and vegetables can effectively inhibit the colonization of H. pylori and thereby reduce the inflammatory response of the gastric mucosa [23]. (ii) Regular exercise can enhance the body's immunity and regular diet can contribute to the stability of the gastric environment, all of which can significantly reduce the risk of H. pylori colonization. In our study, regular betel nut as well as alcohol consumption were associated with increased odds of H. pylori infection. The practice of washing the raw leaves of betel vine and betel nut (used in the preparation of betel nut liquid) in unclean water may explain our findings [24]. We also found that alcohol consumption is an independent risk factor for H. pylori infection. It is well established that home-brewing is more common in Hainan Province, but the production process is crude and the relevant indicators remain untested. A number of previous studies have reported that alcohol consumption has a protective effect or is not associated with H. pylori infection, probably due to increased gastric acid secretion and promotion of gastric emptying after alcohol intake, as alcohol has a powerful and direct antibacterial activity, thus potentially inhibiting the growth of H. pylori in the stomach. In addition, alcohol can promote gastric emptying and reduce the contact time between H. pylori and the gastric mucosa, which in turn can attenuate the rate of H. pylori infection [25, 26]. In particular, red wine was found to prevent H. pylori-induced gastritis in a mouse model [27]. Another study [28] reported alcohol as a significant risk factor for H. pylori infection because alcohol can directly damage the gastric mucosal layer, thus weakening the gastric mucosal defense barrier. Thus, alcohol could theoretically provide a pathway for H. pylori infection, while heavy alcohol consumption may predispose consumers to different social contacts that favor the transmission of H. pylori infection. Therefore, the potential relationship between alcohol consumption and H. pylori infection still requires further longitudinal and epidemiological studies for further explanation.
H. pylori infection serves as an important influencing factor in the development of gastric cancer. For instance, a large cohort study found that the incidence of gastric cancer increased each year with the duration of H. pylori infection [29]. In addition, the risk of gastric cancer as well as the risk of death decreased significantly after H. pylori eradication [30]. Similar to a previous study, we found that a family history of gastric cancer can serve as an independent risk factor for H. pylori infection [31]. Upper gastrointestinal symptoms were identified as one of the important risk factors for H. pylori infection in this study. However, asymptomatic infection is an important feature of most H. pylori-infected patients, who often have developed severe upper GI disease by the time they seek medical attention. Therefore, one should consider upper GI symptoms (e.g., nausea, acid reflux) as an early warning sign of H. pylori infection, which can be an important step for the timely diagnosis and treatment of H. pylori.
The strengths of this study include the fact that this was the first large-scale epidemiological investigation of H. pylori in Hainan Province, China. In addition, the method employed to detect H. pylori infection was highly accurate and specific. Of course, the study has some limitations. First, cross-sectional studies do not accurately reflect the temporal trends in H. pylori infection. Second, outcome and exposure were assessed simultaneously, which does not allow for a temporal relationship to be established. Finally, the age of our subjects was limited to those aged 14 years or older, thus failing to cover the entire age range in Hainan Province.
In conclusion, the prevalence of H. pylori infection in Hainan Province was significantly lower than the overall prevalence in China and closely related to age, local socioeconomic conditions, hygienic status and dietary habits.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- H. pylori :
-
Helicobacter pylori
- 14C-UBT:
-
Carbon-14 urea breath test
- SD:
-
Standard deviation
- CI:
-
Confidence interval
- ORs:
-
Odds ratios
References
Warren JR, Marshall B. Unidentified curved bacilli on gastric epithelium in active chronic gastritis. Lancet. 1983;1(8336):1273–5.
Malfertheiner P, Megraud F, Rokkas T, et al. Management of Helicobacter pylori infection: the Maastricht VI/Florence consensus report. Gut. 2022;66(1):6–30.
De Martel C, Georges D, Bray F, et al. Global burden of cancer attributable to infections in 2018: a worldwide incidence analysis. Lancet Glob Health. 2020;8(2):e180–90.
Franceschi F, Covino M, Roubaud BC. Review: Helicobacter pylori and extragastric diseases. Helicobacter. 2019;24(Suppl 1):e12636.
Li Y, Choi H, Leung K, et al. Global prevalence of Helicobacter pylori infection between 1980 and 2022: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2023;8(6):553–64.
Hooi JKY, Lai WY, Ng WK, et al. Global Prevalence of Helicobacter pylori Infection: systematic review and meta-analysis. Gastroenterology. 2017;153(2):420–9.
Ren S, Cai P, Liu Y, et al. Prevalence of Helicobacter pylori infection in China: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2022;37(3):464–70.
Zhang F, Pu K, Wu Z, et al. Prevalence and associated risk factors of Helicobacter pylori infection in the Wuwei cohort of north-western China. Trop Med Int Health. 2021;26(3):290–300.
Wang X, Shu X, Li Q, et al. Prevalence and risk factors of Helicobacter pylori infection in Wuwei, a high-risk area for gastric cancer in northwest China: An all-ages population-based cross-sectional study. Helicobacter. 2021;26(4):e12810.
Zhou XZ, Lyu NH, Zhu HY, et al. Large-scale, national, family-based epidemiological study on Helicobacter pylori infection in China: the time to change practice for related disease prevention. Gut. 2023;72(5):855–69.
O’Ryan ML, Rabello M, Cortés H, et al. Dynamics of Helicobacter pylori detection in stools during the first 5 years of life in Chile, a rapidly developing country. Pediatr Infect Dis J. 2013;32(2):99–103.
Mitchell HM, Li YY, Hu PJ, et al. Epidemiology of Helicobacter pylori in southern China: identification of early childhood as the critical period for acquisition. J Infect Dis. 1992;166(1):149–53.
Muhsen K, Jurban M, Goren S, et al. Incidence, age of acquisition and risk factors of Helicobacter pylori infection among Israeli Arab infants. J Trop Pediatr. 2012;58(3):208–13.
Ding Z, Zhao S, Gong S, et al. Prevalence and risk factors of Helicobacter pylori infection in asymptomatic Chinese children: a prospective, cross-sectional, population-based study. Aliment Pharmacol Ther. 2015;42(8):1019–26.
Hasosah M, Satti M, Shehzad A, et al. Prevalence and risk factors of Helicobacter pylori infection in Saudi children: a three-year prospective controlled study. Helicobacter. 2015;20:56–63.
Sykora J, Siala K, Varvarovska J, et al. Epidemiology of Helicobacter pylori infection in asymptomatic children: a prospective populationbased study from the Czech Republic. Application of a monoclonalbased antigen-in-stool enzyme immunoassay. Helicobacter. 2009;14:286–97.
Ren Y, Zhou Z, Cao D, et al. Did the Integrated Urban and Rural Resident Basic Medical Insurance Improve Benefit Equity in China? Value Health. 2022;25(9):1548–58.
Moshkowitz M, Horowitz N, Beit-Or A, et al. Gender-associated differences in urea breath test for Helicobacter pylori infection referrals and results among dyspeptic patients. World J Gastrointest Pathophysiol. 2012;3(3):80–4.
Den Hollander WJ, Holster IL, Den Hoed CM, et al. Ethnicity is a strong predictor for Helicobacter pylori infection in young women in a multi-ethnic European city. J Gastroenterol Hepatol. 2013;28(11):1705–11.
Duan M, Li Y, Liu J, et al. Transmission routes and patterns of helicobacter pylori. Helicobacter. 2023;28(1):e12945.
Nouraie M, Latifi-Navid S, Rezvan H, et al. Childhood hygienic practice and family education status determine the prevalence of Helicobacter pylori infection in Iran. Helicobacter. 2009;14(1):40–6.
Wang XQ, Yan H, Terry PD, et al. Interaction between dietary factors and Helicobacter pylori infection in noncardia gastric cancer: a population-based case-control study in China. J Am Coll Nutr. 2012;31(5):375–84.
Wang T, Cai H, Sasazuki S, et al. Fruit and vegetable consumption, Helicobacter pylori antibodies, and gastric cancer risk: A pooled analysis of prospective studies in China, Japan, and Korea. Int J Cancer. 2017;140(3):591–9.
Abebaw W, Kibret M, Abera B. Prevalence and risk factors of H. pylori from dyspeptic patients in northwest Ethiopia: a hospital based cross-sectional study. Asian Pac J Cancer Prev. 2014;15(11):4459–63.
Murray LJ, Lane AJ, Harvey IM, et al. Inverse relationship between alcohol consumption and active helicobacter pylori infection: the Bristol helicobacter project. Am J Gastroenterol. 2002;97:2750–5.
Mark Woodward CM, McColl K. An investigation into factors associated with Helicobacter pylori infection. J Clin Epidemiol. 2000;53:175–81.
Ruggiero P, Rossi G, Tombola F, et al. Red wine and green tea reduce H pylori- or VacA-induced gastritis in a mouse model. World J Gastroenterol. 2007;13:349–54.
Zhang L, Eslick GD, Xia HH, et al. Relationship between alcohol consumption and active helicobacter pylori infection. Alcohol. 2010;45(1):89–94.
Kumar S, Metz DC, Ellenberg S, et al. Risk factors and incidence of gastric cancer after detection of helicobacter pylori infection: a large cohort study. Gastroenterology. 2020;158(3):527-536.e7.
Ford AC, Yuan Y, Forman D, et al. Helicobacter pylori eradication for the prevention of gastric neoplasia. Cochrane Database Syst Rev. 2020;7(7):CD005583.
El-Omar EM, Oien K, Murray LS, et al. Increased prevalence of precancerous changes in relatives of gastric cancer patients: critical role of H. pylori. Gastroenterology. 2000;118(1):22–30.
Acknowledgements
Not applicable.
Funding
This work was supported by Hainan Province Clinical Medical Center (No. 2021818), The specific research fund of The Innovation Platform for Academicians of Hainan Province (YSPTZX202313), Hainan Provincial Health Industry Research Project(22A200078) and Hainan Provincial Postgraduate Innovation Research Project (Qhyb2022-133).
Author information
Authors and Affiliations
Contributions
R.X.C and F.H.B participated in the design of this study and performed the statistical analysis. R.X.C, D.Y.Z and F.H.B drafted the manuscript. X.D.Z and S.J.C recruited participants. X.D.Z, S.J.C, S.M.H, C.C, D.L, F.Z, J.J.C, C.Y.M, L.G, J.T.Z, J.X.X and Z.C participated in the data collection. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol was approved by the institutional ethics committee of the Second Hospital of Hainan Medical University (LW20221025) and performed per Helsinki's Declaration. All participants provided written informed consent for data collection and storage.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, Rx., Zhang, Dy., Zhang, X. et al. A survey on Helicobacter pylori infection rate in Hainan Province and analysis of related risk factors. BMC Gastroenterol 23, 338 (2023). https://doi.org/10.1186/s12876-023-02973-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-023-02973-3