Abstract
Background & Aims
Although non-alcoholic fatty liver disease (NAFLD) remains an uncommon indication for liver transplantation (LT) in the Chinese, the prevalence of NAFLD is increasing. We aimed to determine the prevalence of de novo steatosis and metabolic dysfunction-associated fatty liver disease (MAFLD) after LT.
Methods
Transient elastography assessment for liver stiffness and controlled attenuation parameter (CAP) were performed after LT in 549 patients at median time of 77 months from LT. CAP was compared with implant liver biopsy, and also validated in 42 patients with post-LT liver biopsy. Longitudinal history including diabetes mellitus (DM), dyslipidemia, hypertension, and immunosuppressive regimen were recorded.
Results
The optimal cut-off level of CAP for diagnosing at least mild (≥ S1) and moderate-to-severe steatosis (≥ S2/3) was 266 and 293 dB/m respectively, with AUROC of 0.740 and 0.954 respectively. Using this newly derived cut-off, 28.9% patients have de novo NAFLD, of which 95.6% fulfilled the criteria for MAFLD. After multivariate analysis, BMI (HR 1.34), DM (HR 2.01), hypertension (HR 2.03), HDL-cholesterol (HR 0.25), LDL-cholesterol (HR 1.5) and cryptogenic cirrhosis (HR 4.85) were associated with the development of S2/3 graft steatosis. de novo NAFLD was associated with higher incidence of new-onset hypertension (p < 0.001), graft dysfunction (defined as ALT > 40 U/L; p = 0.008), but not associated with graft fibrosis (defined as liver stiffness > 12 kPa; p = 0.761).
Conclusion
Although NAFLD remains an uncommon primary liver disease indication for LT in Chinese patients, post-transplant de novo graft steatosis is common and the majority is classified as MAFLD. Development of graft steatosis is not associated with an increase in graft fibrosis but was associated with worse metabolic control and graft dysfunction. Routine CAP measurement to detect de novo graft steatosis should be considered after LT regardless of the primary indication of LT.
Similar content being viewed by others
Introduction
Survival after liver transplant (LT) has improved significantly with the availability of potent antiviral therapies and effective immunosuppressive regimens, with an expected 10-year survival of over 80% [1]. Non-liver conditions such as metabolic syndrome, including diabetes mellitus (DM), hypertension, and dyslipidemia, have become important contributors to post-transplant morbidity and mortality. Risk factors for post-transplant metabolic syndrome include immunosuppression, which may favor the development of hyperglycemia, dyslipidemia, and hypertension [2]. Moreover, there is often increase in body weight after surgery, with obesity developing in approximately a third of patients within a few years after transplant [3, 4]. It is therefore not surprising that metabolic syndrome is common after LT, with reported rates of up to 50–60% [5].
The presence of metabolic syndrome has been implicated in the development of recurrent or de novo graft non-alcoholic fatty liver disease (NAFLD) [6, 7]. NAFLD after LT may contribute to liver enzyme derangements, leading to graft dysfunction and fibrosis. Previous studies have reported a post-transplant NAFLD recurrence rate ranging from 20 to 40% [8, 9]. This wide variation is largely due to the different diagnostic methods, with most studies relying on retrospective reviews of liver biopsies. As screening all patients using liver biopsy would not be feasible, the true prevalence of graft NAFLD after LT remains unclear. Transient elastography with controlled attenuation parameter (CAP) has been shown to be a rapid, reliable, and repeatable non-invasive method for assessment of liver steatosis with high patient acceptance [10]. Previous studies have shown a strong correlation between CAP and fat accumulation in the liver in a variety of chronic liver diseases [11]. Although CAP has been studied for the assessment of donor steatosis in living donor (LD)LT [12, 13], there is very limited data in liver transplant recipients [14]. By using a non-invasive technique, it is now feasible to screen a large population of liver transplant recipients for the presence of graft steatosis and fibrosis.
Recently, the term ‘metabolic dysfunction-associated fatty liver disease’ (MAFLD) is advocated for patients with excess hepatic steatosis associated with overweight/obesity, presence of metabolic dysregulation, and type 2 DM [15]. MAFLD denotes individuals who are metabolically unhealthy and are at risk of advanced liver disease and cardiovascular complications. In this study, we aimed to validate the use of CAP measurement in post-transplant graft steatosis, and determine the prevalence of de novo graft steatosis and MAFLD after LT in a large cohort of post-transplant Chinese patients.
Patients and methods
Consecutive patients with age 18 years or over undergoing LT from January 2003 to December 2014 at The Liver Transplant Center, Queen Mary Hospital, Hong Kong, were eligible for inclusion in this study (detailed inclusion/ exclusion criteria are shown in the Supplementary appendix). No organs from executed prisoners were used. Patient records were reviewed in detail. The diagnosis of DM, hypertension, and dyslipidemia was established by the use of anti-diabetic agents, anti-hypertensives, and lipid-lowering agents respectively for at least 3 months. The diagnosis was confirmed by review of the clinical notes of all patients. The time of onset of these conditions was estimated by the starting date of the respective medications. Body mass index (BMI) was recorded at the time of LT and time of transient elastography. The diagnosis of MAFLD follows the positive diagnostic criteria in the expert consensus statement, which identify subjects with excess hepatic steatosis to have MAFLD if they have also one of the following 3 criteria: (1) overweight or obese (BMI ≥ 23 kg/m2 in Asians), (2) for those with normal BMI: presence of ≥ 2 metabolic risk factors [waist circumference ≥ 90/80 cm in Asian men and women, elevated blood pressure ≥ 130/85, raised plasma triglyceride ≥ 1.7 mmol/L or on treatment, reduced high-density lipoprotein (HDL) cholesterol < 1.0 or 1.3 mmol/L for men or women or on treatment, presence of prediabetes, homeostasis model assessment of insulin resistance score ≥ 2.5, or raised plasma high-sensitivity C-reactive protein > 2 mg/L], or (3) presence of type 2 DM [15]. The present study was approved by the Institutional Review Board/ Ethics Committee of the University of Hong Kong and the Hong Kong West Cluster of Hospital Authority. Written informed consent was obtained from all study subjects prior to any study-related procedures.
Immunosuppression
All patients received basiliximab as induction therapy, and maintained on long term tacrolimus. A tacrolimus concentration of 8–10 ng/ml was targeted for in the initial 3 months with or without mycophenolate mofetil, followed by 5 to 8 ng/mL thereafter. Additional or alternative immunosuppression including cyclosporine, sirolimus, everolimus, and corticosteroid was used for patients who required additional immunosuppression, or were unable to tolerate tacrolimus at the desired dosage.
Transient elastography examination
All patients routinely underwent liver stiffness measurement (LSM) and CAP score determination using Fibroscan (Echosens, Paris, France) at various time points after LT. This procedure has been well described previously [16]. All patients were fasted for at least 8 h prior to the procedure. Standard quality criteria were applied for transient elastography. The scan was considered valid only if 10 valid scans were obtained with an interquartile range (IQR) to LSM ratio of < 0.30. The median liver stiffness (LS) of the valid scans was used as the representative value, measured in kilopascals (kPa). CAP was only considered valid with an IQR of < 40 dB/m [17].
Liver biopsies
Liver biopsy was routinely performed at the time of transplantation for all recipients. Liver steatosis was defined as minimal (< 5%), mild (5–33%), moderate (34–66%), and severe (≥ 67%) on microscopic examination. Routine protocol biopsies were not performed during follow-up, and therefore post-LT biopsies were performed only when clinically indicated to determine the cause of underlying graft dysfunction.
Statistical analyses
All statistical analyses were performed using SPSS version 23.0 (IBM Corp., Armonk, NY). Chi-squared test was used for categorical variables. Continuous variables were presented as median values and IQR shown in brackets, after confirming non-normal distribution by Kolmogorov Smirnov test (Supplementary appendix). Those variables with skewed distribution were analyzed using Mann-Whitney test. Those with three or more variables were analyzed using the Kruskal-Wallis test. Comparison of two variables with calculation of correlation co-efficient was performed using Pearson method. The Kaplan-Meier method was used to calculate the cumulative incidence of new onset metabolic disorders. The area under receiver operating characteristic (AUROC) curve was used to derive the optimal cut-off of CAP score in predicting ≥ S1, ≥S2, and S3 steatosis using the highest calculated Youden index. Multivariate analysis using binary logistic regression was adopted to determine independent factors associated to S2/3 steatosis. A two-sided P-value of < 0.05 was considered statistically significant.
Results
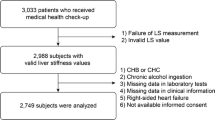
A total of 879 patients underwent LT from January 2003 to December 2014. Of these, 100 patients were transplanted before the age of 18 years, and were excluded. Of the remaining 779 patients, 571 had transient elastography performed. The remaining 208 patients did not have liver stiffness or CAP measurement because of death, re-transplantation, suboptimal medical conditions, or were lost to follow up (Fig. 1). Twenty-two had invalid scans, resulting in 549 patients with valid measurements (Table 1). The median scan age was 59 (range, 23–78) years, with a median scan time from LT of 77 (range, 6–166) months.
Prevalence of metabolic factors
At the time of LT, 114 (14.6%), 71 (9.1%), and 17 (2.2%) had established DM, hypertension, and dyslipidemia respectively. After LT, 192 patients developed new onset DM, with cumulative rate of 17.9%, 24.0%, 32.3%, and 38.4% at 1, 5, 10, and 15 years respectively, 389 patients had new onset hypertension, with cumulative rate of 23.8%, 44.4%, 65.3%, and 72.5% at 1, 5, 10, and 15 years respectively, and 164 patients developed new onset dyslipidemia, with cumulative rate of 2.5%, 14.4%, 24.7%, and 36.6% at 1, 5, 10, and 15 years respectively.
Correlation of CAP score with implantation biopsy
Of the 549 patients with valid transient elastography performed, 422 (76.9%) had < 5% steatosis, 101 (18.4%) had 5–33% steatosis, 18 (3.3%) had 33–66% steatosis, and 8 (1.4%) had > 66% steatosis from the liver biopsy taken at the time of implantation. There was no significant difference in post-transplant CAP scores when correlating with the degree of graft steatosis at the time of transplant. For patients with < 5%, 5–33%, 33–66%, and > 66% steatosis at implant biopsy, the median CAP scores were 225 (range, 114–400), 229 (range, 121–400), 207 (range, 136–305), and 217 (range, 133–318) dB/m respectively (p = 0.935) (Fig. 2A).
Correlation of CAP with liver biopsy after liver transplantation
Liver biopsies performed within a year of valid CAP measurements were available for 42 patients. Of these, 22 (52.4%) had minimal (< 5%) steatosis, 14 (33.3%) had mild (5–33%) steatosis, 2 (4.8%) had moderate (34–66%) steatosis, and 4 (9.5%) had severe (≥ 67%) steatosis. A significantly higher CAP score was observed for higher grades of steatosis, from 200, 254, 318, and 324 dB/m for minimal, mild, moderate, and severe steatosis respectively (p = 0.003) (Fig. 2B). Given the small numbers of those with moderate and severe steatosis, these were grouped together for analysis. The AUROC for diagnosing at least mild, moderate, and severe steatosis using CAP measurement was 0.740, 0.954, and 0.951 respectively (Supplementary Table 1), with an optimal cut-off of 266, 293, and 301 dB/m respectively (Supplementary Fig. 1A, B and C).
Prevalence and risk factors for moderate-severe steatosis and MAFLD
Using the optimal CAP score cut-offs as derived, the prevalence of at least mild (≥ S1), moderate (≥ S2), and severe steatosis (S3) was 28.9%, 17.1%, and 14.0% respectively in the 549 patients with CAP measurements. Of the 159 patients with NAFLD, 152 (95.6%) fulfilled the criteria for MAFLD.
A total of 94 patients had moderate-severe (S2/3) steatosis. No difference was observed in the diagnosis of HBV, HCV, or alcoholic liver disease between those with and without S/3 steatosis, with a higher rate of cryptogenic cirrhosis (7.4% vs. 2.0% respectively, p = 0.011). Ninety-three (98.9%) patients had MAFLD, of which 88 (94.6%) had overweight/obesity, 46 (49.5%) had type 2 DM, and 33 (35.5%) had at least 2 metabolic risk abnormalities. Only 1 patient did not fulfil the MAFLD criteria with standalone hypertension, and interestingly, this patient had intermittent alcohol intake post transplantation for hepatitis B-related cirrhosis.
Patients with S2/3 steatosis, when compared to S0/1 steatosis, had higher cumulative rates of DM (54.3% vs. 35.2% respectively, p = 0.001), hypertension (85.1% vs. 60.2% respectively, p < 0.001), and dyslipidemia (39.4% vs. 23.7% respectively, p = 0.002). The incidence of new-onset hypertension was also higher among those with S2/3 steatosis compared to those without (70.2% vs. 48.6%, p < 0.001), while similar incidence rates for new-onset DM and dyslipidaemia were observed (Supplementary Fig. 2). A higher BMI at the time of transplant and at CAP measurement was observed for those with S2/3 steatosis (23.5 kg/m2 vs. 20.7 kg/m2, p < 0.001 and 26.6 kg/m2 vs. 23.1 kg/m2, p < 0.001 respectively). There was an increasing rate of moderate-severe steatosis observed for those with BMI < 18.5, 18.5–22.9, 23.0-24.9, 25-29.9, and ≥ 30 kg/m2 (0%, 3.1%, 10.0%, 36.0%, and 48.6% respectively, p < 0.001, Supplementary Fig. 3).
Patients with S2/3 steatosis, compared to those without, had higher fasting glucose (6.3 vs. 5.4 mmol/L respectively, p < 0.001), low density lipoprotein (LDL)-cholesterol (2.6 vs. 2.2 mmol/L respectively, p < 0.001), triglyceride (1.5 vs. 1.0 mmol/L respectively, p < 0.001), and lower HDL-cholesterol 1.1 vs. 1.3 mmol/L respectively, p < 0.001) at the time of transient elastography. The results are summarized in Supplementary Table 2.
After multivariate analysis, only BMI at the time of CAP measurement (and not at the time of transplant), cryptogenic cirrhosis as a primary liver disease, the presence of DM, hypertension, HDL-cholesterol and LDL-cholesterol levels remained significant factors associated with S2/3 steatosis (Table 2). The degree of donor graft steatosis at the time of implant (i.e. implant biopsy) was also not associated with S2/3 steatosis (Supplementary Table 4).
Steatosis and graft dysfunction
Patients with moderate-severe steatosis, compared to those without, had higher alanine aminotransferase (ALT) (28 vs. 23 U/L respectively, p < 0.001), and a higher rate of graft dysfunction, defined as serum ALT > 40 U/L (25.5% vs. 14.1%, p = 0.008; Supplementary Fig. 2). There was no significant difference between the 2 groups with respect to bilirubin, alkaline phosphatase (ALP), aminotransferase aspartate, and gamma glutamyl transpeptidase (GGT) levels (p = 0.964, p = 0.559, p = 0.461, and p = 0.066 respectively. The higher prevalence of biliary disease/complications and cholestasis observed in post-LT settings may have masked the difference in GGT levels. By excluding patients with elevated ALP, a significantly higher GGT level was able to be observed for those with S2/3 steatosis (39 vs. 28 IU/L, p = 0.003). Using the local laboratory cut offs of 58 and 45 U/L for males and females respectively, 16 patients (all with MAFLD) had elevated ALT at the time of CAP measurement, with a median level of 62 U/L (range, 57–143). Seven patients had liver biopsies within 1 year, all with steatosis and 3 with evidence of steatohepatitis.
Steatosis and graft fibrosis
There was no significant correlation between CAP and liver stiffness scores (p = 0.886), and no significant difference in the median liver stiffness between those with S2/3 and S0/1 steatosis (5.4 kPa vs. 4.9 kPa, p = 0.091). Of the 94 patients with moderate-severe steatosis, 4 (4.3%) had liver stiffness ≥ 12 kPa, compared to 3.5% among those with minimal or mild graft steatosis (p = 0.761; Supplementary Fig. 2). The characteristics of these 4 patients (all with MAFLD) are summarized in Supplementary Table 3. One patient had steatosis with bridging fibrosis with liver stiffness of 14.3 kPa, who was transplanted for acute flare of chronic hepatitis B, remained negative for serum hepatitis B surface antigen (HBsAg) and hepatitis B virus DNA after transplant without any episodes of rejection.
Discussion
Graft steatosis after LT can occur as a recurrence of underlying disease for those transplanted for NASH-related cirrhosis, or as de novo NAFLD. As protocol liver biopsies are no longer routinely performed, large cohort screening for post-transplant steatosis using liver biopsy is not feasible. Although non-invasive assessment of hepatic steatosis using CAP measurement has been validated previously, there is a paucity of data regarding its use in post-transplant graft steatosis. Moreover, it is recently reported that the cut-off value of CAP for hepatic steatosis in the recipients of LT is different from the non-transplanted population (270 dB/m instead of 248 dB/m) [18]. The current study established an optimal cutoff for moderate-severe steatosis of 293 dB/m with an AUROC of 0.954 (100% sensitivity, 89% specificity, 60% positive predictive value and 100% negative predictive value), and this cut-off was used to determine the prevalence of moderate-severe steatosis in the post-transplant cohort.
Although NAFLD is common in Hong Kong [19, 20], NASH is a rare indication for LT, highlighted by the fact that none of the LT recipients in the current study had NAFLD coded as a primary liver indication. However, the prevalence of de novo graft steatosis was common (28.9%), and over 95% of these had MAFLD. Interestingly, graft status and BMI at the time of transplant were not independent factors associated with S2/3 steatosis, whereas BMI at the time of CAP measurement was. This suggests that the development of MAFLD is dependent on the recipient risk factors, and consistent with a previous study of split liver transplantation where recipient factors were shown to be associated with NASH [21]. In another study of 68 patients, 18% developed de novo NAFLD which was associated with weight gain after transplant [22]. In our study, there was significant increase in the median BMI after LT (from 21.3 to 23.9 kg/m2; p < 0.001), which might be able to explain the high rate of de novo NAFLD after LT among patients who were transplanted for non-NAFLD related causes. The exact mechanisms for post-LT weight gain in our population were not clear, which were likely multifactorial (e.g., immunosuppressant use, reversal of frailty, improvement in appetite after stabilization of medical condition).
The BMI was a strong independent risk factor for S2/3 steatosis, which was observed in almost half of the patients with BMI ≥ 30 kg/m2. The presence of metabolic risk abnormalities (such as DM, hypertension, low HDL-cholesterol, overweight/obesity) was associated with de novo S2/3 graft steatosis, highlighting that these are indeed classified as MAFLD according to the recently advocated diagnostic criteria [15]. The current study is the first to report the risk factors and implications of de novo MAFLD in the post-LT population, with almost all patients with S2/3 steatosis fulfilling the MAFLD criteria. de novo moderate to severe MAFLD was associated with new-onset hypertension, graft dysfunction (Supplementary Fig. 2), and worse metabolic blood profiles (Supplementary Table 2). The rarity of NAFLD as a primary liver disease indication together with < 5% of graft biopsy at implantation showing S2/3 steatosis implicates the intercalated and bidirectional effects of metabolic factors in both contributing to new-onset steatosis after LT, which in turn, is associated with worse metabolic control and graft dysfunction.
The finding of cryptogenic cirrhosis being an independent risk factor for S2/3 graft steatosis did support the long-suspected notion that these could potentially have burnt-out NASH. Since the pre-LT characteristics of those with cryptogenic cirrhosis showed no difference in BMI or prevalence of diabetes, hypertension or dyslipidemia when compared to those with known causes, the true prevalence of burnt-out NASH among patients with cryptogenic cirrhosis remains unclear. Other causes may include prior chronic hepatitis B infection with subsequent HBsAg seroclearance, given that half of the cryptogenic patients were positive for hepatitis B core antibody (data not shown).
Despite the presence of S2/3 steatosis, only a small proportion (3.8%) in the current study had liver stiffness ≥ 12 kPa, suggesting that advance fibrosis/cirrhosis remained rare. This is consistent with the findings of a previous retrospective study of 2360 post-transplant biopsies showing that significant steatosis was not associated with a higher fibrosis stage [23]. The lack of fibrosis may be in part due to the insufficient duration from transplant to liver stiffness measurement (despite a median duration of 77 months), as time is required for both steatosis and subsequent fibrosis to development.
There were several limitations in the current study. Firstly, the diagnosis of steatosis in the large cohort was based on CAP score measurement. However, the CAP score has been shown to correlate well with degrees of steatosis, and the optimal cut-off was determined using available liver histology. It would not have been feasible to perform liver biopsies for all patients in such a large cohort. Moreover, although liver biopsy remains the gold standard, it is also subjected to sampling errors, especially when the fat distribution is not homogenous throughout the liver. Nevertheless, we included subjects with clinically-indicated liver biopsies (i.e. persistently abnormal liver biochemistry) within 1 year of valid transient elastography measurement to ensure the validity of correlation with histology. Secondly, the diagnosis of DM, hypertension, and dyslipidemia were based on treatment received, and this may have underestimated the true prevalence of these metabolic conditions. However, it is likely that those with evidence of these conditions would have been started on appropriate treatment, and therefore would not have been missed. Thirdly, CAP was measured at variable duration after LT and not at fixed timepoints. However, the wide range of post-LT duration for up to 121 months allows for the assessment of steatosis over time. Although steatosis was shown to increase in prevalence with longer duration after transplant [23], this was not observed in the current study. Lastly, some of the metabolic risk parameters such as waist circumference, homoeostasis model assessment of insulin resistance, and plasma high-sensitivity C-reactive protein level were not available. However, it is unlikely to have affected the results as > 95% of NAFLD had fulfilled the MAFLD criteria using available parameters.
In conclusion, although NASH remains an uncommon indication for LT in Chinese patients, post-transplant metabolic disorders are common, and associated with the development of MAFLD in over 25% after liver transplantation. Moderate to severe graft steatosis detected by CAP is associated with new-onset hypertension, graft dysfunction, and worse metabolic profile. Routine CAP measurement should be considered in post-LT patients to identify de novo graft steatosis and associated metabolic risk factors, so that closer monitoring and earlier treatment for the metabolic risk factors can be implemented. Long-term follow-up of this cohort will be required to observe whether development of graft steatosis and/or MAFLD is associated with increase in graft fibrosis.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ALT:
-
Alanine aminotransferase
- ALP:
-
Alkaline phosphatase
- AUROC:
-
Area under receiver operating characteristic
- HBsAg:
-
Hepatitis B surface antigen
- BMI:
-
Body mass index
- CAP:
-
Controlled attenuation parameter
- DDLT:
-
Deceased donor liver transplantation
- DM:
-
Diabetes mellitus
- GGT:
-
Gamma glutamyl transpeptidase
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- HDL:
-
High-density lipoprotein
- IQR:
-
Interquartile range
- kPa:
-
Kilopascals
- LDL:
-
Low density lipoprotein
- LDLT:
-
Living donor liver transplantation
- LS:
-
Liver stiffness
- LSM:
-
Liver stiffness measurement
- LT:
-
Liver transplantation
- MAFLD:
-
Metabolic dysfunction-associated fatty liver disease
- NAFLD:
-
Non-alcoholic fatty liver disease
- NASH:
-
Non-alcoholic steatohepatitis
References
Chan SC, Cheung TT, Chan AC, et al. New insights after the first 1000 liver transplantations at the University of Hong Kong. Asian J Surg. 2016;39(4):202–10.
Charco R, Cantarell C, Vargas V, et al. Serum cholesterol changes in long-term survivors of liver transplantation: a comparison between cyclosporine and tacrolimus therapy. Liver Transplantation and Surgery: Official Publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 1999;5(3):204–8.
Richards J, Gunson B, Johnson J, Neuberger J. Weight gain and obesity after liver transplantation. Transpl International: Official J Eur Soc Organ Transplantation. 2005;18(4):461–6.
Anastacio LR, Ferreira LG, de Sena Ribeiro H, Lima AS, Vilela EG. Toulson Davisson Correia MI: body composition and overweight of liver transplant recipients. Transplantation. 2011;92(8):947–51.
Watt KD, Charlton MR. Metabolic syndrome and liver transplantation: a review and guide to management. J Hepatol. 2010;53(1):199–206.
Watt KD, Pedersen RA, Kremers WK, Heimbach JK, Charlton MR. Evolution of causes and risk factors for mortality post-liver transplant: results of the NIDDK long-term follow-up study. Am J Transplantation: Official J Am Soc Transplantation Am Soc Transpl Surg. 2010;10(6):1420–7.
Sprinzl MF, Weinmann A, Lohse N, et al. Metabolic syndrome and its association with fatty liver disease after orthotopic liver transplantation. Transpl International: Official J Eur Soc Organ Transplantation. 2013;26(1):67–74.
Burra P, Germani G. Orthotopic liver transplantation in non-alcoholic fatty liver disease patients. Rev Recent Clin Trials. 2014;9(3):210–6.
Losurdo G, Castellaneta A, Rendina M, Carparelli S, Leandro G, Di Leo A. Systematic review with meta-analysis: de novo non-alcoholic fatty liver disease in liver-transplanted patients. Aliment Pharmacol Ther. 2018;47(6):704–14.
de Ledinghen V, Vergniol J, Foucher J, Merrouche W, le Bail B. Non-invasive diagnosis of liver steatosis using controlled attenuation parameter (CAP) and transient elastography. Liver International: Official Journal of the International Association for the Study of the Liver. 2012;32(6):911–8.
Karlas T, Petroff D, Sasso M et al. Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J Hepatol 2017, 66(5):1022–30.
Hong YM, Yoon KT, Cho M, et al. Clinical usefulness of controlled attenuation parameter to screen hepatic steatosis for potential donor of living donor liver transplant. Eur J Gastroenterol Hepatol. 2017;29(7):805–10.
Mancia C, Loustaud-Ratti V, Carrier P, et al. Controlled attenuation parameter and liver stiffness measurements for Steatosis Assessment in the liver transplant of Brain Dead Donors. Transplantation. 2015;99(8):1619–24.
Karlas T, Kollmeier J, Bohm S, et al. Noninvasive characterization of graft steatosis after liver transplantation. Scand J Gastroenterol. 2015;50(2):224–32.
Eslam M, Newsome PN, Sarin SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73(1):202–9.
Fung J, Lai CL, Fong DY, Yuen JC, Wong DK, Yuen MF. Correlation of liver biochemistry with liver stiffness in chronic hepatitis B and development of a predictive model for liver fibrosis. Liver International: Official Journal of the International Association for the Study of the Liver. 2008;28(10):1408–16.
Wong VW, Petta S, Hiriart JB, et al. Validity criteria for the diagnosis of fatty liver by M probe-based controlled attenuation parameter. J Hepatol. 2017;67(3):577–84.
Siddiqui MS, Idowu MO, Stromberg K, et al. Diagnostic performance of vibration-controlled transient Elastography in Liver Transplant recipients. Clin Gastroenterol Hepatol; 2020.
Wong VW, Chu WC, Wong GL, et al. Prevalence of non-alcoholic fatty liver disease and advanced fibrosis in Hong Kong Chinese: a population study using proton-magnetic resonance spectroscopy and transient elastography. Gut. 2011;61(3):409–15.
Fung J, Lee CK, Chan M, et al. High prevalence of non-alcoholic fatty liver disease in the chinese - results from the Hong Kong liver health census. Liver International: Official Journal of the International Association for the Study of the Liver. 2015;35(2):542–9.
Boga S, Munoz-Abraham AS, Rodriguez-Davalos MI, Emre SH, Jain D, Schilsky ML. Host factors are dominant in the development of post-liver transplant non-alcoholic steatohepatitis. World J Hepatol. 2016;8(15):659–64.
Seo S, Maganti K, Khehra M, et al. De novo nonalcoholic fatty liver disease after liver transplantation. Liver Transplantation: Official Publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2007;13(6):844–7.
Hejlova I, Honsova E, Sticova E, et al. Prevalence and risk factors of steatosis after liver transplantation and patient outcomes. Liver Transplantation: Official Publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2016;22(5):644–55.
Acknowledgements
none.
Funding
This study was not funded by any sources.
Author information
Authors and Affiliations
Contributions
The authors declare they have participated in the preparation of the manuscript and have seen and approved the final version. LYM analyzed data and wrote the paper. ACYC and TCLW collected data. WCD, WHS, KWM, SLS and KWC acquired data and performed the study. WKS, MFY and CML designed the study and provided study concept. JF designed the study, provided study concept, performed the research and critically revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was approved by the Institutional Review Board/ Ethics Committee of the University of Hong Kong and the Hong Kong West Cluster of Hospital Authority. Written informed consent was obtained from all study subjects prior to any study-related procedures. All study procedures were carried out in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Conflict of interest
JF has been a consultant for Gilead Sciences. MFY received speaker fees and received research funding from Bristol-Myers Squibb and Gilead Sciences. WKS received speaker fees from Mylan and is an advisory board member, received speaker fees and research funding from Gilead Sciences. All other authors: none to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table 1
. Accuracy of CAP score in predicting ≥ S1, ≥ S2 and S3 graft steatosis. Supplementary table 2. Patients with and without moderate-severe steatosis. Supplementary table 3. Patients with S2/3 steatosis and liver stiffness measurement ≥ 12kPa. Supplementary Table 4. Relationship between implant biopsy (i.e. at time of LT, performed for all subjects), post-LT biopsy (performed for clinical indication and within 1 year of TE) and CAP-defined graft steatosis. Supplementary Figure 1. Receiver operating characteristic curve of CAP in the prediction of (A) ≥ S1 steatosis (B) ≥ S2/3 steatosis and (C) S3 steatosis. Supplementary Figure 2. Significance of moderate to severe graft steatosis on the rate of new-onset metabolic risk factors, graft dysfunction and graft fibrosis. Graft dysfunction was defined as serum alanine aminotransferase > 40 U/L. Graft fibrosis was defined as liver stiffness > 12 kPa. CAP: controlled attenuation parameter; DM: diabetes mellitus; HTN: hypertension; LP: dyslipidaemia. Supplementary Figure 3. Prevalence of S2/3 steatosis according to BMI after liver transplantation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mak, LY., Chan, A.C., Wong, T.C. et al. High prevalence of de novo metabolic dysfunction-associated fatty liver disease after liver transplantation and the role of controlled attenuation parameter. BMC Gastroenterol 23, 307 (2023). https://doi.org/10.1186/s12876-023-02940-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-023-02940-y