Abstract
Background
Previous studies have confirmed that preoperative nutritional-inflammatory indicators can predict prognosis in various malignancies. However, to the best of our knowledge, no study has investigated the assessment of systemic inflammatory immunity index (SII) combined with prognostic nutritional index (PNI) scores to predict prognosis after neoadjuvant treatment with imatinib in locally advanced gastrointestinal stromal tumours (LA-GIST). The aim of this study was to evaluate the predictive value of pretreatment SII-PNI scores in predicting recurrence after neoadjuvant therapy with imatinib in patients with LA-GIST.
Methods
We retrospectively analyzed 57 patients with LA-GIST who received imatinib neoadjuvant from January 2013 to March 2019. Patients were divided into recurrence and non-recurrence groups according to their follow-up status, and SII and PNI cut-offs were calculated by receiver operating characteristic. The SII-PNI score ranged from 0 to 2 and were categorized into the following: score of 2, high SII (≥ 544.6) and low PNI (≤ 47.2); score of 1, either high SII (≥ 544.6) or low PNI (≤ 47.2); score of 0, no high SII (≥ 544.6) nor low PNI (≤ 47.2).
Results
All patients received imatinib neoadjuvant therapy for a median treatment period of 8.5 months (ranging from 3.2 to 12.6 months), with 8 patients (14.04%) and 49 patients (85.96%) developing recurrence and non-recurrence, respectively. Patients with a high SII-PNI score had a significantly worse recurrence-free survival time than those with a low SII-PNI score (P = 0.022, 0.046), and had a poorer pathological response (P = 0.014). Multivariate analysis demonstrated that the SII-PNI score was an independent prognostic factor for prediction of recurrence-free survival (P = 0.002).
Conclusion
The pre-treatment SII-PNI score can be used to predict the efficacy after neoadjuvant treatment with imatinib in patients with LA-GIST, which may be a promising predictor of recurrence-free survival time for patients.
Similar content being viewed by others
Introduction
Gastrointestinal stromal tumours (GIST) are the most common mesenchymal derived tumours and most patients have mutations in the c-kit or platelet derived growth factor receptor alpha (PDGFRA) gene [1, 2]. Currently, the preferred treatment for GIST patients is surgical resection, with the goals of obtaining R0 margins, avoiding intraoperative tumour rupture and maximising preservation of organ function [3, 4]. Nevertheless, a growing number of studies have found that direct surgical resection is difficult for patients with specific sites (oesophagogastric junction, low rectum, duodenum) and large tumour diameters [5, 6]. Recently, imatinib, a small molecule tyrosine kinase inhibitor (TKI), has been widely used as an adjuvant therapy for GIST patients after surgery as it can inhibit cell growth and promote apoptosis by blocking tyrosine kinase [7, 8]. Several retrospective studies have found that neoadjuvant treatment with preoperative imatinib can be attempted in patients with locally advanced GIST (LA-GIST) [9,10,11]. Meanwhile, a prospective study of 63 patients with LA-GIST (RTOG 0132) found that surgical resection after 8–12 weeks of preoperative neoadjuvant imatinib (600 mg/d) resulted in an R0 resection rate of 77% and a 5-years overall survival rate of 77% [12]. In addition, several multicentre prospective studies have shown the same results, suggesting that preoperative neoadjuvant therapy with imatinib is effective in the treatment of LA-GIST and has a good “down-staging” effect, improving the R0 resection rate, safety of surgery and facilitating the preservation of organ function [13, 14].
Unfortunately, not all patients benefit from those treatments, and some of them develop recurrent metastases within a short period of time after treatment. Currently, the risk of recurrence after neoadjuvant therapy for LA-GIST is assessed by the National Institutes of Health (NIH) (2008 modified version), the Armed Forces Institute of Pathology (AFIP) criteria, primary tumour site, tumour diameter and mitotic index [15]. However, these assessment indicators are considered only from the perspective of the original GIST and ignore the impact of the patient's inflammatory and nutritional status on the tumour during neoadjuvant therapy.
Presently, inflammation plays an important role in the pathogenesis of malignant tumors, and the latest view is that tumor-related inflammation is considered to be the seventh characteristic of tumors [16, 17]. Numerous studies have found that the systemic inflammatory response can disrupt the host's immune response and promote tumour cells to escape from immune surveillance, which further promotes the development of angiogenesis, invasion and metastasis [18, 19]. At the same time, previous studies have found that the nutritional status of the tumour patient is one of the key factors influencing the progression of the tumour [20, 21]. The systemic immune-inflammatory index (SII) is a comprehensive measure of the body's systemic inflammatory and immune status consisting of peripheral blood neutrophils, lymphocytes and platelets [22]. Accumulating evidence has revealed that SII is closely related to the prognosis of various malignant tumors [22,23,24].
Our previous study also found that 10.09% of newly diagnosed GIST patients had malnutrition, and most of them were middle- and high-risk types [25]. Further follow-up found that the nutritional status of patients was also closely related to prognosis. Therefore, we hypothesise that poor nutritional status during neoadjuvant therapy in patients with LA-GIST may also be strongly associated with poor prognosis. The prognostic nutritional index (PNI), as a simple and feasible nutritional assay, formed based on the combination of lymphocyte count and albumin levels, has been shown to be associated with the prognosis of various malignancies and is widely used to assess the prediction of the efficacy of neoadjuvant therapy and the assessment of prognosis in cancer patients [26, 27].
In previous studies we have found that a new scoring system combining SII with PNI in immunotherapy for locally progressive gastric cancer [28] and in conversion therapy for advanced gastric cancer [29] has good diagnostic value in predicting the efficacy and assessing prognosis. However, previous studies have generally used a single haematological index, including SII [30] and PNI [31], and few studies have used SII in combination with PNI to assess the evaluation of efficacy and prediction of prognosis in LA-GIST patients after neoadjuvant therapy with imatinib. Therefore, in this study, we evaluated the predictive value of the pre-treatment SII-PNI score on the efficacy and prognosis of patients with LA-GIST receiving neoadjuvant therapy with imatinib.
Materials and methods
Study design and participants
This study retrospectively analyzed 57 patients with LA-GIST who underwent neoadjuvant imatinib therapy in the Fourth Hospital of Hebei Medical University from January 2013 to March 2019. The following inclusion criteria were applied: (1) all patients had histopathologically confirmed GIST; (2) genetic tests suggested the imatinib treatment was indicated; (3) age between 18 and 75 years; (4) preoperative imaging examination showed that the lesions were locally advanced, and surgery without pre-operation chemotherapy or radiation therapy may have a significant impact on the quality of life, including: the tumor site ≤ 5 cm from the cardia, ≤ 5 cm from anal dentate line, ≤ 5 cm from duodenal papilla, pancreaticoduodenectomy or combined organ resection is required for surgery; tumor diameter ≥ 10 cm; (5) all patients were treated with radical surgery after neoadjuvant treatment with imatinib; (6) complete hospitalization data, including computed tomography (CT) scans and follow-up data before and after neoadjuvant treatment, were available. Patients were excluded if they presented with the following: (1) the presence of concurrent tumors other than LA-GIST; (2) the presence of acute bleeding, perforation, and obstruction requiring emergency surgery; (3) poor functional reserve of organs that cannot tolerate surgery or patient refusal to undergo surgical treatment, or patient inability to cooperate with treatment; (4) the presence of lumbar spine metal implants; (5) concurrent history of other tumours or haematological disorders and (6) pre-operative co-infection and abnormal blood results. This study was tested and approved by the ethics committee of the Fourth Hospital of Hebei Medical University. All patients provided informed consent.
Imatinib neoadjuvant therapy
The decision to administer imatinib neoadjuvant therapy was made by a multidisciplinary panel of surgeons, oncologists, pathologists, and radiologists after all patients were diagnosed with LA-GIST. The initial dose of imatinib was determined based on the results of genetic testing, which resulted in a dose of 400 mg/d for the KIT exon 11 mutation.
According to the National Comprehensive Cancer Network (NCCN) and the Chinese Society of Clinical Oncology (CSCO) guidelines for the treatment of GIST, the recommended duration of pre-operative neoadjuvant imatinib treatment is 6–12 months to maximize the effectiveness of the drug [32, 33]. The optimal timing of surgery was chosen if the either of the two following criteria was met: (1) two consecutive CT scans revealed no regression of the tumor; (2) surgery was considered by the surgeon to be radical and/or organ-preserving. All patients were treated surgically after 1 week of discontinuation of imatinib.
Assessments
During neoadjuvant treatment, abdominal CT examination was performed every 3 months during preoperative treatment and the efficacy was assessed according to the Choi criteria [34]. A complete response (CR) is defined as the disappearance of all lesions and no new lesions after neoadjuvant therapy. In contrast, a partial response (PR) was defined as ≥ 10% reduction in tumour length and/or ≥ 15% reduction in tumour density, with no new lesions and no significant progression of non-measurable lesions. Progressive disease (PD) is defined as an increase in tumour length of ≥ 10% and tumour density that does not meet the criteria for PR, or the presence of a new lesion, or a new intratumoural nodule, or an increase in the size of an existing intratumoural nodule. In contrast, those that do not meet the criteria for CR, PR and PD are defined as stable disease (SD).
The criteria for evaluating the pathological efficacy of LA-GIST patients after neoadjuvant therapy were based on the “Chinese consensus guidelines for diagnosis and management of gastrointestinal stromal tumor” published in 2017 [35], which classified postoperative pathological specimens into mild effect (≤ 10%), low effect (> 10% and < 50%), moderate effect (≥ 50% and ≤ 90%), and high effect (> 90%) according to the percentage of necrotic degeneration areas in the tumor tissues. In this study, the mild and low effects were combined into a low response group, and the moderate and high effects were combined into a high response group.
Definitions and follow-up
Peripheral venous blood samples were collected in fasting state within 1 week before initiation of chemotherapy in all patients. Peripheral neutrophil, lymphocyte and platelet counts were measured and analysed using an automated haematology analyser (Beckman Coulter LH750) and albumin levels were measured and analysed using an automated haematology analyser (Beckman Coulter AU5800), respectively. Referring to the results in our previous studies, in this study PNI was defined as PNI = albumin (g/L) + 5 × total lymphocyte count (109/L) and SII was defined as SII = platelets × neutrophil/lymphocyte count [28, 29].
All patients were recommended to have an enhanced CT scan of the abdomen every 3 months for the first 3 years postoperatively and every 6 months for the 4–5th years. Follow-up methods mainly included telephone encounter, outpatient visits, and hospitalization. In this study, our primary observational endpoint was recurrence-free survival (RFS), defined as the time from the start of neoadjuvant therapy to the date of documented relapse or death from any cause at follow-up, and the follow-up deadline date for this study was January 31, 2022.
Statistical analyses
SPSS version 26.0 and GraphPad Prism 8.01 were utilized to perform statistical analyses. The optimal cut-off values for SII and PNI with the highest Youden index were determined by plotting the receiveroperator characteristic curve (ROC) based on the patient's RFS survival time. Survival analysis was performed using the Kaplan–Meier method. The change values of tumor diameter measured by CT before and after neoadjuvant therapy in LA-GIST patients were plotted by GraphPad Prism 8.01 software to assess the waterfall of CT imaging efficacy for each patient. Univariate and multivariate analyses were investigated by the Cox proportional hazards regression model. The hazard ratio (HR) and 95% confidence interval (CI) were used to assess relative risks. Spearman correlation analysis was used to evaluate the relationship between PNI and SII. P values < 0.05 were considered as statistically significant.
Results
Patients’ demographic information and tumor characteristics
According to the inclusion and exclusion criteria of this study, a total of 57 patients with LA-GIST were included, of whom 38 (66.67%) were male and 19 (33.33%) were female. Patient demographic information and pathological features are shown in Table 1. The mean age of the patients was 57.4 ± 10.7 years (ranging from 30 to 82 years old), of which 45.61% were ≥ 60 years. The mitotic numbers per HPF were 0–5 and ≥ 5 in 8 (14.04%) and 49 (85.96%) patients, respectively. The median SII and PNI before neoadjuvant therapy with imatinib were 369.7 (ranging from 77.5 to 1432.0) and 49.8 (ranging from 35.1 to 60.5), respectively, and there was a strong negative correlation between them (r = − 0.581, P < 0.0001; Fig. 1A). And after neoadjuvant treatment SII and PNI were 321.3 (ranging from 72.6 to 1152.2) and 46.6 (ranging from 35.2 to 55.7) respectively, which also had a moderate negative correlation (r = − 0.371, P = 0.005; Fig. 1B).
Optimal cut-off values of SII and PNI before and after neoadjuvant therapy
At the time of follow-up, eight patients in the group had recurrence, including five with liver metastases, two with abdominal metastases and one with anastomotic recurrence. The mean SII before neoadjuvant treatment was 431.6 ± 306.7 and PNI was 50.9 ± 5.3 in the 49 patients who did not relapse, while after treatment it was 390.0 ± 252.4 and 46.6 ± 4.0, respectively. In addition, for the eight patients who developed recurrence before neoadjuvant treatment the mean SII and PNI were 1059.0 ± 440.1 and 45.8 ± 6.4, respectively, while after treatment the mean SII was 457.9 ± 348.6 and PNI was 45.4 ± 4.4. We observed that SII was significantly higher in patients with recurrence before neoadjuvant treatment (P = 0.0003), but PNI was significantly lower in patients without recurrence (P = 0.016) (Fig. 2A, B). However, this difference between the two groups of patients was not as significant after neoadjuvant therapy for either SII (P = 0.813) or PNI (P = 0.329) (Fig. 2C, D).
To determine the optimal cut-off values for the continuous variables of SII and PNI, we constructed ROC curves and calculated AUC to assess the predictive ability of SII and PNI in terms of differentiating between patients experiencing recurrence and non-recurrence before and after neoadjuvant treatment with imatinib. SII and PNI before neoadjuvant therapy had good discriminatory ability with optimal cut-off values of 544.6 (AUC = 0.885, 95% CI 0.741–1.000, P = 0.001; sensitivity of 0.875 and specificity of 0.796) and 47.2 (AUC = 0.764, 95% CI 0.556–0.972, P = 0.017; sensitivity of 0.776 and specificity of 0.750) (Fig. 3A, B). However, after neoadjuvant treatment SII (AUC = 0.528, 95% CI 0.270–0.786, P = 0.800) and PNI (AUC = 0.611, 95% CI 0.368–0.854, P = 0.318) failed to accurately distinguish between recurrent and non-recurrent patients (Fig. 3C, D). Therefore, all LA-GIST patients were divided into three groups based on the optimal cut-off values for SII and PNI before imatinib neoadjuvant therapy: score 2 (n = 11), high SII (≥ 544.6) and low PNI (≤ 47.2); score 1 (n = 13), high SII (≥ 544.6) or low PNI (≤ 47.2); and score 0 (n = 33), no high SII (≥ 544.6) or low PNI (≤ 47.2).
The relationship between SII-PNI score and neoadjuvant therapy response
All patients received imatinib neoadjuvant therapy for a median treatment period of 8.5 months (ranging from 3.2 to 12.6 months) with no discontinuations during treatment. 57 patients with LA-GIST completed abdominal CT-enhanced scans before and after neoadjuvant therapy and only 4 patients (7.02%) had SD according to the Choi criteria, the remaining patients had PR (Fig. 4). There were no significant differences between the groups with different SII-PNI scores in the evaluation of imaging efficacy (P = 0.233), but changes in pathological response were significantly different between the groups (P = 0.014), with the lower the score, the more pronounced the changes (Table 2).
A waterfall plot of ranked best tumor shrinkage. Dashed lines indicate a 10% increase in tumor diameter from baseline for progression (progressive disease) and 10% for tumor regression (partial response). Of all LA-GIST patients treated with neoadjuvant imatinib, only 4 of 57 (7.02%) showed stable disease, while the remaining 53 patients (92.98%) showed partial responses and none showed disease progression
Relationship between SII-PNI score and prognosis
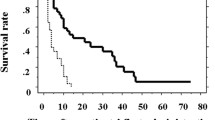
Fifty (87.72%) of the 57 patients with LA-GITS continued postoperative oral imatinib therapy at 400 mg/d, while the remaining 7 (12.28%) patients refused adjuvant therapy with postoperative imatinib. The median duration of oral imatinib in these 50 patients who received adjuvant therapy was 38.9 months (95% CI 15.3–62.4 months). All patients completed follow-up with a median follow-up period of 42.1 months (13.2–64.2 months), with no recurrent metastases in patients in the SII-PNI score group 0, and 2 and 6 recurrent metastases in patients in score groups 1 and 2, respectively. The 3-years recurrence-free survival (RFS) for the whole group was 85.96%, with the 3-years RFS for patients with a SII-PNI score of 0 being 100.00%, compared to 84.62% and 45.45% for patients with a score of 1 and 2 subgroups respectively, with significant differences between the three groups. The comparison of 3 years RFS among patients with different SII-PNI scores was statistically significant (all P < 0.05) (Fig. 5). Cox multivariate analysis showed that tumour response (P = 0.012), the SII-PNI score (P = 0.002), tumour size (P = 0.020) and postoperative imatinib treatment (P = 0.008) were independent risk factors for 3-years RFS (Table 3).
Recurrence-free survival of LA-GIST patients with different SII-PNI scores. A Recurrence-free survival in patients with SII-PNI score of 0; B recurrence-free survival in patients with SII-PNI score of 1; C recurrence-free survival in patients with SII-PNI score of 2; D comparison of non-recurrence survival time of patients with different SII-PNI scores
Discussion
In recent years, with the rapid development of surgical techniques and multimodal therapies such as TKI molecular targeting drugs, the clinical outcomes and quality of life of GIST patients have improved significantly [3]. Nowadays, neoadjuvant treatment with imatinib for patients with LA-GIST has attracted much attention, with the following advantages [33, 35]: firstly, it can reduce the tumor volume and decrease the clinical stage; secondly, it can also reduce the scope of surgery and avoid unnecessary combined organ resection, reducing the risk of surgery and also increasing the chance of radical resection; in addition, it can protect the structure and function of important organs for tumors in specific sites; finally, for patients with large tumor diameter and high risk of intraoperative rupture, neoadjuvant treatment can reduce the possibility of drug-induced dissemination therapy. However, not all patients with LA-GIST benefit from this, with 10–20% of patients experiencing progression after 3 years of treatment [36]. In our cohort, we observed disease progression of 14.04% at 3 years after neoadjuvant imatinib treatment, which is consistent with previous studies [11, 36]. Currently, the common approach to predicting recurrence for LA-GIST is the 2008 revised NIH, AFIP and other guideline consensus, but these are only assessed from the perspective of postoperative pathology and do not take into account the dynamic changes in inflammatory and nutritional status of patients during neoadjuvant therapy [15].
Numerous studies have found that the biological behaviour of malignant tumourigenesis, development and invasion depends not only on the malignant characteristics of the tumour cells, but also on the tumour microenvironment [16, 18]. Inflammatory cells are considered to be an important component of the tumour microenvironment, and their mediated inflammatory response promotes invasion and metastasis by disrupting the immune response and further leading to immune escape of tumour cells [37]. Currently, a growing number of studies have found that inflammatory cells in peripheral blood can migrate through the body circulation to act in local tumour tissues, and therefore systemic inflammatory markers can be used to predict tumour prognosis in the tumour microenvironment in relation to the immune response [38]. The SII has received increasing attention as a more comprehensive measure of the status of the systemic inflammatory response, and several studies have confirmed its value in predicting tumour prognosis and outcome [18, 19, 23]. Besides, the nutritional status of GIST patients has received increasing attention in recent years. Our previous studies have demonstrated that nutritional status of GIST patients is a risk factor affecting the prognosis whether at the initial diagnosis or after surgery [22, 39]. The PNI is an index calculated from serum albumin and peripheral blood lymphocytes that provides a comprehensive reflection of the patient's nutritional status and immune function [26, 27]. To the best of knowledge, this is the first study to demonstrate the prognosis prediction of SII combined with PNI in patients with LA-GIST after neoadjuvant imatinib.
Our study showed that patients who developed recurrence had higher SII and lower PNI than the non-recurrence group at baseline, but this difference was less pronounced after neoadjuvant therapy. Meanwhile, we also found that the SII-PNI score correlated with pathological response after neoadjuvant chemotherapy, with the higher the score at baseline, the worse the pathological response in LA-GIST patients, which was consistent with our previous study [28, 29]. We speculate that the reasons for this outcome may include: firstly, elevated SII prior to neoadjuvant therapy indicates the presence of an inflammatory microenvironment that promotes tumor invasion and metastasis, whereas reduced PNI indicates poorer immune function and nutritional status, further promoting the formation of an inflammatory microenvironment as it was described by Yamanaka et al. [40]. Furthermore, epithelial-mesenchymal transition (EMT) mediated by the local inflammatory microenvironment of the tumor promotes tumor cell escape and resistance to therapeutic agents, which in turn affects the pathological response to neoadjuvant therapy in patients with LA-GIST [41, 42].
In recent years, there has also been increasing interest in the impact of SII and PNI on the prognosis of GIST patients. A retrospective study involving 431 GIST patients found that compared with the low PNI group (PNI < 47.45), the recurrence-free survival (RFS) of the high PNI group (PNI ≥ 47.45) was significantly prolonged (the 5-years RFS rates were 89.9% and 70.8%, respectively, P < 0.001) [31]. Interestingly, Elif Yuce et al. [43] found that PNI was not a risk factor for the prognosis of GIST patients. Furthermore, As Dolan et al. [44] published a retrospective analysis including 160 patients who underwent GIST surgery, the authors demonstrated that SII could be used as a prognostic predictor. Similar results were obtained in another retrospective analysis that included 45 GIST patients [30]. In this study, we also assessed the relationship between SII-PNI scores and neoadjuvant treatment recurrence in patients with LA-GIST. The 3-years RFS for patients with SII-PNI scores of 0 was 100.00% compared to 84.62% and 45.45% for patients with scores of 1 and 2 respectively, with significant differences between the three groups. The possible mechanism of SII-PNI predicting prognosis are as the followings: firstly, elevated neutrophils significantly inhibit lymphokine-activated killer cell-mediated cytotoxic effects, thereby down-regulating the patient's anti-tumor cell immune response and thus promoting tumor cell proliferation and migration [45, 46]; secondly, platelets promote tumour growth by secreting tumour growth factors such as platelet-derived growth factor (PDGF) and vascular endothelial growth factor (VEGF). Platelets can also play an integrative role in the process of tumor cell metastasis, causing tumor cells to evade the host immune system, thus protecting tumor cells from being easily recognized and facilitating tumor cell dissemination [47]; furthermore, lymphocytopenia suggests a decrease in the body's immune function, inducing apoptosis of tumor-specific T cells and inhibiting the activation and proliferation of T cells, further promoting the proliferation and migration of tumor cells [48, 49]; finally, systemic inflammatory responses exacerbate malnutrition and decreased body function in patients with malignancy, promoting poor prognosis in patients with malignancy [40].
It is noteworthy that a few limitations of current research also exist. Firstly, this study was a single-centre retrospective study with a relatively small number of patients included, which may have been subject to selection bias. Secondly, this study only analysed the relationship between SII-PNI scores and recurrence in LA-GIST patients, and not the overall survival time of patients. Therefore, more large-sample, prospective, multicentre studies are needed for validation in order to determine the predictive value of the parameters examined in the study.
Conclusions
In conclusion, our study suggests that systemic inflammation and nutritional status are equally important in the tumourigenesis of LA-GIST cases. This study was the first to show that the SII-PNI score based on peripheral blood counts in LA-GIST patients is a promising predictor of pathological response and recurrence outcome after neoadjuvant therapy. These findings may facilitate the development of treatment strategies and clinical risk stratification.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Søreide K, Sandvik OM, Søreide JA, Giljaca V, Jureckova A, Bulusu VR. Global epidemiology of gastrointestinal stromal tumours (GIST): a systematic review of population-based cohort studies. Cancer Epidemiol. 2016;40:39–46.
Arshad J, Ahmed J, Subhawong T, Trent JC. Progress in determining response to treatment in gastrointestinal stromal tumor. Expert Rev Anticancer Ther. 2020;20(4):279–88.
Maki RG, Blay JY, Demetri GD, Fletcher JA, Joensuu H, Martín-Broto J, Nishida T, Reichardt P, Schöffski P, Trent JC. Key issues in the clinical management of gastrointestinal stromal tumors: an expert discussion. Oncologist. 2015;20(7):823–30. https://doi.org/10.1634/theoncologist.2014-0471.
Nishida T, Yoshinaga S, Takahashi T, Naito Y. Recent progress and challenges in the diagnosis and treatment of gastrointestinal stromal tumors. Cancers. 2021;13(13):3158. https://doi.org/10.3390/cancers13133158.
Ronellenfitsch U, Hohenberger P. Surgery for gastrointestinal stromal tumors: state of the art of laparoscopic resection and surgery for M1 tumors. Visc Med. 2018;34(5):367–74. https://doi.org/10.1159/000491799.
Iordanou C, Theodoridis CA, Lykoudis PM, Dimitroulis D, Machairas N, Spartalis E, Kouki P, Pikoulis E, Nikiteas N. Current evidence on laparoscopic vs open resection for gastric stromal tumours. Oncol Lett. 2021;22(4):734. https://doi.org/10.3892/ol.2021.12995.
Mechtersheimer G, Egerer G, Hensel M, Rieker RJ, Libicher M, Lehnert T, Penzel R. Gastrointestinal stromal tumours and their response to treatment with the tyrosine kinase inhibitor imatinib. Virchows Arch. 2004;444(2):108–18. https://doi.org/10.1007/s00428-003-0945-5.
Steinert DM, McAuliffe JC, Trent JC. Imatinib mesylate in the treatment of gastrointestinal stromal tumour. Expert Opin Pharmacother. 2005;6(1):105–13. https://doi.org/10.1517/14656566.6.1.105.
Rutkowski P, Gronchi A, Hohenberger P, Bonvalot S, Schöffski P, Bauer S, Fumagalli E, Nyckowski P, Nguyen BP, Kerst JM, Fiore M, Bylina E, Hoiczyk M, Cats A, Casali PG, Le Cesne A, Treckmann J, Stoeckle E, de Wilt JH, Sleijfer S, Tielen R, van der Graaf W, Verhoef C, van Coevorden F. Neoadjuvant imatinib in locally advanced gastrointestinal stromal tumors (GIST): the EORTC STBSG experience. Ann Surg Oncol. 2013;20(9):2937–43. https://doi.org/10.1245/s10434-013-3013-7.
Wang J, Yin Y, Shen C, Yin X, Cai Z, Pu L, Fu W, Wang Y, Zhang B. Preoperative imatinib treatment in patients with locally advanced and metastatic/recurrent gastrointestinal stromal tumors: a single-center analysis. Medicine. 2020;99(9):e19275. https://doi.org/10.1097/MD.0000000000019275.
Vassos N, Jakob J, Kähler G, Reichardt P, Marx A, Dimitrakopoulou-Strauss A, Rathmann N, Wardelmann E, Hohenberger P. Preservation of organ function in locally advanced non-metastatic gastrointestinal stromal tumors (GIST) of the stomach by neoadjuvant imatinib therapy. Cancers. 2021;13(4):586. https://doi.org/10.3390/cancers13040586.
Wang D, Zhang Q, Blanke CD, Demetri GD, Heinrich MC, Watson JC, Hoffman JP, Okuno S, Kane JM, von Mehren M, Eisenberg BL. Phase II trial of neoadjuvant/adjuvant imatinib mesylate for advanced primary and metastatic/recurrent operable gastrointestinal stromal tumors: long-term follow-up results of Radiation Therapy Oncology Group 0132. Ann Surg Oncol. 2012;19(4):1074–80. https://doi.org/10.1245/s10434-011-2190-5.
Wang SY, Wu CE, Lai CC, Chen JS, Tsai CY, Cheng CT, Yeh TS, Yeh CN. Prospective evaluation of neoadjuvant imatinib use in locally advanced gastrointestinal stromal tumors: emphasis on the optimal duration of neoadjuvant imatinib use, safety, and oncological outcome. Cancers. 2019;11(3):424. https://doi.org/10.3390/cancers11030424.
Marqueen KE, Moshier E, Buckstein M, Ang C. Neoadjuvant therapy for gastrointestinal stromal tumors: a propensity score-weighted analysis. Int J Cancer. 2021;149(1):177–85. https://doi.org/10.1002/ijc.33536.
Miettinen M, Lasota J. Gastrointestinal stromal tumors: review on morphology, molecular pathology, prognosis, and differential diagnosis. Arch Pathol Lab Med. 2006;130(10):1466–78. https://doi.org/10.5858/2006-130-1466-GSTROM.
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–44. https://doi.org/10.1038/nature07205.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74. https://doi.org/10.1016/j.cell.2011.02.013.
Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(11):e493-503. https://doi.org/10.1016/S1470-2045(14)70263-3.
Roxburgh CS, McMillan DC. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Fut Oncol. 2010;6(1):149–63. https://doi.org/10.2217/fon.09.136.
Mantzorou M, Koutelidakis A, Theocharis S, Giaginis C. Clinical value of nutritional status in cancer: what is its impact and how it affects disease progression and prognosis? Nutr Cancer. 2017;69(8):1151–76. https://doi.org/10.1080/01635581.2017.1367947.
Gupta D, Vashi PG, Lammersfeld CA, Braun DP. Role of nutritional status in predicting the length of stay in cancer: a systematic review of the epidemiological literature. Ann Nutr Metab. 2011;59(2–4):96–106. https://doi.org/10.1159/000332914.
Hu B, Yang XR, Xu Y, Sun YF, Sun C, Guo W, Zhang X, Wang WM, Qiu SJ, Zhou J, Fan J. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;20(23):6212–22. https://doi.org/10.1158/1078-0432.CCR-14-0442.
Hirahara N, Tajima Y, Matsubara T, Fujii Y, Kaji S, Kawabata Y, Hyakudomi R, Yamamoto T, Uchida Y, Taniura T. Systemic immune-inflammation index predicts overall survival in patients with gastric cancer: a propensity score-matched analysis. J Gastrointest Surg. 2021;25(5):1124–33. https://doi.org/10.1007/s11605-020-04710-7.
Huang H, Liu Q, Zhu L, Zhang Y, Lu X, Wu Y, Liu L. Prognostic value of preoperative systemic immune-inflammation index in patients with cervical cancer. Sci Rep. 2019;9(1):3284. https://doi.org/10.1038/s41598-019-39150-0.
Ding P, Guo H, Yang P, Sun C, Tian Y, Liu Y, Li Y, Zhao Q. Association between the nutritional risk and the survival rate in newly diagnosed GIST patients. Front Nutr. 2021;8:743475. https://doi.org/10.3389/fnut.2021.743475.
Nakatani M, Migita K, Matsumoto S, Wakatsuki K, Ito M, Nakade H, Kunishige T, Kitano M, Kanehiro H. Prognostic significance of the prognostic nutritional index in esophageal cancer patients undergoing neoadjuvant chemotherapy. Dis Esophagus. 2017;30(8):1–7. https://doi.org/10.1093/dote/dox020.
Migita K, Matsumoto S, Wakatsuki K, Ito M, Kunishige T, Nakade H, Kitano M, Nakatani M, Kanehiro H. A decrease in the prognostic nutritional index is associated with a worse long-term outcome in gastric cancer patients undergoing neoadjuvant chemotherapy. Surg Today. 2017;47(8):1018–26. https://doi.org/10.1007/s00595-017-1469-y.
Ding P, Guo H, Sun C, Yang P, Kim NH, Tian Y, Liu Y, Liu P, Li Y, Zhao Q. Combined systemic immune-inflammatory index (SII) and prognostic nutritional index (PNI) predicts chemotherapy response and prognosis in locally advanced gastric cancer patients receiving neoadjuvant chemotherapy with PD-1 antibody sintilimab and XELOX: a prospective study. BMC Gastroenterol. 2022;22(1):121. https://doi.org/10.1186/s12876-022-02199-9.
Ding P, Yang P, Sun C, Tian Y, Guo H, Liu Y, Li Y, Zhao Q. Predictive effect of systemic immune-inflammation index combined with prognostic nutrition index score on efficacy and prognosis of neoadjuvant intraperitoneal and systemic paclitaxel combined with apatinib conversion therapy in gastric cancer patients with positive peritoneal lavage cytology: a prospective study. Front Oncol. 2022;11:791912. https://doi.org/10.3389/fonc.2021.791912.
Yilmaz A, Mirili C, Bilici M, Tekin SB. A novel predictor in patients with gastrointestinal stromal tumors: systemic immune-inflammation index (SII). J BUON. 2019;24(5):2127–35.
Sun J, Mei Y, Zhu Q, Shou C, Tjhoi WEH, Yang W, Yu H, Zhang Q, Liu X, Yu J. Relationship of prognostic nutritional index with prognosis of gastrointestinal stromal tumors. J Cancer. 2019;10(12):2679–86. https://doi.org/10.7150/jca.32299.
von Mehren M, Kane JM, Bui MM, Choy E, Connelly M, Dry S, et al. NCCN Guidelines Insights: soft tissue sarcoma, version 1.2021. J Natl Compr Canc Netw. 2020;18(12):1604–12. https://doi.org/10.6004/jnccn.2020.0058.
Shen L, Cao F, Qin SK, Ye YJ, Li J, Wang J, et al. Chinese consensus on the diagnosis and treatment of gastrointestinal mesenchymal tumors (2017 edition). Electr J Compr Cancer Therapy. 2018;4(01):31–43.
Choi H. Response evaluation of gastrointestinal stromal tumors. Oncologist. 2008;13(Suppl 2):4–7. https://doi.org/10.1634/theoncologist.13-S2-4.
Li J, Ye Y, Wang J, Zhang B, Qin S, Shi Y, He Y, Liang X, Liu X, Zhou Y, Wu X, Zhang X, Wang M, Gao Z, Lin T, Cao H, Shen L. Chinese Society Of Clinical Oncology Csco Expert Committee On Gastrointestinal Stromal Tumor: Chinese consensus guidelines for diagnosis and management of gastrointestinal stromal tumor. Chin J Cancer Res. 2017;29(4):281–93. https://doi.org/10.21147/j.issn.1000-9604.2017.04.01.
Al-Share B, Alloghbi A, Al Hallak MN, Uddin H, Azmi A, Mohammad RM, Kim SH, Shields AF, Philip PA. Gastrointestinal stromal tumor: a review of current and emerging therapies. Cancer Metastasis Rev. 2021;40(2):625–41. https://doi.org/10.1007/s10555-021-09961-7.
Elinav E, Nowarski R, Thaiss CA, Hu B, Jin C, Flavell RA. Inflammation-induced cancer: crosstalk between tumours, immune cells and microorganisms. Nat Rev Cancer. 2013;13(11):759–71. https://doi.org/10.1038/nrc3611.
Choi Y, Kim JW, Nam KH, Han SH, Kim JW, Ahn SH, Park DJ, Lee KW, Lee HS, Kim HH. Systemic inflammation is associated with the density of immune cells in the tumor microenvironment of gastric cancer. Gastric Cancer. 2017;20(4):602–11. https://doi.org/10.1007/s10120-016-0642-0.
Ding P, Guo H, Sun C, Yang P, Tian Y, Liu Y, Zhang Z, Wang D, Zhao X, Tan B, Liu Y, Li Y, Zhao Q. Relationship between nutritional status and clinical outcome in patients with gastrointestinal stromal tumor after surgical resection. Front Nutr. 2022;9:818246. https://doi.org/10.3389/fnut.2022.818246.
Yamanaka T, Matsumoto S, Teramukai S, Ishiwata R, Nagai Y, Fukushima M. The baseline ratio of neutrophils to lymphocytes is associated with patient prognosis in advanced gastric cancer. Oncology. 2007;73(3–4):215–20. https://doi.org/10.1159/000127412.
Suarez-Carmona M, Lesage J, Cataldo D, Gilles C. EMT and inflammation: inseparable actors of cancer progression. Mol Oncol. 2017;11(7):805–23. https://doi.org/10.1002/1878-0261.12095.
Zhou C, Liu J, Tang Y, Liang X. Inflammation linking EMT and cancer stem cells. Oral Oncol. 2012;48(11):1068–75. https://doi.org/10.1016/j.oraloncology.2012.06.005.
Yuce E, Alandag C, Cakir E, Fidan E. Prognostic factors in gastrointestinal stromal tumors (GIST): could prognostic nutritional index (PNI) be a new prognostic factor? J Coll Physicians Surg Pak. 2022;32(1):81–5. https://doi.org/10.29271/jcpsp.2022.01.81.
Lu Z, Li R, Cao X, Liu C, Sun Z, Shi X, Shao W, Zheng Y, Song J. Assessment of systemic inflammation and nutritional indicators in predicting recurrence-free survival after surgical resection of gastrointestinal stromal tumors. Front Oncol. 2021;11:710191. https://doi.org/10.3389/fonc.2021.710191.
Shau HY, Golub SH. Inhibition of lymphokine-activated killer- and natural killer-mediated cytotoxicities by neutrophils. J Immunol. 1989;143(3):1066–72.
Gong Y, Koh DR. Neutrophils promote inflammatory angiogenesis via release of preformed VEGF in an in vivo corneal model. Cell Tissue Res. 2010;339(2):437–48. https://doi.org/10.1007/s00441-009-0908-5.
Verheul HM, Jorna AS, Hoekman K, Broxterman HJ, Gebbink MF, Pinedo HM. Vascular endothelial growth factor-stimulated endothelial cells promote adhesion and activation of platelets. Blood. 2000;96(13):4216–21.
Whiteside TL. Immune modulation of T-cell and NK (natural killer) cell activities by TEXs (tumour-derived exosomes). Biochem Soc Trans. 2013;41(1):245–51. https://doi.org/10.1042/BST20120265.
Feng XY, Wen XZ, Tan XJ, Hou JH, Ding Y, Wang KF, Dong J, Zhou ZW, Chen YB, Zhang XS. Ectopic expression of B and T lymphocyte attenuator in gastric cancer: a potential independent prognostic factor in patients with gastric cancer. Mol Med Rep. 2015;11(1):658–64. https://doi.org/10.3892/mmr.2014.2699.
Acknowledgements
Not applicable.
Funding
This work was supported by the Cultivating Outstanding Talents Project of Hebei Provincial Government Fund (No. 2019012); Hebei public health committee county-level public hospitals suitable health technology promotion and storage project (No. 2019024); Hebei University Science and Technology Research Project (No. ZD2019139).
Author information
Authors and Affiliations
Contributions
Contributions: (I) conception and design: QZ; (II) Administrative support: QZ; (III) Provision of study materials or patients: PD, PY, YT, HG, JW; (IV) collection and assembly of data: PD, PY, YT, HG, YL, HW, LM; (V) data analysis and interpretation: PD, CS, SL, HW; (VI) manuscript writing: All authors; (VII) Final approval of manuscript: All authors. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All patients were informed about the adverse effects accompanying therapies and they all signed informed consent forms. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study design was approved by the Ethics Committee of the Fourth Hospital of Hebei Medical University.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ding, P., Wu, J., Wu, H. et al. Inflammation and nutritional status indicators as prognostic indicators for patients with locally advanced gastrointestinal stromal tumors treated with neoadjuvant imatinib. BMC Gastroenterol 23, 23 (2023). https://doi.org/10.1186/s12876-023-02658-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-023-02658-x