Abstract
Background
Esophageal perforation (EP) has a high mortality rate and poor prognosis. This single-center retrospective study aims to analyze the related risk factors for benign EP.
Methods
We retrospectively analyzed 135 patients with benign EP admitted to the First Affiliated Hospital of Nanchang University from January 2012 to December 2020. Univariate and multivariate logistic analysis were performed to estimate risk factors for prognosis of esophageal perforation patients.
Results
There were 118 EP patients with foreign body ingestion and 17 patients with nonforeign body ingestion. Fish bones (78/118) were the most common foreign body and most of the nonforeign EPs were caused by spontaneous esophageal rupture (14/17). Foreign body perforations occurred mostly in the upper thoracic segment (70/118) and middle thoracic segment (31/118), and spontaneous esophageal ruptures occurred mostly in the lower thoracic segment (15/17). Fifteen patients (11.1%) died during hospitalization or within one month of discharge. Multivariable logistic regression analysis showed that high white blood cell (WBC) levels [odds ratio (OR) = 2.229, 95% confidential interval (CI): 0.776–6.403, P = 0.025], chest or mediastinal emphysema (OR = 7.609, 95% CI: 2.418–23.946, P = 0.001), and time to treatment > 72 h (OR = 3.407, 95% CI: 0.674–17.233, P = 0.018) were independent risk factors for poor prognosis.
Conclusion
Foreign body was the major reason for benign EP. High WBC level, chest or mediastinal emphysema and time to treatment > 72 h were risk factors for poor prognosis.
Similar content being viewed by others

Introduction
Benign esophageal perforation (EP) is a life-threatening complaint in the emergency room. Nonspecific clinical symptoms often delay patient treatment, which greatly increases the risk of complications and death from esophageal injury [1].
Esophageal foreign bodies (EFBs) usually occur in young children and specific high-risk groups of adults such as those with an underlying esophageal disease, prisoners, those who are mentally retarded, and those with psychiatric illnesses, and there are multiple types and incarcerated locations of foreign bodies, which increases the difficulty of clinical treatment [2,3,4]. Studies have shown that foreign bodies account for 12% of all EPs, and the mortality rate is 2.1% [5]. The anatomical location of the thoracic esophagus is adjacent to the trachea, heart, and blood vessels of the chest. EFB is often accompanied by serious medical conditions, such as tracheoesophageal fistula, esophagus-aortic fistula, hemorrhage, and mediastinal abscess complications [1]. Iatrogenic causes occur as commonly as esophageal foreign bodies [6], which account for 47.6–60% of EPs [7, 8]. Another cause of nonforeign body EP is spontaneous esophageal rupture, also known as Boerhaave syndrome, which is an uncommon and life-threatening disease that was first described in 1724 [6, 9, 10]. The mortality rate associated with EP is high, between 10 and 40% reported in some centers [11,12,13,14]. Early diagnosis and treatment are considered key factor for successful treatment [15, 16].
According to the impacted position of the EFB, it can be divided into cervical, thoracic, and abdominal foreign bodies, and foreign bodies in the corresponding positions cause corresponding esophageal injury. A systematic review of the literature included 61 studies and revealed 5044 EFBs impacted in the cervical esophagus (66.9%), 1862 in the thoracic esophagus (24.7%) and 635 in the lower esophagus (8.4%) [1]. Some scholars divided EP patients into a ≤ 24 h group and > 24 h group according to whether the treatment time after eating foreign bodies exceeded 24 h [17]. In 2009, a research group from the University of Pittsburgh proposed an EP severity scoring system (PSS) based on clinical factors [11]. This scoring system ranks esophageal perforation as low, intermediate, and high risk (on a scale of 0–18) according to the patient’s clinical risk factors, and is designed to measure the severity of esophageal rupture by weighting clinical variables. Their study showed that among patients with scores ≤ 2, 3–5, and > 5, the complication rates were 53%, 65%, and 81% respectively, and the mortality rates were 1%, 3%, and 27% respectively [11]. The classification of all types is mainly based on the patient’s medical history and clinical manifestations, to guide follow-up treatment and predict prognosis, but there is no clear consensus on the classification standards.
Currently, there is no consensus on the management of benign EP. Nonoperative management included conservative and endoscopic interventions. Various surgical approaches to the treatment of esophageal perforation have been the mainstays of therapy for decades [18,19,20]. Although operative management remains the standard in most of patients with EP, nonoperative management may be successfully implemented in selected patients with low morbidity and mortality if favorable radiographic and clinical characteristics are present.
The treatment of benign EP generally requires individualized attention such as supportive care that needs to be further practiced and summarized in clinical practice. Although there are various treatment methods, many factors are still considered to be associated with poor prognoses, such as time to treatment, site of perforation, vital signs, and sepsis [14, 15, 21]. In this study, we analyzed the diagnosis and treatment of benign EP and determined the patients’ potential risk factors associated with poor prognosis to guide clinical treatment.
Materials and methods
Subjects and study design
This retrospective study was conducted in the First Affiliated Hospital of Nanchang University, and patient diagnoses of EP from January 2012 to December 2020 were retrospectively analyzed through the electronic medical record system. Diagnostic criteria were as follows: (1) With or without a history of ingestion or eating the suspicious foreign body, or fever, pain in swallowing, chest and back pain, dysphagia, foreign body sensation, and other related symptoms. (2) Lesions penetrating the outer wall of the esophagus, extraluminal air or fluid surrounding the esophagus or within the mediastinum, or pleural effusions, and other lesions detected by computed tomography (CT), endoscopy, X-ray, gastrointestinal angiography, and other auxiliary examinations.
Detailed inclusion criteria were as follows: (1) Patients diagnosed with benign EP or esophageal rupture. (2) Patients whose lesions were adjacent to intrathoracic blood vessels, important organs, mediastinum, or diseases that were within the scope of thoracic surgery due to perforation. Exclusion criteria were as follows: (1) Patients with atypical esophageal perforation or perforation and rupture not reaching the full thickness of the esophagus. (2) Patients with incomplete demographic data.
All patients with suspected perforation subsequently underwent CT (Fig. 1A). Operative management included any kind of surgical intervention. Nonoperative management comprised all nonsurgical approaches ranging from simple conservative treatment to advanced interventional and endoscopic measures such as stent insertion and removal of foreign bodies (Fig. 2A, B). We used white blood cells (WBCs) > 10.02 × 109/L as the cutoff for high WBC levels. Fistula were detected by endoscopy, X-ray, CT, and other imaging methods (Figs. 1B and 2C).
The patients were divided into Groups A and B according to the prognosis. Group A: patients were in good states and no complications occurred during hospitalization or within one month of discharge. Group B: included patients who died during hospitalization or accompanied with esophageal fistula or esophagotracheal fistula during hospitalization or within one month of discharge.
Data collection
The following information regarding initial presentation, treatment, clinical course, and outcome was collected: age, sex, etiology of perforation, symptoms, time to treatment, type of management, site of perforation, complications, hospitalization, outcome, and levels of WBCs and neutrophils before treatment and follow-up. For patients with perforation of the foreign body, time to diagnosis, time to treatment, and the situation of foreign bodies were collected. Follow-up was conducted one month after discharge.
Statistical analysis
Statistical analyses to identify prediction factors were performed using SPSS 25.0 for Windows (SPSS, Chicago, IL). Continuous variables are expressed as the mean ± standard deviation, and categorical data are presented as absolute numbers and percentages. The chi-square test was used to determine the significance of differences between categorical variables, and the t-tests was used for continuous variables. We performed univariate logistic hazard regression analysis in a forward stepwise manner. Significant variables in univariate analysis (P < 0.05) were carried into a multivariate logistic analysis to obtain the odds ratio (OR) and corresponding 95% confidential interval (CI) for every independent prognostic variable. Statistical significance was designated by P < 0.05.
Results
Baseline characteristics
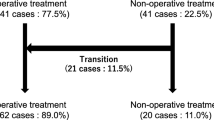
The study comprises a total of 135 patients with EP (Fig. 3). The baseline characteristics of the patients are presented in Table 1. The mean age of these patients was 55.6 ± 14.3 years, and 77 of these patients (57.0%) were female. There were 118 cases of EP caused by foreign bodies and 17 cases developed nonforeign body perforation. The most common clinical symptoms were chest and back pain (77.8%), followed by swallowing pain (74.1%). In the foreign body group, swallowing pain was the most common symptom (73.7%), followed by chest and back pain (66.7%). Of 80 patients who received treatment for perforation after 24 h, only 40.7% (55/135) received treatment within 24 h. Sixty-eight patients (50.4%) had pleural or mediastinal pneumonitis, 46 patients (34.1%) had pleural effusion, 77 patients (57.0%) were complicated by esophageal inflammation or mediastinal abscess, and 9 patients (6.6%) developed mediastinitis. The average number of WBCs in the foreign body group was 10.1 ± 4.1 × 109/L, while the average number of WBCs in the nonforeign body group was 13.6 ± 5.6 × 109/L. In terms of imaging characteristics, among the patients with foreign body perforation, 84 patients (71.2%) had foreign bodies adjacent to the great intrathoracic blood vessels and pericardium, six patients penetrated the esophagus and pierced the aorta, two patients had tracheal rupture, and one patient pierced the pericardium. Two patients were misdiagnosed with esophageal tumors by CT scan, jujube pits were then detected through endoscopy. Figure 4 compares the location of the EP for different reasons. There were 70 patients (59.3%) with foreign bodies located in the upper thoracic segment, followed by 31 patients (26.3%) with foreign bodies in the middle thoracic segment. Fifteen patients (88.2%) had nonforeign body perforations located in the lower thoracic segment.
Types of foreign body and nonforeign body EPs are shown in Table 2. Among the foreign body group, 78 cases (66.1%) were due to fish bones, 25 cases (21.2%) were due to animal bones (chicken, duck, pig), six cases (5.1%) were due to jujube pits, other animal bones (rabbit, bullfrog, turtle, etc.) and other foreign bodies (iron pieces, braces, eggshells, etc.) had three cases each. Among the foreign body group, three patients had a history of foreign body swallowing, but no foreign body was found by intraoperative digestive endoscopy. Among the nonforeign body group, 14 patients (82.4%) had a spontaneous EP, and iatrogenic injury accounted for 11.8%. One patient developed traumatic EP.
Treatment method and treatment result
The details the treatment methods, treatment outcomes, and causes of death are shown in Table 3. A total of 135 patients were included. Endoscopy is a major treatment for removing EFBs. Surgery is considered a last resort and is usually reserved for high-risk cases in which severe complications are suspected. During hospitalization and within one month after discharge, 15 patients (11.1%) died, 9 patients developed esophageal fistula and empyema after discharge, and 21 patients had EP wounds exceeding 1 cm.
Clinical features and risk factors for prognosis of esophageal perforation
To stratify the clinical risks associated with EP, all the patients were divided into two groups according to prognosis during hospitalization or within one month of discharge. Group A: Patients were in good states and no complications occurred during hospitalization or within one month of discharge. Group B: included patients who died during hospitalization or had esophageal fistula or esophagotracheal fistula during hospitalization or within one month of discharge. As shown in Table 4, EP caused by foreign bodies usually had a poor prognosis compared to the nonforeign body group (P = 0.029). Patients with infection symptoms such as esophagitis or esophageal abscess (P = 0.003), high WBC level (P = 0.013), and chest or mediastinal emphysema (P = 0.002) tended to develop a worse outcome. There were no significant differences between Group A and Group B for age, sex, and location of perforation. The heart rate (P < 0.001) and temperature (P = 0.014) were higher in Group B than in Group A.
The risk factors for prognosis are provided in Table 5. Univariate analysis showed that nonforeign body, WBC > 10.02 × 109/L, esophagitis or esophageal abscess, hydrothorax, chest or mediastinal emphysema and time to treatment > 72 h were significantly correlated with poor prognosis (P < 0.05). Multivariable logistic regression analysis showed that high WBC level (OR = 2.229, 95% CI: 0.776–6.403, P = 0.025), chest or mediastinal emphysema (OR = 7.609, 95% CI: 2.418–23.946, P = 0.001), and time to treatment > 72 h (OR = 3.407, 95% CI: 0.674–17.233, P = 0.018,) were independent risk factors for poor prognosis.
Discussion
EP is a clinically critical disease with high mortality. Improper or delayed treatment can lead to various complications [10]. Symptoms (pain, vomiting, hematemesis, dysphagia, or tachypnea) and signs (tachycardia, fever, subcutaneous emphysema, cardiac crunch, chest personality, or dullness) of EP vary with cause and location (cervical, thoracic, or abdominal). Pain was the most common symptom, present in 70 to 90% of patients, usually referring directly to the site of perforation [22]. In our study, regardless of the cause of EP, two patients were misdiagnosed as aortic dissection due to severe chest and back pain at the first diagnosis. This suggests that in patients with relevant medical history, attention should be given to the identification of chest and back pain-related diseases. In patients with foreign body perforation, swallowing pain and chest and back pain were the most common causes due to foreign body incarceration, and tachycardia, respiratory limitation, hypotension, and other emergencies occurred less frequently. In a small number of cases, due to prolonged incarceration of the foreign body, abscesses often lead to fever, pleural effusion, and chest tightness. At the same time, this study also found that the level of WBCs in the nonforeign body group was higher than that in the foreign body group, which may indicate a heavier infection. In addition, some patients required mechanical ventilation upon admission, and early surgical debridement, and treatment for such patients can effectively reduce the complications of patients and save their lives. A study conducted by Shaker et al. [23] confirmed that early diagnosis and management (golden 24 h) were crucial for successful outcomes in patients with a ruptured esophagus.
Various reasons lead to EP. In our study, foreign bodies accounted for most benign EPs, followed by spontaneous esophageal perforation, which differs from previous studies [24, 25]. In our study, we found that foreign body EP was more common in the upper and middle thoracic segments, consistent with previous studies [26, 27], which is mostly due to the second esophagus stenosis, where the aortic arch and the left main bronchus cross, located in the upper and middle thoracic segments. At the same time, we found that spontaneous EP was almost always located in the lower thoracic segment, similar to the study conducted by Schweigert et al. [28].
Over the last two decades, advances in endoscopic technologies have facilitated salvage of the native esophagus in the setting of a perforation [1, 29]. Before treatment, physicians from the department of cardiothoracic surgery, otolaryngology, or digestive endoscopy were consulted to evaluate the patient’s clinical condition. When it is difficult to decide the operation method or there is a risk of endoscopic treatment, the surgeon should accompany the patients, and endoscopic removal under sedation or general anesthesia in the operating room should be considered. Laryngoscopy and digestive endoscopy are both diagnostic and therapeutic measures. Esophagoscopy is a traditional method to remove foreign bodies, with the advantage of protecting the airway. After endoscopic removal of the foreign body, if there is a large mediastinal abscess, a large esophageal fistula, or other conditions that require surgical treatment, early surgical treatment is generally performed. The surgical methods included abscess incision and drainage, foreign body removal, esophageal fistula repair, esophageal fistula exclusion, and secondary suturing. A previous study showed that surgical treatment is usually associated with low mortality [30]. However, in our study, the mortality rate between open surgery and thoracoscopic surgery was 27.6%. This is probably due to the presence of foreign bodies and abscesses involving or adjacent to the aorta.
At present, various studies are focusing on the risk factors affecting the prognosis of patients with benign EP. In this study, we used death combined with adverse events as treatment outcome indicators, consistent with previous studies [18, 31]. According to univariate analysis, nonforeign body, WBC > 10.02 × 109/L, esophagitis or esophageal abscess, hydrothorax, chest or mediastinal emphysema, and time to treatment > 72 h were significantly correlated with poor prognosis. Multivariate analysis showed that high WBC level, chest or mediastinal emphysema, time to treatment > 72 h were prognostic factors. Various studies divided time to treatment into two types, ≤ 24 h and > 24 h, and mentioned that greater than 24 h between diagnosis and treatment served as a significant predictor [32,33,34]. Our study provided a more refined classification and demonstrated that time to treatment > 72 h was associated with a higher risk of poor prognosis. Studies conducted by Bhatia et al. [18] and Huang et al. [31] also, suggest that inflammation and abscess are key factors affecting patient prognosis and mortality. The scoring criteria for EP proposed by Abbas et al. [18] included pleural effusion and increased WBC counts. The criteria also included indicators such as fever, respiratory function involvement, hypotension, and obvious perforation and leakage, which were consistent with the results of our univariate analysis.
This study does have some limitations. First, our study was retrospective in a single center and had a limited sample size. Second, it only involved patients from one region, so the eating habits of these patients only reflect southern Chinese customs. Finally, the currently accepted evaluation standard for EP is the PSS, which was not evaluated in this study. In subsequent studies, the PSS should be evaluated, and its validity can be verified.
Conclusion
Benign EP has a high mortality rate and a high risk of poor prognosis, especially for patients caused by nonforeign body. High WBC level, chest or mediastinal emphysema, and time to treatment > 72 h were independent risk factors for benign EP and were significantly associated with poor prognosis. Prompt identification of perforation as the cause of a patient’s problem, reduce the risk of infection, and timely choice of a therapeutic approach are keys to maximize successful outcomes. The results of this study may help better identify patients with EP who are at higher risk for developing poor prognoses and improve their follow-up treatment and clinical course, but large prospective randomized clinical trials are still needed.
Availability of data and materials
The data that support the findings of this study are available from the correspond author but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the correspond author.
Abbreviations
- EP:
-
Esophageal perforation
- EFBs:
-
Esophageal foreign bodies
- PSS:
-
Pittsburgh severity scoring system
- CT:
-
Computed tomography
- WBCs:
-
White blood cells
- OR:
-
Odds ratio
- CI:
-
Confidential interval
References
Aiolfi A, Ferrari D, Riva CG, Toti F, Bonitta G, Bonavina L. Esophageal foreign bodies in adults: systematic review of the literature. Scand J Gastroenterol. 2018;53(10–11):1171–8.
Sahn B, Mamula P, Ford CA. Review of foreign body ingestion and esophageal food impaction management in adolescents. J Adolesc health: official publication Soc Adolesc Med. 2014;55(2):260–6.
Popel J, El-Hakim H, El-Matary W. Esophageal foreign body extraction in children: flexible versus rigid endoscopy. Surg Endosc. 2011;25(3):919–22.
Brady PG. Esophageal foreign bodies. Gastroenterol Clin N Am. 1991;20(4):691–701.
Hossain SM, de Caestecker J. Acute oesophageal symptoms. Clin Med. 2015;15(5):477–81.
Brinster CJ, Singhal S, Lee L, Marshall MB, Kaiser LR, Kucharczuk JC. Evolving options in the management of esophageal perforation. Ann Thorac Surg. 2004;77(4):1475–83.
Ceuterick V, Decaluwé H, Coosemans W, Nafteux P, Van Veer H, Van Raemdonck D, et al. Esophageal wall rupture after EUS-FNA for mediastinal staging: report of two cases. Acta Chir Belg. 2016;116(1):48–50.
Di Leo M, Maselli R, Ferrara EC, Poliani L, Al Awadhi S, Repici A. Endoscopic management of Benign esophageal ruptures and leaks. Curr Treat Options Gastroenterol. 2017;15(2):268–84.
Sulpice L, Dileon S, Rayar M, Badic B, Boudjema K, Bail JP, et al. Conservative surgical management of Boerhaave’s syndrome: experience of two tertiary referral centers. Int J Surg 2013;11(1):64–7.
Jones II WG, Ginsberg RJ. Esophageal perforation: a continuing challenge. Ann Thorac Surg. 1992;53(3):534–43.
Abbas G, Schuchert MJ, Pettiford BL, Pennathur A, Landreneau J, Landreneau J, et al. Contemporaneous management of esophageal perforation. Surgery 2009;146(4):749–55; discussion 55–6.
Puerta Vicente A, Priego Jiménez P, Cornejo López M, García-Moreno Nisa F, Rodríguez Velasco G, Galindo Álvarez J, et al. Management of esophageal perforation: 28-Year experience in a major Referral Center. Am Surg. 2018;84(5):684–9.
Hasimoto CN, Cataneo C, Eldib R, Thomazi R, Pereira RS, Minossi JG, et al. Efficacy of surgical versus conservative treatment in esophageal perforation: a systematic review of case series studies. Acta Cirurg Bras. 2013;28(4):266–71.
Gupta NM, Kaman L. Personal management of 57 consecutive patients with esophageal perforation. Am J Surg. 2004;187(1):58–63.
Kim-Deobald J, Kozarek RA. Esophageal perforation: an 8-year review of a multispecialty clinic’s experience. Am J Gastroenterol. 1992;87(9):1112–9.
Reeder LB, DeFilippi VJ, Ferguson MK. Current results of therapy for esophageal perforation. Am J Surg. 1995;169(6):615–7.
Zhang X, Jiang Y, Fu T, Zhang X, Li N, Tu C. Esophageal foreign bodies in adults with different durations of time from ingestion to effective treatment. J Int Med Res. 2017;45(4):1386–93.
Bhatia P, Fortin D, Inculet RI, Malthaner RA. Current concepts in the management of esophageal perforations: a twenty-seven year canadian experience. Ann Thorac Surg. 2011;92(1):209–15.
DeVivo A, Sheng AY, Koyfman A, Long B. High risk and low prevalence diseases: esophageal perforation. Am J Emerg Med. 2022;53:29–36.
Sepesi B, Raymond DP, Peters JH. Esophageal perforation: surgical, endoscopic and medical management strategies. Curr Opin Gastroenterol. 2010;26(4):379–83.
Liao F, Zhu Z, Pan X, Li B, Zhu Y, Chen Y, et al. Safety and efficacy of nonoperative treatment in esophageal perforation caused by foreign bodies. Clin Transl Gastroenterol. 2022;13(1):e00451.
Gouge TH, Depan HJ, Spencer FC. Experience with the Grillo pleural wrap procedure in 18 patients with perforation of the thoracic esophagus. Ann Surg 1989;209(5):612-7; discussion 7–9.
Shaker H, Elsayed H, Whittle I, Hussein S, Shackcloth M. The influence of the ‘golden 24-h rule’ on the prognosis of oesophageal perforation in the modern era. Eur J Cardiothorac Surg. 2010;38(2):216–22.
Jiang J, Yu T, Zhang YF, Li JY, Yang L. Treatment of cervical esophageal perforation caused by foreign bodies. Dis Esophagus. 2012;25(7):590–4.
Freeman RK, Van Woerkom JM, Vyverberg A, Ascioti AJ. Esophageal stent placement for the treatment of spontaneous esophageal perforations. Ann Thorac Surg. 2009;88(1):194–8.
Sdralis EIK, Petousis S, Rashid F, Lorenzi B, Charalabopoulos A. Epidemiology, diagnosis, and management of esophageal perforations: systematic review. Dis Esophagus. 2017;30(8):1–6.
Law TT, Chan JY, Chan DK, Tong D, Wong IY, Chan FS, et al. Outcomes after oesophageal perforation: a retrospective cohort study of patients with different aetiologies. Hong Kong medical journal = Xianggang yi xue za zhi. 2017;23(3):231–8.
Schweigert M, Dubecz A, Solymosi N, Ofner D, Stein HJ. Times and trends in the treatment of spontaneous perforation of the esophagus: from Herman Boerhaave to the present age. Am Surg. 2013;79(9):902–8.
Khaitan PG, Famiglietti A, Watson TJ. The etiology, diagnosis, and management of esophageal perforation. J Gastrointest Surg. 2022;26(12):2606–15.
Richardson JD. Management of esophageal perforations: the value of aggressive surgical treatment. Am J Surg. 2005;190(2):161–5.
Huang Y, Lu T, Liu Y, Zhan C, Ge D, Tan L, et al. Surgical management and prognostic factors in esophageal perforation caused by foreign body. Esophagus. 2019;16(2):188–93.
Freeman RK, Ascioti AJ, Dake M, Mahidhara RS. An analysis of esophageal stent placement for persistent leak after the operative repair of intrathoracic esophageal perforations. Ann Thorac Surg 2014;97(5):1715-9; discussion 9–20.
Abu-Daff S, Shamji F, Ivanovic J, Villeneuve PJ, Gilbert S, Maziak DE, et al. Esophagectomy in esophageal perforations: an analysis. Dis Esophagus. 2016;29(1):34–40.
Glatz T, Marjanovic G, Kulemann B, Hipp J, Theodor Hopt U, Fischer A, et al. Management and outcome of esophageal stenting for spontaneous esophageal perforations. Dis Esophagus. 2017;30(3):1–6.
Acknowledgements
We would like to thank Pro. Xiaoming Liu provided the funding by grants from the National Natural Science Foundation of China for this writing assistance.
Funding
This study was supported by grants from the National Natural Science Foundation of China (Grant No. 82060507, PI: Xiaoming Liu).
Author information
Authors and Affiliations
Contributions
QYY data analysis, and manuscript writing. HPL: sample collecting and data analysis. XS and XML: project development. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research protocol of the Chinese cohort was approved by the Ethics Committee of the First Affiliated Hospital of Nanchang University. All the patients provided informed consent. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, Q., Liu, H., Shu, X. et al. Risk factors for the poor prognosis of Benign esophageal perforation: 8-year experience. BMC Gastroenterol 22, 537 (2022). https://doi.org/10.1186/s12876-022-02624-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-022-02624-z