Abstract
Background
Primary squamous cell carcinoma (SCC) of the pancreas with pseudocysts, especially diagnosed by endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA), is extremely rare.
Case presentation
A 64-year-old man was admitted to our department for abdominal distension. Two months ago, he experienced abdominal pain for 1 day and was diagnosed with acute pancreatitis in another hospital. After admission, laboratory tests showed the following: amylase 400 U/L, lipase 403 U/L, and carbohydrate antigen 19–9 (CA19-9) 347 U/mL. Abdominal computed tomography (CT) revealed pancreatitis with a pseudocyst with a diameter measuring 7 cm. During linear EUS, a large pseudocyst (5.4 × 5.2 cm) was observed in the pancreatic body. EUS-FNA was performed. We obtained specimens for histopathology and placed a plastic stent through the pancreas and stomach to drain the pseudocyst. Puncture fluid examination revealed the following: CA19-9 > 12,000 U/mL carcinoembryonic antigen (CEA) 7097.42 ng/ml, amylase 27,145.3 U/L, and lipase > 6000 U/L. Cytopathology revealed an abnormal cell mass, and cancer was suspected. Furthermore, with the result of immunohistochemistry on cell mass (CK ( +), P40 ( +), p63 ( +), CK7 (−) and Ki-67 (30%)), the patient was examined as squamous cell carcinoma (SCC). However, the patient refused surgery, radiotherapy and chemotherapy. After drainage, the cyst shrank, but the patient died 3 months after diagnosis due to liver metastasis and multiple organ failure.
Conclusion
For patients with primary pancreatic pseudocysts with elevated serum CEA and CA19-9 levels, we should not rule out pancreatic cancer, which may also be a manifestation of primary pancreatic SCC. EUS-FNA is helpful for obtaining histopathology and cytology and thus improving diagnostic accuracy.
Similar content being viewed by others
Background
Pancreatic squamous cell carcinoma (SCC) is a primary rare malignancy, accounting for 0.5–2.0% of all malignant pancreatic tumors, and is considered an aggressive subtype with a poor prognosis [1, 2]. In recent years, an increasing number of pancreatic lesions have been diagnosed by endoscopic ultrasound-guided fine-needle aspiration or biopsy (EUS-FNA or EUS-FNB) [3,4,5,6,7]. However, nearly all of the cases were solid or solid-cystic lesions of the pancreas. To our knowledge, there have been no cases of primary SCC of the pancreas with pseudocysts, especially those diagnosed by EUS-FNA. Here, we report a rare case of SCC of the pancreas with a pseudocyst as the main presentation.
Case presentation
A 64-year-old man was admitted to our department for abdominal distension. Two months ago, he experienced abdominal pain for 1 day and was diagnosed with acute pancreatitis in another hospital. There was no cystic lesion of pancreas at that time. The patient did not present with cutaneous or sclera icterus, fever, melena, swallowing difficulties or diarrhea but did present with weight loss of 2 kg. After admission, the physical examination showed that the patient had tenderness in the upper abdomen, and a mass approximately 5.0 × 6.0 cm in size and soft in texture could be felt in the upper abdomen. The results of other physical examinations were unremarkable. He denied alcohol use or any history of chronic or significant medical or family illnesses. After admission, laboratory tests showed the following: amylase 400 U/L (normal, 0–40 U/L), lipase 403 U/L (normal, 0–60 U/L), carbohydrate antigen 19–9 (CA19-9) 347 U/mL (normal, < 39 U/mL), and albumin 31.4 g/L. Other routine laboratory tests did not indicate any abnormalities.
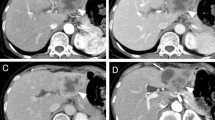
Contrast-enhanced abdominal computed tomography (CT) revealed pancreatitis with a pseudocyst (diameter 7 cm), in which there was fluid (Fig. 1). In the cyst, no necrotic tissue was found and the boundary was clear. Additionally, no obvious low-density mass was found around the cyst and the tail of pancreas was atrophied. The diameter of the pancreatic duct was approximately 0.45 cm. There were no enlarged lymph nodes in the upper abdomen. In addition, the CT scan of the chest was normal. MRCP revealed that there was no debris in the cyst, the pancreatic duct in the head of pancreas was not dilated, and the main pancreatic duct was not connected with the cyst.
Gastric endoscopy showed no abnormal findings in the upper gastrointestinal tract. During the linear EUS examination, a large pseudocyst was observed in the body of the pancreas with a maximum US cross-section of approximately 5.4 × 5.2 cm. The margin of the cyst was clear and no blood flow was detected with color Doppler ultrasonography. Some hyperechoic floccules were observed in the cyst and there was septum in the lumen. There was no debris in the cyst, and the cyst fluid aspirated by EUS-FNA was also without debris. There was no obvious dilatation of the pancreatic duct. Endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) was performed. The exact site of EUS-FNA was the posterior wall of the upper part of the stomach, and the distance between the ultrasonic probe and the cyst was no more than 1 cm. After puncturing the cystic lesion, the stylet was removed, and 10 mL of negative pressure suction was applied within the lesion. The syringe was filled with brown liquid. We collected 20 ml of fluid for the examination of amylase, carcinoembryonic antigen (CEA), and CA19-9. We also performed EUS-FNA to obtain specimens for histopathology and placed a plastic stent for drainage of the pseudocyst through the pancreas and stomach (Fig. 2). Puncture fluid examination revealed the following: CA19-9 > 12,000 U/ml, CEA 7097.42 ng/ml, amylase 27,145.3 U/L, and lipase > 6000 U/L.
After EUS-FNA, pathological cytology revealed an atypical cell mass, and cancer was suspected. Based on the immunohistochemistry results, CK ( +), P40 ( +), p63 ( +), CK7 (-) and Ki-67 (30%), the patient was diagnosed as squamous cell carcinoma (SCC) (Fig. 3).
The patient refused surgery, radiotherapy and chemotherapy. After drainage, the cyst shrank, but the patient died 3 months after diagnosis, due to liver metastasis and multiple organ failure.
Summary of previously reported cases from 2009 to 2020
We searched PubMed for the following keywords in the title/abstract and found 15 cases of SCC of the pancreas reported from 2009 to 2020: “squamous cell carcinoma”, “pancreas”, “endoscopic ultrasound-guided fine-needle aspiration” and “EUS-FNA” [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23]. A summary of these cases is displayed (Table 1). The patients ranged in age from 45 to 82 years, with a mean age of 67.9 ± 6.7 years. Among these 15 patients, only one had cystic lesions, which was diagnosed by EUS-guided confocal endoscopy, 1 had cystic and solid lesions, and the others had solid masses of the pancreas. There were no reports on pseudocyst-associated pancreatic SCC. Among the 15 patients, more than 50% (8/15) had metastasis at diagnosis. Although the patients received different treatments, including surgery, radiotherapy and chemotherapy, the survival time of almost all patients was less than 12 months. The prognosis of pancreatic SCC is poor.
Discussion and conclusions
SCC is a very rare exocrine pancreatic malignant tumor. The clinical presentation of primary SCC of the pancreas is similar to that of ductal adenocarcinoma of the pancreas [24]. In 2019, Tella SH et al. searched the National Cancer Database (NCDB) (2004–15) and reported 182,090 patients prior to matching, 181,575 with pancreatic adenocarcinoma and 515 with SCC; thus, SCC accounted for only 0.28% of all pancreatic cancers. The proportions of patients with stage III and IV disease at diagnosis were 14% and 62%, respectively. For stage IV disease, the most common distant sites of metastases were the liver (32%) and lungs (6%) [25]. Although different therapeutic methods have been used to treat pancreatic SCC, including surgical resection, chemotherapeutic regimens, and radiotherapy, none have proven effective [26]. The proportion of patients with stage III and IV disease at diagnosis was above 76%, so survival was poor [25, 26].
EUS-FNA has been increasingly used for the identification of solid pancreatic lesions and has shown high sensitivity and specificity [5, 6]. EUS-FNA is also helpful for obtaining histopathology and cytology results to improve diagnostic accuracy in pancreatic cystic neoplasms. A combined analysis of cyst fluid CEA, CA19-9, and cyst fluid lipase levels provides the highest accuracy for differentiating malignant and benign pancreatic cystic lesionsn [27]. Pancreatic malignant cysts usually have the following characteristics: they are found in middle-aged and elderly people without a history of pancreatitis; imaging is often accompanied by separation, calcification, and pancreatic duct expansion; the contents of the cysts are mostly mucus, nipple, and solid components; and the level of amylase in the cysts is low [28]. However, in our case, there was no obvious sign of a malignant cyst at the initial examination. The patient experienced abdominal pain and was diagnosed with acute pancreatitis, which ultimately resulted in a large pseudocyst. During EUS-guided drainage, the color of the cyst fluid was brown, consistent with the appearance of a pseudocyst. Due to the increase in CA19-9, we performed EUS-FNA, but the final diagnosis was SCC of the pancreas. Disease progression was also consistent with that of pancreatic SCC.
Normally, the pancreas lacks squamous epithelium. Although there are many hypotheses, the pathogenesis of pure SCC of the pancreas remains elusive [24]. However, for patients with pancreatic pseudocysts with elevated serum CEA and CA19-9 levels, we should not rule out pancreatic cancer, which may also be a manifestation of primary pancreatic SCC. Additional molecular biological studies are needed to confirm these findings.
Availability of data and materials
This case report contains clinical data from the electronic medical record in The People’s Hospital of Nanchuan, Chongqing, China. Additional information is available from the corresponding author on reasonable request from the editor.
Abbreviations
- SCC:
-
Squamous cell carcinoma
- EUS-FNA:
-
Endoscopic ultrasound-guided fine-needle aspiration
- CA19-9:
-
Carbohydrate antigen 19–9
- CEA:
-
Carcinoembryonic antigen
- CT:
-
Computed tomography
References
Brown HA, Dotto J, Robert M, Salem RR. Squamous cell carcinoma of the pancreas. J Clin Gastroenterol. 2005;39(10):915–9.
Makarova-Rusher OV, Ulahannan S, Greten TF, Duffy A. Pancreatic squamous cell carcinoma: a population-based study of epidemiology clinicopathologic characteristics and outcomes. Pancreas. 2016;45(10):1432–7.
Attiyeh MA, Chakraborty J, Doussot A, Langdon-Embry L, Mainarich S, Gonen M, Balachandran VP, D’Angelica MI, DeMatteo RP, Jarnagin WR, et al. Survival prediction in pancreatic ductal adenocarcinoma by quantitative computed tomography image analysis. Ann Surg Oncol. 2018;25(4):1034–42.
Tadic M, Stoos-Veic T, Kujundzic M, Turcic P, Aralica G, Boskoski I. Insulin-like growth factor 2 binding protein 3 expression on endoscopic ultrasound guided fine needle aspiration specimens in pancreatic ductal adenocarcinoma. Eur J Gastroenterol Hepatol. 2020;32(4):496–500.
Chen J, Yang R, Lu Y, Xia Y, Zhou H. Diagnostic accuracy of endoscopic ultrasound-guided fine-needle aspiration for solid pancreatic lesion: a systematic review. J Cancer Res Clin Oncol. 2012;138(9):1433–41.
Yoshinaga S, Suzuki H, Oda I, Saito Y. Role of endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) for diagnosis of solid pancreatic masses. Digest Endosc. 2011;23(Suppl 1):29–33.
Oppong KW, Bekkali NLH, Leeds JS, Johnson SJ, Nayar MK, Darne A, Egan M, Bassett P, Haugk B. Fork-tip needle biopsy versus fine-needle aspiration in endoscopic ultrasound-guided sampling of solid pancreatic masses: a randomized crossover study. Endoscopy. 2020;52(6):454–61.
Lai LH, Romagnuolo J, Adams D, Yang J. Primary squamous cell carcinoma of pancreas diagnosed by EUS-FNA: a case report. World J Gastroenterol. 2009;15(34):4343–5.
Soto Iglesias S, Baltar Arias R, Vazquez Rodriguez S, Alvarez M, Gomez Martinez P, Alvarez Sanchez MV, Vazquez Astray E. Virchow’s node as the form of onset of squamous cell carcinoma of the pancreas. Gastroenterol Hepatol. 2009;32(10):693–6.
Nikfam S, Sotoudehmanesh R, Pourshams A, Sadeghipour A, Sotoudeh M, Mohamadnejad M. Squamous cell carcinoma of the pancreas. Arch Iran Med. 2013;16(6):369–70.
Brijbassie A, Stelow E, Shami VM. Squamous cell carcinoma of the pancreas: a case report and review of literature. Gastroenterol Res. 2014;7(3–4):102–4.
Mehta M, Sinha J, Ogawa M, Ganguly A, Xiang D, Poddar N. Unusual case of squamous cell carcinoma of pancreas with review of literature. J Gastrointest Cancer. 2015;46(4):426–9.
Rowe K, Mehta J, Nehme F, Salyers W. Primary squamous cell carcinoma of the pancreas as a cause of biliary obstruction. Cureus. 2016;8(10):e856.
Modi RM, Kamboj AK, Shen R, Krishna SG. Endosonography and confocal endomicroscopy of primary keratinizing squamous cell carcinoma of the pancreas. ACG Case Rep J. 2017;4:e 17.
Martinez de Juan F, Reolid Escribano M, Martinez Lapiedra C, Maiade Alcantara F, Caballero Soto M, Calatrava Fons A, Machado I. Pancreatic adenosquamous carcinoma and intraductal papillary mucinous neoplasm in a CDKN2A germline mutation carrier. World J Gastrointest Oncol. 2017;9(9):390–6.
Kashani A, Kahn M, Jamil LH. Diagnosis of primary squamous cell carcinoma of the pancreas using endoscopic ultrasound-guided core needle biopsy. Gastroenterol Rep. 2015;5(1):72–4.
Zhang G, Cheng ZZ, Xu GH, Jiang X, Wang XX, Wang QF. Primary squamous cell carcinoma of the pancreas with effective comprehensive treatment: a case report and literature review. Medicine. 2018;97(41):12253.
Alajlan BA, Bernadt CT, Kushnir VM. Primary squamous cell carcinoma of the pancreas: a case report and literature review. J Gastrointest Cancer. 2019;50(1):130–3.
Kodavatiganti R, Campbell F, Hashmi A, Gollins SW. Primary squamous cell carcinoma of the pancreas: a case report and review of the literature. J Med Case Rep. 2012;6:295.
Glass R, Andrawes SA, Hamele-Bena D, Tong GX. Metastatic tonsillar squamous cell carcinoma masquerading as a pancreatic cystic tumor and diagnosed by EUS-guided FNA. Diagn Cytopathol. 2017;45(11):1042–5.
Abedi SH, Ahmadzadeh A, Mohammad Alizadeh AH. Pancreatic squamous cell carcinoma. Case Rep Gastroenterol. 2017;11(1):219–24.
De Moura DTH, Coronel M, Chacon DA, Tanigawa R, Chaves DM, Matuguma SE, Dos Santos MEL, Jukemura J, De Moura EGH. Primary adenosquamous cell carcinoma of the pancreas: the use of endoscopic ultrasound guided - fine needle aspiration to establish a definitive cytologic diagnosis. Revista de gastroenterologia del Peru : organo oficial de la Sociedad de Gastroenterologia del Peru. 2017;37(4):370–3.
Machairas N, Paspala A, Schizas D, Ntomi V, Moris D, Tsilimigras DI, Misiakos EP, Machairas A. Metastatic squamous cell carcinoma to the pancreas: report of an extremely rare case. Mol Clin Oncol. 2019;10(1):144–6.
Minami T, Fukui K, Morita Y, Kondo S, Ohmori Y, Kanayama S, Taenaka N, Yoshikawa K, Tsujimura T. A case of squamous cell carcinoma of the pancreas with an initial symptom of tarry stool. J Gastroenterol Hepatol. 2001;16(9):1077–9.
Tella SH, Kommalapati A, Yadav S, Bergquist JR, Truty MJ, Durgin L, Ma WW, Cleary SP, McWilliams RR, Mahipal A. Survival and prognostic factors in patients with pancreatic squamous cell carcinoma. Eur J Surg Oncol. 2019;45(9):1700–5.
Lin E, Veeramachaneni H, Addissie B, Arora A. Squamous cell carcinoma of the pancreas. Am J Med Sci. 2018;355(1):94–6.
Pancreas ESGoCTot: European evidence-based guidelines on pancreatic cystic neoplasms. Gut 2018, 67(5):789–804.
European Study Group on Cystic Tumours of the P. European evidence-based guidelines on pancreatic cystic neoplasms. Gut 2018, 67(5):789–804.
Acknowledgements
We would like to express special gratitude to Professor Qiang Ma for kindly providing pathology knowledge and experience.
Funding
None.
Author information
Authors and Affiliations
Contributions
X.Q., K.Y.M. and J.Z. diagnosed the patient and prepared the manuscript; X.Q. and M.L. prepared the manuscript; and C.T. and M.W. designed and proofread the manuscript. All authors reviewed the final version of the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient ‘s son for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Qiu, X., Meng, Y., Lu, M. et al. Primary squamous cell carcinoma of the pancreas with a large pseudocyst of the pancreas as the first manifestation: a rare case report and literature review. BMC Gastroenterol 21, 208 (2021). https://doi.org/10.1186/s12876-021-01804-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-021-01804-7