Abstract
Background
CMUSE is a rare disease whose diagnosis remains difficult because the lesion is confined to the small bowel.
Case presentation
Here, we present a case of 43-year-old female patient suffered chronic abdominal pain for 20 years, and finally diagnosed with CMUSE. Capsule endoscopy was performed when general endoscopic investigation failed to find the lesion, but the capsule was stranded in the small intestine. Moreover, capsule retention results in acute intestinal obstruction. Thus, surgery was performed and CMUSE was confirmed. The patient was recovered after partial small intestine resection.
Conclusions
Capsule retention occurred in nearly 60% of patients with CMUSE. Capsule endoscopy should be avoided when the patient is suspected of CMUSE, especially with severe anemia and radiologic finding in the ileum.
Similar content being viewed by others
Background
Cryptogenic multifocal ulcerous stenosing enteritis (CMUSE) is a rare disease with unknown etiology and pathophysiology. This disease is an independent entity characterized by chronic and intermittent bouts of moderate ileus resulting from multiple short stenoses of the small bowel with shallow ulcers [1,2,3]. It has been reported in both adults and children but were mainly diagnosed during adulthood with a mean age of approximate 40 years [2, 4,5,6]. The clinical characteristics of CMUSE include abdominal pain and iron-deficiency anemia, moreover, the location of ulcerative strictures was usually located in the ileum [4, 5, 7]. The diagnosis of CMUSE remains difficult because of the unspecific clinical manifestations and vague radiologic findings such as the presence or absence of strictures and superficial ulcers in abdominal computed tomography (CT) or small bowel series (SBS). Thus, small intestine wireless capsule endoscopy (CE) seems to be the best non-invasion inspection of CMUSE. However, capsule retention in the bowel is becoming a common complication of CMUSE should not be neglected.
Case presentation
A 43-year-old woman with remittent abdominal pain, dizziness, and fatigue for 20 years was admitted to our hospital in May 2018. She was also suffered from iron deficiency anemia since her adolescence. There were positive results of stool occult blood test but no evidence of bleeding in gastroscopy and colonoscopy during the progression of the disease. On examination, she had lower limbers edema and mild abdominal tenderness around the umbilicus. Vital signs were within normal range.
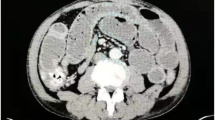
Her past medical history included appendectomy, oophorocystectomy, and caesarean section. She denied NSAIDs taking. Laboratory examination confirmed iron deficiency anemia (hemoglobin level 86 g/L, normal range: 130–175 g/L) and hypoalbuminemia level (14.7 g/L, normal range: 35–55 g/L), C-reaction protein (30.95 mg/L, normal range: 0.08–7.6 mg/L) was elevated. In addition, the fecal occult blood test was positive. Other test results, such as renal and liver functions, autoimmune antibodies, T-spot were within normal range. Meanwhile, colonoscopy and gastroscopy showed normal results. However, abdominal CT scan revealed segmentally thickened small intestinal walls but no mention of stenosis (Fig. 1). Due to the presence of a metal intrauterine device, magnetic resonance (MR) enterography was prohibited. Therefore, CE was used for further inspection. The result found multiple circular ulcerations, and stenoses (Fig. 2). Double balloon endoscopy (DBE) was performed for capsule retained which showed multiple ulcerative stenoses (Fig. 3) but failed to find out the retained capsule. Biopsy report suggested nonspecific moderate chronic inflammation, and villi became widen and shorten. The culture of bacteria or acid-fast stain for tuberculosis were negative. Based on the results above, CMUSE was diagnosed temporarily. The patient received a tentative treatment of methylprednisolone (40 mg/day) and parenteral nutrition and the retained capsule was waiting for discharge by itself.
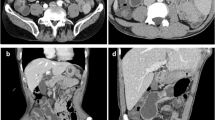
Unfortunately, exploratory laparotomy was performed because of acute intestinal obstruction which may be induced by retained capsule after 2 weeks. During the operation, multiple segmental stenoses of the small intestinal were observed and the endoscopy-capsule was found in the ileum. A section of the small intestine, about 60 cm in length, was removed. There were approximately 26 circumferential superficial ulcers with strictures and the minimal distance between two strictures was about 1.5–3.5 cm (Fig. 4). Postoperative pathology showed superficial ulcerations which limited to the mucosal and submucosal layers (Fig. 5) without granulomas, lymphadenopathy or vasculitis. Finally, CMUSE was diagnosed and she was recovered well after the surgery. Oral steroids were suggested to the patient, but she refused.
Discussion and conclusions
Since Debray et al. [1] reported the first case of CMUSE in 1964, this rare disease has been found in the worldwide region. and Matsumoto et al. [8] call this distinctive entity chronic nonspecific multiple ulcers (CNSU) of the small intestine. However, CNSU is now considered as a different entity called chronic enteropathy associated with SLCO2A1 gene (CEAS) [9]. Moreover, neuromuscular and vascular hamartoma (NMVH) is supposed to be the same disease of CMUSE [10]. The etiology of CMUSE is still unclear, but several hypotheses such as immunopathological pathogenesis [3], excessive formation of fibrous tissue and disturbance of collagen degradation [3, 11], vasculopathy induced by partial C2 deficiency [2, 12], recessive mutations in the PLA2G4A [13] genes had been suspected.
CMUSE is a chronic and recurrent disease. The most common symptoms include abdominal pain, anemia, and gastrointestinal bleeding [4, 5]. Diagnosis of this disease remains difficult due to the lack of specific characteristics and the lesion mainly located in the small bowel. Differential diagnosis of CMUSE includes Crohn’s disease (CD) [14, 15], NSAIDs-induced enteropathy [16], tuberculous enteritis and other chronic infections of the small intestine [17,18,19].
In order to directly observe the lesions in the small intestine, both CE and DBE are viable [20,21,22]. Generally, capsule endoscopy, serve as non-invasive detection, is preferred to use before balloon endoscopy. However, the capsule retention rate of CMUSE patients is extremely high which should not be neglected. After reviewing pieces of literature of CMUSE and some cases in China, 22 patients with CMUSE were performed CE and the presence of capsule retention is also clearly described. Surprisingly, 13 patients underwent capsule retention [3, 5, 10, 14, 17, 23,24,25,26,27,28,29,30]. It means that nearly 60% of patients with CMUSE who receives CE will contribute to retention in the small intestine. Capsule retention has been reported in approximately 1.4% of CE procedures [31]. Even in the patient with known CD, the incidence rate is only about 13% [32].
Capsule retention is a potential disadvantage of intestinal obstruction which may require endoscopic or surgical retrieval of the capsule [33, 34]. Moreover, some capsules will disintegrate in the small bowel [3, 27]. However, the reason why some patients with CMUSE are more likely to undergo capsule retention remains unknown. For further study, a total of 12 patients with CMUSE were finally included in the analysis. Among them, 7 patients have undergone capsule retention and 5 patients have not (Table 1). Based on their clinical characteristics, we found severe anemia and the location of lesion are the main causes of capsule retention. Notably, almost all the patients with capsule retention had some radiologic findings, but unfortunately, those findings were inconspicuous. Therefore, we suggest that patient who is suspected of CMUSE with severe anemia and radiologic findings in the ileum, should avoid using CE which may lead to capsule retention. For these patients, DBE is recommended for further inspection. As the development of patency capsule, we suggest those patients with CMUSE and do not have severe anemia and radiologic findings in the ileum take patency capsule before CE to minimize risk of retention.
As for treatment, the most effective is immunotherapy [2, 3] and surgery. However, the recurrence rate of CMUSE is high [2, 5], and most patients develop corticosteroid dependence. Intriguingly, infliximab (anti-TNF-α therapy) was reported useful in CMUSE [26]. Moreover, gene mutations are closely related to this disease [35], genetic therapy may be effective for this rare disease in the future.
Change history
29 April 2019
Following publication of the original article [1], the author reported the wrong version of Table 1 has been published. The word of 'Capsule' was mistakenly written as 'Capusle'.
Abbreviations
- CD:
-
Crohn’s disease
- CE:
-
Capsule endoscopy
- CEAS:
-
Chronic enteropathy associated with SLCO2A1 gene
- CMUSE:
-
Cryptogenic multifocal ulcerous stenosing enteritis
- CNSU:
-
Chronic nonspecific multiple ulcers
- CT:
-
Computed tomography
- DBE:
-
Double balloon endoscopy
- MR:
-
Magnetic resonance
- NMVH:
-
Neuromuscular and vascular hamartoma
- SBS:
-
Small bowel series
References
Debray C, Besancon F, Hardouin JP, Martin E, Marche C, Khoury K. Cryptogenetic Plurifocal ulcerative Stenosing enteritis. Arch Mal Appar Dig Mal Nutr. 1964;53:193–206.
Perlemuter G, Guillevin L, Legman P, Weiss L, Couturier D, Chaussade S. Cryptogenetic multifocal ulcerous stenosing enteritis: an atypical type of vasculitis or a disease mimicking vasculitis. Gut. 2001;48(3):333–8.
Kohoutova D, Bures J, Tycova V, Bartova J, Tacheci I, Rejchrt S, et al. Severe cryptogenic multifocal ulcerous stenosing enteritis. A report of three cases and review of the literature. Acta Med (Hradec Kralove). 2010;53(1):25–9.
Chung SH, Park SU, Cheon JH, Kim ER, Byeon JS, Ye BD, et al. Clinical characteristics and treatment outcomes of cryptogenic multifocal ulcerous Stenosing enteritis in Korea. Dig Dis Sci. 2015;60(9):2740–5.
Hwang J, Kim JS, Kim AY, Lim JS, Kim SH, Kim MJ, et al. Cryptogenic multifocal ulcerous stenosing enteritis: radiologic features and clinical behavior. World J Gastroenterol. 2017;23(25):4615–23.
Ooms H, De Schepper HU, Moreels TG. Case series of cryptogenic multifocal ulcerating Stenosing enteritis (CMUSE). Acta Gastroenterol Belg. 2017;80(3):361–4.
Kohoutova D, Bartova J, Tacheci I, Rejchrt S, Repak R, Kopacova M, et al. Cryptogenic multifocal ulcerous stenosing enteritis: a review of the literature. Gastroenterol Res Pract. 2013;2013:918031.
Matsumoto T, Iida M, Matsui T, Yao T. Chronic nonspecific multiple ulcers of the small intestine: a proposal of the entity from Japanese gastroenterologists to Western enteroscopists. Gastrointest Endosc 2007;66(3 Suppl):S99–107.
Umeno J, Esaki M, Hirano A, Fuyuno Y, Ohmiya N, Yasukawa S, et al. Clinical features of chronic enteropathy associated with SLCO2A1 gene: a new entity clinically distinct from Crohn's disease. J Gastroenterol. 2018;53(8):907–15.
Setaffy L, Osuna MJ, Plieschnegger W, del Pino Florez Rial M, Geboes K, Langner C. Cryptogenic multifocal ulcerous stenosing enteritis (CMUSE), and neuromuscular and vascular hamartoma (NMVH): two sides of the same coin. Endoscopy. 2015;47(4):345–8.
Vozenin-Brotons MC, Milliat F, Sabourin JC, de Gouville AC, Francois A, Lasser P, et al. Fibrogenic signals in patients with radiation enteritis are associated with increased connective tissue growth factor expression. Int J Radiat Oncol Biol Phys. 2003;56(2):561–72.
Perlemuter G, Chaussade S, Soubrane O, Degoy A, Louvel A, Barbet P, et al. Multifocal stenosing ulcerations of the small intestine revealing vasculitis associated with C2 deficiency. Gastroenterology. 1996;110(5):1628–32.
Brooke MA, Longhurst HJ, Plagnol V, Kirkby NS, Mitchell JA, Ruschendorf F, et al. Cryptogenic multifocal ulcerating stenosing enteritis associated with homozygous deletion mutations in cytosolic phospholipase A2-alpha. Gut. 2014;63(1):96–104.
Zhang Y, Huang L, Liu R, Wang M, Jiang Z, Zhou W, et al. Case report of a pair of siblings with cryptogenic multifocal ulcerating stenosing enteritis: a rare disease easily to be misdiagnosed as Crohn disease. Medicine (Baltimore). 2017;96(32):e7527.
Hosoe N, Ohmiya N, Hirai F, Umeno J, Esaki M, Yamagami H, et al. Chronic enteropathy associated with SLCO2A1 gene [CEAS]-characterisation of an enteric disorder to be considered in the differential diagnosis of Crohn's disease. J Crohns Colitis. 2017;11(10):1277–81.
Chung SH, Jo Y, Ryu SR, Ahn SB, Son BK, Kim SH, et al. Diaphragm disease compared with cryptogenic multifocal ulcerous stenosing enteritis. World J Gastroenterol. 2011;17(23):2873–6.
Chang DK, Kim JJ, Choi H, Eun CS, Han DS, Byeon JS, et al. Double balloon endoscopy in small intestinal Crohn's disease and other inflammatory diseases such as cryptogenic multifocal ulcerous stenosing enteritis (CMUSE). Gastrointest Endosc. 2007;66(3 Suppl):S96–8.
Chamberlain RS, Atkins S, Saini N, White JC. Ileal perforation caused by cytomegalovirus infection in a critically ill adult. J Clin Gastroenterol. 2000;30(4):432–5.
Hayashi K, Horie Y, Takahata H, Adachi Y, Kitamura Y, Kato M. Ileal ulcers and cytomegalovirus infection in a case of Churg-Strauss syndrome. Arch Pathol Lab Med. 2005;129(6):e141–3.
Iddan G, Meron G, Glukhovsky A, Swain P. Wireless capsule endoscopy. Nature. 2000;405(6785):417.
Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, et al. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53(2):216–20.
May A, Nachbar L, Wardak A, Yamamoto H, Ell C. Double-balloon enteroscopy: preliminary experience in patients with obscure gastrointestinal bleeding or chronic abdominal pain. Endoscopy. 2003;35(12):985–91.
Yang Y, Zhao L, Zhang Y. A steroid-resistant cryptogenic multifocal ulcerous stenosing enteritis. Niger J Clin Pract. 2018;21(5):678–80.
Kijmassuwan T, Tanpowpong P, Molagool S, Treepongkaruna S. A rare cause of multiple small bowel ulcers and strictures in a 10-year-old child. Turk J Gastroenterol. 2018;29(1):112–5.
Singh A, Sahu MK, Panigrahi MK, Misra D. Cryptogenic multifocal ulcerous Stenosing enteritis (CMUSE): a tale of three decades. ACG Case Rep J. 2017;4:e44.
De Schepper H, Macken E, Van Marck V, Spinhoven M, Pelckmans P, Moreels T. Infliximab induces remission in cryptogenic multifocal ulcerous stenosing enteritis: first case. World J Gastroenterol. 2013;19(10):1661–4.
Tacheci I, Ryska A, Rejchrt S, Kopacova M, Horava V, Bures J. Spontaneous disintegration of a retained video capsule in a patient with cryptogenic multifocal ulcerous stenosing enteritis: a rare complication. Endoscopy. 2008;40(Suppl 2):E104–5.
Kwon SO, Kim YS, Kim SY, Hong SW, Lee HK, Moon JS. A case of cryptogenic multifocal ulcerous stenosing enteritis: differential diagnosis from Crohn's disease. J Gastrointestin Liver Dis. 2012;21(3):309–12.
Fraile G, Norman F, Reguero ME, Defargues V, Redondo C. Cryptogenic multifocal ulcerous stenosing enteritis (CMUSE) in a man with a diagnosis of X-linked reticulate pigmentary disorder (PDR). Scand J Gastroenterol. 2008;43(4):506–10.
Guisado Vasco P, Fraile Rodriguez G. Cryptogenia multifocal ulcerous stenosing enteritis: an entity on its own as a cause of abdominal pain, iron deficiency anemia and protein-losing enteropathy. Revista clinica espanola. 2014;214(1):26–30.
Enns RA, Hookey L, Armstrong D, Bernstein CN, Heitman SJ, Teshima C, et al. Clinical practice guidelines for the use of video capsule endoscopy. Gastroenterology. 2017;152(3):497–514.
Cheifetz AS, Kornbluth AA, Legnani P, Schmelkin I, Brown A, Lichtiger S, et al. The risk of retention of the capsule endoscope in patients with known or suspected Crohn's disease. Am J Gastroenterol. 2006;101(10):2218–22.
Rondonotti E, Soncini M, Girelli C, Ballardini G, Bianchi G, Brunati S, et al. Small bowel capsule endoscopy in clinical practice: a multicenter 7-year survey. Eur J Gastroenterol Hepatol. 2010;22(11):1380–6.
Baichi MM, Arifuddin RM, Mantry PS. Small-bowel masses found and missed on capsule endoscopy for obscure bleeding. Scand J Gastroenterol. 2007;42(9):1127–32.
Umeno J, Matsumoto T, Hirano A, Fuyuno Y, Esaki M. Genetic analysis is helpful for the diagnosis of small bowel ulceration. World J Gastroenterol. 2018;24(28):3198–200.
Acknowledgements
Not applicable.
Funding
Not applicable.
Availability of data and materials
All the data supporting the conclusions of this article are included within the published article and its additional files.
Author information
Authors and Affiliations
Contributions
THZ, YFW, JTT, YXC, and QYG carried out the clinical diagnosis, provided the clinical details and participated in designing the report. EWT and QYG drafted the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor in Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional information
The original version of this article was revised: the author reported the wrong version of Table 1 has been published.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tao, EW., Zou, TH., Wang, YF. et al. Case report of cryptogenic multifocal ulcerous stenosing enteritis (CMUSE): a rare disease may contribute to endoscopy-capsule retention in the small intestine. BMC Gastroenterol 19, 49 (2019). https://doi.org/10.1186/s12876-019-0962-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-019-0962-8