Abstract
Background
In metastatic colorectal cancer, the location of the primary tumor has been suggested to have biological significance. In this study, we investigated whether primary tumor location affects cetuximab efficacy in patients with RAS wild-type metastatic colorectal cancer.
Methods
Genotyping by the SequenomMassARRAY technology platform (OncoMap) targeting KRAS, NRAS, PIK3CA, and BRAF was performed in tumors from 307 patients who had been given cetuximab as salvage treatment. Tumors with mutated RAS (KRAS or NRAS; n = 127) and those with multiple primary location (n = 10) were excluded. Right colon cancer was defined as a tumor located in the proximal part to splenic flexure.
Results
A total of 170 patients were included in the study (right versus left, 23 and 147, respectively). Patients with right colon cancer showed more mutated BRAF (39.1% vs. 5.4%), mutated PIK3CA (13% vs. 1.4%), poorly differentiated tumor (17.4% vs. 3.4%), and peritoneal involvement (26.1% vs. 8.8%) than those with left colon and rectal cancer. Right colon cancer showed poorer progression-free survival (2.0 vs.5.0 months, P = 0.002) and overall survival (4.1 months and 13.0 months, P < 0.001) than the left colon and rectal cancer. By multivariable analysis, BRAF mutation, right colon primary, poorly differentiated histology, and peritoneal involvement were associated with risk of death.
Conclusions
In RAS wild-type colon cancer treated with cetuximab as salvage treatment, right colon primary was associated with poorer survival outcomes than left colon and rectal cancer.
Similar content being viewed by others
Background
Colorectal cancer (CRC) represents 10% of cancer incidence globally, and it is the fourth leading cause of cancer-related deaths worldwide. South Korea has one of the highest incidences of CRC in the world [1]. The survival of metastatic CRC has gradually been improved with advancements in medical therapy, which include not only the development of new drugs but also the discovery of predictive biomarkers.
Previous studies have suggested that primary tumor location (PTL) may be a surrogate for tumor biology that may affect treatment outcomes [2, 3]. In terms of embryology and molecular carcinogenesis, CRC can be divided into distinct disease entities according to the PTL; the right side of the colon, including the cecum, the ascending colon, and the transverse colon is derived from the midgut, while the remaining parts of the colon and rectum come from the hindgut [2]. Tumors of the right colon (RC) tend to more frequently exhibit a poorly differentiated histology, BRAF mutation, a hypermethylated phenotype, and microsatellite instability (MSI), while c-MYC expression occurs more commonly in tumors of left colon and rectum(LC) than in those in the RC [2, 4, 5].
The prognostic and predictive implications of PTL have been addressed in numerous studies, but there is no clear consensus on the role of PTL in treatment decisions. Generally, RC cancer is associated with poorer survival compared to LC cancer [6, 7], and recent evidences have shown that patients with RC cancer may respond poorly to anti-epidermal growth factor receptor (EGFR) antibodies, such as cetuximab or panitumumab, which are the backbone of treatment for metastatic CRC [8, 9]. However, the predictive value of PTL should be analyzed in consideration of RAS mutation,the most powerful predictor of response of anti-EGFR antibodies [10, 11].
In our current study, we investigated the association between PTL and clinical outcomes in RAS wild-type metastatic CRC patients who received cetuximab as a salvage treatment.
Methods
Patients
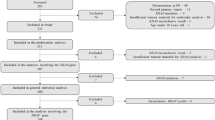
We retrospectively reviewed the medical records of 307 metastatic CRC patients treated with cetuximab with or without irinotecan as a salvage treatment between December 2003 and June 2013 at Asan Medical Center, Seoul, Republic of Korea. All of them were given cetuximab as a third or later line of treatment for metastatic CRC and had sufficient tissue to conduct extended RAS analyses. After extended RAS testing, 127 RAS mutant patients were excluded from the analysis, and additional 10 patients with synchronous multiple colon cancers were excluded due to an inability to define PTL. Finally, 170 patients were analyzed and assigned to either RC or LC group (Fig. 1). Clinicopathologic variables, including age, gender, initial stage, histologic differentiation, metastatic sites, MSI status (determined as previously described [12] by the Bethesda panel), and details of treatment given before cetuximab were extracted from medical records. This study was conducted in accordance with the declaration of Helsinki and was approved by the Institutional Review Board of Asan Medical Center. Informed consent was obtained in all participants except patients who were dead at the time of this study. Institutional Review Board of Asan Medical Center approved to waive the requirement to obtain informed consent from the dead according to Bioethics and Biosafety Act in Korea.
Genotyping
Mutational analysis was done using the SequenomMassARRAY technology platform (OncoMap version 4.0), as previously described [13, 14]. A pathologist (JK) reviewed formalin-fixed paraffin-embedded tissue and marked tumor portions, where DNA was extracted from using the QIAamp DNA Tissue kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions. Multiplex polymerase chain reaction amplification using iPLEXchemistry (#10134–2; Sequenom, San Diego, CA), and homogenous mass extension validation of mutation were implemented. Single-base extension was done and a MALDI-TOF mass spectrometer was used to determine the unique mass value according to the mutation site. Target genes were KRAS (exon 2, 3, and 4), NRAS (exon 2, 3, and 4), PIK3CA (exon 9 and 20), and BRAF (exon 15).
Tumor locations
The tumor location was determined based on operation records and colonoscopy findings. The RC group consisted of cancers occurring in the cecum, the ascending colon, hepatic flexure, and the transverse colon, while the LC group included primary tumors from the splenic flexure to the rectum.
Statistical analysis
The statistical tests were exploratory in nature. Demographic and baseline clinical characteristics were compared according to the PTL. Fisher’s exact test and the Mann–Whitney U-test were used for categorical variables and continuous variables, respectively. The Kaplan–Meier method was used to estimate progression-free survival (PFS) and overall survival (OS), and the survival outcomes were compared according to PTL by the log-rank test. PFS was defined as the time from the date of the first administration of cetuximab to the date of documented disease progression or the date of death from any cause, if progression was not documented before death. OS was defined as the time from the date of first cetuximab dose to the date of death from any cause. To evaluate clinical outcomes by PTL, the Cox proportional hazards regression model was used for multivariable analysis. In these analyses, we selected statistically significant or clinically meaningful variables as predictors for the final model. Thus, PFS and OS were adjusted for age, sex, presence of peritoneal seeding, histologic grade, and BRAF mutational status. Hazard ratio (HR) associated with each variable was suggested with 95% confidence interval (CI). All statistical analyses were two-sided, with a level of significance established at p < 0.05, and performed using the Statistical Package for Social Sciences version 21.0 (IBM Corp., Armonk, NY). The Kaplan–Meier curves were drawn using STATA software (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP).
Role of the funding source
The study funders had no role in the design, analysis, interpretation or manuscript preparation. All authors prepared the drafts of this report and approved the submission. The corresponding author had full access to all the data and final responsibility to submit for publication.
Results
Patient characteristics
Among a total of 170 RAS wild-type patients, 23 were classified as belonging to the RC group and 147 as belonging to the LC group (Fig. 1). The baseline characteristics of the study patients are presented in Table 1. All patients were treated with cetuximab as third or later-line therapy, and half of them received it in combination with irinotecan. All patients were treated with irinotecan before cetuximab; no significant difference was seen in previously exposed chemotherapeutic agents (oxaliplatin, fluoropyrimidine, and bevacizumab). The median age was similar between the groups, while the proportion of female patients was higher in the RC group, without statistical significance. The most common metastatic organ was liver in both groups, while peritoneal metastasis was more common in RC cancer than in LC cancer (26.1% vs. 8.8%, p = 0.026). The proportion of unfavorable histology, including poorly differentiated adenocarcinoma and signet ring cell carcinoma, was 20.0% in RC and 5.0% in LC (p = 0.031). The interval between first-line chemotherapy and cetuximab treatment was slightly shorter in the RC group than the LC group, without statistical significance (16.4 vs. 18.2 months, p = 0.552).
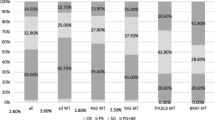
Molecular information according to PTL
The results of genotyping are summarized in Table 1. The BRAF V600E mutation was detected in nine (39.1%) patients in the RC group and eight (5.4%) in the LC group. The PIK3CA mutation was also more frequently detected in the RC group (13% vs. 1.4%, p = 0.018). The MSI test is not routinely performed for metastatic CRC in our institution, so information for MSI status was only available for 108 patients (63.5%), among whom only 1 patient, in the LC group, had an MSI-high tumor.
Clinical outcomes by primary tumor location
A profound difference in OS according to PTL was observed: 4.1 months (95% CI, 2.1 to 8.1) in the RC group and 13.0 months (95% CI 11.5 to 14.0) in the LC group (p < 0.001) (Fig. 2a). The PFS was also poorer in the RC group (2.0 months, 95% CI 0.9 to 4.0) than in the LC group (5.0 months, 95% CI 4.5 to 6.3, p = 0.002) (Fig. 2b).
BRAF mutation was significantly associated with poor clinical outcome: OS in BRAF wild-type and mutants were 13.0 months and 4.1 months (p < 0.0001), respectively. PFS was 5.1 months in BRAF wild-type, and 1.2 months in BRAF mutants (p < 0.0001).
Within the RAS and BRAF wild-type population (n = 153, 14 in RC group and 139 in LC group), OS was still poorer in the RC group than in the LC group (5.7 months vs. 13.2 months, respectively), with marginal significance (p = 0.055, Fig. 2c). PFS did not significantly differ between the two groups when BRAF mutants were excluded (3.7 months in RC group vs. 5.3 months in LC group, p = 0.219; Fig. 2d).
The presence of peritoneal metastasis, BRAF mutation, unfavorable histology (poorly differentiated adenocarcinoma or signet ring cell carcinoma), and PTL were statistically meaningful parameters in bivariate analysis for OS and PFS using the Cox proportional hazard model (Tables 2 and 3). By multivariable analysis, RC was associated with a poorer OS (hazards ratio 1.84, 95% CI 1.10 to 3.09, p = 0.021, Table 2), and there was a trend toward a lower PFS (HR 1.55, 95% CI 0.92 to 2.61, p = 0.099, Table 3).
Discussion
We observed in our current analysis that RC was associated with poor OS and PFS outcomes in RAS wild-type metastatic CRC patients treated with cetuximab as salvage therapy. OS was still poorer in the RC group when BRAF mutants were excluded. These findings suggest that PTL may be a factor in deciding on salvage chemotherapy with cetuximab in RAS wild-type patients.
Several studies have suggested that clinical benefits from anti-EGFR treatment may differ according to PTL. In data from a phase II trial of cetuximab-based chemotherapy, LC cancer was found to be associated with significantly longer PFS and OS than RC cancer in KRAS exon 2 wild-type patients [9]. Similarly, the NCIC CO.17 trial, a phase III study that compared cetuximab with the best supportive care in refractory metastatic CRC, showed that patients with LC cancer had benefit from cetuximab in terms of PFS, but those with RC cancer did not in KRAS exon 2 wild-type population [8]. Post-hoc analysis of the CALGB 80405 trial, a phase III trial that compared cetuximab and bevacizumab in front-line settings, also showed that cetuximab-treated KRAS exon 2 wild-type patients with RC cancer had markedly poorer survival than those with LC cancer (16.7 months in RC and 36.0 in LC, p < 0.0001) [15]. All of these analyses were performed in KRAS exon 2 wild-type patients, so the possibility that RAS mutations other than KRAS exon 2 may have contributed to the relatively poorer outcome in RC cancer in these studies could not be excluded. Recent studies for RAS wild-type subgroup of randomized trials which compared anti-EGFR treatment with chemotherapy +/− bevacizumab addressed this issue, by showing OS, PFS and objective response rate with anti-EGFR treatment was poorer in RC cancer than in LC cancer [16, 17].
A strength of our present study is that we excluded all RAS mutants from our analysis using a highly sensitive high-throughput method, the SequenomMassARRAY system. Our previous study showed that this method was more helpful for selecting candidates for cetuximab treatment than less-sensitive Sanger sequencing [14]. This means that the poorer outcomes with anti-EGFR treatment in RC cancer than in LC cancer were maintained even after all RAS mutants with low-allele frequency were excluded.
We further found in our analysis that BRAF and PIK3CA mutants were enriched in RC cancer, as shown in previous studies [5], which may partly explain the different therapeutic effects of anti-EGFR according to the PTL. However, the difference in OS was still retained, even after excluding BRAF mutants. Although we should be careful interpreting this subset analysis due to small sample size and relatively low proportion of RC (in RAS and BRAF wild-type subgroup, n = 14 for RC compared to n = 139 in LC), PTL may be associated with poor prognostic biological features other than RAS or BRAF mutation. The prognostic impact of PTL irrespective of RAS and BRAF mutation was also suggested by subgroup analyses of 3 randomized trials on anti-EGFR vs. chemotherapy +/− bevacizumab (FIRE3, PRIME, and PEAK), which showed poor prognosis of RC in patients with RAS/BRAF wild-type metastatic CRC [18, 19].
Recent studies have suggested that biologic features of RC cancer that may explain the poor prognosis or resistance to anti-EGFR treatment. A translational study in PETACC-3 trial reported that BRAF-mutant-like tumors, which were BRAF wild-type but shared similar gene expression profile with BRAF mutant tumors, were enriched in RC and had poor prognosis [20]. The abundant expression of epiregulin and amphiregulin, which are known to be predictors of good response to anti-EGFR treatment, was shown to be more prevalent in LC cancer than in RC cancer [21]. On the other hand, MiR-31-3p, a poor predictor for anti-EGFR response, was shown to be overexpressed more frequently in RC cancer than in LC cancer [22]. In addition, Consensus Molecular Subtype (CMS)1, which is associated with a poorer survival rate after relapse, is more common in RC [23]. However, there might be more unknown features of biologic relevance of PTL, since recent translational study from CALGB 80405 showed PTL was independent prognostic factor when adjusted to BRAF mutation, MSI and CMS [24].
It is uncertain whether PTL is just a negative prognostic indicator reflecting tumor biology irrespective of treatment or is a genuine predictive marker of the response to anti-EGFR treatment. In CALGB 80405 trial, the OS was better in LC than in RC cancer in bevacizumab-treated patients, although the interaction between the PTL and the treatment (cetuximab versus bevacizumab) was significant (p = 0.005) [15]. This prognostic as well as predictive impact of PTL was consistently shown by the pooled analysis of 6 randomized trials (5 in first-line and 1 in second-line setting) on anti-EGFR in terms of OS and PFS although the interaction between sidedness and treatment effect was not always significant in all of the trials [16]. However, in NCIC CO.17 study, a randomized study in chemo-refractory setting, PFS and OS in the best supportive care arm was not affected by PTL, implying that it was not prognostic, but only predictive of PFS benefit from cetuximab (interaction p = 0.002) [8]. To date, collective evidences are suggesting high likelihood of no clinical benefit from anti-EGFR in RC cancer, at least in first-line setting, and possibly in later-line treatment. PTL seems to be also prognostic for metastatic CRC in first-line setting, but unclear in chemo-refractory patients.
In our current study, PTL showed a significant relationship with OS in multivariable analysis, but not in PFS; the prognostic impact of PTL seems to be more prominent than the predictive role in these results. However, the limitations of our present analysis hamper such an interpretation; the sample size of our patients with RC cancer was too small and we did not include a control group without cetuximab. Thus, it was difficult to conclude whether PTL is purely prognostic or predictive from our present study.
The characteristics of our study patients were comparable to those of previous reports, namely frequent poorly differentiated histology and peritoneal seeding, as well as the mutation profile previously mentioned [2, 6, 25]. However, the proportion of RC patients in our study population was relatively too small (13.5%, 23/170) to have adequate power of comparison according to PTL. This probably resides in the low proportion of proximal colon cancer in Korean populations: 18.6% in male and 24.2% in female according to 2009 statistics from national registry [26]. This is consistent with the racial difference in subsite-specific CRC incidence in United States; Asia-Pacific islanders had lowest proportion of proximal colon cancer (28% in male, 34% in female) compared to other racial groups (usually ≥40%) [27]. The association of racial difference in subsite distribution and prognosis according to treatment warrants further investigation.
Our current study had other limitations, including its retrospective nature, the heterogeneous regimen of cetuximab, insufficient information on MSI, and the lack of biological information other than hotspot mutation profiles, such as gene expression or the CpG island methylation profile.
Conclusions
PTL in RC might be associated with a poor OS outcome in patients with RAS wild-type metastatic CRC being treated with cetuximab as salvage treatment. Despite of the limitations from the retrospective study of small sample size, this finding supports the conclusions of previous studies that PTL may be a surrogate for tumor biology and should be considered as a biomarker and as a stratification factor in conducting clinical trials. Further studies are needed to validate the impact of PTL on treatment outcomes in various clinical settings.
Abbreviations
- CI:
-
Confidence interval
- CRC:
-
Colorectal cancer
- EGFR:
-
Epidermal growth factor receptor
- HR:
-
Hazard ratio
- LC:
-
Left colon and rectum
- MSI:
-
Microsatellite instability
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- PTL:
-
Primary tumor location
- RC:
-
Right colon
References
GLOBOCAN. 2012: estimated cancer incidence, mortality and prevalence worldwide in 2012. International Agency for Research on Cancer: Lyon; 2015.
Lee GH, Malietzis G, Askari A, Bernardo D, Al-Hassi HO, Clark SK. Is right-sided colon cancer different to left-sided colorectal cancer? - a systematic review. Eur J Surg Oncol. 2015;41(3):300–8.
Yahagi M, Okabayashi K, Hasegawa H, Tsuruta M, Kitagawa Y. The worse prognosis of right-sided compared with left-sided colon cancers: a systematic review and meta-analysis. J Gastrointest Surg. 2016;20(3):648–55.
Rothberg PG, Spandorfer JM, Erisman MD, Staroscik RN, Sears HF, Petersen RO, Astrin SM. Evidence that c-myc expression defines two genetically distinct forms of colorectal adenocarcinoma. Br J Cancer. 1985;52(4):629–32.
Shen H, Yang J, Huang Q, Jiang MJ, Tan YN, JF F, Zhu LZ, Fang XF, Yuan Y. Different treatment strategies and molecular features between right-sided and left-sided colon cancers. World J Gastroenterol. 2015;21(21):6470–8.
Benedix F, Kube R, Meyer F, Schmidt U, Gastinger I, Lippert H. Comparison of 17,641 patients with right- and left-sided colon cancer: differences in epidemiology, perioperative course, histology, and survival. Dis Colon rectum. 2010;53(1):57–64.
Meguid RA, Slidell MB, Wolfgang CL, Chang DC, Ahuja N. Is there a difference in survival between right- versus left-sided colon cancers? Ann Surg Oncol. 2008;15(9):2388–94.
Brule SY, Jonker DJ, Karapetis CS, O'Callaghan CJ, Moore MJ, Wong R, Tebbutt NC, Underhill C, Yip D, Zalcberg JR, et al. Location of colon cancer (right-sided versus left-sided) as a prognostic factor and a predictor of benefit from cetuximab in NCIC CO.17. European journal of cancer (Oxford, England : 1990). 2015;51(11):1405–14.
von Einem JC, Heinemann V, von Weikersthal LF, Vehling-Kaiser U, Stauch M, Hass HG, Decker T, Klein S, Held S, Jung A, et al. Left-sided primary tumors are associated with favorable prognosis in patients with KRAS codon 12/13 wild-type metastatic colorectal cancer treated with cetuximab plus chemotherapy: an analysis of the AIO KRK-0104 trial. J Cancer Res Clin Oncol. 2014;140(9):1607–14.
Douillard JY, Oliner KS, Siena S, Tabernero J, Burkes R, Barugel M, Humblet Y, Bodoky G, Cunningham D, Jassem J, et al. Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N Engl J Med. 2013;369(11):1023–34.
Sorich MJ, Wiese MD, Rowland A, Kichenadasse G, McKinnon RA, Karapetis CS, Extended RAS. Mutations and anti-EGFR monoclonal antibody survival benefit in metastatic colorectal cancer: a meta-analysis of randomized, controlled trials. Ann Oncol. 2015;26(1):13–21.
Kim JE, Hong YS, Ryu MH, Lee JL, Chang HM, Lim SB, Kim JH, Jang SJ, Kim MJ, CS Y, et al. Association between deficient mismatch repair system and efficacy to irinotecan-containing chemotherapy in metastatic colon cancer. Cancer Sci. 2011;102(9):1706–11.
Kim YM, Lee SW, Chun SM, Kim DY, Kim JH, Kim KR, Kim YT, Nam JH, van Hummelen P, MacConaill LE, et al. Analysis and comparison of somatic mutations in paired primary and recurrent epithelial ovarian cancer samples. PLoS One. 2014;9(6):e99451.
Kim D, Hong YS, Kim JE, Kim KP, Lee JL, Chun SM, Kim J, Jang SJ, Kim TW. Use of a high-throughput genotyping platform (OncoMap) for RAS mutational analysis to predict Cetuximab efficacy in patients with metastatic colorectal cancer. Cancer Res Treat. 2016;49(1):37–43.
Venook AP, Niedzwiecki D, Innocenti F, Fruth B, Greene C, O'Neil BH, Shaw JE, Atkins JN, Horvath LE, Polite BN, et al. Impact of primary tumor location on overall survival (OS) and progression-free survival (PFS) in patients (pts) with metastatic colorectal cancer (mCRC): Analysis of CALGB/SWOG 80405 (Alliance). J Clin Oncol. 2016;34 Suppl:3504-3504.
Arnold D, Lueza B, Douillard JY, Peeters M, Lenz HJ, Venook A, Heinemann V, Van Cutsem E, Pignon JP, Tabernero J, et al. Prognostic and predictive value of primary tumour side in patients with RAS wild-type metastatic colorectal cancer treated with chemotherapy and EGFR directed antibodies in six randomised trials. Ann Oncol. 2017;28(8):1713–29.
Tejpar S, Stintzing S, Ciardiello F, et al. Prognostic and predictive relevance of primary tumor location in patients with ras wild-type metastatic colorectal cancer: retrospective analyses of the crystal and fire-3 trials. JAMA oncology. 2017;3(2):194–201.
Peeters M: Outcome according to Left vs. Right side in the Panitumumab studies. In: ESMO 2016 Congress.
Heinemann V: Outcome according to Left vs. Right side in the FOLFIRI Cetuximab and FIRE 3 study. In: ESMO 2016 Congress.
Popovici V, Budinska E, Tejpar S, Weinrich S, Estrella H, Hodgson G, Van Cutsem E, Xie T, Bosman FT, Roth AD, et al. Identification of a poor-prognosis BRAF-mutant-like population of patients with colon cancer. J Clin Oncol. 2012;30(12):1288–95.
Seligmann JF, Elliott F, Richman SD, Jacobs B, Hemmings G, Brown S, Barrett JH, Tejpar S, Quirke P, Seymour MT. Combined Epiregulin and Amphiregulin expression levels as a predictive biomarker for Panitumumab therapy benefit or lack of benefit in patients with RAS wild-type advanced colorectal cancer. JAMA Oncol. 2016;2(5):633–42.
Laurent-Puig P, Grisoni ML, Heinemann V, Fontaine K, Vazart C, Decaulne V, Rousseau F, Courtieu B, Lieabert F, Jung A et al.: MiR-31-3p is a predictive biomarker of cetuximab response in FIRE3 clinical trial. Ann Oncol 2016, 27(suppl_6):457O-457O.
Guinney J, Dienstmann R, Wang X, de Reynies A, Schlicker A, Soneson C, Marisa L, Roepman P, Nyamundanda G, Angelino P, et al. The consensus molecular subtypes of colorectal cancer. Nat Med. 2015;21(11):1350–6.
Venook AP, Ou F-S, Lenz H-J, Kabbarah O, Qu X, Niedzwiecki D, Zemla T, Goldberg RM, Hochster HS, O'Neil BH. Primary (1°) tumor location as an independent prognostic marker from molecular features for overall survival (OS) in patients (pts) with metastatic colorectal cancer (mCRC): Analysis of CALGB/SWOG 80405 (Alliance). J Clin Oncol. 2017;35 Suppl:3503-3503.
Yamauchi M, Morikawa T, Kuchiba A, Imamura Y, Qian ZR, Nishihara R, Liao X, Waldron L, Hoshida Y, Huttenhower C, et al. Assessment of colorectal cancer molecular features along bowel subsites challenges the conception of distinct dichotomy of proximal versus distal colorectum. Gut. 2012;61(6):847–54.
Shin A, Kim KZ, Jung KW, Park S, Won YJ, Kim J, Kim DY, JH O. Increasing trend of colorectal cancer incidence in Korea, 1999-2009. Cancer research and treatment : official journal of Korean Cancer Association. 2012;44(4):219–26.
Wu X, Chen VW, Martin J, Roffers S, Groves FD, Correa CN, Hamilton-Byrd E, Jemal A. Subsite-specific colorectal cancer incidence rates and stage distributions among Asians and Pacific islanders in the United States, 1995 to 1999. Cancer Epidemiol Biomarkers Prev. 2004;13(7):1215–22.
Acknowledgments
Not applicable.
Funding
This study was funded by the National R&D Program for Cancer Control, Ministry of Health and Welfare, Republic of Korea (1420030), and the Asan Institute for Life Sciences, Seoul, Republic of Korea (2016–0735), and was supported in part by CJ HealthCare, Corp, Seoul, Korea.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
DK, SYK, YSH, JEK, KK, YY and TWK contributed conception and design of this study. DK and SYK contributed to clinical data acquisition and manuscript drafting. DK, SYK and JSL contributed to statistical analysis. JK and SJJ contributed to genomic data acquisition. All the authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the declaration of Helsinki and was approved by the Institutional Review Board of Asan Medical Center.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kim, D., Kim, S.Y., Lee, J.S. et al. Primary tumor location predicts poor clinical outcome with cetuximab in RAS wild-type metastatic colorectal cancer. BMC Gastroenterol 17, 121 (2017). https://doi.org/10.1186/s12876-017-0694-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-017-0694-6