Abstract
Background
Guidelines worldwide recommend that physicians should not treat their family members. However, studies in the U.S. have shown that approximately 74–83% of physicians have experience of treating family members. Primary care physicians were more likely to have such experiences than other specialists. In Japan, physicians do not have any guidelines regarding treating family members, and little is known about the experiences of primary care physicians. Therefore, we investigated the experience of treating family members or relatives among primary care physicians in Japan.
Methods
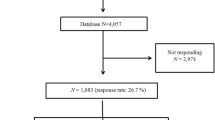
This cross-sectional study used an online questionnaire. We recruited 2,000 physicians who were members of the Japan Primary Care Association using random sampling. Data were collected from February 10 to March 10, 2021. We compare the experiences of treating family members between clinic-based doctors and hospital-based doctors using the chi-square test. We performed logistic regression analysis to adjust for gender, age, presence of a doctor in family, and physician’s geographic location (rural or not rural).
Results
A total of 466 physicians (response rate = 23.3%) completed the survey. Of the sample, 79.8% had experience of treating family members or relatives. In the univariate analysis, being a clinic-based physician was associated with experience in treating family members compared to hospital-based physicians (87.6% vs. 74.9%, p = 0.001). Multivariable analysis showed that being a clinic-based physician (odds ratio 2.30, 95% confidence interval 1.31–4.04) and age of 45–64 years (odds ratio 2.93, 95% confidence interval 1.74–4.93) were significantly related to experience treating family. Gender and geographic location were not statistically significant factors.
Conclusions
A high percentage of Japanese primary care physicians, especially those who worked in clinics, reported experience treating family members or relatives. These findings will serve as basic data for future studies regarding the care of families and relatives of physicians in Japan.
Similar content being viewed by others
Background
For physicians, providing medical care to family members and relatives raises ethical and clinical issues [1, 2]. The reasons are a possible lack of objectivity, potential failure to ask about sensitive topics or to perform intimate examinations, risk of practicing outside the scope of training, over testing, and inappropriate prescribing [1,2,3,4]. The American Medical Association Code of Medical Ethics guidelines state that “In general, physicians should not treat themselves or members of their own families [3].” Similarly, the American College of Physicians recommends not entering into dual relationships, referring to patient-physician relationships and family-physician relationships [4]. The Canadian Medical Association asks physicians to limit the treatment of their immediate family to minor or emergency interventions and only when another physician is not readily available [5]. The UK’s General Medical Council also asserts that physicians must avoid prescribing to anyone they have a close personal relationship with whenever possible [6].
However, a study by La Puma showed that more than 99% of physicians had received requests from family members asking for medical advice, diagnosis, or treatment, and 83% of physicians had prescribed for relatives [7]. This study revealed that primary care physicians provided more services to families or relatives than physicians in other specialties. Previous studies in the US also showed that 74–80% of physicians had treated their family members [8,9,10]. In a German study, 96.7% of the GPs had treated at least one family member in the last 12 months [11].
In Japan, physicians do not have guidelines regarding treating their families and relatives, and little is known about the experiences of primary care physicians. As in other countries, the number of physicians with experience is not expected to be small, but there has been no previous research on the actual situation.
Therefore, the purpose of this study was to investigate the experience of treating family members or relatives among primary care physicians in Japan.
Methods
Study design
We performed a cross-sectional study using an online questionnaire.
Setting and participants
Participants were physicians who were members of the Japan Primary Care Association (JPCA). The JPCA is an academic organization which comprises many Japanese primary care physicians and has around 10,470 members (as of February 2019). We recruited 2,000 physicians using random sampling, who were at least three years postgraduate. The first and second years after graduation from medical school fall under the category of initial postgraduate clinical training [12], and were thus excluded.
In Japan, primary care services are provided by both clinics and hospitals [13]. Also, the boundary between primary care and specialty areas is ambiguous and the census reports that approximately 32% of physicians work in clinics and 64% work in hospitals among all physicians [14]. Therefore, the respondents included physicians working in hospitals.
In addition, there are two important characteristics of the healthcare system in Japan, which are universal health insurance and free access [13]. All residents of Japan are required by law to be enrolled in a health insurance program, and co‐payment rates range from 10 to 30%. Patients are free to choose any healthcare facility, regardless of the severity of their disease and their insurance status.
Study period
Data were collected from February 10 to March 10 in 2021.
Data collection
Participants answered the questionnaire on the Web using Microsoft Forms. We provided URLs via email and sent a total of three reminder emails over the period of data collection. The first 300 respondents received an Amazon gift certificate worth JPY 2,000 (approximately USD 17.4).
Primary outcome: having experience in treating their family members or relatives
The following question was used to explore participants’ experience in treating family members. “Looking back over the past few years, have you ever provided medical care (including medical examinations, prescriptions, procedures, etc.) to your family members or relatives at least once?”.
Based on past studies and reports, we defined “family members or relatives” to include parents, children, siblings, grandparents, grandchildren, spouses, and spouses’ first-and second-degree relatives [2, 7, 15].
Explanatory variable: field of practice (clinic or hospital)
Participants chose their fields of practice from the following: clinics without admission, clinics with admission (1–19 beds), small hospitals (less than 200 beds), medium hospitals (200–499 beds), large hospitals (500 beds or more), and others. In Japan, a hospital is defined as a medical institution with 20 beds or more, whereas a clinic is defined as having less than 20 beds or no beds. In addition, there is a difference in the medical fees among hospitals with more than 200 beds and those with less than 200 beds. Therefore, this classification was used in a previous study conducted in Japan [12].
Covariates
Based on the previous studies, we included covariates for age, gender, geographic location, and whether or not physicians had relatives who were doctors [7, 10, 15]. These covariates were evaluated as categorical variables through a self-administered questionnaire.
Types of treatment, reasons and factors behind the treatment, and physicians’ feelings during the treatment
We also collected information on the type of medical treatment families and relatives received, the reasons and factors behind the treatment, and their feelings (satisfaction or hesitation) during treatment. Some of the questions were: “What were your reasons for providing medical care to your family or relatives?;” “Have you felt satisfied/hesitant while treating family or relatives?” For the latter question, we asked participants to choose from “Often,” “Sometimes,” “Rarely,” and “Never.” These questions and alternatives were based on past studies [7, 15].
Statistical analysis
Nominal data were expressed as percentages, whereas medians with interquartile ranges were calculated for continuous variables. Responses were excluded if there were missing or apparent inconsistencies in them.
We conducted a chi-square test with field of practice (binary variable of hospital or clinic) as the independent variable, and the percentage of doctors who had treated family members or relatives as the outcome. In addition, we conducted a logistic regression analysis with the following factors: age, gender, physician’s geographic location, and presence of a doctor in the family. Age was classified into three groups: < 45 [7], 45–64, ≥ 65 years, and included in the model as a categorical variable.
As four variables, that is, age, gender, physician’s geographic location, and presence of a doctor in the family were included in the final model, and the percentage of “having experience in treating family members or relatives” was estimated to be 80% from previous studies, we calculated that we would require at least 250 responses for this study. All statistical analyses were conducted using StataCorp software (Stata Statistical Software, Release 15, College Station, TX, StataCorp LLC, 2017).
Results
In total, 468 physicians responded to the survey. Two respondents with inappropriate answers regarding age were excluded from the study, so the data of 466 was used (response rate = 23.3%). Table 1 presents the demographic characteristics of the participants. Women accounted for 20.8% of the total participants, men for 78.1%. The age range was 27–80 years with a median age of 44 years (interquartile range: 37–54 years). Of the respondents, 161 (34.5%) worked in clinics, 299 (64.2%) in hospitals, and 6 (1.3%) in others. In terms of geographic location, 59 (12.7%) were in remote islands or rural areas, and 407 (87.3%) were in neither of these locations.
The total number of physicians with experience in treating family members and relatives was 370 (79.4%). The percentage of physicians treating family members or relatives was significantly higher in the clinic group than in the hospital group (87.6% vs. 74.9%, p = 0.0014).
Table 2 shows the results of the multivariable analysis. Working in a clinic (OR 2.30, 95% CI 1.31–4.04) and the age group of 45–64 years(OR 2.93, 95% CI 1.74–4.93) were significantly associated with experience. There were no associations with gender, presence of a doctor in the family, or geographic location (rural or not rural).
Figures 1 and 2 illustrate the types of medical care provided. Prescription rates for acute and chronic diseases were 82.4% and 50.5%, respectively. Vaccination was 61.6%, routine pediatric care was 10.0%, and medical checkups for adults was 17.8%. Obstetric or gynecological examination, including pelvic examination, was performed by 1.6% of the participants.
Types of experience in treating family members or relatives (2) (n = 370). Legend: The percentages of those who had experience with vaccine injections, admission care, medical check-up on adult, routine pediatric care, major surgery, and obstetric/gynecological care were 61.6%, 23.5%, 17.8%, 10.0%, 6.5%, and 1.6%, respectively
Figure 3 shows the reasons for providing medical care to families. The physicians who were satisfied with the treatment comprised 89.2%, including the “Often” and “Sometimes” responses. The percentage of physicians who were hesitant during treatment was 42.4%. The reasons for satisfaction and hesitance with providing medical care are shown in Figs. 4 and 5, respectively.
Reasons for treating family members or relatives (n = 370). Legend: The question was “What were your reasons for providing medical care to your family or relatives.” The respondents were asked to choose “Often”, “Sometimes”, “Rarely”, or “Never” for each of them. This figure shows the results for “Often” and “Sometimes” combined
In addition, 72.5% of the respondents did not know about the guidelines in Europe and the US for the treatment of family members and relatives, and 45.1% of the respondents agreed or somewhat agreed, 20.4% disagreed or somewhat disagreed, and 34.5% were undecided regarding the creation of guidelines in Japan.
Discussion
In this study, we found that about 80% of primary care physicians in Japan had experience of treating family members, which is similar to the findings of previous studies in the US. We had considered the possibility that the percentage of physicians treating family members might be higher than in other countries due to Japan’s universal health insurance and free access, but the results showed almost the same numbers.
The proportion of physicians with experience in treating family members or relatives was significantly higher in the clinic group than in the hospital group. In previous studies, convenience, saving costs, and having greater knowledge and concern than their colleagues were cited as the reasons for providing medical care to family members [10]. In this study, the most common reason for providing care was “request from family or relatives.” We assume that higher accessibility compared to hospitals results in a higher percentage of medical experience in family treatment in the clinic group.
In previous studies, age ≥ 45 years was associated with more experience in providing medical care to family members [7], and the logistic regression analysis in this study also showed that a relatively higher age was a significant factor. Considering that the most common reason for providing medical care is a request from family members or relatives, it is natural that an increase in the number of opportunities to be asked will increase experience. Moreover, for physicians aged ≥ 65 years, such opportunities may decrease. The types of medical care for family members or relatives were similar to those reported in previous studies [7, 15].
Regarding the reasons for providing medical care to families, the Malaysian qualitative study cites the influence of the socio-cultural milieu in Malaysia, where families are expected to help each other [16]. Given that the most common reason for treating family members or relatives was the request from them in this study, such influence may apply to Japan as well. In the study by Reagan, saving relative’s money was the third of the options as a reason for treating family members, but in this study it was the second from the bottom of the options [15]. This may be due to Japan’s universal health insurance, which may have influenced the results.
We did not expect that the percentage of physicians who felt satisfied with the care of family members would reach nearly 90%, whereas the percentage of physicians who felt hesitant was merely 40%. Regarding the development of the guideline, 45.1% of the respondents agreed or somewhat agreed, 20.4% disagreed or somewhat disagreed, and 34.5% were undecided. These results might explain the reason why Japanese primary care physicians have never created the guideline before.
Study strengths
This is the first study to identify the experiences of Japanese physicians in treating their family members or relatives. The number of respondents was relatively large compared to previous studies. Furthermore, to the best of our knowledge, no previous study has evaluated the differences in experiences between those working in clinics and those working in hospitals. The results of the study might be useful for other countries where primary care physicians involve inpatient care such as the US and Canada [17, 18].
Study limitations
Our study has several limitations. First, physicians who had a greater interest in treating their family members might have responded to the survey in greater numbers, leading to an overestimation of the actual rate. However, the rate of about 80% is similar to that observed in previous studies, and we consider the result to reflect reality in Japan. Second, the study was limited to physicians who were members of the JPCA. The number of members is approximately 10,000 among a total of more than 300,000 physicians in Japan. As the definition of primary care is ambiguous in Japan [13], we chose the most representative academic organizations in Japan to minimize this bias. However, the results need to be carefully extrapolated to other primary care societies such as the Japan Society of Hospital General Medicine or other specialties. Third, we were unable to track the outcomes of patients after treatment. This issue needs to be addressed in the future because no previous research has quantitatively tracked patient outcomes, although several qualitative studies have revealed good and bad outcomes or changes in relationships [16, 19,20,21].
Conclusions
As in other countries, nearly 80% of primary care physicians in Japan have treated family members or relatives, especially those who are clinic-based. These findings should stimulate discussions regarding family treatment by primary care physicians and serve as basic data for future studies on the care of physicians’ families or relatives.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available because we did not receive informed consent concerning data sharing from the participants, but the datasets are available from the corresponding author on reasonable request.
Abbreviations
- JPCA:
-
Japan Primary Care Association
References
Gold KJ, Goldman EB, Kamil LH, Walton S, Burdette TG, Moseley KL. No appointment necessary? ethical challenges in treating friends and family. N Engl J Med. 2014;371(Suppl 13):1254–8.
Joel MG, Catherine AM, Kenneth VI. Emergency physician care of family members, friends, colleagues and self. Am J Emerg Med. 2019;37(5):942–6.
American Medical Association. Treating self or family. AMA code of medical ethics opinions on patient-physician relationships, 2016. https://www.ama-assn.org/system/files/2019-01/code-of-medical-ethics-chapter-1_0.pdf. Accessed 1 January 2022.
Sulmasy LS, Bledsoe TA, ACP Ethics, Professionalism and Human Rights Committee. American college of physicians ethics manual: seventh edition. Ann Intern Med. 2019;15 Suppl 170:S1-S32.
Canadian Medical Association. CMA code of ethics and professionalism. approved by the CMA board of directors. 2018. https://policybase.cma.ca/documents/policypdf/PD19-03.pdf. Accessed 1 January 2022.
General Medical Council. Good practice in prescribing and managing medicines and devices content. Ethical guidance for doctors. 2021. https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/good-practice-in-prescribing-and-managing-medicines-and-devices. Accessed 1 January 2022.
La Puma J, Stocking CB, La Voie D, Darling CA. When physicians treat members of their own families. Practices in a community hospital. N Engl J Med. 1991;325(Suppl 18):1290–4.
Boiko PE, Schuman SH, Rust PF. Physicians treating their own spouses: relationship of physicians to their own family’s health care. J Fam Pract. 1984;18(Suppl 6):891–6.
Evans RW, Lipton RB, Ritz KA. A survey of neurologists on self-treatment and treatment of their families. Headache. 2007;47(Suppl 1):58–64.
Scarff JR, Lippmann S. When physicians intervene in their relatives’ health care. HEC Forum. 2012;24(Suppl 2):127–37.
Mücke NA, Schmidt A, Kersting C, Kalitzkus V, Pentzek M, Wilm S, Mortsiefer A. General practitioners treating their own family members: a cross-sectional survey in Germany. BMC Prim Care. 2022;3:23.
Tanaka K, Son D. Experiential learning for junior residents as a part of community-based medical education in Japan. Educ Prim Care. 2019;30(Suppl 5):282–8.
Kato D, Ryu H, Matsumoto T, Abe K, Kaneko M, Ko M, et al. Building primary care in Japan: literature review. J Gen Fam Med. 2019;20(Suppl 5):170–9.
Ministry of Health, Labour and Welfare in Japan. Summary of statistics on physicians, dentists, and pharmacists in 2018. https://policybase.cma.ca/documents/policypdf/PD19-03.pdf. Accessed 25 August 2022.
Reagan B, Reagan P, Sinclair A. ‘Common sense and a thick hide’. Physicians providing care to their own family members. Arch Fam Med. 1994;3(Suppl 7):599–604.
Nik-Sherina H, NG CJ. Doctors treating family members: a qualitative study among primary care practitioners in teaching hospital in Malaysia. Asia Pac Fam Med. 2006;5(Suppl 2):1–6.
Rieger EY, Kushner JNS, Sriram V, Klein A, Wiklund LO, Meltzer DO, Tang JW. Primary care physician involvement during hospitalisation: a qualitative analysis of perspectives from frequently hospitalised patients. BMJ Open. 2021;11(12):e053784.
Chen MA, Hollenberg JP, Michelen W, Peterson JC, Casalino LP. Patient care outside of office visits: a primary care physician time study. J Gen Intern Med. 2011;26(1):58–63.
Fromme EK, Farber NJ, Babbott SF, Pickett ME, Beasley BW. What do you do when your loved one is ill? The line between physician and family member. Ann Intern Med. 2008;149(Suppl 11):825–31.
Giroldi E, Freeth R, Hanssen M, Muris JWM, Margareth K, Cals JWL. Family physicians managing medical requests from family and friends. Ann Fam Med. 2018;16(Suppl 1):45–51.
Chen FM, Feudtner C, Rhodes LA, Green LA. Role conflicts of physicians and their family members: rules but no rulebook. West J Med. 2001;175(Suppl 4):236–9.
Acknowledgements
We would like to thank the participants of the questionnaire in this study. We also would like to thank Editage (www.editage.com) for English language editing.
Funding
This study was funded by a grant from the Future Research Leader Training Program of JPCA. The study sponsor had no role in the study design, data collection, analysis, interpretation, writing of the report, or the decision of submitting the article for publication.
Author information
Authors and Affiliations
Contributions
TM and MK designed the study and participated in implementation, data collection, data analysis, and the writing of the manuscript. TM and MK also served as the guarantors. MI and MF contributed to the study design and critically reviewed the manuscript. TM and MK analyzed the data. All authors had full access to the data and take responsibility for the integrity and accuracy of the analyses. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was performed in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Hamamatsu University School of Medicine (approval number 20–251,2020). Informed consent was obtained from all the participants.
Consent for publication
Not applicable.
Competing interest
The authors declare no conflicts of interest directly relevant to the contents of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Matsunaga, T., Kaneko, M., Fetters, M.D. et al. Japanese primary care physicians’ experience in treating their family members: a cross-sectional study. BMC Prim. Care 23, 240 (2022). https://doi.org/10.1186/s12875-022-01848-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-022-01848-y