Abstract
Background
The Charlson and Elixhauser Comorbidity Indices are the most widely used comorbidity assessment methods in medical research. Both methods are adapted for use with the International Classification of Diseases, which 10th revision (ICD-10) is used by over a hundred countries in the world. Available Charlson and Elixhauser Comorbidity Index calculating methods are limited to a few applications with command-line user interfaces, all requiring specific programming language skills. This study aims to use Microsoft Excel to develop a non-programming and ICD-10 based dataset calculator for Charlson and Elixhauser Comorbidity Index and to validate its results with R- and SAS-based methods.
Methods
The Excel-based dataset calculator was developed using the program’s formulae, ICD-10 coding algorithms, and different weights of the Charlson and Elixhauser Comorbidity Index. Real, population-wide, nine-year spanning, index hip fracture data from the Estonian Health Insurance Fund was used for validating the calculator. The Excel-based calculator’s output values and processing speed were compared to R- and SAS-based methods.
Results
A total of 11,491 hip fracture patients’ comorbidities were used for validating the Excel-based calculator. The Excel-based calculator’s results were consistent, revealing no discrepancies, with R- and SAS-based methods while comparing 192,690 and 353,265 output values of Charlson and Elixhauser Comorbidity Index, respectively. The Excel-based calculator’s processing speed was slower but differing only from a few seconds up to four minutes with datasets including 6250–200,000 patients.
Conclusions
This study proposes a novel, validated, and non-programming-based method for calculating Charlson and Elixhauser Comorbidity Index scores. As the comorbidity calculations can be conducted in Microsoft Excel’s simple graphical point-and-click interface, the new method lowers the threshold for calculating these two widely used indices.
Trial registration
retrospectively registered.
Similar content being viewed by others
Background
Identification of preexisting clinical conditions or comorbidities is of interest in all types of medical research. The Charlson and Elixhauser Comorbidity Indices are of the most widely used comorbidity assessment methods [1,2,3,4,5,6,7,8,9,10] validated on several patient populations like cancer [11], chronic renal failure [12], coronary artery bypass grafting [12], diabetes [12], hip fracture [10, 13,14,15], and stroke [16]. The Charlson Comorbidity Index (CCI) is a weighted score that accounts for the presence of 19 comorbid diseases [1]. CCI was later adapted for use with administrative data based on the International Classification of Diseases [4]. Later, Quan and his colleagues (2011) provided updated weights for CCI, as treatment of some diseases has improved in time [5]. The Elixhauser comorbidity system was initially developed for administrative data when measuring the presence of 30 comorbidities [17]. Van Walraven and his colleagues (2009) later modified the initial classification system into a single weighted score – Elixhauser Comorbidity Index (ECI) [9]. Later studies have provided different weighting schemes for ECI: Thompson and AHRQ (the Agency for Healthcare Research and Quality, Canada) weights [18, 19].
Currently, available CCI and ECI calculation methods are limited to a few software applications, which can only be operated through a command-line user interface, requiring R, SAS or SQL programming language skills [20,21,22,23,24,25,26,27]. Other available calculators allow measuring only a single patient’s comorbidities at a time [28]. As all CCI and ECI dataset calculators require specific programming-based software, the indices’ accessibility is limited for those who use other software for statistical analyses or have no prior programming experience. Thus, the accessibility of CCI and ECI can be increased by developing new methods using more user-friendly interfaces. Microsoft Excel is a widely used spreadsheet programme, and its graphical point-and-click interface allows use without programming. Thus, this study aims to use Microsoft Excel to develop a non-programming and ICD-10 based dataset calculator for CCI and ECI and to validate its results with R- and SAS-based methods.
Methods
Patients
We used real retrospective hip fracture population-wide data from the Estonian Health Insurance Fund. The Estonian Health Insurance Fund organises a national, solidarity-based mandatory health insurance system in Estonia, covering 94% of the population [29]. The hip fracture population was chosen as ICD-10 codes have been found suitable for fracture identification [30], and CCI and ECI have been validated among these patients [10, 13,14,15, 31]. The inclusion and exclusion criteria were chosen in concordance to multiple other studies [30, 32,33,34,35]: (1) age 50 or over; (2) ICD-10 codes S72.0–2 identifying index hip fracture between 1 January 2009–30 September 2017; (3) data validation confirming hip fracture diagnosis and excluding isolated acetabular, pelvic, periprosthetic, isolated greater and lesser trochanter fractures.
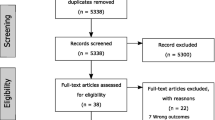
Data validation
The data validation was based on a logic check or the reviewal of patients’ medical information (Fig. 1). Firstly, patients’ Nordic Medico-Statistical Committee’s Classification of Surgical Procedures (NOMESCO) surgical management was reviewed to confirm their hip fracture diagnosis. Following codes confirmed the diagnosis: NFB20, NFB30, NFB40, NFB99, NFB00–9; NFB10–9, NFJ70–3, NFJ60–3, NFJ80–3, NFJ50–3 [36]. If these codes were not available, a patient’s digital images and medical records were reviewed. Two national databases were used to review digital images and medical records: the Foundation of Estonian PACS (an image archiving and communication system database) and the Estonian National Health Information System (https://ap.digilugu.ee/arstiportaal). Uploading medical data to both databases is mandatory by law, particularly since 2010 for medical records and since 2014 for digital images. Digital images were reviewed from January to July 2017 and medical records from January to March 2019. An orthopaedic surgeon and a radiologist reviewed the digital images, and a geriatrician reviewed the medical records. Hip fracture diagnosis was confirmed if one or both of the data sources approved its presence.
Patients’ comorbidities
Comorbidities were defined as diagnoses coded as ICD-10 at any hospital or outpatient health care claims during a four-year period: at the time of the index HF and during the preceding 4 years. The 4 year preceding period was chosen to avoid under-ascertainment of comorbidities [37]. Finally, a restriction was applied to increase the validity of comorbidity assessment: only ICD-10 codes that appeared at least two times, and at least 7 days apart were included [13, 38].
Development of excel-based calculator
The Microsoft Excel-based dataset calculator was developed using ICD-10 coding algorithms [4], and different weighting schemes of CCI and ECI, the program’s basic formulae and wide format (Additional file 1). The 10th revision of the International Classification of Diseases was chosen as it is used by more than a hundred countries, including Estonia, and cited in more than 20,000 scientific articles world [4, 39]. The weighting schemes included the original [1] and the updated [5] CCI weights, and van Walraven [9] and AHRQ weights [18]. The calculator also takes into account the hierarchy of comorbidities: milder disease forms are excluded if a more severe one is present. Excel’s basic formulae were used for making the calculator as this makes it simple and flexible for users. It calculates comorbidity scores in two steps. If cell A2 is a patient’s ID and B2 contains her/his diseases as ICD-10 codes, the first step identifies the patient’s comorbidity categories [=IF (SUM (IF((LEN(B2)-LEN (SUBSTITUTE (UPPER(B2),{“CODE-1”;"CODE-2”; …; “CODE-N”},”“))),1,0)) > 0,1,0)] and the second step uses the output of the previous step and calculates total score using necessary weights (multiplications) and hierarchical conditions (IF functions) [=(C2*1) + IF(C2 = 0,D2*1,0) + … + IF(M2 = 0,L2*2,0)]. These basic formulae also allow users to edit or adapt the calculator for other weights or versions of the International Classification of Diseases codes. Wide-format, showing one subject per row, was preferred as this is the most used final data structure in statistical analysis. As ICD-10 data is occasionally in long format - one morbidity per row, simple data transformation solutions are included in the calculator’s instructions and in its one-minute instructional video (Additional file 2). Data transformations were done with an Excel’s add-in named Ablebits (www.ablebits.com). The add-in’s functions ‘Merge Duplicates’ (transforms long format to wide format), ‘Merge Cells’ (combines codes from multiple columns into one) and ‘Split Text (splits codes from one cell to multiple columns or rows; transforms wide format to long format) are useful for such purposes. The calculator allows ICD-10 codes to be inserted in any format: lowercase, uppercase, with or without punctuation, and any separators can be used between diagnoses. Finally, the calculator’s ability to identify all ICD-10 codes used in CCI and ECI was tested since the used hip fracture population may not cover all of the diseases used in the indicies. The calculator identified all ICD-10 codes used in the two indices.
Statistical analysis
Continuous variables were presented as “median (25th-75th percentile)” and categorical as proportions. The patients’ Charlson weight comorbidity score and the presence of different diseases were calculated using the Excel-based calculator and the R package “comorbidity” [21] and two SAS macros [40, 41]. The Excel-based calculator was validated by comparing the three methods’ results. The calculators’ processing speeds were compared using the study’s data (multiplicated for larger sample sizes). Excel-based calculator’s processing speed was assessed by running formulae in all columns at once. The analyses were run on a Lenovo T480 laptop released at the beginning of 2018 (i5-8250U 1.6 GHz CPU, 16GB RAM, Windows 10 Enterprise 20H2). Data analyses were done in Microsoft™ Excel™ 365 MSO 16.0.13528.203018 64bit (Microsoft Corporation, Redmond, Washington, USA), R 4.0.4 (R Core Team, 2017) and SAS OnDemand for Academics, release 3.8 (Enterprise edition) (SAS Institute Inc., Cary, NC, USA). Adobe Illustrator and Adobe InDesign (versions CC, Adobe Systems, San Jose, CA, USA) and GraphPad Prism (version 7.0, GraphPad Software, Incorporation, San Diego, CA, USA) were used for creating or finalising figures. Wondershare Filmora (version 10.1.20.16(6.0.0..54.8), Wondershare Technology Corporation, South Shenzhen, China) was used for video editing.
Results
Patients and their comorbidities
A total of 11,491 patients were included in the study (Fig. 1). Their median age was 81 years (73–87), 72% (8246) were female, and 51% (5883) had an intracapsular fracture. The Excel-based calculator’s results are presented in two tables: the original and the updated weight CCI scores in Table 1; and AHRQ and van Walraven weight ECI scores in Table 2.
Comparison of the two methods
A total of 192,690 Charlson’s and 353,265 Elixhauser’s output values were compared. The Excel-based calculator’s results were consistent, revealing no discrepancies, with the R- and SAS-based methods.
Processing speed
The Excel-based calculator performed well with sample sizes of up to 200,000 patients, showing a processing time from 2 s up to 4 min and 10 s (Fig. 2). However, calculating comorbidities for 400,000 patients took 21 min and 32 s for CCI and 36 min and 34 s for ECI with the used hard- and software. In contrast, the R- and SAS-based calculators performed all calculations in less than 22 s.
Discussion
This study proposes a novel, simple and validated tool for the most used comorbidity indices in medical research – CCI and ECI. The compared methods performed similarly in terms of accuracy, although the new tool has advantages and disadvantages that should be considered. The main advantage of the Excel-based method is its ease of use: comorbidity scores can be calculated by just copying and pasting patients’ identification numbers and ICD-10 codes from one spreadsheet to another. This can be done in a simple graphical point-and-click interface, requiring no coding skills from its user. However, the Excel-based calculator has limitations. Other programming-based methods allow calculating CCI and ECI with earlier versions or adaptions of the International Classification of Diseases: ICD-9, ICD-9-CM, Enhanced ICD-9-CM codes, or ICD-10-CM [5, 20,21,22,23,24,25,26,27]. The new calculator’s processing speed is reasonable with datasets of up to 200,000 patients and relatively capable hardware, taking up to few minutes in total. Still, it may take a considerable amount of time with larger data. This is explained by the calculator’s formulae-based nature, as they are duplicated in millions of spreadsheet cells, requiring a considerable amount of computing power. Computers with better hardware specifications (especially central processing unit’s [CPU] speed, random-access memory [RAM]) and 64bit version Microsoft Excel are therefore recommended for analysing large data. On the other hand, most medical research studies examine smaller sample sizes, large data splitting is always an option, and an hour-long calculation still takes significantly less time than learning to code. Another limitation is that Excel’s spreadsheets are limited to slightly over a million rows. Therefore, large long-format data may require splitting and should be prepared using multiple sheets.
Ultimately, the final choice between using the Excel-based and other methods depends on a user’s skills, preference, available software and needs. All these factors vary among researchers. The new calculator may be useful for users preferring Microsoft Excel to prepare or analyse data, or those who have no programming skills, or whose used statistical software does not have a module for calculating CCI or ECI. Thus, the new simple Excel-based method lowers the threshold for calculating CCI and ECI, making these indices accessible to a broader audience.
Conclusions
This study proposes a novel, validated, non-programming based method for calculating two of the most used comorbidity indices in medical research - CCI and ECI. The Excel-based calculator allows calculating these comorbidity indices by simply copying and pasting data in a graphical point-and-click interface, thereby lowering the threshold for calculating CCI and ECI. The method may be useful for users preferring Microsoft Excel to prepare or analyse data, or those who have no programming skills, or whose statistical software does not have a corresponding module. The calculator’s slower processing speed is a downside that should be taken into account with very large datasets or less capable hardware or 32bit version of Microsoft Excel.
Availability of data and materials
The study data was not publicly available, but EHIF allowed making anonymized ICD-10 data publicly available. The dataset analysed during the current study is available in the figshare repository, https://doi.org/10.6084/m9.figshare.14046311.
Abbreviations
- AHRQ:
-
The Agency for Healthcare Research and Quality
- CCI:
-
Charlson Comorbidity Index
- ECI:
-
Elixhauser Comorbidity Index
- ICD-9:
-
International Classification of Diseases, 9th revision
- ICD-9-CM:
-
International Classification of Diseases, 9th revision, Clinical Modification
- ICD-10:
-
International Classification of Diseases, 10th revision
- ICD-10-CM:
-
International Classification of Diseases, 10th revision, Clinical Modification
References
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Charlson M, Wells MT, Ullman R, King F, Shmukler C. The Charlson Comorbidity Index can be used prospectively to identify patients who will incur high future costs. PLoS ONE. 2014;9:e112479.
de Groot V, Beckerman H, Lankhorst GJ, Bouter LM. How to measure comorbidity: a critical review of available methods. J Clin Epidemiol. 2003;56:221–9.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi J-C, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9.
Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173:676–82.
Sharabiani MTA, Aylin P, Bottle A. Systematic review of comorbidity indices for administrative data. Med Care. 2012;50:1109–18.
Karres J, Heesakkers NA, Ultee JM, Vrouenraets BC. Predicting 30-day mortality following hip fracture surgery: evaluation of six risk prediction models. Injury. 2015;46:371–7.
Lu M, Sajobi T, Lucyk K, Lorenzetti D, Quan H. Systematic review of risk adjustment models of hospital length of stay (LOS). Med Care. 2015;53:355–65.
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47:626–33.
Metcalfe D, Masters J, Delmestri A, Judge A, Perry D, Zogg C, et al. Coding algorithms for defining Charlson and Elixhauser co-morbidities in read-coded databases. BMC Med Res Methodol. 2019;19:115.
Arrigo RT, Kalanithi P, Cheng I, Alamin T, Carragee EJ, Mindea SA, et al. Predictors of survival after surgical treatment of spinal metastasis. Neurosurgery. 2011;68:674–81.
Li B, Evans D, Faris P, Dean S, Quan H. Risk adjustment performance of Charlson and Elixhauser comorbidities in ICD-9 and ICD-10 administrative databases. BMC Health Serv Res. 2008;8:12.
Radley DC, Gottlieb DJ, Fisher ES, Tosteson ANA. Comorbidity risk-adjustment strategies are comparable among persons with hip fracture. J Clin Epidemiol. 2008;61:580–7.
Toson B, Harvey LA, Close JCT. The ICD-10 Charlson comorbidity index predicted mortality but not resource utilization following hip fracture. J Clin Epidemiol. 2015;68:44–51.
Ondeck NT, Bovonratwet P, Ibe IK, Bohl DD, McLynn RP, Cui JJ, et al. Discriminative ability for adverse outcomes after surgical management of hip fractures: a comparison of the Charlson comorbidity index, Elixhauser comorbidity measure, and modified frailty index. J Orthop Trauma. 2018;32:231–7.
Goldstein LB, Samsa GP, Matchar DB, Horner RD. Charlson index comorbidity adjustment for ischemic stroke outcome studies. Stroke. 2004;35:1941–5.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27.
Moore BJ, White S, Washington R, Coenen N, Elixhauser A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: the AHRQ Elixhauser comorbidity index. Med Care. 2017;55:698–705.
Thompson NR, Fan Y, Dalton JE, Jehi L, Rosenbaum BP, Vadera S, et al. A new Elixhauser-based comorbidity summary measure to predict in-hospital mortality. Med Care. 2015;53:374–9.
Stagg V. CHARLSON: Stata module to calculate Charlson index of comorbidity. 2017. https://econpapers.repec.org/software/bocbocode/S456719.htm. Accessed 10 May 2021.
Gasparini A. comorbidity: An R package for computing comorbidity scores. J Open Source Softw. 2018;3:648.
Healthcare Cost and Utilization Project (HCUP). Elixhauser Comorbidity Software Refined for ICD-10-CM. Agency for Healthcare Research and Quality. 2020. https://www.hcup-us.ahrq.gov/toolssoftware/comorbidityicd10/comorbidity_icd10.jsp. Accessed 10 May 2021.
Manitoba Centre for Health Policy. Concept: Charlson Comorbidity Index (SAS code). 2020. http://mchp-appserv.cpe.umanitoba.ca/viewConcept.php?conceptID=1098. Accessed 10 May 2021.
Manitoba Centre for Health Policy. Concept: Elixhauser Comorbidity Index (SAS code). 2020. http://mchp-appserv.cpe.umanitoba.ca/viewConcept.php?conceptID=1436. Accessed 10 May 2021.
Stagg V. ELIXHAUSER: Stata module to calculate Elixhauser index of comorbidity. 2015. https://ideas.repec.org/c/boc/bocode/s458077.html. Accessed 10 May 2021.
Syed S, Baghal A, Prior F, Zozus M, Al-Shukri S, Syeda HB, et al. Toolkit to compute time-based Elixhauser comorbidity indices and extension to common data models. Healthc Inform Res. 2020;26:193–200.
Wasey JO. R “icd” package. 2020. https://www.rdocumentation.org/packages/icd/versions/4.0.9. Accessed 10 May 2021.
Hall WH, Ramachandran R, Narayan S, Jani AB, Vijayakumar S. An electronic application for rapidly calculating Charlson comorbidity score. BMC Cancer. 2004;4:94.
Organisation for Economic Co-operation and Development. Estonia: country health profile 2019. 2019. http://www.oecd.org/publications/estonia-country-health-profile-2019-0b94102e-en.htm. Accessed 10 May 2021.
Lix LM, Azimaee M, Osman BA, Caetano P, Morin S, Metge C, et al. Osteoporosis-related fracture case definitions for population-based administrative data. BMC Public Health. 2012;12:1–10.
Lix LM, Quail J, Teare G, Acan B. Performance of comorbidity measures for predicting outcomes in population-based osteoporosis cohorts. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA. 2011;22:2633–43.
Brozek W, Reichardt B, Kimberger O, Zwerina J, Dimai HP, Kritsch D, et al. Mortality after hip fracture in Austria 2008-2011. Calcif Tissue Int. 2014;95:257–66.
Diamantopoulos AP, Hoff M, Skoie IM, Hochberg M, Haugeberg G. Short- and long-term mortality in males and females with fragility hip fracture in Norway. A population-based study. Clin Interv Aging. 2013;8:817–23.
Jain R, Basinski A, Kreder HJ. Nonoperative treatment of hip fractures. Int Orthop. 2003;27:11–7.
Jürisson M, Vorobjov S, Kallikorm R, Lember M, Uusküla A. The incidence of hip fractures in Estonia, 2005-2012. Osteoporos Int. 2015;26:77–84.
Nordic Medico-Statistical Committee. NOMESCO classification of surgical procedures, Version 1.6. 2001. https://haigekassa.ee/uploads/userfiles/NCSP_1_.pdf. Accessed 10 May 2021.
Jürisson M, Raag M, Kallikorm R, Lember M, Uusküla A. The impact of comorbidities on hip fracture mortality: a retrospective population-based cohort study. Arch Osteoporos. 2017;12:1–10.
Tosteson ANA, Gottlieb DJ, Radley D, Fisher ES, Melton LJ. Excess mortality following hip fracture: the role of underlying health status. Osteoporos Int. 2007;18:1463–72.
The World Health Organization. World Health Organization. ICD Information Sheet WHO http://www.who.int/classifications/icd/factsheet/en/. Accessed 10 May 2021.
Turner K, Burchill C. Elixhauser Comorbidty index macro for SAS. 2006. http://mchp-appserv.cpe.umanitoba.ca/Upload/SAS/_ElixhauserICD10.sas.txt. Accessed 11 Oct 2021.
Turner K, Burchill C. Charlson Comorbidty index macro for SAS. 2006. http://mchp-appserv.cpe.umanitoba.ca/Upload/SAS/_CharlsonICD10.sas.txt. Accessed 11 Oct 2021.
Acknowledgements
We acknowledge Associate Professor Raul Kangro for calculating comorbidity scores in SAS, the Estonian Health Insurance Fund for their cooperation, Dr. Pirja Sarap, Dr. Egon Puuorg for their help in data validation, and Mr. Tuudur Tamme for providing background music for the instructional video.
Funding
This work was supported by (grant numbers IUT20–46 and PSG610) from the Estonian Research Council, and by the European Union through the European Regional Development Fund (grant number MMVCM16293I) and through the Seventh Framework Programme (grant number 602398). The funders had no involvement in study design, data collection or analysis, interpretation or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors designed the study. PP and KT performed the data analysis and developed the Excel-based calculator. TS, ES and HK validated the data. PP and KT jointly wrote the first draft. All authors jointly and critically revised the manuscript to its final form. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All the study’s methods were performed in accordance with the Declaration of Helsinki and approved by the Research Ethics Committee of the University of Tartu on 17 June 2013 (reference 227/T-12) and by the Estonian Data Protection Inspectorate for the use of personalised data on 1 December 2017 (reference 2.2.-1/17/47). Informed consent was not required by the Research Ethics Committee of the University of Tartu for this retrospective cohort study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Prommik, P., Tootsi, K., Saluse, T. et al. Simple Excel and ICD-10 based dataset calculator for the Charlson and Elixhauser comorbidity indices. BMC Med Res Methodol 22, 4 (2022). https://doi.org/10.1186/s12874-021-01492-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12874-021-01492-7