Abstract
Background
In Oslo, the majority of patients with acute poisoning are treated in primary care, at an emergency outpatient clinic with limited diagnostic and treatment resources. We describe the poisonings currently seen in this setting. We compare our findings with previous studies, with special concern for the appearance of new toxic agents, and changes in overall numbers and patterns of poisoning.
Methods
Observational study. Patients above the age of 12 years presenting at Oslo Accident and Emergency Outpatient Clinic (Oslo Legevakt) with acute poisoning were included consecutively from October 2011 through September 2012. Physicians and nurses registered data on preset forms. Main outcome measures were toxic agents, age, sex, intention, referral and time of presentation.
Results
There were 2923 episodes of acute poisoning in 2261 patients. Median age of the patients was 32 years, and 1430 (63 %) were males. The most frequent toxic agents were ethanol in 1684 (58 %) episodes, heroin in 542 (19 %), benzodiazepines in 521 (18 %), amphetamine in 275 (9 %), fire smoke in 192 (7 %), gamma-hydroxybutyrate (GHB) in 144 (5 %), and cannabis in 143 (5 %). In 904 (31 %) poisonings there were more than one toxic agent. In 493 episodes (17 %), the patient was hospitalised, and in 60 episodes (2 %) admitted to a psychiatric ward. Most poisonings, 2328 (80 %), were accidental overdoses with substances of abuse, 276 (9 %) were suicide attempts, and 312 (11 %) were accidents. Among ethanol poisonings in patients above the age of 26 years, 685/934 (73 %) were in males, and 339/934 (36 %) presented during weekends. However, among ethanol poisonings in patients under the age of 26 years, 221/451 (49 %) were in females, and 297/451 (66 %) presented during weekends.
Conclusions
The poisonings treated in this primary care setting were mostly due to accidental overdoses with ethanol or other substances of abuse. There is a disconcerting weekend drinking pattern among adolescents and young adults, with young females presenting as often as young males with ethanol poisoning.
Similar content being viewed by others
Background
Acute poisoning constitutes a major health problem. It causes frequent presentations to emergency services, and is mainly due to suicidal behaviour, substance use disorders, or accidents. Irrespective of intention, the long-term mortality is high for this patient group [1]. The pattern of poisoning varies between areas and changes over time. New drugs appear [2, 3], poisoning patterns for familiar substances change [4, 5], there are local endemics [6] and epidemics [7, 8]. To keep track of trends and changes, updated studies are needed.
Most patients with acute poisoning are treated as outpatients in hospital emergency departments. In Oslo, however, the majority of poisoned patients are treated in primary care, at the Oslo Accident and Emergency Outpatient Clinic (OAEOC, Oslo Legevakt). Previous studies in 2003 and 2008 have shown that treatment of acute poisoning at the OAEOC is safe, considering the low mortality during treatment and immediately after discharge [9, 10].
The prognosis for patients treated for acute poisoning is serious, whether the poisoning was a suicide attempt or associated with substance abuse [1, 11, 12]. The repetition rate is high; one in three patients present with acute poisoning again within the first year [13]. Follow-up is usually initiated after suicide attempt, but less frequently for patients with substance abuse [14–17]. This is also the case at the OAEOC [9]. In our study from 2008 we assessed follow-up initiated from the OAEOC [9], but not whether the patients actually presented at the institution or clinic they were referred to. In the present study, carried out in 2012, this will be addressed. This article presents the epidemiological data from the 2012 study. The follow-up data will be presented later.
The number of poisonings treated at the OAEOC more than doubled from 2003 to 2008, in contrast to the stable incidence of poisoning seen at Oslo hospitals in the same time period [9, 10]. This trend needs to be tracked. Furthermore, as the majority of poisonings with substances of abuse in Oslo are treated at the OAEOC [9, 15], it is well suited as a sentinel post for assessing changes in their epidemiology.
Objective
The objective was to describe the current poisoning pattern seen at the OAEOC, with special concern for the appearance of new toxic agents and changes in overall numbers, patterns of poisoning, intention and referral. The study was designed similarly to the studies in 2003 and 2008 [9, 10], in order to compare results.
Methods
Design
The study was an observational cross-sectional study, part of a larger prospective study of treatment of acute poisoning at the OAEOC.
Setting
The Norwegian emergency care system has two levels; hospitals and primary care emergency services. Local primary care emergency services are provided by regular general practitioners during office hours, and by general practice out-of-hours services in local casualty clinics during nights and weekends. Some casualty clinics are in service at all hours. Patients cannot present directly to hospital emergency departments, but have to be assessed in primary care or by the ambulance service first.
The OAEOC is the main casualty clinic in Oslo, serving the entire city at all hours. It has about 200 000 consultations a year, equally split between departments for accidents and for emergency general practice. It also contains emergency social services and a psychiatric emergency outpatient clinic. There are facilities for observation of poisoned patients for up to four hours. However, diagnostic tools and treatment options are limited, making the management of poisoned patients less costly than in hospitals. Other casualty clinics in Oslo do not treat patients with acute poisoning to any significant extent. About one in ten patients presenting to the OAEOC are referred to hospital. Oslo is the capital of Norway and as of January 1st 2012 had 613 285 inhabitants, of whom 502 336 were above the age of 12.
Inclusion
All patients above the age of 12 treated at the OAEOC with a main diagnosis of acute poisoning were included. Patients with other main diagnoses, but a co-diagnosis of acute poisoning, were included if the poisoning necessitated treatment. The study period was set to one year to encompass seasonal variations. Patients were included consecutively from October 1st 2011 to September 30th 2012, by the physician treating them. Patient lists in the electronic medical records were regularly and systematically searched during the study period to ensure the inclusion of all eligible patients. Any eligible patients not included while treated, were included when found in these searches.
Data collection
The physician and nurse treating the patient registered data on preset forms. We reviewed the registration forms, and any missing information was collected, if available, from the local electronic medical records. Data for patients included from the patient list searches was collected from the local electronic medical records.
Outcome measures
The outcome measures were toxic agents, age, sex, intention, referral, and time and mode of presentation.
The physician treating the patient made diagnoses of toxic agents based on all information available at the time, including statements from the patient and companions, clinical examination, and information from the police or ambulance service. No toxicological screening tests are done at the OAEOC, except for ethanol breath analyser test. In poisonings with more than one toxic agent, the main agent was defined as the one considered most toxic in the doses taken.
The physician also categorised intention. Poisonings with substances of abuse (including ethanol, opioids, benzodiazepines, Z-hypnotics, gamma-hydroxybutyrate (GHB), cannabis, cocaine, amphetamine and related substances, hallucinogens, other novel psychoactive substances, and other substances with abuse potential) taken for intoxication or recreational purposes were classified as accidental overdoses with substances of abuse (AOSAs). Poisonings with any degree of suicidal intention were classified as suicide attempts. Poisonings with no intention of self-harm or intoxication were classified as accidents.
Time of presentation was categorised as weekend or weekday. Weekend was defined as presentation between Saturday 00:00 and Sunday 23:59.
Ethics
The study was performed in accordance with the Helsinki declaration. It was approved by the Regional Committee South East for Medical and Health Research Ethics (REK nr 2010/1129–1) and by the Privacy Protection Ombudsman at Oslo University Hospital.
Statistics
Analyses were done in IBM SPSS version 21 (IBM Corp.). Pearson’s chi-square test or Fisher’s exact test (for expected cell values five or less) were used to compare frequencies. Mann-Whitney U-test was used in age comparisons.
Results
There were 3139 episodes of acute poisoning during one year. In 216 (7 %) episodes, the patient declined participation, leaving 2923 cases of acute poisoning in 2261 patients included in the study. There were 1430 (63 %, p < 0.001) male patients, and 1919 (66 %, p < 0.001) of the poisoning episodes occurred in males. Median age was 32 years, 35 years for males and 28 years for females (Table 1). There was no significant difference in age (p = 0.81) or sex (p = 0.75) between the included patients and those who declined.
The most frequent toxic agents were ethanol in 1684 (58 %) episodes, heroin in 542 (19 %), benzodiazepines in 521 (18 %), and amphetamine in 275 (9 %) (Table 2).
In 904 (31 %) episodes there were more than one toxic agent. Among these, 647 had one co-agent, 194 had two co-agents, 63 had from three to five co-agents, and 599/904 (66 %, p < 0.001) were in males. Most common were combinations of opioids with benzodiazepines or central stimulants (Table 3).
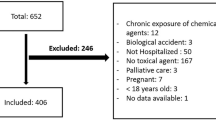
Patient flow is presented in Fig. 1. One in five patients were hospitalised. No patients died at the OAEOC.
Poisonings with illegal substances of abuse were more common in males, and pharmaceuticals in young females (Fig. 2). While ethanol poisonings overall were more common in males, among the 451 ethanol poisonings in patients under the age of 26 years, 221 (49 %, p = 0.67) were in females. Of the 37 patients with five or more poisoning episodes, 20 (54 %) were males aged from 36 to 60. They mainly presented with ethanol or heroin poisonings.
Age, sex and main toxic agents. Age and sex distribution for groups of main agents among poisonings treated at Oslo Accident and Emergency Outpatient Clinic during one year. For ethanol poisoning, the peaks in the young age groups were due to many patients with one poisoning episode. The peak among older males was due to a group of patients with repeated poisonings
Most poisonings, 2328 (80 %), were AOSAs, 276 (9 %) were suicide attempts, and 312 (11 %) were accidents. AOSAs were more frequent among males, 1652/2328 (71 %, p < 0.001). Suicide attempts were more frequent among females, 186/276 (67 %, p < 0.001). Accidents were more evenly distributed, with 171/312 (55 %, p = 0.09) occurring among males. Among the suicide attempters 24/276 (9 %) were admitted to psychiatric wards (including four patients admitted for compulsory observation), 123/276 (45 %) admitted to somatic hospitals, 79/276 (29 %) referred to psychiatric outpatient clinics, and 25/276 (9 %) to other follow-up, while 6/276 (2 %) were discharged with no follow-up and 19/276 (7 %) left against medical advice (Fig. 1). Benzodiazepines and paracetamol were the most common main agents taken in suicide attempts (Table 2). Most of the accidents, 191/312 (61 %), were exposures to fire smoke, requiring hospitalisation in 27/191 (14 %) cases.
Young patients with ethanol poisoning more often presented during weekends than on weekdays; 297/451 (66 %, p < 0.001) of those under the age of 26 years, 105/198 (53 %, p < 0.001) of those aged 26 to 35 years, and 76/196 (39 %, p = 0.002) of those aged 36 to 45 years, presented on Saturdays or Sundays. This weekend presentation trend for ethanol poisoning was not seen among patients above the age of 45. Ethanol poisonings in weekends were more common in males, but among patients under the age of 26, 143/297 (48 %, p = 0.52) were in females. GHB poisonings, 50/115 (43 %, p < 0.001), were also more frequent during weekends.
Discussion
Summary of main results
The majority of the 2923 poisonings were AOSAs, and the most frequent toxic agents were ethanol, heroin, benzodiazepines, and amphetamine. One in five patients were hospitalised. Half of the ethanol poisonings in patients under the age of 26 were in females. Most young patients with ethanol poisoning presented during weekends.
Strengths and limitations
Patients were registered consecutively during one year to ensure that all poisonings were included, and to encompass seasonal variations. Though some patients declined to participate, the study gives a nearly complete picture of the poisonings seen at the OAEOC. It does not, however, give the full picture of poisoning in Oslo, mainly because the most severely poisoned patients are not treated at the OAEOC. There are approximately 120 deaths from poisoning in Oslo annually, 80–90 % occur outside the health services and are declared dead on site [15, 18]. Some 700 poisonings per year bypass the OAEOC on their way to Oslo hospitals, most of them poisonings with pharmaceuticals triaged by the ambulance service [10, 15]. In 2003, 750 patients were discharged on site by the ambulance service, mainly after treatment for opioid poisoning [10]. However, most poisonings with substances of abuse in Oslo are treated at the OAEOC [9, 15]. Thus, this study should be a good indicator of trends and changes in this category of poisonings in Oslo.
No toxicological screening tests are done at the OAEOC, except for ethanol breath analyser test. No confirmative tests were done in this study, rendering the diagnosis of toxic agents uncertain. This is a major limitation. However, the study mirrors the actual clinical situation in emergency settings such as the OAEOC. There may also be inter-rater differences in the diagnostic assessments, as many physicians participated.
Some co-categorisations make the results less precise. Both amphetamine and methamphetamine are probably present in the amphetamine category. Users in Oslo rarely distinguish between them, but Norwegian police has seized more methamphetamine than amphetamine since 2003 [19]. In 2008 Z-hypnotics made up 15 % of the sedatives [9]. Developments, however, cannot be traced, as Z-hypnotics were categorised as benzodiazepines in the present study. From comments written on the registration forms it is evident that poisonings with synthetic cannabinoids first appeared at the OAEOC in the fall of 2011. However, no separate category had been made on the registration forms, and they were categorised as cannabis.
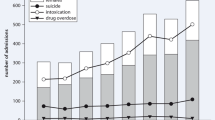
Trends and changes
The number of poisonings treated at the OAEOC has increased by 24 % since 2008 [9]. In comparison, the population of Oslo has grown by 8 %. Thus, the increase observed from 2003 to 2008 [9] has continued. GHB poisonings more than doubled (148 % increase), and there were substantial increases in ethanol (36 %), amphetamine (40 %) and cocaine (66 %) poisonings. In contrast, there was a decrease in fire smoke exposures. The proportions of ambulance referrals, hospital admissions and suicide attempts were largely unchanged since 2008 [9].
Total sales of alcohol in Norway has been stable since 2007, and total consumption among adolescents and young adults had been decreasing from 2003 to 2008 [19]. Still, the number of acute ethanol poisonings at the OAEOC has increased, many of them, as elsewhere [20, 21], in young patients in weekends. Studies from different European cities also report an increase in the number of ethanol poisonings over the last decade, especially among young adults and adolescents [4, 21–23]. It is possible that a segment of the younger population drink larger quantities than before, as some studies have shown [5, 23, 24]. If so, this is a disconcerting trend, as binge drinking carries the risk of serious consequences [25, 26].
Half of the young patients with ethanol poisoning were female. Though most studies report a majority of males [4, 5, 20, 21], similar findings have been reported from Slovakia [23], and a Swiss study showed an increasing number of young females with ethanol poisoning [22]. About 80 % of Norwegians under the age of 20 report having drunk alcohol. The proportion has been slightly larger for females than males during the last decades [19]. However, young females presenting with ethanol poisoning as often as young males, has not been reported in Norway before.
The increase in GHB poisoning is probably a reflection of more widespread use in Norway, consistent with the increase in police seizures [19].
Poisonings with novel central stimulant drugs were hardly seen. This contrasts with findings from the UK [2]. Ecstasy poisonings were few, similar to in the UK [2], and consistent with decreasing seizures by Norwegian police [19]. Poisoning with these substances may have been misclassified as amphetamine or cocaine, both increased compared to 2008 [9]. Amphetamine still dominated, as has been usual in Norway [27].
The widespread combination of opioids with benzodiazepines and central stimulants is worrying [28, 29]. Most fatal poisonings in Oslo are due to opioids, usually combined with other agents [15, 18, 30].
In 2008, 48 % of the patients were discharged without follow-up [9]. This proportion was reduced to 36 % in this study, mainly because many patients were enrolled in a new follow-up program for the young run by the Emergency Social Services. A major incitement for creating this program was the large proportion of patients discharged without follow-up shown in the 2008 study. The emergency setting is an opportunity for interventions to reduce alcohol and drug use and abuse, and such interventions should be encouraged [31, 32].
Only two percent of patients with suicidal intention were discharged without follow-up, a reassuring finding, as these patients have a higher risk of future suicide [1]. Compared to 2008, patients were referred to psychiatric outpatient treatment rather than hospitalised, after suicide attempts [9]. More detailed data on the follow-up initiated from the OAEOC, and whether the patients actually presented at the institution they were referred to, will be presented in separate articles.
Acute poisoning in primary care
This study shows the wide range of poisonings treated in a primary care setting. Four fifths of the patients with acute poisoning brought to the OAEOC were treated locally and discharged without transfer to hospital, as in the previous studies [9, 10], and no patients died at the OAEOC. As long as the patients in need of hospital management are identified and transferred, it seems sensible to treat poisoned patients in primary care outpatient emergency clinics.
Conclusions
A large and increasing number of acute poisonings were treated at the OAEOC, mostly accidental overdoses with ethanol or other substances of abuse. There is a disconcerting weekend drinking pattern among adolescents and young adults, with young females presenting as often as young males with ethanol poisoning.
Abbreviations
- AOSA:
-
Accidental overdose with substances of abuse
- GHB:
-
Gamma-hydroxybutyrate
- NSAIDs:
-
Non-steroid anti-inflammatory drugs
- OAEOC:
-
Oslo Accident and Emergency Outpatient Clinic
- UK:
-
United Kingdom of Great Britain and Northern Ireland
- Z-hypnotics:
-
Zolpidem and zopiclone
References
Bjornaas MA, Jacobsen D, Haldorsen T, Ekeberg O. Mortality and causes of death after hospital-treated self-poisoning in Oslo: a 20-year follow-up. Clin Toxicol. 2009;47:116–23.
Wood DM, Greene SL, Dargan PI. Five-year trends in self-reported recreational drugs associated with presentation to a UK emergency department with suspected drug-related toxicity. Eur J Emerg Med. 2013;20:263–7.
Rosenbaum CD, Carreiro SP, Babu KM. Here today, gone tomorrow…and back again? A review of herbal marijuana alternatives (K2, Spice), synthetic cathinones (bath salts), kratom, Salvia divinorum, methoxetamine, and piperazines. J Med Toxicol. 2012;8:15–32.
Haberkern M, Exadaktylos AK, Marty H. Alcohol intoxication at a university hospital acute medicine unit--with special consideration of young adults: an 8-year observational study from Switzerland. Emerg Med J. 2010;27:199–202.
Allely P, Graham W, McDonnell M, Spedding R. Alcohol levels in the emergency department: a worrying trend. Emerg Med J. 2006;23:707–8.
Knudsen K, Greter J, Verdicchio M. High mortality rates among GHB abusers in Western Sweden. Clin Toxicol. 2008;46:187–92.
Vallersnes OM, Lund C, Duns AK, Netland H, Rasmussen IA. Epidemic of poisoning caused by scopolamine disguised as Rohypnol tablets. Clin Toxicol. 2009;47:889–93.
Vevelstad M, Oiestad EL, Middelkoop G, Hasvold I, Lilleng P, Delaveris GJ, et al. The PMMA epidemic in Norway: comparison of fatal and non-fatal intoxications. Forensic Sci Int. 2012;219:151–7.
Lund C, Vallersnes OM, Jacobsen D, Ekeberg O, Hovda KE. Outpatient treatment of acute poisonings in Oslo: poisoning pattern, factors associated with hospitalization, and mortality. Scand J Trauma Resusc Emerg Med. 2012;20:1.
Heyerdahl F, Hovda KE, Bjornaas MA, Nore AK, Figueiredo JC, Ekeberg O, et al. Pre-hospital treatment of acute poisonings in Oslo. BMC Emerg Med. 2008;8:15.
Bjornaas MA, Bekken AS, Ojlert A, Haldorsen T, Jacobsen D, Rostrup M, et al. A 20-year prospective study of mortality and causes of death among hospitalized opioid addicts in Oslo. BMC Psychiatry. 2008;8:8.
Bargagli AM, Hickman M, Davoli M, Perucci CA, Schifano P, Buster M, et al. Drug-related mortality and its impact on adult mortality in eight European countries. Eur J Public Health. 2006;16:198–202.
Heyerdahl F, Bjornaas MA, Dahl R, Hovda KE, Nore AK, Ekeberg O, et al. Repetition of acute poisoning in Oslo: 1-year prospective study. Br J Psychiatry. 2009;194:73–9.
Bjornaas MA, Hovda KE, Heyerdahl F, Skog K, Drottning P, Opdahl A, et al. Suicidal intention, psychosocial factors and referral to further treatment: a one-year cross-sectional study of self-poisoning. BMC Psychiatry. 2010;10:58.
Lund C, Teige B, Drottning P, Stiksrud B, Rui TO, Lyngra M, et al. A one-year observational study of all hospitalized and fatal acute poisonings in Oslo: epidemiology, intention and follow-up. BMC Public Health. 2012;12:858.
Cook S, Moeschler O, Michaud K, Yersin B. Acute opiate overdose: characteristics of 190 consecutive cases. Addiction. 1998;93:1559–65.
Bennewith O, Peters TJ, Hawton K, House A, Gunnell D. Factors associated with the non-assessment of self-harm patients attending an Accident and Emergency Department: results of a national study. J Affect Disord. 2005;89:91–7.
Bjornaas MA, Teige B, Hovda KE, Ekeberg O, Heyerdahl F, Jacobsen D. Fatal poisonings in Oslo: a one-year observational study. BMC Emerg Med. 2010;10:13.
RusStat. SIRUS Norwegian Institute for Alcohol and Drug Research [http://statistikk.sirus.no/sirus]
Johansen IH, Morken T, Hunskaar S. Contacts related to psychiatry and substance abuse in Norwegian casualty clinics. A cross-sectional study. Scand J Prim Health Care. 2009;27:180–5.
Bitunjac K, Saraga M. Alcohol intoxication in pediatric age: ten-year retrospective study. Croat Med J. 2009;50:151–6.
Holzer BM, Minder CE, Schatti G, Rosset N, Battegay E, Muller S, et al. Ten-year trends in intoxications and requests for emergency ambulance service. Prehospital Emerg Care. 2012;16:497–504.
Kuzelova M, Hararova A, Ondriasova E, Wawruch M, Riedel R, Benedekova M, et al. Alcohol intoxication requiring hospital admission in children and adolescents: retrospective analysis at the University Children's Hospital in the Slovak Republic. Clin Toxicol. 2009;47:556–61.
Hallgren M, Leifman H, Andreasson S. Drinking less but greater harm: could polarized drinking habits explain the divergence between alcohol consumption and harms among youth? Alcohol Alcohol. 2012;47:581–90.
Stolle M, Sack PM, Thomasius R. Binge drinking in childhood and adolescence: epidemiology, consequences, and interventions. Dtsch Arztebl Int. 2009;106:323–8.
Courtney KE, Polich J. Binge drinking in young adults: Data, definitions, and determinants. Psychol bull. 2009;135:142–56.
European Drug Report 2013: Trends and developments [http://www.emcdda.europa.eu/attachements.cfm/att_213154_EN_TDAT13001ENN1.pdf]
Jones JD, Mogali S, Comer SD. Polydrug abuse: a review of opioid and benzodiazepine combination use. Drug Alcohol Depend. 2012;125:8–18.
Herbeck DM, Brecht ML, Lovinger K, Raihan A, Christou D, Sheaff P. Poly-drug and marijuana use among adults who primarily used methamphetamine. J Psychoactive Drugs. 2013;45:132–40.
Gjersing L, Jonassen KV, Biong S, Ravndal E, Waal H, Bramness JG, et al. Diversity in causes and characteristics of drug-induced deaths in an urban setting. Scand J Public Health. 2013;41:119–25.
D'Onofrio G, Becker B, Woolard RH. The impact of alcohol, tobacco, and other drug use and abuse in the emergency department. Emerg Med Clin North Am. 2006;24:925–67.
Crawford MJ, Patton R, Touquet R, Drummond C, Byford S, Barrett B, et al. Screening and referral for brief intervention of alcohol-misusing patients in an emergency department: a pragmatic randomised controlled trial. Lancet. 2004;364:1334–9.
Acknowledgments
We thank the physicians and nurses at the OAEOC for including patients and registering data, and dr Sheranthi de Mel for revising and improving the English in the manuscript.
This work was funded by The Norwegian Medical Association’s General Practice Research Fund, grant number AMFF-11-07.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
DJ and OMV conceived the study. All authors developed the idea and designed the study. OMV collected and analysed the data. MB, OE and DJ supervised the study. OMV drafted the manuscript. All authors revised the manuscript and approved the final version.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Vallersnes, O.M., Jacobsen, D., Ekeberg, Ø. et al. Patients presenting with acute poisoning to an outpatient emergency clinic: a one-year observational study in Oslo, Norway. BMC Emerg Med 15, 18 (2015). https://doi.org/10.1186/s12873-015-0045-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-015-0045-2