Abstract
Background
Diabetes Mellitus (DM) is a rapidly growing disorder worldwide, especially in the Middle East. A higher incidence of coronary artery diseases requiring coronary artery bypass graft (CABG) surgery has been reported in patients with diabetes. We assessed the association between type 2 diabetes mellitus (T2DM) and in-hospital major adverse cardiac and cerebrovascular events (MACCEs) and postoperative complications among patients who underwent on-pump isolated CABG.
Methods
In this retrospective cohort study, we used the data registered for CABG patients from two heart centers in the Golestan province (North of Iran) between 2007 and 2016. The study population included 1956 patients divided into two groups: 1062 non-diabetic patients and 894 patients with diabetes (fasting plasma glucose ≥126 mg/dl or using antidiabetic medications). The study outcome was in-hospital MACCEs, a composite outcome of myocardial infarction (MI), stroke and cardiovascular death, and postoperative complications, including postoperative arrhythmia, acute atrial fibrillation (AF), major bleeding (defined as reoperation due to bleeding), and acute kidney injury (AKI).
Results
During the 10-year study period, 1956 adult patients with a mean (SD) age of 59.0 (9.60) years were included. After adjustment for age, gender, ethnicity, obesity, opium consumption, and smoking, diabetes was a predictor of postoperative arrhythmia (AOR 1.30, 95% CI 1.08–1.57; P = 0.006). While it was not a predictor of in-hospital MACCEs (AOR 1.35, 95% CI 0.86, 2.11; P = 0.188), AF (AOR 0.85, 95% CI 0.60–1.19; P = 0.340), major bleeding (AOR 0.80, 95% CI 0.50, 1.30; P = 0.636) or AKI (AOR 1.29, 95% CI 0.42, 3.96; P 0.656) after CABG surgery.
Conclusion
Findings indicated that diabetes increased the risk of postoperative arrhythmia by 30%. However, we found similar in-hospital MACCEs, acute AF, major bleeding, and AKI following CABG surgery in both diabetic and non-diabetic patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Type 2 Diabetes Mellitus (T2DM) is a multifaceted disorder affecting an increasing portion of the population worldwide [1, 2]. The Middle East, in particular, is one of the primary regions where the number of diabetic patients is rapidly increasing [3, 4]. Diabetic patients are associated with a 4.4-fold increased risk due to cardiovascular disorders [5].
While percutaneous interventions (PCI) have become a widespread treatment for coronary artery disease (CAD), coronary artery bypass graft surgery (CABG) remains the optimal strategy for patients with severe and multivessel CADs. In addition, due to the multivessel nature of CAD in patients with T2DM, various studies have suggested that CABG surgery can be superior to PCI in patients with diabetes and other major cardiovascular risk factors [6,7,8]. Therefore, CABG surgery is more common among patients with diabetes.
Diabetes can also affect the postoperative outcomes of CABG [9, 10], besides having a greater risk of CAD and CAD-related death [11]. Thus, recent studies have reported worse postoperative outcomes for CABG patients with DM [12,13,14].
The northeastern region of Iran is significant due to its unique ethnic profile. Unlike other areas of the country, a large population of Turkmen ethnicities resides in this region [15]. Several studies of the population of northeastern Iran and Turkmen ethnics have reported a higher prevalence of congenital heart disorders [16], obesity [17], metabolic syndrome [18], cardiovascular diseases [19], hypertension [20], and a high waist circumference [18] compared to other regions of the country. According to the Golestan Cohort Study data, a significantly lower diabetes awareness was reported in this region [21]. The precise reason for these discrepancies is unknown. However, genetic predispositions, higher rural populations, and socioeconomic and lifestyle differences are considered the main contributing factors to this region’s higher prevalence of cardiovascular risk factors [19, 22].
Furthermore, there has been little research on the relationship between diabetes and cardiovascular disorders in this region. As a result, we sought to investigate the effect of T2DM on in-hospital major adverse cardiac and cerebrovascular events (MACCEs) and postoperative complications, such as postoperative arrhythmia, acute AF, major bleeding, and acute kidney injury (AKI) in patients undergoing on-pump isolated CABG in Iran’s northeastern region. Understanding the effects of diabetes on the postoperative outcomes of CABG surgery can be essential for applying better treatment strategies for these patients, considering the unique characteristics of the population in this region.
Methods
Study design
This retrospective cohort study was performed in northeastern Iran (Golestan province, Iran). The study protocol was approved by the institutional review board (IRB) (approval ID 950505.06) and research ethics committee (REC) (ID IR.GOUMS.REC.1395.137) of Golestan University of Medical Sciences in 2016.
Setting
In this study, we used the data registry of the characteristics of patients who underwent CABG surgery from 2007 to 2016 in Golestan province. Data were collected from two heart centers, including the Kordkuy heart center of Amiralmomenin hospital, affiliated with Golestan University of Medical Sciences (Gorgan, Iran), and the Shafa private heart center, which provides medical services to patients all over the province.
Participants
Adult patients (> 18 years old) of both sexes who had isolated on-pump CABG procedures between 2007 and 2016 and had complete data on study exposure (status of DM) and covariates were included in the study analysis.
Variables and measurement
Study variables were demographic and clinical, including past medical history, comorbidities, lipid profile, preoperative medications, clinical characteristics, and operation characteristics. The demographic variables included age, gender, ethnicity, obesity, opium consumption, and smoking status. Opium consumption and smoking status were self-reported data. We considered ethnicity as Turkmen and non-Turkmen ethnicities, the main ethnicities living in Golestan province. In order to define obesity, we calculated the body mass index (BMI) according to the weight and height of each patient. Then, according to the BMI categorization by the center for disease control and prevention (CDC), we considered a BMI of 30 or above as obese [23]. For past medical history, we retrieved the family history of cardiovascular diseases (CVDs) and previous myocardial infarction (MI), which were self-reported data. In addition, various comorbidities were assessed, including hyperlipidemia, hypertension (HTN), chronic obstructive pulmonary disease (COPD), and a lipid profile consisting of low-density lipoprotein (LDL), total cholesterol, and non-high-density lipoprotein (HDL) cholesterol. Non-HDL cholesterol refers to the total cholesterol value minus the HDL cholesterol value. Preoperative medications included Beta-blocker (BB), Statins, and Aspirin. Preoperative clinical characteristics were left ventricular ejection fraction (LVEF) by transthoracic echocardiography (TTE), diagnosis of three-vessel disease, and left main coronary artery (LMCA) stenosis by coronary artery angiography (CAG). Also, operation characteristics included emergency CABG, the left internal mammary artery (LIMA) graft, the number of grafts, cardiopulmonary bypass (CPB) time, and clamp time, which were recorded according to the surgeon’s and perfusionist’s report.
The study outcomes were in-hospital MACCEs (a composite outcome of MI, stroke, and cardiovascular death), postoperative arrhythmia, acute atrial fibrillation (AF), major bleeding, and AKI. Further interpretation and analysis regarding MACCE definitions are presented in the appendix.
-
Myocardial infarction was defined as clinical evidence of acute myocardial ischemia and detection of a rise in cardiac troponin levels with at least one value above the 99th percentile upper limit and at least one of the following:
-
Symptoms of myocardial ischemia
-
New ischemic electrocardiogram changes
-
Development of pathological Q waves [24]
-
-
Stroke was defined as a new focal neurological deficit that lasted more than 24 hours and was confirmed by imaging [25].
-
Postoperative AF and arrhythmias were detected by electrocardiograms (ECGs) read by the attending cardiologists.
-
Major postoperative bleeding was defined as significant bleeding requiring a reoperation [26].
-
AKI was defined as an absolute increase in serum creatinine concentration of 0.3 mg/dL or greater [27, 28].
-
Study exposure was T2DM, which was defined according to fasting plasma glucose (FPG) ≥126 mg/dl or using antidiabetic medications (i.e., Anti-diabetes oral tablets or Insulin).
Operative Procedure
After general anesthesia, a median sternotomy and aortic-right atrial cannulation were performed to achieve a cardiopulmonary bypass [29]. The ascending aorta was occluded, and a cardioplegic solution (Thomas crystalloid cardioplegia solution) was perfused into the heart during CABG [30, 31]. Several infusions of the cardioplegic solution might be administered if an electrical activity or prolonged ischemic time was observed. After completing distal anastomoses, the aortic cross-clamp was removed during myocardial revascularization. After reperfusion, partial occlusion clamps were used to complete the proximal anastomosis. The cross-clamp could still be used after the distal grafts have been conducted to facilitate the proximal grafts [32]. The left internal thoracic artery and greater saphenous vein were the most commonly used bypass grafts.
Statistical analysis
First, we compared the patients` data across diabetes status. The normality assumption for continuous variables was checked graphically by a histogram plot and the Shapiro-Wilk statistical test. Because of the non-normal distribution of the study variables, they were reported as the median and interquartile range (IQR) and were compared using Mann-Whitney U tests. In order to compare categorical variables, Chi-square tests were used, and the data were reported as numbers and percentages. We used univariate logistic regression analysis to evaluate the association between diabetes and in-hospital outcomes. Then, we used the change-in-estimate (CIE) criterion with a cut-off of more than 10% to detect the probable confounders of this association. Multiple logistic regression analysis was used to adjust for confounders identified by the CIE criterion. Both crude and adjusted ORs were reported for the association between diabetes and in-hospital outcomes with a 95% confidence interval (CI). Data analyses were performed by the statistical package STATA/IC version 14.2 (Stata Corp LP College Station, TX, USA).
Results
During the 10-year study from 2007 to 2016, demographic and clinical characteristics of 3704 patients who underwent on-pump isolated CABG surgery in the Golestan province were registered. Data related to 1748 patients were excluded due to incomplete data regarding study exposure and baseline data. Thus, the study population included 1956 patients (Fig. 1) with a mean (SD) age of 59.0 (9.60) years. According to the definitions, 1062 patients were non-diabetics, and 894 had diabetes.
Baseline Characteristics
The patients’ data are demonstrated in Table 1. According to this table, patients with DM were younger, and 44% were female, significantly different from patients without diabetes. Opium consumption and smoking were lower among patients with diabetes. The two groups were similar regarding family history of CVDs, prior MI, and comorbidities. Although there were no differences in lipid profiles between the two groups, LDL, total cholesterol, and non-HDL cholesterol levels were higher than normal values. The frequency of Beta-blocker, Statin and Aspirin consumption, three-vessel disease, and the number of grafts > 3 were higher among patients with diabetes compared to non-diabetics. The proportion of patients with DM with 40% LVEF was higher than in the non-diabetic group (20% vs. 17%), but this difference was not statistically significant (P = 0.061). However, CPB time and clamp time were similar among the two groups (Table 1).
Postoperative Data
In-hospital adverse events occurred in 5% (n/N = 44/894) of patients with diabetes and 4% (n/N = 39/1062) of patients without diabetes (P = 0.172). According to the crude analysis, diabetes was not significantly associated with in-hospital MACCEs (Crude OR 1.36, 95%CI 0.87, 2.11; P = 0.174). Furthermore, after adjustment for age, gender, ethnicity, obesity, opium consumption, and smoking, diabetes was not a predictor of major adverse events following CABG surgery (adjusted OR 1.35, 95% CI 0.86, 2.11; P = 0.188). (Table 2).
The distribution of postoperative complications in patients with and without diabetes is demonstrated in Fig. 2. Despite a higher proportion of in-hospital MACCEs and postoperative arrhythmia in patients with diabetes compared to non-diabetics, these differences were not statistically significant (P 0.174 and P 0.052, respectively).
Postoperative complications by diabetes. MACCEs: Major adverse cardiac and cerebrovascular events (i.e., composite of MI, stroke and cardiovascular death). Post-op: Postoperative. AF: Atrial fibrillation. DM: Diabetes. AKI: Acute kidney injury. P: Probability value (i.e. P < 0.05 was considered as statistically significant)
Table 2 compares postoperative complications between patients with and without diabetes mellitus undergoing isolated on-pump CABG surgery and indicates the results of the crude and adjusted analyses. According to this table, patients with diabetes experienced a higher proportion of in-hospital MACCEs compared to those without diabetes (5% vs. 4%, respectively). However, the crude analysis indicated no significant association between diabetes and in-hospital MACCEs (crude OR 1.36, 95% CI 0.87, 2.11; P = 0.174). Furthermore, diabetes was not a predictor of major adverse events following CABG surgery (adjusted OR 1.35, 95% CI 0.86, 2.11; P = 0.188) (Table 2).
Diabetic patients experienced a higher proportion of postoperative arrhythmia than non-diabetic patients (47% vs. 44%, respectively). However, it was not statistically significant (crude OR 1.20, 95% CI 0.99–1.43, P = 0.052). While, after adjustment by age, gender, ethnicity, obesity, opium consumption, and smoking status, we found an association between diabetes and postoperative arrhythmia, as diabetes was associated with a 30% increase in the risk of postoperative arrhythmia (adjusted OR 1.30, 95% CI 1.08–1.57, P = 0.006) (Table 2).
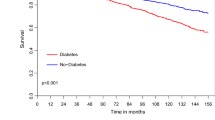
The proportions of acute AF, major bleeding, and AKI were not different between the two groups. Crude analyses indicated no association between diabetes and acute AF (Crude OR 0.80, 95% CI 0.60–1.1; P = 0.158), major bleeding (Crude OR 0.75, 95% CI 0.47–1.18; P = 0.216) or AKI (Crude OR 1.39, 95%CI 0.46, 4.15, P = 0.556) after surgery. Adjusted analyses indicated that diabetes was not a predictor of acute AF (adjusted OR 0.85, 95% CI 0.60–1.19, P = 0.340), major bleeding (adjusted OR 0.80, 95% CI 0.50–1.30, P = 0.636) or AKI (adjusted OR 1.29, 95% CI 0.42, 3.96, P = 0.656) after CABG surgery, as well (Table 2). The results of the adjusted analyses for study outcomes are demonstrated in Fig. 3.
Discussion
In this retrospective cohort study of patients undergoing CABG surgery, patients with T2DM were significantly younger and had a higher percentage of women than other patients. Diabetic patients were treated with more preoperative medications, including Beta-blockers, Statins, and Aspirin. Furthermore, being burdened with DM was significantly associated with a higher chance of developing three-vessel disease and receiving more than three grafts during the surgery. However, even after adjustment for other known risk factors, DM was not a predictor of in-hospital major adverse events in these patients. On the other hand, the adjusted analysis indicated that DM was a predictor of postoperative arrhythmias and increased the risk by 30%.
In addition to being a major risk factor for CAD, diabetes can affect the treatment strategy for CAD [33]. Accordingly, 20 to 30% of patients undergoing CABG are burdened with diabetes [34,35,36].
In our study, diabetic patients undergoing CABG surgery were significantly younger than non-diabetic patients (76.5% under 65 years old vs. 70%, P = 0.003). These results were consistent with the Wang et al. study [37], in which the mean age of diabetic patients treated with Insulin who underwent CABG was significantly lower than non-diabetic patients [mean (SD): 62.7 (9.3) vs. 64.2 (8.4), P < 0.001]. In this regard, Stamou et al. [38] revealed that DM was more common among CABG patients aged 60–69 years compared to patients older than 80 (28% vs. 15%). In a cohort study conducted in the USA and Canada, Carson et al. [34] showed that diabetic patients treated with Insulin undergoing CABG are younger than non-diabetic patients [mean (SD): 63.8 (10.2) vs. 65.1(1.09)]; Also, consistent with our study, they revealed that male gender predominancy was imperceptible among DM patients (55.4% vs. 74.0% for non-diabetics).
Three-vessel disease and LMCA stenosis are indications for CABG surgery [39]. In a 2015 study, Jia et al. [40] utilized CT coronary angiography to compare CAD in patients with and without DM. They reported a significant association between DM and the number of diseased segments [OR (95%CI): 2.14 (1.09–2.6)] and a higher rate of multivessel disease among diabetic patients (15% vs. 7%, P < 0.001). Our study showed that three-vessel disease was significantly more common among diabetic patients (71.0% vs. 66.5, P: 0.020), but no significant difference was observed regarding the left main coronary artery (LMCA) stenosis (P = 0.153). This was consistent with the Yamaguchi et al. [41] study, in which three-vessel disease was significantly more prevalent among diabetic CABG candidates (75.1% vs. 68.5%, P < 0.001). Furthermore, in their study, the proportion of LMCA stenosis was not significantly different among the two groups. In 2020, wang et al. [37] conducted a study on 4325 CABG patients and reported that both three-vessel disease and LMCA stenosis were significantly more common among Insulin treated diabetic patients compared to non-diabetic patients. In this regard, no difference was detected among non-diabetic and oral-treated diabetic patients.
In Yamaguchi et al. study [41], there was no significant difference between diabetic and non-diabetic patients regarding post-CABG in-hospital death or stroke; Our study supports their findings, suggesting that DM is not significantly associated with in-hospital adverse events. Further to previous studies, DM was not a predictor of in-hospital MACCE following CABG surgery after adjustment by other risk factors. Furthermore, in a Chinese cohort study by Zhang et al. [42], DM was not associated with in-hospital post-CABG death, cerebrovascular accident (CVA), or MI. However, it was a predictor of long-term death or CVA. Their study assessed the resources and surgery costs in both groups, revealing that DM patients had higher costs for both initial hospitalization and follow-up.
Additionally, we analyzed the distribution of other postoperative complications in the two groups. After adjustment for potential confounders, our analysis showed that DM is a predictor of postoperative arrhythmias, increasing its risk by 30%. However, we detected no association between diabetes and postoperative AF. Diabetic patients are generally associated with a higher rate of arrhythmia [43,44,45]. However, studies have contradictory reports regarding diabetes and postoperative arrhythmias; In a retrospective cohort study on the assessment of postoperative Atrial Fibrillation (POAF) in CABG patients, Ismail et al. reported diabetes as an independent factor for POAF in these patients [46]. Mangi et al. also reported significantly higher rates of diabetes in post-CABG patients with POAF compared to patients without postoperative arrhythmia [47]. Although, in a meta-analysis on post-CABG arrhythmia by Woldendorp et al., diabetes was not significantly higher in patients with POAF compared to patients with a normal postoperative sinus rhythm [48].
One of the most serious postoperative complications in our patients was post-CABG major bleeding. The adjusted analysis indicated that diabetes was not associated with major postoperative bleeding in CABG patients. In a multicenter European study, Biancari et al. assessed the risk factors of post-CABG bleeding. Similar to our results, they indicated that diabetes was not associated with an increased risk of post-CABG bleeding [49]. Moreover, in the results of a large-scale study on post-CABG bleeding by Hansson et al., diabetes was also not associated with post-CABG bleeding [26].
Furthermore, our study failed to detect an association between diabetes and postoperative AKI. Previous studies have reported contradictive results. While various studies have indicated diabetes as a risk factor for postoperative AKI [50,51,52], several other studies did not suggest diabetes as a significant risk factor [53,54,55]. Inconsistencies in the definition of AKI might be a main contributing factor to the variations observed in the study results [56].
Due to its high prevalence and increasing incidence rate, diabetes is a significant public health issue in Iran [20, 57, 58]. Additionally, compared to previous years, the age-standardized mortality rate of DM had a notable rise in 2015 (11.3% in 2015 vs. 8.7% in 2000) [59]. In a 2011 study, Javanbakht et al. [60] reported 842.6 ± 102 USD for the average medical cost of diabetes per capita, and 412.8 ± 64.5 USD were complication costs. They reported cardiovascular disease expenditure as the most significant complication cost component (42.3%). Thus, conducting extensive studies on the issue in different regions is necessary to develop effective management strategies for cardiovascular disease in diabetic patients.
Limitations
This large-scale study was conducted in Northeastern Iran. The current study was the first from this region, including ethnic diversities, especially Turkmen ethnicity. However, our study faced some limitations. Several variables, such as duration of diabetes, HbA1C level, and type of antidiabetic medications (oral pills or Insulin), were unavailable in the dataset we used to consider in the analysis, which may affect the study results. In this study, the in-hospital outcome was considered, and the long-term outcomes were not evaluated.
Conclusion
To the best of our knowledge, this is the first study from Northeastern Iran focusing on the effect of DM on the in-hospital MACCEs and postoperative complications after CABG surgery. Severe and multivessel coronary artery disease was more common among diabetic CABG patients compared to other CABG patients. This difference could explain the higher number of grafts used in these patients during the operation. Despite the differences, the risk of in-hospital MACCEs, acute AF, major bleeding, and AKI was not statistically significant between diabetic and non-diabetic patients following a CABG surgery. While, diabetes was associated with a 30% increase in the risk of postoperative arrhythmia, which requires further attention.
Availability of data and materials
The datasets regarding the current study are available from the corresponding author upon reasonable request.
Abbreviations
- DM:
-
Diabetes mellitus
- CABG:
-
Coronary artery bypass graft
- T2DM:
-
Type 2 diabetes mellitus
- MACCEs :
-
Major adverse cardiac and cerebrovascular events
- FPG:
-
Fasting plasma glucose
- AKI:
-
Acute kidney injury
- SD:
-
Standard deviation
- PCI:
-
Percutaneous interventions
- CAD:
-
Coronary artery disease
- HTN:
-
Hypertension
- REC:
-
Research ethics committee
- BMI:
-
Body mass index
- CDC:
-
Center for disease control and prevention
- MI:
-
Myocardial infarction
- COPD:
-
Chronic obstructive pulmonary disease
- LDL:
-
Low-density lipoprotein
- HDL:
-
High-density lipoprotein
- BB:
-
Beta-blocker
- LVEF:
-
Left ventricular ejection fraction
- TTE:
-
Transthoracic echocardiography
- LMCA:
-
Left main coronary artery
- CAG:
-
Coronary artery angiography
- LIMA:
-
Left internal mammary artery
- IQR:
-
Interquartile range
- CIE:
-
Change-in-estimate
- CPB:
-
Cardio pulmonary bypass
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- ICU:
-
Intensive care unit
- POAF:
-
Post operative atrial fibrilation
References
World Health Organization. Global report on diabetes. Geneva: World Health Organization; 2016. Available from: https://apps.who.int/iris/handle/10665/204871
Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018;17(1):83.
Al Busaidi N, Shanmugam P, Manoharan D. Diabetes in the Middle East: government health care policies and strategies that address the growing diabetes prevalence in the Middle East. Curr Diab Rep. 2019;19(2):8.
Zabetian A, Keli HM, Echouffo-Tcheugui JB, Narayan KMV, Ali MK. Diabetes in the Middle East and North Africa. Diabetes Res Clin Pract. 2013;101(2):106–22.
Glovaci D, Fan W, Wong ND. Epidemiology of diabetes mellitus and cardiovascular disease. Curr Cardiol Rep. 2019;21(4):21.
Godoy LC, Rao V, Farkouh ME. Diabetes and multivessel disease: coronary artery bypass grafting remains king. Curr Opin Cardiol. 2018;33(5):551–7.
Aronson D, Edelman ER. Coronary artery disease and diabetes mellitus. Cardiol Clin. 2014;32(3):439–55.
Bianco V, Kilic A, Mulukutla SR, Gleason TG, Kliner D, Aranda-Michel E, et al. Coronary artery bypass grafting vs percutaneous coronary intervention in patients with diabetes. Semin Thorac Cardiovasc Surg. 2021;33(2):368–77.
Kim YG, Park DW, Lee WS, Park GM, Sun BJ, Lee CH, et al. Influence of diabetes mellitus on long-term (five-year) outcomes of drug-eluting stents and coronary artery bypass grafting for multivessel coronary revascularization. Am J Cardiol. 2012;109(11):1548–57.
aeen FB, Pakzad R, Tayebi Z, Kashkooli RI, Abdi F. Clinical outcomes of off-pump coronary artery bypass graft in patients with diabetes and non-diabetics: a systematic review and meta-analysis. Diabetes Metab Syndr Clin Res Rev. 2022;16(11):102643.
Herlitz J, Wognsen GB, Karlson BW, Sjöland H, Karlsson T, Caidahl K, et al. Mortality, mode of death and risk indicators for death during 5 years after coronary artery bypass grafting among patients with and without a history of diabetes mellitus. Coron Artery Dis. 2000;11(4):339–46.
Bundhun PK, Bhurtu A, Yuan J. Impact of type 2 diabetes mellitus on the long-term mortality in patients who were treated by coronary artery bypass surgery: a systematic review and meta-analysis. Medicine (Baltimore). 2017;96(22):e7022.
Skendelas JP, Phan DK, Friedmann P, Rodriguez CJ, Stein D, Arbab-Zadeh A, et al. Perioperative cardiometabolic targets and coronary artery bypass surgery mortality in patients with diabetes. J Am Heart Assoc. 2022;11(9):e023558.
Herlitz J, Wognsen GB, Emanuelsson H, Haglid M, Karlson BW, Karlsson T, et al. Mortality and morbidity in diabetic and non-diabetic patients during a 2-year period after coronary artery bypass grafting. Diabetes Care. 1996;19(7):698–703.
Golalipour MJ, Jahanshahi M, Haidari K. Morphological evaluation of head in Turkman males in Gorgan-North of Iran. Int J Morphol. 2007;25(1):99–102.
Nikyar B, Sedehi M, Qorbani M, Nikyar A, Golalipour MJ. Ethnical variations in the incidence of congenital heart defects in Gorgan, Northern Iran: a single-center study. J Tehran Univ Heart Cent. 2014;9(1):9.
Veghari G, Sedaghat M, Maghsodlo S, Banihashem S, Moharloei P, Angizeh A, et al. Differences in the prevalence of obesity among fars-native, turkman, and sisstanish ethnic groups in Iranian Northern adults in 2010. 2013;
Shahini N, Shahini I, Marjani A. Prevalence of metabolic syndrome in Turkmen ethnic groups in Gorgan. J Clin Diagn Res JCDR. 2013;7(9):1849.
Khoddam H, Alemi Z, Modanloo M. Comparison of prevalence and risk factors of acute coronary syndrome in patients with different ethnicity: a cross-sectional study. Ethiop J Health Sci. 2021;31(5).
Malekzadeh H, Lotfaliany M, Ostovar A, Hadaegh F, Azizi F, Yoosefi M, et al. Trends in cardiovascular risk factors in diabetic patients in comparison to general population in Iran: findings from National Surveys 2007–2016. Sci Rep. 2020;10(1):11724.
Golozar A, Khademi H, Kamangar F, Poutschi H, Islami F, Abnet CC, et al. Diabetes mellitus and its correlates in an Iranian adult population. PLoS One. 2011;6(10):e26725.
Rafati R, Jalal R, Asoodeh A, Matin MM. Brief report: Association Of RS12255372 (TCF7L2) And D76N (PDX-1) polymorphisms with type 2 diabetes in a population living in Northeast Iran; 2015.
All About Adult BMI. In: Centers for Disease Control and Prevention; CDC, 2022. Available from: https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html. cited 2022 Nov 11.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation. 2018;138(20):e618–51.
Chandrasekhar J, Marley P, Allada C, McGill D, O’Connor S, Rahman M, et al. Symptom-to-balloon time is a strong predictor of adverse events following primary percutaneous coronary intervention: results from the Australian Capital Territory PCI registry. Heart Lung Circ. 2017;26(1):41–8.
Hansson EC, Jidéus L, Åberg B, Bjursten H, Dreifaldt M, Holmgren A, et al. Coronary artery bypass grafting-related bleeding complications in patients treated with ticagrelor or clopidogrel: a nationwide study. Eur Heart J. 2016;37(2):189–97.
Benedetto U, Angeloni E, Luciani R, Refice S, Stefanelli M, Comito C, et al. Acute kidney injury after coronary artery bypass grafting: does rhabdomyolysis play a role? J Thorac Cardiovasc Surg. 2010;140(2):464–70.
Chang TI, Leong TK, Boothroyd DB, Hlatky MA, Go AS. Acute kidney injury after CABG versus PCI: an observational study using 2 cohorts. J Am Coll Cardiol. 2014;64(10):985–94.
Abramov D, Tamariz MG, Fremes SE, Guru V, Borger MA, Christakis GT, et al. Trends in coronary artery bypass surgery results: a recent, 9-year study. Ann Thorac Surg. 2000;70(1):84–90.
Carvajal C, Goyal A, Tadi P. Cardioplegia. StatPearls: StatPearls Publishing; 2021.
Melikulov A, Merzlyakov VY, Klyuchnikov I, Akhmedova M. Coronary artery bypass grafting in high-risk patients.
Cohn LH, Adams DH. Cardiac surgery in the adult: McGraw-Hill Education; 2017.
Arnold SV, Bhatt DL, Barsness GW, Beatty AL, Deedwania PC, Inzucchi SE, et al. Clinical management of stable coronary artery disease in patients with type 2 diabetes mellitus: a scientific statement from the american heart association. Circulation. 2020;141(19):e779–806.
Carson JL, Scholz PM, Chen AY, Peterson ED, Gold J, Schneider SH. Diabetes mellitus increases short-term mortality and morbidity in patients undergoing coronary artery bypass graft surgery. J Am Coll Cardiol. 2002;40(3):418–23.
Sarnak MJ, Amann K, Bangalore S, Cavalcante JL, Charytan DM, Craig JC, et al. Chronic kidney disease and coronary artery disease. J Am Coll Cardiol. 2019;74(14):1823–38.
Turner RC, Millns H, Neil HAW, Stratton IM, Manley SE, Matthews DR, et al. Risk factors for coronary artery disease in non-insulin dependent diabetes mellitus: United Kingdom prospective diabetes study (UKPDS: 23). BMJ. 1998;316(7134):823.
Wang R, Zhang H, Zhu Y, Chen W, Chen X. The impact of diabetes mellitus on acute kidney injury after coronary artery bypass grafting. J Cardiothorac Surg. 2020;15(1):289.
Stamou SC, Dangas G, Dullum MKC, Pfister AJ, Boyce SW, Bafi AS, et al. Beating heart surgery in octogenarians: perioperative outcome and comparison with younger age groups. Ann Thorac Surg. 6.
null nullHillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, et al. 2011 ACCF/AHA Guideline for coronary artery bypass graft surgery. Circulation. 2011;124(23):e652–735.
Jia S. Characteristics of coronary artery lesion in patients with and without diabetes mellitus. Ir J Med Sci. :8.
Yamaguchi A, Kimura N, Itoh S, Adachi K, Yuri K, Okamura H, et al. Efficacy of multiple arterial coronary bypass grafting in patients with diabetes mellitus. Eur J Cardiothorac Surg. 2016;50(3):520–7.
Zhang H, Yuan X, Osnabrugge RLJ, Meng D, Gao H, Zhang S, et al. Influence of diabetes mellitus on long-term clinical and economic outcomes after coronary artery bypass grafting. Ann Thorac Surg. 2014;97(6):2073–9.
Agarwal G, Singh SK. Arrhythmias in type 2 diabetes mellitus. Indian J Endocrinol Metab. 2017;21(5):715–8.
Wang A, Green JB, Halperin JL, Piccini JP. Atrial fibrillation and diabetes mellitus: JACC review topic of the week. J Am Coll Cardiol. 2019;74(8):1107–15.
Fitzpatrick C, Chatterjee S, Seidu S, Bodicoat DH, Ng GA, Davies MJ, et al. Association of hypoglycaemia and risk of cardiac arrhythmia in patients with diabetes mellitus: a systematic review and meta-analysis. Diabetes Obes Metab. 2018;20(9):2169–78.
Ismail MF, El-Mahrouk AF, Hamouda TH, Radwan H, Haneef A, Jamjoom AA. Factors influencing postoperative atrial fibrillation in patients undergoing on-pump coronary artery bypass grafting, single center experience. J Cardiothorac Surg. 2017;12(1):40.
Mangi AR, Zia K, Ali TA, Karim M, Fatimi SH. Postoperative atrial fibrillation among patients undergoing isolated coronary artery bypass grafting. Cureus. 2019;11(3) Available from: https://www.cureus.com/articles/18733-postoperative-atrial-fibrillation-among-patients-undergoing-isolated-coronary-artery-bypass-grafting. Cited 2023 Jan 13.
Woldendorp K, Farag J, Khadra S, Black D, Robinson B, Bannon P. Postoperative Atrial Fibrillation After Cardiac Surgery: A Meta-Analysis. Ann Thorac Surg. 2021;112(6):2084–93.
Biancari F, Brascia D, Onorati F, Reichart D, Perrotti A, Ruggieri VG, et al. Prediction of severe bleeding after coronary surgery: the WILL-BLEED Risk Score. Thromb Haemost. 2017;117(3):445–56.
Oezkur M, Wagner M, Weismann D, Krannich JH, Schimmer C, Riegler C, et al. Chronic hyperglycemia is associated with acute kidney injury in patients undergoing CABG surgery--a cohort study. BMC Cardiovasc Disord. 2015;15:41.
Amini S, Najafi MN, Karrari SP, Mashhadi ME, Mirzaei S, Tashnizi MA, et al. Risk factors and outcome of acute kidney injury after isolated CABG surgery: a prospective cohort study. Braz J Cardiovasc Surg. 2019;34(1):70–5.
Kristovic D, Horvatic I, Husedzinovic I, Sutlic Z, Rudez I, Baric D, et al. Cardiac surgery-associated acute kidney injury: risk factors analysis and comparison of prediction models. Interact Cardiovasc Thorac Surg. 2015;21(3):366–73.
Ortega-Loubon C, Fernández-Molina M, Pañeda-Delgado L, Jorge-Monjas P, Carrascal Y. Predictors of Postoperative Acute Kidney Injury after Coronary Artery Bypass Graft Surgery. Braz J Cardiovasc Surg. 2018;33(4):323–9.
Barkhordari K, Fakhre Yasseri AM, Yousefshahi F, Shafiee A. Risk factors for acute kidney injury in coronary artery bypass graft surgery patients based on the acute kidney injury network criteria. J Tehran Univ Heart Cent. 2018;13(2):52–7.
Fortescue EB, Bates DW, Chertow GM. Predicting acute renal failure after coronary bypass surgery: cross-validation of two risk-stratification algorithms. Kidney Int. 2000;57(6):2594–602.
Seabra VF, Alobaidi S, Balk EM, Poon AH, Jaber BL. Off-pump coronary artery bypass surgery and acute kidney injury: a meta-analysis of randomized controlled trials. Clin J Am Soc Nephrol CJASN. 2010;5(10):1734–44.
Esteghamati A, Khalilzadeh O, Anvari M, Meysamie A, Abbasi M, Forouzanfar M, et al. The economic costs of diabetes: a population-based study in Tehran. Iran Diabetologia. 2009;52(8):1520–7.
Mirzaei M, Rahmaninan M, Mirzaei M, Nadjarzadeh A, Dehghani tafti AA. Epidemiology of diabetes mellitus, pre-diabetes, undiagnosed and uncontrolled diabetes in Central Iran: results from Yazd health study. BMC Public Health. 2020;20(1):166.
Veisani Y, Khazaei S, Jenabi E, Delpisheh A. Diabetes mortality and morbidity trends and related risk factors in Iranian Adults: an appraisal via current Data. J Tehran Heart Cent. 2018;13(4):195–7.
Javanbakht M, Baradaran HR, Mashayekhi A, Haghdoost AA, Khamseh ME, Kharazmi E, et al. Cost-of-illness analysis of type 2 diabetes mellitus in Iran. PLoS One. 2011;6(10):e26864.
Nomali M, Heidari ME, Ayati A, Moghaddam K, Mosallami S, Khosravi A, et al. Risk factors of in-hospital mortality for isolated on-pump coronary artery bypass graft surgery in the northeast of Iran from 2007 to 2016. Ir J Med Sci. 2023. https://doi.org/10.1007/s11845-023-03298-6. Epub ahead of print.
Acknowledgments
In this article, we used the dataset [61] from the study and received a grant from the student research committee of Iran’s ministry of health. The authors would like to thank the Student Research Committee and Research and Technology Deputy of Golestan University of Medical Sciences (Gorgan, Iran) for their support in facilitating the study.
Funding
All funding was provided by the grant from the National Student Research Committee of the Ministry of Health and the Research and Technology Deputy of Golestan University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
Conceptualization and Design: MN, AA, KM, GR, SM, GR. Data Curation: MN, KM, MR, MY, MN, GR, SM. Data Analysis and Interpretation: MN, AA, ME, GR. Drafting and Revision: AA, MN, AT, GR. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and consent to participate
This study was approved by the institutional review board (IRB) of Golestan University of Medical Sciences (GOUMS) on 26 July 2016 (approval no.950505.06) and the research ethics committee (REC) on 4 September 2016 (approval no. IR.GOUMS.REC.1395.137). All methods were carried out in accordance with relevant guidelines and regulations. Since we used the CABG data registry, written informed consent was not applicable in the present study.
Consent for publication
All authors have consent for publication of the article.
Competing interests
All authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix
. Table S1. Comparison of In-hospital MACCEs (+Acute kidney injury) between patients with and without diabetes mellitus undergoing isolated on-pump CABG surgery.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nomali, M., Ayati, A., Tayebi, A. et al. Type 2 diabetes mellitus and In-hospital Major Adverse Cardiac and Cerebrovascular Events (MACCEs) and postoperative complications among patients undergoing on-pump isolated coronary artery bypass surgery in Northeastern Iran. BMC Cardiovasc Disord 23, 130 (2023). https://doi.org/10.1186/s12872-023-03163-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03163-5