Abstract
Objective
In this study we aimed to compare on-pump and off-pump coronary artery bypass grafting (CABG) outcomes in patients presented with low left ventricular ejection fraction (EF) as a high-risk group of patients.
Methods
In this registry-based study from 2014 and 2016, all patients with severe left ventricular dysfunction (EF less than 35%) were included and followed until 2020. The median follow-up period was 47.83 [38.41, 55.19] months. Off pump CABG (OPCABG) was compared with on-pump CABG (ONCABG) in terms of mid-term non-fatal cardiovascular events (CVEs) and all-cause mortality. Propensity score method (with inverse probability weighting technique) was used to compare these two groups.
Results
From 14,237 patients who underwent isolated CABG, 2055 patients with EF ≤ 35% were included; 1705 in ONCABG and 350 patients in OPCABG groups. Although OPCABG was associated with lower risk of 30-days mortality (Odds Ratio [OR]: 0.021; Confidence Interval [CI] 95% [0.01, 0.05], P < 0.001); there was no significant difference between OPCABG and ONCABG in term of mid-term mortality and non-fatal CVEs ((Hazard ratio [HR]: 0.822; 95%CI [0.605, 1.112], p = 0.208) and (HR: 1.246; 95%CI [0.805, 1.929], p = 0.324), respectively). Patients with more than three traditional coronary artery disease risk factors, had more favorable outcomes (in terms of mid-term mortality) if underwent OPCABG (HR: 0.420; 95%CI [0.178, 0.992], p = 0.048).
Conclusion
OPCABG was associated with lower risk of 30-days mortality; however, mid-term outcomes were comparable in both OPCABG and ONCABG techniques.
Similar content being viewed by others
Introduction
Coronary artery bypass grafting (CABG) has long been used for surgical revascularization in patients with coronary artery disease (CAD) and is most commonly performed using cardiopulmonary bypass (CPB) (on-pump CABG, ONCABG) [1]. Besides other known predictive factors such as diabetes mellitus, kidney disease and advanced age; left ventricular dysfunction is an important risk factor that might affect surgical coronary revascularization outcomes [2, 3]. It has been shown that reduced ejection fraction (EF) is associated with poor short- and long-term outcomes after CABG and ejection fraction is a component of preoperative risk assessment [4, 5]. Moreover, patients with reduced EF have several comorbid conditions that may affect the post-CABG outcomes [6]. However, CABG is the treatment of choice in those with low left ventricular EF and several studies have shown a long-term survival benefit after CABG in those patients, compared to medical treatment [6]. CABG can be done with two techniques; off vs. on pump and although, several studies compared these methods, there are too many controversies in results [7]. As technology has advanced, OPCABG is well tolerated by most patients [8]; however, this procedure may be associated with incomplete revascularization and also hemodynamic deterioration especially in patients with left ventricular dysfunction [9, 10]. Multiple reports have been published on the outcomes of ONCABG and OPCABG in patients with low left ventricular EF, however the results are conflicting [11, 12].
In this study, we aimed to compare early and mid-term outcomes of ONCABG vs. OPCABG in patients presented with left ventricular dysfunction.
Methods
Study cohort
This study is a registry-based cohort which conducted retrospectively in clinical registry of Tehran Heart Center [13]. We reported this study according to the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) statement. Patients who underwent isolated CABG from January 2014 to December 2016 were retrospectively evaluated, additionally patients with lack of adequate data were excluded from the study. Inclusion criteria comprised patients with: (1) A pre-operation EF ≤ 35%, which was evaluated by transthoracic echocardiography (TTE); (2) Surgical revascularization criteria for ischemic heart disease [14]; and (3) No requirement for concomitant valve surgery or minimally invasive direct coronary artery bypass‐surgery. The main exclusion criteria were incomplete registry data and loss to follow up. Conclusively, 2055 patients were selected for this study.
Definition of variables
EF was evaluated through an expert cardiologist via eyeballing and Simpson technique. Diabetes mellitus was defined as fasting plasma glucose ≥ 126 mg/dL and/or random plasma glucose ≥ 200 mg/dL and/or hemoglobin A1c (HbA1c) ≥ 6.5% [15] and/or treatment with either oral hypoglycemic agents or insulin. Minimum systolic blood pressure of 140 mm Hg or a minimum diastolic blood pressure of 90 mm Hg or a history of antihypertensive therapy labeled as hypertension. Dyslipidemia considers as existence one of follows, minimum total cholesterol level of 240 mg/dL; LDL-C level more than 160 mg/dL; a minimum triglyceride level of 200 mg/dL; and HDL-C of less than 40 mg/dL in men and less than 50 mg/dL in women; or a history of prescribed lipid medications based on the National Cholesterol Education Program (NCEP) Adult Treatment Plan (ATP) III [16]. Renal failure was defined as glomerular filtration rate < 60 mL/min/1.73 m2 or stage 3a and higher chronic kidney disease. Cerebrovascular accident was defined as, ischemic stroke, hemorrhagic stroke, and transient ischemic attack. A family history of CAD was defined as having a first-degree relative with a history of CAD; i.e., acute myocardial infarction or documented CAD, which diagnosed by either invasive coronary angiography or computed tomography coronary angiography. Cigarette smoking status was defined as current smoker and stated from the patient’s self-reported status. Opium consumption was defined as the current consumption of opium either smoking opium or drinking opium dissolved in tea. Patients divided into three categories in the term of urgency of the procedure, emergent (surgery should take place as soon as possible, in the following 6 h), urgent (surgery should take place in the following 6–24 h), and elective.
Surgical technique
To reduce the effect of differential expertise bias, all surgeons who performed procedures were highly experienced in both OPCABG and ONCABG. All surgeons which included in this study has been performed at least 500 OPCABG and ONCABG procedures. The selection of patients to receive either on-pump or off-pump CABG was by surgeon discretion at the time of the procedure. “No-touch” technique was preformed to harvest saphenous vein grafts (SVG) and “pedicled technique” was performed to harvest left and right internal mammary arteries (LIMA and RIMA). The procedure routine was using LIMA for the left ascending artery (LAD) and SVG for right coronary, left circumflex, and diagonal artery, furthermore the choices of using grafting conduits was based on surgeon’s preference concerning.
For ONCABG procedure, single right atrium and aortic cannulation was made to achieve CPB, furthermore, Heparin was used to conserve activated clotting time (ACT) at ≥ 480 s. During the surgery anterograde cold blood cardioplegia was made. Protamine sulfate prescribed to neutralize the Heparin at the end of surgery. The patients’ systemic temperature was sustained at 36 °C to avoid hypothermia-induced arrhythmia.
For OPCABG procedure, carbon dioxide blower (Medtronic Inc., Minneapolis, MN) was used for better visualization of operative field and anastomosis cites. Heparin was given to reach ACT ≥ 350 s. Proximal anastomoses to the aorta was made by 6‐0 monofilament sutures, while 8–0 monofilament sutures was used for distal anastomosis.
Follow up and study endpoints
The patients follow up protocol was as follows; 4, 6, and 12 months after surgery and annually after last visit through attending visits at the post-op clinics. For individuals who were incapable to appear at the clinics, telephone interviews were made.
The primary endpoints were in-hospital mortality (which was defined as death occurring during the same hospital admission or first 30 days mortality after procedure), mid-term all-cause mortality, and mid-term non-fatal cardiovascular events (CVEs) occurrence (acute coronary syndrome, need for repeat revascularization [percutaneous coronary intervention [PCI] or redo-CABG], stroke or transient ischemic attack).
Statistical analysis
Descriptive statistics were used to describe baseline characteristics, subsequently, categorical variables were described as absolute and frequencies, and continuous variables were reported as mean and standard deviation or median and interquartile range according to their distribution. The Fisher’s exact test or the chi-squared test was used to compare categorical variables. Normally and non-normally distributed continuous variables were compared using Student t-test and Mann–Whitney U test, respectively.
Inverse probability weights (IPW) used to stabilize potential selection biases of treatment, balance variables, and confounders adjustment (Additional file 1: Table S1). Weights were calculated from propensity score (PS) (Additional file 1: Figure S2), which was generated by predicted probabilities of logistic regression on identified potential confounders. The C-statistic for the model was 0.81 (Additional file 1: Figure S1). Weights for each case (Wi) calculated as 1/PS(Xi) for Off-pump surgery, and 1/(1 − PS(Xi)) for On-pump surgery. The confounders selected based on three main criteria. First of all, we considered only available variables in our data bank. Second, we considered clinically proven confounders for IPW estimation. In the last step we used bidirectional selection, by utilizing multivariable cox-regression to include other variables with P-value < 0.25 in our estimation.
Sensitivity analysis conducted using multivariable proportional hazard models. The standardized mean difference (SMD) used as balance metric to evaluate the difference between distributions of a pre-treatment variable, balance indicator considered as ‘SMD < 0.1’(Additional file 1; Table S2).
Event rates were based on Kaplan–Meier estimates in time to first event. log-rank test and univariate proportional hazard model were preformed to compare to surgical methods. On-pump surgery was considered as reference in all reported hazard ratios (HRs). The multiple comparisons of off-pump strategy effect in the subgroup analysis were performed using multiple tests with Bonferroni-adjusted correction and (p-value < 0.007) considered as significant.
All statistical analyses were conducted applying IBM SPSS Statistics for Mac, version 26.0 (Armonk, NY: IBM Corp.) and R version 4.0.3. Besides, we used several packages in R: "survival" (package for survival analysis in R), "survminer" (drawing survival curves), and “ggplot2”.
Results
Study population
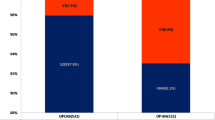
Totally 14,237 patients underwent isolated CABG surgery between January 2014 and December 2016 were included in this study. After concerning inclusion and exclusion criteria 2055 patients were remained (Fig. 1). Consequently, 350 and 1705 patients underwent OPCABG and ONCABG, respectively. The median follow-up period was 47.83 [38.41, 55.19] months.
Patients’ demographics and preoperative data are summarized in Table 1. Briefly, 24% and 19.7% of patients were female in OPCABG and ONCABG (p = 0.070), respectively. The mean age of individuals was 62.05 years in OPCABG and 61.82 years in ONCABG (p = 0.429).
Survival outcomes
Table 2 demonstrated the absolute number of 4-P MACE events. In-hospital and mid-term mortality was significantly lower in OPCABG group, (2.0% vs 4.0%, p < 0.001, and 19.1% vs 26.4%, p < 0.001). Hence; the incidence of ACS and revascularization were same in both technique.
First 30-days mortality
In-hospital mortality was lower in OPCABG group (OR: 0.136; 95%CI [0.068, 0.274], p < 0.001) in non-adjusted model and adjusted inverse probability weighting-based model (OR: 0.21; 95%CI [0.14, 0.52], P < 0.001).
All-cause mortality
All-cause mortality rate was 25.16 percent in overall (Fig. 2). Table 2 demonstrated incidence rate in each studied group. OPCABG was associated with lower risk of mortality (HR: 0.687; 95%CI [0.532, 0.889], p = 0.004) (Fig. 3A). However, after adjustment for different confounders according to weighted method (IPW technique), there was no differences between two surgical methods (HR: 0.822; 95%CI [0.605, 1.112], p = 0.208) (Fig. 3B). Sensitivity analysis with in parallel with our main results (Table 3).
Non-fatal cardiovascular events (CVEs)
Non-fatal CVEs rate was 6.8 percent among all patients. In both non-adjusted and adjusted models, non-fatal CVEs were not different between two groups; HR: 1.329 95%CI [0.887, 1.992], p = 0.168 for non-adjusted model) (Fig. 4A) and (HR: 1.246; 95%CI [0.805, 1.929], p = 0.324) (Fig. 4B) in IPW.
Subgroup Analysis
Table 4 demonstrate subgroup analysis for mortality and non-fatal CVEs. “Risk factor > 3” was the single factor which modify the results, which was not significant according to multiple test correction. There were no other factors which impact our main results.
Discussion
In this conducted study, we aimed to compare 30-day mortality, mid-term mortality and mid-term non-fatal CVEs in 2055 patients with left ventricular dysfunction (EF ≤ 35%) who underwent either off or on pump CABG procedure. In-hospital mortality was significantly lower in patients underwent OPCABG. However, mid-term results were comparable in both groups. In current study, we implanted IPW, which uses the whole data set and by reweighting individuals, increases the weight of those with unexpected exposures; ultimately, IPW creates a pseudo-population in which the covariates are balanced excellent between studied groups [17].
Management of patients with CAD and low EF remains a challenge; however, CABG seems to be a good surgical option in terms of survival and quality of life [18]. Moreover, ventricular dysfunction is considered as a risk factor for worse prognosis after cardiac surgery [19, 20]. The lower risk of in-hospital mortality in patients underwent OPCABG compared to ONCABG could be partly explain by the effect of CPB. Using CPB pump, as in ONCABG procedure, could increases organism’s inflammatory, oxidative and coagulators stress [21] mostly due to conversion of laminar flow, interaction of blood with the artificial bypass surface, hypothermia, and cold cardiac ischemia; consequently, this may affect outcomes of patients after CABG especially low EF population. Additionally, damaging effect of CPB could be partially explained by changing the geometry of left ventricle, which causes obstruction of coronary collateral flow that supplies ischemic myocardium [22]. Instead, OPCABG is associated with less inflammatory release, less hypercoagulable state, reduced transfusion requirement, and lower risk of postoperative kidney disease and may be more beneficial in patients with low EF [23, 24]. Based on previous conducted study, one possible reason for this improvement in in-hospital outcomes after OPCABG for patients with low EF may be the lack of ischemia during off-pump procedure and the performance of fewer distal anastomoses [25].
Based on previous studies, high-risk CABG candidates may benefit from avoiding CPB (OPCABG) [22, 26, 27]. This is in line with our findings which indicated that high-risk patients with more than three CAD risk factors had better survival when underwent OPCABG. This may be explained by CBP inflammatory reactions, higher risk of myocardial infarction after ONCABG [28], and renal dysfunction after ONCABG due to systemic inflammation and hypoperfusion [29]. It has been shown that oxidative metabolism recovers rapidly after off-pump bypass surgery and also the degree of myocyte injury and intraoperative cardiac troponin T concentrations are lesser in OPCABG compared to on-pump surgery [28]. Thus, elimination of CBP in addition to use of minimal incisions, as are seen in off-pump coronary bypass, may help to reduce the inflammatory reactions and lead to better outcomes compared to ONCABG [22, 30].
Although several studies have been compared off-pump and on-pump CABG in patients with low EF, the results are conflicting. Few studies showed that OPCABG was associated with lower risk of in-hospital mortality [2, 25], and some showed that in-hospital outcomes were the same between OPCABG and ONCABG [31,32,33,34,35]. Regarding mid- and long-term outcomes, in line with our results, some studies showed similar risk between off- and on-pump procedures [33, 34]. There are several conducted studies in this field, although none of them consider individuals genomic and epigenomic profiles composed. Future studies should identify the finest care for an individual based on a unique personal profile instead of the normal population [36].
The present study should be interpreted in the context of several possible limitations. First, due to lack of “cause of death” data recording, we were unable to specify “cause of death” in each patient. Moreover, unmeasured variables including surgery time duration and post-operative variables may alter our results and identified or unadjusted confounding effects cannot be ruled out for the association of lower 30-day mortality with OPCABG. Furthermore, our findings were based on 4-year follow up, and further studies with longer follow-up are needed to achieve results that are more accurate. This study was conducted in a single medical center (THC) and the generalizability of our results should be assessed. Still, THC is the referral educational university, which serves patients from all of the country. In order to precisely compare OPCABG and ONCABG we need large randomized clinical trials however, with IPW technique, we tried to overcome this limitation. IPW method balance two groups according to their risk factors, which computes from propensity scores for each patient.
The major strengths of this study are as follows; first, we adjusted our results with IPW to overcome the influence of baseline characteristics differences on the final result; hence, all study population maintained; second, our data extracted from THC registry data bank which records patient’s data prospectively; third, to overcome surgical expertise limitation, we chose expert surgeons who had done at least 100 and 400 OPCABG and ONCABG procedures previously.
In conclusion, for patients with ventricular dysfunction and EF ≤ 35% who need surgical coronary revascularization, OPCABG techniques compared to ONCABG strategies are associated with superior short-term results and comparable or even better mid-term outcomes, especially in those with multiple risk factors.
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available due Tehran Heart Center data privacy protocol, but are available from the corresponding author (K.H) on reasonable request.
References
Hoffman SN, TenBrook JA, Wolf MP, Pauker SG, Salem DN, Wong JB. A meta-analysis of randomized controlled trials comparing coronary artery bypass graft with percutaneous transluminal coronary angioplasty: one- to eight-year outcomes. J Am Coll Cardiol. 2003;41(8):1293–304.
Guan Z, Guan X, Gu K, Lin X, Lin J, Zhou W, et al. Short-term outcomes of on- vs off-pump coronary artery bypass grafting in patients with left ventricular dysfunction: a systematic review and meta-analysis. J Cardiothorac Surg. 2020;15(1):84.
Ahmed WA, Tully PJ, Baker RA, Knight JL. Survival after isolated coronary artery bypass grafting in patients with severe left ventricular dysfunction. Ann Thorac Surg. 2009;87(4):1106–12.
Hillis GS, Zehr KJ, Williams AW, Schaff HV, Orzulak TA, Daly RC, et al. Outcome of patients with low ejection fraction undergoing coronary artery bypass grafting: renal function and mortality after 3.8 years. Circulation. 2006;114(1 Suppl):I414–9.
Dalén M, Lund LH, Ivert T, Holzmann MJ, Sartipy U. Survival after coronary artery bypass grafting in patients with preoperative heart failure and preserved vs reduced ejection fraction. JAMA Cardiol. 2016;1(5):530–8.
Topkara VK, Cheema FH, Kesavaramanujam S, Mercando ML, Cheema AF, Namerow PB, et al. Coronary artery bypass grafting in patients with low ejection fraction. Circulation. 2005;112(9_supplement):I-344–I−350.
Thakur U, Nerlekar N, Muthalaly RG, Comella A, Wong NC, Cameron JD, et al. Off- vs. on-pump coronary artery bypass grafting long-term survival is driven by incompleteness of revascularisation. Heart Lung Circ. 2020;29(1):149–55.
Verma S, Fedak PWM, Weisel RD, Szmitko PE, Badiwala MV, Bonneau D, et al. Off-pump coronary artery bypass surgery. Circulation. 2004;109(10):1206–11.
Benedetto U, Gaudino M, Di Franco A, Caputo M, Ohmes LB, Grau J, et al. Incomplete revascularization and long-term survival after coronary artery bypass surgery. Int J Cardiol. 2018;254:59–63.
Mishra M, Shrivastava S, Dhar A, Bapna R, Mishra A, Meharwal ZS, et al. A prospective evaluation of hemodynamic instability during off-pump coronary artery bypass surgery. J Cardiothorac Vasc Anesth. 2003;17(4):452–8.
Darwazah AK, Abu Sham’a RA, Hussein E, Hawari MH, Ismail H. Myocardial revascularization in patients with low ejection fraction ≤35%: effect of pump technique on early morbidity and mortality. J Card Surg. 2006;21(1):22–7.
Emmert MY, Salzberg SP, Theusinger OM, Rodriguez H, Sündermann SH, Plass A, et al. Off-pump surgery for the poor ventricle? Heart Vessels. 2012;27(3):258–64.
Poorhosseini H, Abbasi SH. The Tehran Heart Center. Eur Heart J. 2018;39(29):2695–6.
Eagle KA, Guyton RA, Davidoff R, Ewy GA, Fonger J, Gardner TJ, et al. ACC/AHA guidelines for coronary artery bypass graft surgery: executive summary and recommendations: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to revise the 1991 guidelines for coronary artery bypass graft surgery). Circulation. 1999;100(13):1464–80.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–9.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1082–143.
Sheikhy A, Fallahzadeh A, Sadeghian S, Forouzannia K, Bagheri J, Salehi-Omran A, et al. Mid-term outcomes of off-pump versus on-pump coronary artery bypass graft surgery; statistical challenges in comparison. BMC Cardiovasc Disord. 2021;21(1):412.
Velazquez EJ, Lee KL, Jones RH, Al-Khalidi HR, Hill JA, Panza JA, et al. Coronary-artery bypass surgery in patients with ischemic cardiomyopathy. N Engl J Med. 2016;374(16):1511–20.
Yau TM, Fedak PWM, Weisel RD, Teng C, Ivanov J. Predictors of operative risk for coronary bypass operations in patients with left ventricular dysfunction. J Thorac Cardiovasc Surg. 1999;118(6):1006–13.
Fallahzadeh A, Sheikhy A, Ajam A, Sadeghian S, Pashang M, Shirzad M, et al. Significance of preoperative left ventricular ejection fraction in 5-year outcome after isolated CABG. J Cardiothorac Surg. 2021;16(1):353.
Alam SR, Stirrat C, Spath N, Zamvar V, Pessotto R, Dweck MR, et al. Myocardial inflammation, injury and infarction during on-pump coronary artery bypass graft surgery. J Cardiothorac Surg. 2017;12(1):115.
Stamou SC, Corso PJ. Coronary revascularization without cardiopulmonary bypass in high-risk patients: a route to the future. Ann Thorac Surg. 2001;71(3):1056–61.
Paone G, Brewer R, Theurer PF, Bell GF, Cogan CM, Prager RL. Preoperative predicted risk does not fully explain the association between red blood cell transfusion and mortality in coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2012;143(1):178–85.
Garg AX, Devereaux PJ, Yusuf S, Cuerden MS, Parikh CR, Coca SG, et al. Kidney function after off-pump or on-pump coronary artery bypass graft surgery: a randomized clinical trial. JAMA. 2014;311(21):2191–8.
Keeling WB, Williams ML, Slaughter MS, Zhao Y, Puskas JD. Off-pump and on-pump coronary revascularization in patients with low ejection fraction: a report from the society of thoracic surgeons national database. Ann Thorac Surg. 2013;96(1):83–8 (discussion 8-9).
Magee MJ, Coombs LP, Peterson ED, Mack MJ. Patient selection and current practice strategy for off-pump coronary artery bypass surgery. Circulation. 2003;108(10_suppl_1):II-9–II−14.
Yokoyama T, Baumgartner FJ, Gheissari A, Capouya ER, Panagiotides GP, Declusin RJ. Off-pump versus on-pump coronary bypass in high-risk subgroups. Ann Thorac Surg. 2000;70(5):1546–50.
Koh TW, Carr-White GS, DeSouza AC, Ferdinand FD, Hooper J, Kemp M, et al. Intraoperative cardiac troponin T release and lactate metabolism during coronary artery surgery: comparison of beating heart with conventional coronary artery surgery with cardiopulmonary bypass. Heart (Br Cardiac Soc). 1999;81(5):495–500.
Ascione R, Lloyd CT, Underwood MJ, Lotto AA, Pitsis AA, Angelini GD. Inflammatory response after coronary revascularization with or without cardiopulmonary bypass. Ann Thorac Surg. 2000;69(4):1198–204.
Gu YJ, Mariani MA, van Oeveren W, Grandjean JG, Boonstra PW. Reduction of the inflammatory response in patients undergoing minimally invasive coronary artery bypass grafting. Ann Thorac Surg. 1998;65(2):420–4.
Xia L, Ji Q, Song K, Shen J, Shi Y, Ma R, et al. Early clinical outcomes of on-pump beating-heart versus off-pump technique for surgical revascularization in patients with severe left ventricular dysfunction: the experience of a single center. J Cardiothorac Surg. 2017;12(1):11.
Neumann A, Serna-Higuita L, Detzel H, Popov AF, Krüger T, Vöhringer L, et al. Off-pump coronary artery bypass grafting for patients with severely reduced ventricular function—a justified strategy? J Card Surg. 2021. https://doi.org/10.1111/jocs.16054.
Zhou Z, Liang M, Zhuang X, Liu M, Fu G, Liu Q, et al. Long-term outcomes after on-pump vs off-pump coronary artery bypass grafting for ischemic cardiomyopathy. Ann Thorac Surg. 2022. https://doi.org/10.1016/j.athoracsur.2021.12.063.
Marin-Cuartas M, Deo SV, Ramirez P, Verevkin A, Leontyev S, Borger MA, et al. Off-pump coronary artery bypass grafting is safe and effective in patients with severe left ventricular dysfunction. Eur J Cardiothorac Surg. 2021;61(3):705–13.
Shennib H, Endo M, Benhamed O, Morin JF. Surgical revascularization in patients with poor left ventricular function: on- or off-pump? Ann Thorac Surg. 2002;74(4):S1344–7.
Sheikhy A, Fallahzadeh A, Aghaei Meybodi HR, Hasanzad M, Tajdini M, Hosseini K. Personalized medicine in cardiovascular disease: review of literature. J Diabetes Metab Disord. 2021;20(2):1793–805.
Acknowledgements
Our sincerest gratitude goes to the research division and data base registry section of Tehran Heart Center.
Funding
None.
Author information
Authors and Affiliations
Contributions
KH and SS contributed in study design and draft revision. AS, AF, and MT contributed in drafting. AS contributed in data analysis. MP and KF contributed in data gathering. SM (Momtahen), SM (Mansourian), and MS contributed in data gathering and critical revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study approved by Tehran Heart Center (THC) ethical board (IR-THC-13799) and involving human data was in accordance to guidelines of Declaration of Helsinki. This study didn’t meet criteria for informed consent form. THC ethical board waived informed consent form since no human personal information reported.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Table S1. Variables used in propensity score estimations. Fig. S1. C-statistic for propensity score modeling. Fig. S2. Estimated Propensity scores. Table S2. Standardized mean differences (SMD) percentage of characteristic variables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sheikhy, A., Fallahzadeh, A., Forouzannia, K. et al. Off-pump versus on-pump coronary artery bypass graft surgery outcomes in patients with severe left ventricle dysfunction: inverse probability weighted study. BMC Cardiovasc Disord 22, 488 (2022). https://doi.org/10.1186/s12872-022-02895-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-022-02895-0